ThisiscontentfromElsevier'sDrugInformation
Amphetamine; Dextroamphetamine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
5 mg PO once or twice daily, initially.[54902] May increase the dose by 5 mg/day at weekly intervals based on clinical response.[31563] Usual Max: 40 mg/day.[54902] Doses more than 40 mg/day are rarely needed.[31563] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
5 mg PO once or twice daily, initially.[54902] May increase the dose by 5 mg/day at weekly intervals based on clinical response.[31563] Usual Max: 40 mg/day.[54902] Doses more than 40 mg/day are rarely needed.[31563] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
5 mg PO once or twice daily, initially. May increase the dose by 5 mg/day at weekly intervals based on clinical response.[31563] However, a maximum dose of 60 mg/day may be considered.[45900] [54902] Use the lowest effective dose.[31563] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
5 mg PO once or twice daily, initially. May increase the dose by 5 mg/day at weekly intervals based on clinical response. Usual Max: 40 mg/day. Doses more than 40 mg/day are rarely needed. Use the lowest effective dose.[31563] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
2.5 mg PO once daily in the morning, initially. May increase the dose by 2.5 mg/day at weekly intervals based on clinical response. Usual Max: 40 mg/day.[31563] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332] The American Academy of Pediatrics (AAP) does not recommend the use of dextroamphetamine in this age group due to lack of safety and efficacy data.[46924]
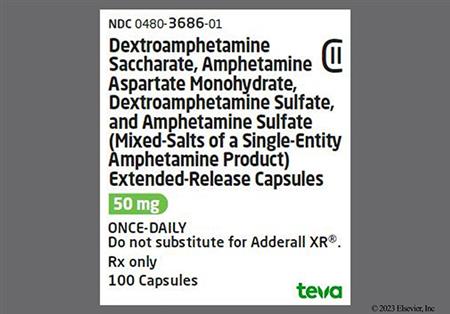
20 mg PO once daily in the morning. In clinical trials, titration doses were allowed up to 60 mg/day; however, there was no consistent evidence that doses above 20 mg/day conferred additional benefit. Persons taking divided doses of immediate-release amphetamine; dextroamphetamine (e.g., twice daily), may be switched to extended-release amphetamine; dextroamphetamine at the same total daily dose taken once daily. Use the lowest effective dose. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
10 mg PO once daily in the morning, initially. May increase the dose to 20 mg/day after 1 week based on clinical response. In clinical trials, titration doses were allowed up to 40 mg/day for weight 75 kg or less and from 50 to 60 mg/day for weight more than 75 kg; however, there was no consistent evidence that doses above 20 mg/day conferred additional benefit. Persons taking divided doses of immediate-release amphetamine; dextroamphetamine (e.g., twice daily), may be switched to extended-release amphetamine; dextroamphetamine at the same total daily dose taken once daily. Use the lowest effective dose. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
5 to 10 mg PO once daily in the morning, initially. May increase the dose by 5 to 10 mg/day at weekly intervals based on clinical response. Max: 30 mg/day. Persons taking divided doses of immediate-release amphetamine; dextroamphetamine (e.g., twice daily), may be switched to extended-release amphetamine; dextroamphetamine at the same total daily dose taken once daily. Use the lowest effective dose. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[29332]
12.5 mg PO once daily in the morning, initially; an initial dose of 25 mg PO once daily may be considered for some. May increase the dose by 12.5 mg/day at weekly intervals based on clinical response. Max: 50 mg/day. Doses more than 50 mg/day have not shown additional clinically meaningful benefit. Use the lowest effective dose. For patients switching from another medication or amphetamine product, discontinue that treatment, and titrate using the titration schedule. Do not substitute for other amphetamine products on a milligram-per-milligram basis because of different amphetamine base compositions and differing pharmacokinetic profiles. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[62038]
12.5 mg PO once daily in the morning, initially. May increase the dose by 12.5 mg/day at weekly intervals based on clinical response. Max: 25 mg/day. Use the lowest effective dose. For patients switching from another medication or amphetamine product, discontinue that treatment, and titrate using the titration schedule. Do not substitute for other amphetamine products on a milligram-per-milligram basis because of different amphetamine base compositions and differing pharmacokinetic profiles. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[62038]
5 to 60 mg/day PO in 2 or 3 divided doses.[31563] [72190] [72191]
10 mg/day PO in 1 to 3 divided doses, initially. May increase the dose by 10 mg/day at weekly intervals based on clinical response and tolerability. Max: 60 mg/day.[31563] [72191] [72193]
5 mg/day PO in 1 to 3 divided doses, initially. May increase the dose by 5 mg/day at weekly intervals based on clinical response and tolerability. Max: 60 mg/day.[31563] [72191] [72193]
Usual dose: 60 to 80 mg/day. Some data indicate patients may require dosing at or above the FDA-labeled max dose for ADHD in order to effectively reduce cocaine use (low certainty, conditional recommendation). A meta-analysis indicated that psychostimulant medications, including extended-release mixed amphetamine salts (ER-MAS), were associated with better cocaine-related outcomes, including sustained abstinence and cocaine-negative urine screen results. However, no difference was noted in treatment retention. ER-MAS may be particularly helpful in individuals with comorbid ADHD to assist with treatment of both conditions simultaneously. Results of a randomized, placebo-controlled trial in adults with cocaine use disorder and concomitant ADHD showed that patients receiving ER-MAS had significant improvement in ADHD symptom severity as well as reduced cocaine use and improved rates of continuous abstinence vs. placebo. One guideline suggests that the use of psychostimulants for this indication be limited to specialists who are board certified in addiction medicine, addiction psychiatry, or commensurate training and competency.[70082]
Doses up to 60 mg/day, given along with topiramate therapy, have been used. Some data indicate patients may require dosing at or above the FDA-labeled max dose for ADHD in order to effectively reduce cocaine use (low certainty, conditional recommendation). The extended-release mixed amphetamine salts (ER-MAS) in combination with topiramate may be helpful for reducing cocaine cravings and achieving cocaine abstinence. A meta-analysis found the combination had positive effects in establishing a period of cocaine abstinence when compared to placebo treatment. Additionally, a randomized controlled trial demonstrated that cocaine cravings decreased more quickly with combination treatment vs. placebo. These effects may be even more pronounced in patients with frequent cocaine use. This combination may be helpful for patients with comorbid ADHD or alcohol use disorder, as topiramate has shown benefit in reducing alcohol consumption. One guideline suggests that the use of psychostimulants for this indication be limited to specialists who are board certified in addiction medicine, addiction psychiatry, or commensurate training and competency.[70082]
For immediate-release tablets, 40 mg/day PO for ADHD (doses up to 60 mg/day PO have been used for weight more than 50 kg) or 60 mg/day PO for narcolepsy. For extended-release Adderall XR capsules, 20 mg/day PO is the recommended dose; in clinical trials for adult ADHD, 60 mg/day PO was the highest titration dose used. For extended-release Mydayis capsules, 50 mg/day PO for ADHD.
