Acute Bronchitis, Pediatric
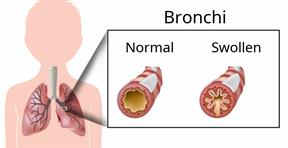
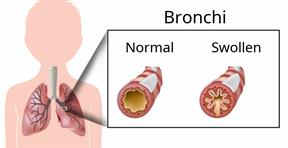
Acute bronchitis is sudden inflammation of the main airways (bronchi) that come off the windpipe (trachea) in the lungs. The swelling causes the airways to get smaller and make more mucus than normal. This can make it hard for your child to breathe and can cause coughing or loud breathing (wheezing).
Acute bronchitis may last several weeks. The cough may last longer. Allergies, asthma, and exposure to smoke may make the condition worse.
What are the causes?
This condition can be caused by germs and by substances that irritate the lungs, including:
Cold and flu viruses. The most common cause of this condition is the virus that causes the common cold.
In children younger than 1 year, the most common cause of this condition is respiratory syncytial virus (RSV).
Bacteria. This is less common.
- Substances that irritate the lungs, including:
Smoke from cigarettes and other forms of tobacco.
Dust and pollen.
Fumes from household cleaning products, gases, or burned fuel.
Indoor and outdoor air pollution.
What increases the risk?
This condition is more likely to develop in children who:
Have a weak body defense system, or immune system.
Have a condition that affects their lungs and breathing, such as asthma.
What are the signs or symptoms?
Symptoms of this condition include:
Coughing. This may bring up clear, yellow, or green mucus from your child's lungs (sputum).
Wheezing.
Runny or stuffy nose.
Having too much mucus in the lungs (chest congestion).
Shortness of breath.
Aches and pains, including sore throat or chest.
How is this diagnosed?
This condition is diagnosed based on:
Your child's symptoms and medical history.
A physical exam. During the exam, your child's health care provider will listen to your child's lungs.
Your child may also have other tests, including tests to rule out other conditions, such as pneumonia. These tests include:
How is this treated?
Most cases of acute bronchitis go away over time without treatment. Your child's health care provider may recommend:
Having your child drink more fluids. This can thin your child's mucus so it is easier to cough up.
Giving your child inhaled medicine (inhaler) to improve air flow in and out of his or her lungs.
Using a vaporizer or a humidifier. These are machines that add water to the air to help with breathing.
Giving your child a medicine that thins mucus and clears congestion (expectorant).
It isnot common to take an antibiotic for this condition.
Follow these instructions at home:
Medicines
-
Give over-the-counter and prescription medicines only as told by your child's health care provider.
-
Do not give honey or honey-based cough products to children who are younger than 1 year because of the risk of botulism. For children who are older than 1 year, honey can help to lessen coughing.
-
Do not give your child cough suppressant medicines unless your child's health care provider says that it is okay. In most cases, cough medicines should not be given to children who are younger than 6 years.
-
Do not give your child aspirin because of the association with Reye's syndrome.
General instructions

-
Have your child get plenty of rest.
-
Have your child drink enough fluid to keep his or her urine pale yellow.
-
Do not allow your child to use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes.
-
Do not smoke around your child. If you or your child needs help quitting, ask your health care provider.
-
Have your child return to his or her normal activities as told by his or her health care provider. Ask your child's health care provider what activities are safe for your child.
-
Keep all follow-up visits. This is important.
How is this prevented?

To lower your child's risk of getting this condition again:
Make sure your child washes his or her hands often with soap and water for at least 20 seconds. If soap and water are not available, have your child use hand sanitizer.
Have your child avoid contact with people who have cold symptoms.
Tell your child to avoid touching his or her mouth, nose, or eyes with his or her hands.
Keep all of your child's routine shots (immunizations) up to date. Make sure your child gets the flu shot every year.
Help your child avoid breathing secondhand smoke and other harmful substances.
Contact a health care provider if:
-
Your child's cough or wheezing lasts for 2 weeks or gets worse.
-
Your child has trouble coughing up the mucus.
-
Your child's cough keeps him or her awake at night.
-
Your child has a fever.
-
Has trouble breathing.
-
Coughs up blood.
-
Feels pain in his or her chest.
-
Feels faint or passes out.
-
Has a severe headache.
-
Is younger than 3 months and has a temperature of 100.4°F (38°C) or higher.
-
Is 3 months to 3 years old and has a temperature of 102.2°F (39°C) or higher.
These symptoms may represent a serious problem that is an emergency. Do not wait to see if the symptoms will go away. Get medical help right away. Call your local emergency services (911 in the U.S.).
Summary
-
Acute bronchitis is inflammation of the main airways (bronchi) that come off the windpipe (trachea) in the lungs. The swelling causes the airways to get smaller and make more mucus than normal.
-
Give your child over-the-counter and prescription medicines only as told by your child's health care provider.
-
Do not smoke around your child. If you or your child needs help quitting, ask your health care provider.
-
Have your child drink enough fluid to keep his or her urine pale yellow.
-
Contact a health care provider if your child's symptoms do not improve after 2 weeks.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.

 To lower your child's risk of getting this condition again:
To lower your child's risk of getting this condition again: