Acute Respiratory Distress Syndrome, Pediatric
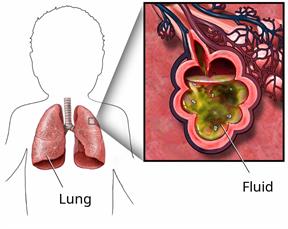
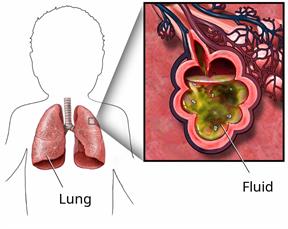
Acute respiratory distress syndrome (ARDS) is when the lungs become inflamed, causing blood vessels to swell and leak fluid into the air sacs (alveoli). This prevents the lungs from working well. It also makes it hard to get oxygen into the blood. As a result, other vital organs can get damaged, such as the heart, kidneys, liver, or brain.
ARDS is a life-threatening condition. It needs treatment in an intensive care unit (ICU) in a hospital.
What are the causes?
The condition usually happens because of a major illness, surgery, injury, or widespread infection (sepsis).
Other causes may include:
An infection in the blood, lungs, or kidneys.
A serious injury to the head, chest, or other areas of the body.
Breathing in harmful chemicals, smoke, water, or vomit.
Getting donated blood (blood transfusion).
Inflammation of the pancreas (pancreatitis).
What are the signs or symptoms?
The main symptoms of this condition are sudden shortness of breath and fast, shallow breathing.
Other symptoms may include:
A fast or irregular heartbeat.
Crackling sounds in the lungs.
Grunting or flaring of the nostrils when breathing.
Tiredness or loss of energy.
Chest pain, especially when taking a breath.
Coughing.
Feeling restless or anxious.
How is this diagnosed?
This condition is diagnosed based on your child's medical history, symptoms, and a physical exam.
Your child may also have other tests, including:
A test that measures the amount of oxygen in your child's blood (pulse oximetry). This is done with a sensor that is placed on your child's finger, toe, or earlobe.
Blood tests.
Chest X-rays or CT scans to look for fluid in the lungs.
Tests to rule out other conditions or infections in your child's body.
How is this treated?
The goal of treatment is to support your child while the lungs heal and the underlying cause is treated. Treatment may include:
Oxygen therapy.
- Noninvasive ventilation. This is a device to help with breathing by giving oxygen and pressure through a mask or helmet. Examples of these machines are:
Prone positioning. This means having your child lie on their stomach.
A breathing machine called a ventilator. This gives your child oxygen and pressure through a tube that is put through the mouth and into the windpipe (trachea).
Tracheostomy placement, if your child is on a ventilator for a long time. A tracheostomy is a breathing tube put through the neck and into the trachea.
Fluid and medicine given through an IV.
- Medicines that:
Help your child relax (sedatives).
Treat blood pressure.
Treat infection (antibiotics).
Prevent blood clots (anticoagulants).
Help get rid of extra fluid (diuretics).
Extracorporeal life support (ECLS), in severe cases. This treatment takes over the actions of the heart and lungs for a short time. ECLS gives oxygen and removes carbon dioxide. It also gives the lungs a chance to rest and recover.
Follow these instructions at home:
Medicines
-
Give your child over-the-counter and prescription medicines only as told by your child's health care provider.
-
Do not give your child aspirin because of the association with Reye's syndrome.
-
If your child was prescribed antibiotics, give them as told by the health care provider. Do not stop giving the antibiotic even if your child starts to feel better.
General instructions

-
Do not allow your child to use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If your child needs help quitting, ask a health care provider.
-
Do not smoke around your child.
-
Have your child return to normal activities as told by the health care provider. Ask the health care provider what activities are safe for your child.
-
It may take your child a while to get back to doing normal activities and routines.
-
Your child may feel depressed or anxious, or have trouble with memory and focus. Talk with the health care provider about ways to help your child feel better.
-
Keep all follow-up visits.
Contact a health care provider if:
-
Your child becomes short of breath during activity or while resting.
-
Your child develops a cough that does not go away.
-
Your child has a fever.
-
Your child's symptoms do not get better or they get worse.
-
Your child becomes anxious or depressed, or does not feel like doing their normal activities.
-
Your child has trouble breathing.
-
Your child who is younger than 3 months has a temperature of 100.4°F (38°C) or higher.
-
Your child who is 3 months to 3 years old has a temperature of 102.2°F (39°C) or higher.
-
Your child gets sudden chest pain that does not go away.
-
Your child's heart starts beating very fast.
-
Your child gets swelling or pain in one leg.
-
Your child coughs up blood.
-
Your child's skin, lips, or fingernails turn blue.
These symptoms may be an emergency. Do not wait to see if the symptoms will go away. Get help right away. Call 911.
Summary
-
Acute respiratory distress syndrome (ARDS) is when the lungs become inflamed, causing blood vessels to swell and leak fluid into the air sacs (alveoli). This prevents the lungs from working well and is life-threatening.
-
ARDS usually happens because of a major illness, surgery, injury, or widespread infection (sepsis).
-
If your child was prescribed antibiotics, give them as told by the health care provider. Do not stop giving the antibiotic even if your child starts to feel better.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.