For immediate-release tablets, 60 mg/day PO for narcolepsy; geriatric patients have not been evaluated for ADHD. For extended-release capsules, geriatric patients have not been evaluated.
For immediate-release tablets, 40 mg/day PO for ADHD (doses up to 60 mg/day PO have been used for weight more than 50 kg) or 60 mg/day PO for narcolepsy. In clinical trials of extended-release Adderall XR capsules, titration doses were allowed up to 40 mg/day PO for weight 75 kg or less and from 50 to 60 mg/day PO for weight more than 75 kg; however, there was no consistent evidence that doses above 20 mg/day PO conferred additional benefit. For extended-release Mydayis capsules, 25 mg/day PO for ADHD.
6 years and older: For immediate-release tablets, 40 mg/day PO for ADHD (doses up to 60 mg/day PO have been used for weight more than 50 kg) or 60 mg/day PO for narcolepsy. For extended-release Adderall XR capsules, 30 mg/day PO for ADHD. For extended-release Mydayis capsules, safety and efficacy have not been established.
3 to 5 years: Maximum dosage information is not provided by FDA-approved labeling; doses should not exceed 40 mg/day PO for immediate-release tablets. Do not use extended-release capsules.
Less than 3 years: Safety and efficacy have not been established.
Not indicated.
Specific guidelines for dosage adjustments in hepatic impairment are not available; the FDA-approved product labeling states that hepatic dysfunction has the potential to inhibit the elimination of amphetamine and result in prolonged exposures; use caution.[29332][31563][62038]
Immediate-release products:
Specific guidelines for dosage adjustments of immediate-release products in renal impairment in adults and pediatric patients are not available; the FDA-approved product labeling states that renal dysfunction has the potential to inhibit the elimination of amphetamine and result in prolonged exposures; use caution.[31563]
ADULT RENAL DOSE ADJUSTMENTS
Adult renal dose adjustments for extended-release capsules (Adderall XR)
eGFR 15 to 29 mL/minute/1.73 m2: 15 mg PO once daily in the morning.
eGFR less than 15 mL/minute/1.73 m2: Initiation of extended-release capsules (Adderall XR) is not recommended.[29332]
Adult renal dose adjustments for extended-release capsules (Mydayis)
eGFR 15 to 29 mL/minute/1.73 m2: Starting dose is is 12.5 mg PO once daily. Maximum dose is 25 mg PO once daily.
eGFR less than 15 mL/minute/1.73 m2: Initiation of extended-release capsules (Mydayis) is not recommended.[62038]
PEDIATRIC RENAL DOSE ADJUSTMENTS
Pediatric renal dose adjustments (6 to 17 years of age) for extended-release capsules (Adderall XR)
eGFR 15 to 29 mL/minute/1.73 m2: 5 mg PO once daily is the recommended dose. The maximum dose for children 6 to 12 years of age is 20 mg PO once daily.
eGFR less than 15 mL/minute/1.73 m2: Initiation of extended-release capsules (Adderall XR) is not recommended.[29332]
Pediatric renal dose adjustments (13 to 17 years of age) for extended-release capsules (Mydayis)
eGFR 15 to 29 mL/minute/1.73 m2: Starting and maximum dose is is 12.5 mg PO daily.
eGFR less than 15 mL/minute/1.73 m2: Initiation of extended-release capsules (Mydayis) is not recommended.[62038]
† Off-label indication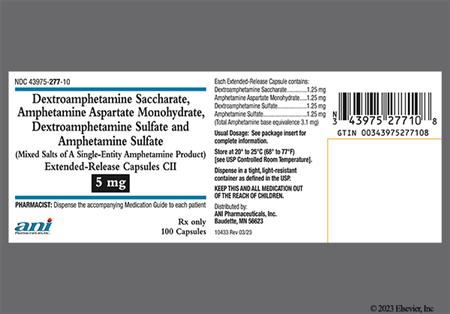






























Amphetamine and dextroamphetamine mixed salts are used in combination as an oral preparation to treat attention-deficit hyperactivity disorder (ADHD) or narcolepsy. Stimulants are considered first-line agents in the treatment of ADHD.[31567][31586][31588][31589] Amphetamine- and methylphenidate-containing products are considered equally effective in the treatment of ADHD; patients who do not respond to one may respond to the other. The most common adverse reactions associated with amphetamine use include anorexia, abdominal pain, irritability, restlessness, insomnia, emotional lability, and tachycardia. Stimulants can induce or exacerbate psychiatric symptoms and should be used with caution in patients with a history of mania, psychosis, or substance abuse. Stimulant use has also been associated with new or worsening tics or worsening Tourette's syndrome. Close monitoring for the emergence or worsening of psychiatric symptoms, tics, or Tourette's syndrome is recommended. Stimulants have also been associated with sudden death in patients with structural cardiac abnormalities or other serious cardiac disease when used at recommended ADHD doses; patients with structural heart defects, cardiomyopathy, coronary artery disease, serious cardiac arrhythmias, or other serious cardiac disease may be at risk for adverse cardiac events. The American Academy of Pediatrics and the American Heart Association recommend careful screening of all children and adolescents prior to initiating pharmacologic therapy for ADHD, including a detailed patient and family history and physical examination; any significant findings should be further assessed and referred for consultation with a pediatric cardiologist prior to initiating treatment.[29332][31563][34206][46924][69646]
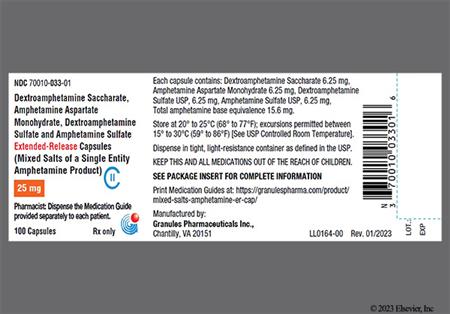
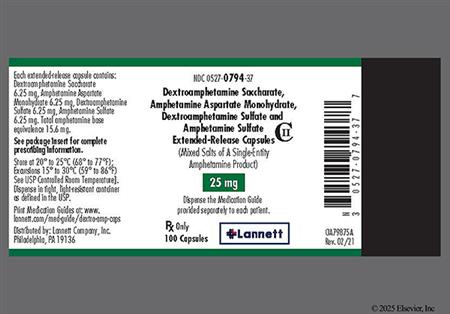
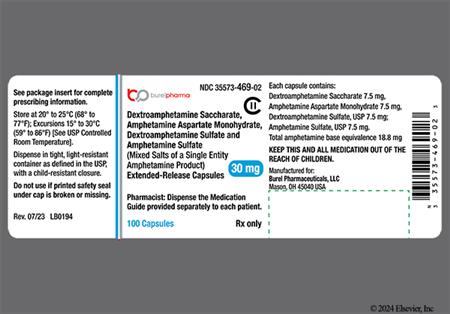
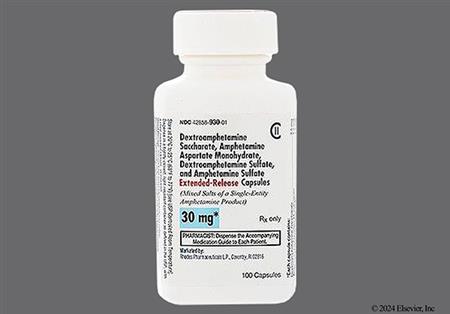
For storage information, see the specific product information within the How Supplied section.
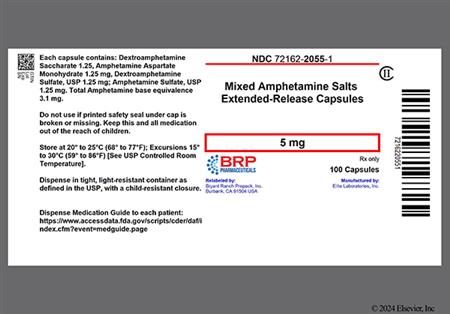
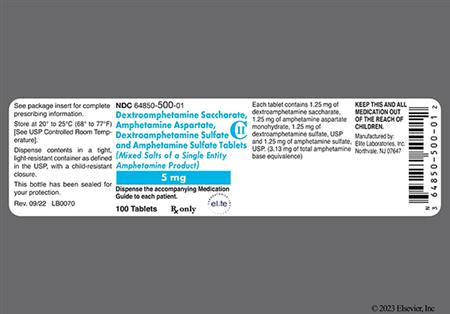
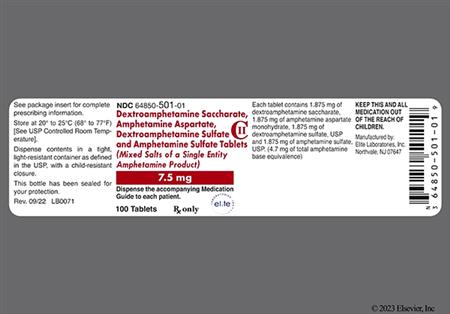
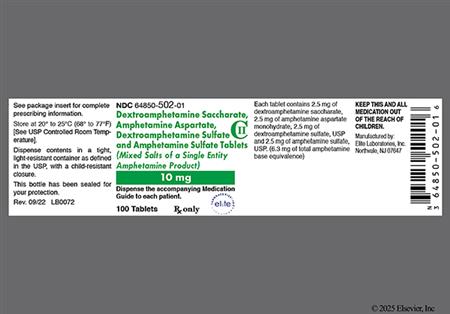
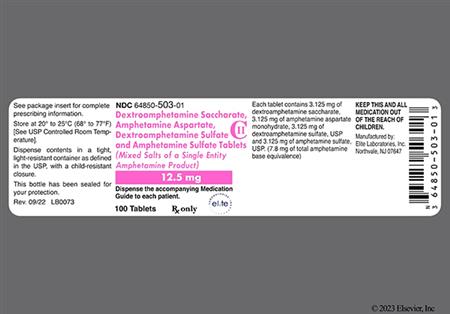
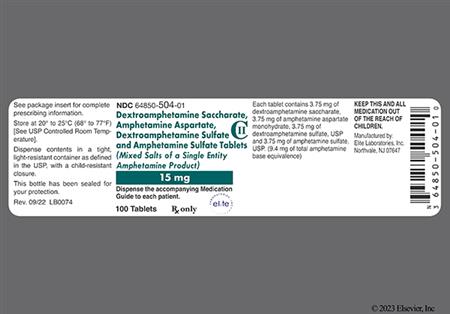
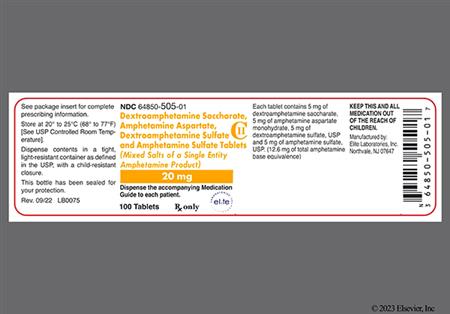
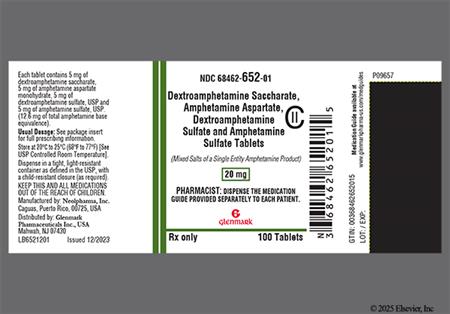
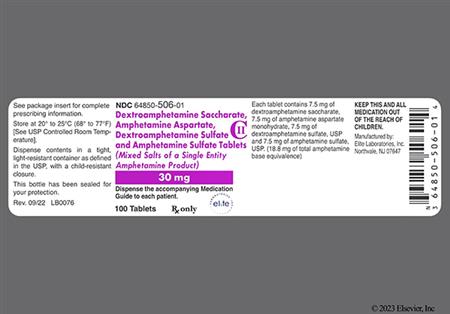
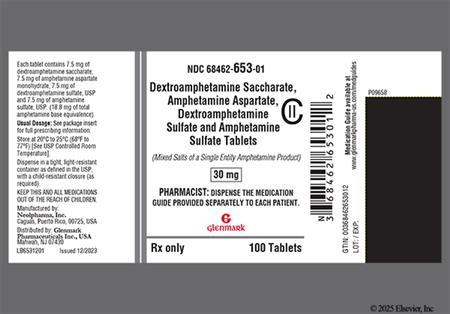
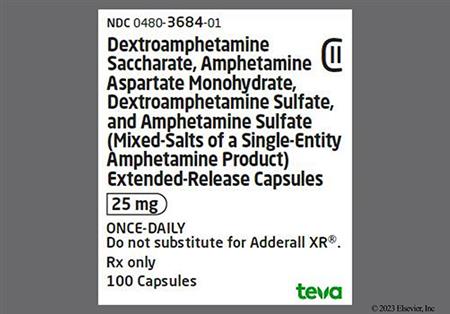
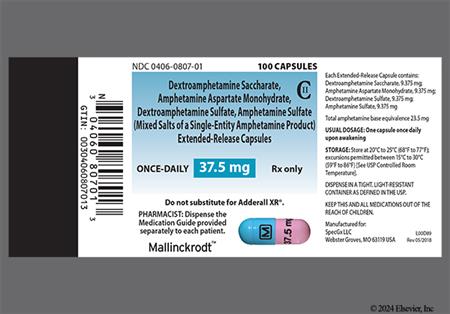
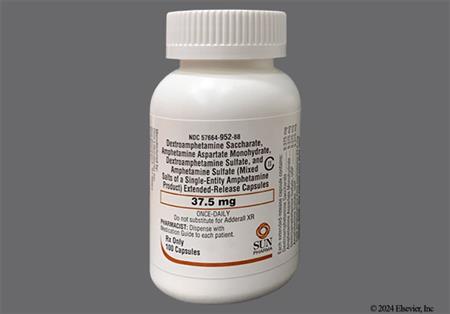
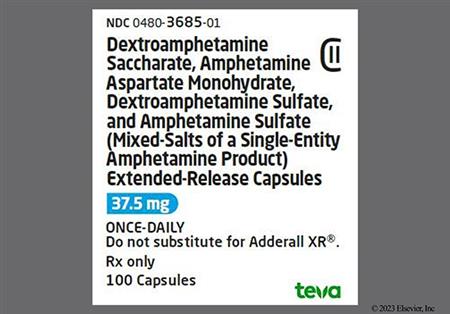
Immediate-release tablets:
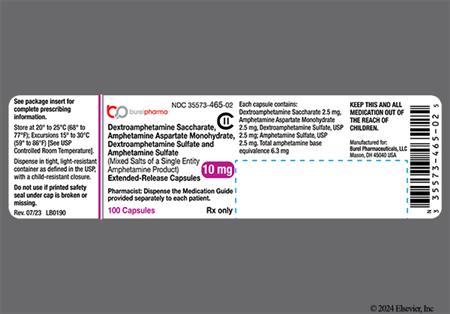
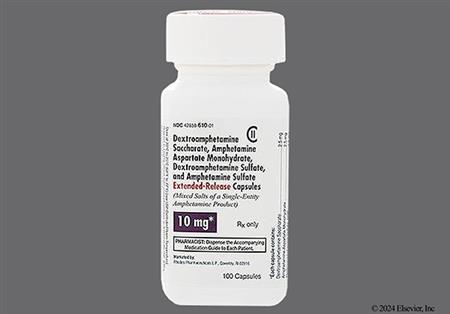
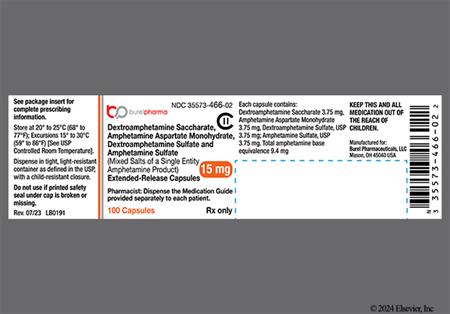
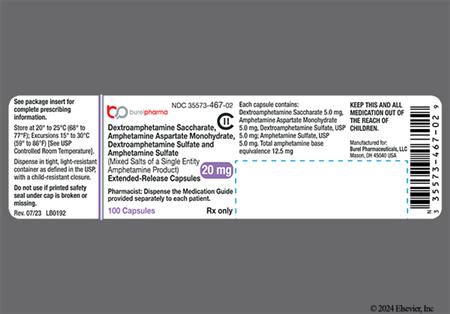
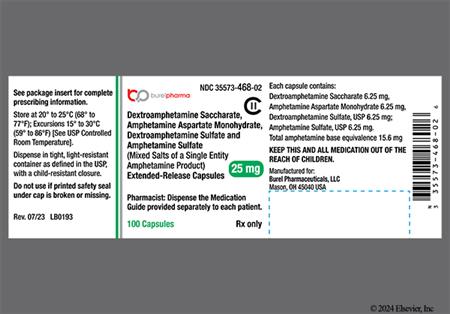
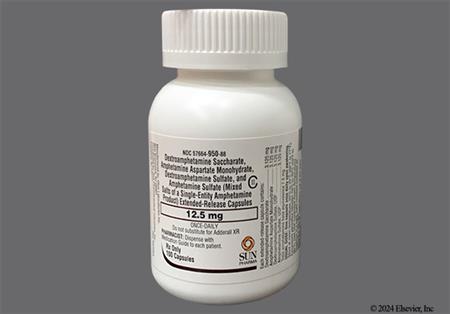
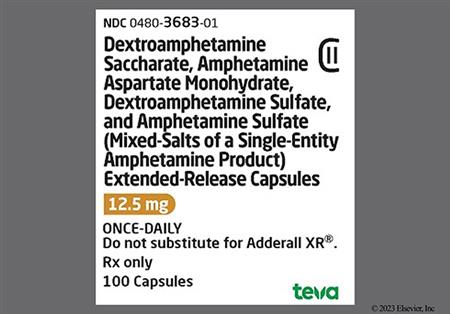
Extended-release capsules (Adderall XR):
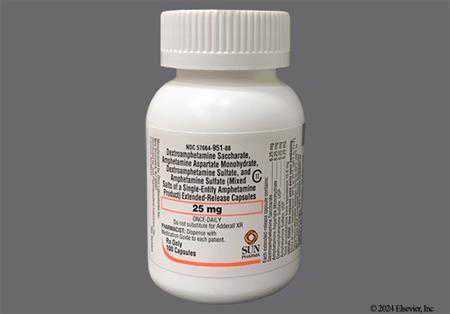
Extended-release capsules (Mydayis):
Insomnia is one of the most common centrally-mediated effects of amphetamines. Insomnia will typically resolve within a few days of amphetamine use provided the dosage is appropriate and doses are not administered within 6 hours of bedtime. Avoidance of exercising late in the day, limiting caffeinated beverages, and setting regular bedtime schedules may limit sleep disruption. Continued interrupted sleep patterns may indicate a need for dosage reduction. During clinical trial evaluations of extended-release amphetamine; dextroamphetamine, the following CNS effects were reported in adults and/or pediatric patients: headache (26% of adults), insomnia (27% to 31% of adults, 8% to 12% of adolescents, 17% of children), dizziness (7% of adults, 4% of adolescents, 2% of children), feeling jittery (2% of adults), asthenia (6% of adults, 2% of children), somnolence/drowsiness (2% to 4% of adults), speech disorder (e.g., stuttering or dysphemia, excessive speech, logorrhea) (2% to 4% of adults), twitching (2% to 4% of adults), and accidental injury (3% of children). Other CNS effects that have been associated with the use of amphetamines include overstimulation, dysphoria, tremor, euphoria, restlessness, and paresthesias (including formication). Children who become overly preoccupied with a task (over-focused or inflexible) or are described as 'zombie-like' are considered to exhibit supranormalization; these behaviors typically require dosage reduction. Once-daily morning dosing of amphetamine; dextroamphetamine is effective in many children and may also help to limit intolerable adverse reactions.[29332] [31563] [62038]
Dyskinesia has been reported during postmarketing use of CNS stimulants, including amphetamine; dextroamphetamine products. The onset or exacerbation of motor and verbal tics has also been reported. Individuals should be monitored for the emergence or worsening of dyskinesias, tics, or Tourette syndrome; consider dose reduction or discontinuation of treatment if clinically indicated.[29332] [31563]
Anorexia (reported as loss or decrease of appetite) and other appetite changes is one of the most common gastrointestinal (GI) adverse reactions associated with stimulant use. Weight loss is a dose-related adverse effect commonly associated with stimulant use and is of particular concern in growing children and adolescents. In a controlled trial of extended-release amphetamine; dextroamphetamine in adolescents, the mean change in weight during the first 4 weeks of therapy was -1.1 lbs and -2.8 lbs, respectively for patients who received 10 mg and 20 mg daily.[29332] [31563] [62038] An FDA analysis reported children younger than 6 years receiving extended-release stimulants have higher medication exposure and significant weight loss (at least 10% decrease) compared to older children on the same dose. Due to these findings, the benefits may not outweigh the risks in this age group.[72428] During clinical trial evaluations of extended-release amphetamine; dextroamphetamine, the following GI effects were reported in adults and/or pediatric patients: loss of appetite (30% to 33% of adults, 22% to 36% of adolescents, 22% of children), weight loss (9% to 10% of adults, 5% to 9% of adolescents, 4% of children), vomiting (7% of children), nausea (8% of adults, 8% of adolescents, 5% of children), diarrhea (3% to 6% of adults), teeth grinding (bruxism) (2% of adults), dyspepsia (2% of children), xerostomia (23% to 35% of adults), constipation (2% to 4% of adults), and abdominal pain (4% to 11% of adolescents, 14% of children). Bowel ischemia has been reported during postmarketing use. Dysgeusia has been associated with the use of amphetamines although the frequency has not been determined.[29332] [31563] [62038] Complaints of xerostomia or dysgeusia may be limited by sucking sugarless hard candy, crushed ice, and drinking plenty of water or other fluids. Eating small, frequent meals or snacks may help limit gastrointestinal effects.
Growth inhibition is a possible long-term side effect of the use of stimulants in children and adolescents; proposed mechanisms have included the suppression of appetite or an alteration in growth hormone secretion. Some have suggested that the use of drug holidays will allow growth to 'catch-up'. However, drug holidays are typically reserved for children with well-controlled ADHD symptoms, and drug holidays are of unproved value in limiting growth suppression. Growth rebound has been observed after the discontinuation of the stimulants in children and clinical studies do not indicate that amphetamines compromise the attainment of normal adult height and weight. However, practitioners should monitor for this side effect by monitoring height and weight parameters relative to age at the initiation of treatment and periodically during therapy (at minimum yearly). Patients who are not growing or gaining weight as expected may need to have their treatment interrupted.[45900] In a 24-month follow-up, the Multimodal Treatment Study showed a deceleration of growth of roughly 1 cm per year with stimulant use. In general, growth remained in the normal curve for most children, except those in the lowest percentiles of height for age.[31578] [31592] Data obtained on the effects of stimulants on growth suppression in children 7 to 10 years suggested that regularly medicated children (7 days/week) had a temporary average slowing in growth of 2 cm in height and 2.7 kg in weight over 3 years; it is anticipated that chronic amphetamine use may cause similar suppression.[31563]
Like other stimulant medications, amphetamine; dextroamphetamine is associated with cardiovascular adverse effects ranging in severity from mild to fatal. In normal therapeutic doses, amphetamines may induce increases in both systolic and diastolic blood pressure and exacerbate hypertension. In a single dose pharmacokinetic study of adolescents with ADHD (n = 23), increases in systolic blood pressure above the upper 95% CI for age, gender, and stature occurred in 12% of patients given 10 mg of extended-release amphetamine;dextroamphetamine (Adderall XR) and 35% of patients given 20 mg. Maximal increases occurred 2 to 4 hours after dosing, were transient, and were not associated with symptoms. In a second study of adolescents with ADHD treated over a 4-week period, systolic blood pressure increases (15 mmHg or more) occurred in 7% of patients receiving Adderall XR (n = 100) and 11% of patients receiving placebo (n = 64). Diastolic blood pressure increases (8 mmHg or more) occurred in 22% of patients receiving Adderall XR and 25% of patients receiving placebo. In general, stimulant medications cause an average increase in blood pressure of about 2 to 4 mmHg.[29332] A reflex sinus bradycardia, which is not usually clinically significant, may occur. In general, stimulant medications increase heart rate by an average of 3 to 6 bpm, but some patients may experience significantly higher increases. During clinical trial evaluations of extended-release amphetamine; dextroamphetamine in adults, the following cardiac effects were reported more frequently in patients receiving extended-release amphetamine; dextroamphetamine than placebo: tachycardia (6%), increased heart rate (9%), dyspnea (2% to 4%), and palpitations (2% to 4%). Other cardiovascular-related events that have been reported with the use of amphetamines include sudden death, myocardial infarction, stroke (unspecified), and isolated cases of cardiomyopathy with chronic administration. Sudden cardiac death has also been reported in association with CNS stimulant treatment at usual doses in children, adolescents, and adults with structural cardiac abnormalities and other serious heart conditions. Although some structural cardiac abnormalities alone may carry an increased risk of sudden death, stimulant products generally should not be used in children, adolescents, or adults with known structural cardiac abnormalities or other serious heart conditions. All patients should be advised of the risk of serious cardiovascular events (e.g., arrhythmia or arrhythmia exacerbation, tachycardia, hypertension, hypotension) with stimulant use. Patients who develop symptoms such as exertional chest pain (unspecified), unexplained syncope, or other symptoms suggestive of cardiac disease during amphetamine; dextroamphetamine treatment should undergo a prompt cardiac evaluation.[29332] [31563]
During clinical trial evaluations of extended-release amphetamine; dextroamphetamine in adults, the following genitourinary effects were reported more frequently in patients receiving extended-release amphetamine; dextroamphetamine than placebo: dysmenorrhea (2% to 4%), libido decrease (2% to 4%), and impotence (erectile dysfunction) (2% to 4%). Frequent or prolonged erections have occurred during administration of amphetamine derivatives. Similar reactions, including priapism, have been reported during use of other ADHD medications such as methylphenidate and atomoxetine.[51955] [28405] Reported cases of priapism have occurred after a period of time on stimulant therapy and often subsequent to a dose increase. Priapism has also been reported during periods of drug withdrawal (e.g., drug holidays or discontinuation). Prolonged erections in male patients should be promptly reported, as immediate diagnosis and treatment are essential to avoid tissue damage. Amphetamines have been reported to occasionally cause libido increase.[29332] [31563] [62038]
Stimulant medications have the potential to lower the seizure threshold in patients with a prior history of seizures, in patients with a history of EEG abnormalities without a history of seizures, and rarely in patients without a seizure history or EEG abnormalities. Stimulant medications should be discontinued if seizures develop. Seizures are also associated with amphetamine; dextroamphetamine toxicity; carefully evaluate the patient for other signs and symptoms of overdose if seizures occur.[29332]
Dermatologic and allergic reactions to amphetamines are rare, however serious events such as angioedema, anaphylactoid reactions, Stevens-Johnson syndrome, and toxic epidermal necrolysis have all been reported with the use of amphetamine or amphetamine derivatives. During clinical trial evaluation of extended-release amphetamine; dextroamphetamine in adults, hyperhidrosis and photosensitivity reaction occurred in 2% to 4% of patients receiving extended-release amphetamine; dextroamphetamine and at a greater frequency than placebo. Urticaria, rash (unspecified), and alopecia have also been reported during the administration of amphetamines.[29332] [31563] [62038]
Visual impairment, including blurred vision, difficulties with visual accommodation, and mydriasis, has been reported during postmarketing use of amphetamines. Patients are encouraged to report any unusual changes in vision promptly for examination and evaluation.[29332] [31563] [62038]
Stimulants used to treat ADHD, including amphetamine; dextroamphetamine, are associated with peripheral vasculopathy. Effects of peripheral vasoconstriction, including Raynaud's phenomenon, were observed in postmarketing reports at therapeutic doses in all age groups throughout the course of treatment. Signs and symptoms are usually intermittent and mild and generally improve after reduction in dose or discontinuation of drug. However, very rare sequelae include digital skin ulcer and/or soft tissue breakdown. Carefully monitor for digital changes during treatment with ADHD stimulants. Further clinical evaluation (e.g., rheumatology referral) may be appropriate for certain patients.[29332] [31563]
Stimulant medications, such as amphetamine; dextroamphetamine, can cause psychotic or manic symptoms (i.e., hallucinations, delusional thinking, or mania) in patients without a prior history of psychosis or mania, and have occurred during use of recommended doses and with toxicity or abuse. These symptoms occurred in approximately 0.1% of patients treated with stimulants (methylphenidate or amphetamine at usual doses) compared to 0% in placebo-treated patients in a pooled analysis of short-term, placebo-controlled studies.[29332] [56750] [56766] In a cohort study assessing 221,846 adolescents and young adults who received a prescription for a stimulant for ADHD, new-onset psychosis occurred in approximately 1 in 660 patients. The percentage of patients who had a psychotic episode was 0.1% in patients receiving methylphenidate compared to 0.21% in patients receiving amphetamine (hazard ratio with amphetamine use, 1.65; 95% CI 1.31 to 2.09). The median time from when the stimulant was dispensed to the psychotic episode was 128 days.[64025] Aggression, hostility, and suicidal ideation or behaviors have also been reported during the use of medications for ADHD.[28405] [29332] [56750] [56766] Although causality to the drugs has not been established and these behaviors are often observed in children and adolescents with ADHD, close monitoring is recommended. If suicide-related events emerge during treatment, consideration should be given to dose reduction or drug discontinuation, especially if symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.[56765] During clinical trial evaluation of extended-release amphetamine; dextroamphetamine, the following psychiatric effects occurred in adults and/or pediatric patients: anxiety (7% to 8% of adults), nervousness (13% of adults, 6% of adolescents, 6% of children), irritability (6% of adolescents), emotional lability (2% to 4% of adults, 9% of children), depression (3% of adults), and agitation (2% to 8% of adults). Other psychiatric effects that have been associated with the use of amphetamine; dextroamphetamine include anger and dermatillomania. Patients and their caregivers should be advised to promptly report any changes in mood or behavior. Discontinuation of the drug may be required if psychiatric symptoms are persistent or severe. Abrupt discontinuation of amphetamines after chronic administration may unmask severe depression, suicidal ideation, anxiety, agoraphobia, dysphoria, psychomotor agitation, or symptoms of overactive behaviors.[62038] [29332] [31563]
Toxic effects of amphetamines are more variable in children than in adults and appear to occur over a wide dosage range. Signs of excessive dosages or acute overdose may include: anxiety, headache, euphoria, hyperactivity, agitation, confusion, delirium, paranoia, hallucinations, tremor, paresthesias, palpitations, sinus tachycardia, hypertension, chest pain (unspecified), nausea, vomiting, diaphoresis, mydriasis, dyspnea, tachypnea, hyperthermia, and hyperreflexia. Minor manifestations of any of these symptoms during prescription use indicate a need for dosage reduction or discontinuation. Severe manifestations of amphetamine overdose include cardiac arrhythmias, refractory hypotension, myocardial infarction, circulatory collapse, ischemic stroke, rhabdomyolysis, seizures, acute renal failure (unspecified), fulminant hyperthermia, coma, and death. Symptoms of chronic intoxication with amphetamines include severe dermatoses, marked insomnia, irritability, hyperactivity, and psychosis indistinguishable from schizophrenia. Some severe manifestations of toxicity may also occur during therapeutic use of amphetamines, such as rhabdomyolysis, seizures, cardiac arrhythmias, and psychosis; however, they are most often associated with sympathomimetic toxicity. The product labeling for amphetamines includes a boxed warning stating that misuse of amphetamines may cause sudden death or serious cardiovascular adverse events.[28488] [29332] [31563] [31971] [31972] [59447] [61065] [62090]
Amphetamines stimulate the release of serotonin (5-HT) and may act as direct agonists on central serotonin receptors. Thus, amphetamines are both direct and indirect stimulants of serotonin activity. Serotonin syndrome may occur when amphetamines are combined with other medications (e.g., SSRIs) that enhance serotonin activity within the CNS or following overdose. Serotonin syndrome is characterized by the rapid development of hyperthermia, hypertension, myoclonus, rigidity, autonomic instability, mental status changes (e.g., agitation, delirium, hallucinations, coma), and in rare cases, death. The use of amphetamines with potent CYP2D6 inhibitors, such as paroxetine or fluoxetine, may also increase the risk through inhibition of amphetamine metabolism and an increase in systemic exposure. If serotonin syndrome becomes evident during treatment, the amphetamine and any other serotonergic agents should be discontinued and appropriate medical treatment should be initiated.[62038]
Psychological dependence, physiological dependence, and tolerance may occur with amphetamine; dextroamphetamine therapy. Abrupt discontinuation or a significant dose reduction of CNS stimulants after prolonged use may produce withdrawal symptoms that include dysphoria, depression, fatigue, vivid and unpleasant dreams, insomnia or hypersomnia, increased appetite, and psychomotor retardation or agitation. Signs and symptoms of chronic amphetamine abuse include severe dermatoses, marked insomnia, irritability, hyperactivity, personality changes, and psychosis with features indiscriminate from schizophrenia.[29332] [31563]
Patients receiving extended-release amphetamine; dextroamphetamine salts in clinical trials experienced fever (5% of children), infection (3% of children), viral infection (1% of adolescent patients) and urinary tract infection (5% of adults). Other infections occurring in 2% to 4% of adults receiving extended-release amphetamine; dextroamphetamine and at a greater frequency than placebo included tooth infection (dental caries).[29332] [62038]
Amphetamines can cause a significant elevation in plasma corticosteroid levels; this increase is greatest in the evening. Amphetamines may cause laboratory test interference with urinary steroid determinations. These effects may need to be considered during testing.[29332]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Central nervous system (CNS) stimulants, such as amphetamine; dextroamphetamine mixed salts, have a high potential for abuse and misuse, which can lead to the development of a substance abuse disorder, including addiction. Assess each individual's risk for substance abuse (including alcoholism), misuse, or addiction before prescribing a CNS stimulant, and monitor for the development of these behaviors or conditions throughout treatment.[29332] [31563] [68987] Children and adolescents with attention-deficit hyperactivity disorder (ADHD) are more prone to substance abuse compared to those without ADHD, and those with co-occurring mental health conditions (e.g., depression, disruptive behavior disorders) are at even greater risk; however, appropriate treatment of ADHD with medication and behavior therapy may reduce the risk of developing a substance abuse disorder.[57647] Prescribing and dispensing the smallest appropriate quantity may help to minimize abuse, misuse, and overdosage.[31563] CNS stimulants can be diverted for non-medical use into illicit channels or distribution. The most common source of non-medical use is sharing from family or friends with misuse of the individual's own prescription or obtaining from illicit channels occurring less frequently. Sharing of CNS stimulant medications can lead to substance abuse disorder and addiction in those they are shared with. Misuse and abuse of CNS stimulants can result in potential for overdose or poisoning and death; the risk is increased with higher doses or unapproved methods of administration, such as snorting or injection.[68987] Educate individuals and their families about these risks, proper storage, and proper disposal of any unused medication. Misuse or abuse may cause increased heart rate, respiratory rate, or blood pressure; sweating; dilated pupils; hyperactivity; restlessness; insomnia; decreased appetite; loss of coordination; tremors; flushed skin; vomiting; and/or abdominal pain. Anxiety, psychosis, hostility, aggression, and suicidal or homicidal ideation have also been observed with stimulant abuse or misuse.[29332] [31563] [68987]
