Acute Coronary Syndrome
Acute coronary syndrome (ACS) is a serious problem in which there is suddenly not enough blood and oxygen reaching the heart. ACS can result in chest pain or a heart attack.
This condition is a medical emergency. If you have any symptoms of this condition, get help right away.
What are the causes?
This condition may be caused by:
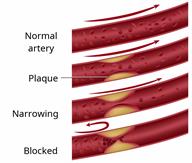
Atherosclerosis, which is a buildup of fat and cholesterol inside the arteries. This is the most common cause. The buildup (plaque) can cause blood vessels in the heart (coronary arteries) to become narrow or blocked, reducing blood flow to the heart. Plaque can also break off and lead to a clot, which can block an artery and cause a heart attack or stroke.
Sudden tightening of the muscles around the coronary arteries. This is called a coronary spasm.
Tearing of a coronary artery (spontaneous coronary artery dissection).
Very low blood pressure (hypotension).
An abnormal heartbeat (arrhythmia).
Other medical conditions that cause a decrease of oxygen to the heart, such as anemiaorrespiratory failure.
Using drugs such as cocaine or methamphetamine.
What increases the risk?
The following factors may make you more likely to develop this condition:
Age. The risk for ACS increases as you get older.
Personal or family history of chest pain, heart attack, peripheral vascular disease, or stroke.
Having taken chemotherapy or immune-suppressing medicines.
Being male.
Being overweight.
- Having any of these conditions:
- Lifestyle choices such as:
Excessive alcohol use.
Not exercising enough.
Smoking.
What are the signs or symptoms?
Common symptoms of this condition include:
- Chest pain. The pain may last a long time, or it may stop and come back (recur). It may feel like:
Arm, neck, jaw, or back pain.
Heartburn or indigestion.
Shortness of breath.
Nausea.
Sudden cold sweats.
Light-headedness, dizziness, or passing out.
Tiredness (fatigue).
Sometimes there are no symptoms.
How is this diagnosed?
This condition may be diagnosed based on:
How is this treated?
Treatment for this condition may include:
Follow these instructions at home:
Medicines
Eating and drinking
-
Eat a heart-healthy diet that includes whole grains, fruits and vegetables, lean proteins, and low-fat or nonfat dairy products.
-
Limit how much salt (sodium) you eat as told by your health care provider. Follow instructions from your health care provider about any other eating or drinking restrictions, such as limiting foods that are high in fat and processed sugars.
-
Use healthy cooking methods such as roasting, grilling, broiling, baking, poaching, steaming, or stir-frying.
-
Work with a dietitian to follow a heart-healthy eating plan.
Activity
-
Follow your cardiac rehabilitation program. Do exercises as told by your physical therapist.
-
Ask your health care provider what activities and exercises are safe for you. Follow his or her instructions about lifting, driving, or climbing stairs.
Lifestyle
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
-
Do not drink alcohol if:
Your health care provider tells you not to drink.
You are pregnant, may be pregnant, or are planning to become pregnant.
- If you drink alcohol:
- Limit how much you have to:
Know how much alcohol is in your drink. In the U.S., one drink equals one 12 oz bottle of beer (355 mL), one 5 oz glass of wine (148 mL), or one 1½ oz glass of hard liquor (44 mL).
-
Maintain a healthy weight. If you need to lose weight, work with your health care provider to do so safely.
General instructions
-
Tell all the health care providers who provide care for you about your heart condition, including your dentist. This may affect the medicines or treatment you receive.
-
Manage any other health conditions you have, such as hypertension or diabetes. These conditions affect your heart.
- Pay attention to your mental health. You may be at higher risk for depression.
- Keep your vaccinations up to date.
-
If directed, monitor your blood pressure at home.
-
Keep all follow-up visits. This is important.
Contact a health care provider if:
-
You feel overwhelmed or sad.
-
You have trouble doing your daily activities.
-
You have dark stools or blood in your stool.
-
You have sudden light-headedness or dizziness.
These symptoms may represent a serious problem that is an emergency. Do not wait to see if the symptoms will go away. Get medical help right away. Call your local emergency services (911 in the U.S.). Do not drive yourself to the hospital.
Summary
-
Acute coronary syndrome (ACS) is when there is not enough blood and oxygen being supplied to the heart. ACS can result in chest pain or a heart attack.
-
Treatment includes medicines and procedures to open the blocked arteries and restore blood flow.
-
Acute coronary syndrome is a medical emergency. Get help right away if you have sudden pain in your chest, arms, back, neck, jaw, or upper body. Seek help if you have unexplained nausea, vomiting, or shortness of breath.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.
 This condition may be caused by:
This condition may be caused by: