ThisisPatientEngagementcontent
Achalasia
Learn more about our Patient Engagement products now! Turn your patients into active participants in their healthcare by giving them easy access to the same evidence-based information you trust – but delivered in an easy-to-understand format.
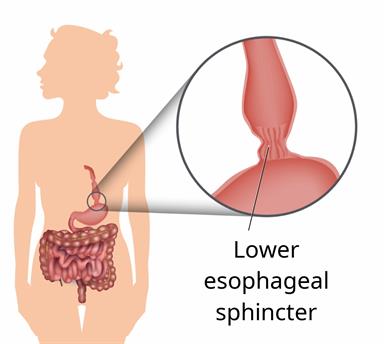
Your esophagus is the part of your body that moves food from your mouth to your stomach. When you swallow, muscles in a part of your esophagus called the lower esophageal sphincter (LES) relax to let food into your stomach.
If the muscles don't relax like they should, you may have a condition called achalasia. This can cause there to be more pressure near the LES. It can also make it hard for you to swallow.
The cause of this condition is not known.
Eating and drinking
General instructions
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.