CNS stimulants should be used with caution in those with bipolar disorder or a pre-existing psychotic disorder (e.g., schizophrenia). CNS stimulants may exacerbate symptoms of behavior disturbance and thought disorder in individuals with pre-existing psychosis. These medications can also induce mania or a mixed episode in individuals with bipolar disorder. Prior to initiating treatment with amphetamine; dextroamphetamine, screen individuals for risk factors for bipolar disorder or developing an episode of mania (e.g., mood disorder, comorbid or history of depressive symptoms or a family history of suicide, bipolar disorder, or depression). At recommended doses, CNS stimulants may also cause psychotic or manic symptoms (such as hallucinations, delusions, or mania) in individuals without a prior history of psychosis or mania. Advise individuals and their caregivers to promptly report suicidal ideation or any changes in mood or behavior and consider discontinuing treatment if these symptoms occur.[31563] [29332] [56750] [56766]
Sudden death has been reported in individuals with structural cardiac abnormalities or other serious cardiac disease who were treated with CNS stimulants at the recommended ADHD dosages. Avoid use of CNS stimulants in individuals with known structural cardiac abnormalities, cardiomyopathy, serious cardiac arrhythmias, coronary artery disease, or other serious cardiac disease. Prior to initiating any CNS stimulant, carefully assess patient for the presence of cardiac disease (i.e., perform a careful patient history, assess for any family history of sudden cardiac death or ventricular arrhythmia, and complete a physical exam) and counsel individuals to report symptoms of cardiac disease (i.e., exertional chest pain, unexplained syncope) immediately.[34206] [46635] [46636] [31563] [29332] [62038] Although it is reasonable for a health care provider to obtain an ECG as part of the cardiovascular evaluation, it is not mandatory. Treatment with stimulant products should not be withheld because an ECG is not performed.[69646] However, any individual with significant findings on physical examination, ECG, or from patient or family history (such as known congenital heart disease, structural heart disease, arrhythmias, or a family history of sudden cardiac death in members younger than 35 years of age) should be referred for consultation with a pediatric cardiologist prior to starting the stimulant medication. Overall, studies have not shown an association between the use of ADHD medications and adverse cardiovascular events; however, long-term cardiovascular risks associated with ADHD medications are unknown.[69645] [34206] [46635] [46636] CNS stimulant medications, including amphetamine; dextroamphetamine, can cause an increase in blood pressure (mean increase approximately 2 to 4 mmHg) and heart rate (mean increase approximately 3 to 6 beats per minute). Some individuals may have larger increases. Monitor all individuals receiving amphetamine; dextroamphetamine for hypertension and tachycardia.[31563] [63187] Careful monitoring should be performed after initiation of stimulant medications; if any abnormal findings or arrhythmias are diagnosed during treatment, consider discontinuation of the stimulant.[34206]
Extended-release amphetamine; dextroamphetamine is not recommended for use in children younger than 6 years due to higher medication exposure and increased adverse reactions. An FDA analysis reported children younger than 6 years receiving extended-release stimulants have higher adverse reaction rates, particularly significant weight loss, compared to older children on the same dose. For children younger than 6 years who experience weight loss or other adverse reactions while receiving extended-release stimulants, consider discontinuing the medication or switching to an alternative, such as an immediate-release stimulant. Monitor growth and development and provide necessary interventions to minimize weight loss.[29332] [72428]
CNS stimulants, including amphetamine; dextroamphetamine products, have been associated with the onset or exacerbation of motor and verbal tics. Worsening of Tourette syndrome has also been reported. Prior to initiating amphetamine; dextroamphetamine, carefully assess family history and clinically evaluate individuals for motor or verbal tics or Tourette syndrome. Regularly monitor amphetamine; dextroamphetamine-treated individuals for the emergence or worsening of tics or Tourette syndrome and discontinue treatment if clinically appropriate.[29332] [31563] [62038]
Geriatric adults or debilitated individuals may be more susceptible to the CNS and sympathomimetic side effects of the amphetamines; use with caution in the older adult. Medication should be titrated with low doses initially and with a slow increase.[29332] [31563]
Use amphetamine; dextroamphetamine with caution in individuals with renal impairment or renal failure. Amphetamine; dextroamphetamine extended-release product dosages should be reduced in individuals with an eGFR less than 30 mL/minute/1.73 m2, and use of these dosage forms in individuals with renal failure (end-stage renal disease) is not recommended.[29332] [62038]
Available data on the use of prescription amphetamines during human pregnancy have not identified a drug-associated risk of major birth defects and miscarriage. Infants born to individuals taking amphetamines during pregnancy have an increased risk of premature delivery and low birth weight. Amphetamines cause vasoconstriction and may decrease placental perfusion. In addition, amphetamines can stimulate uterine contractions, increasing the risk of premature delivery.[31563] [62038] [63187] Much of the historical data on amphetamine use during pregnancy is derived from studies of illicit use, which may be complicated by comorbid substance abuse or ingestion of higher-than-prescribed doses.[65048] [69068] These studies report increased incidence of premature birth, low birth weight and length, lower occipitofrontal circumference, and neonatal withdrawal symptoms (e.g., abnormal sleep patterns, poor feeding, tremor, agitation, fatigue, hypertonia).[48417] [65048] [69068] However, more recent data demonstrate that risks associated with the use of prescription amphetamines may be lower than initially thought.[69111] Among 671 mother-child pairs enrolled in the Collaborative Perinatal Project who had first trimester exposure to amphetamines and 1,898 mother-child pairs with amphetamine exposures at any time during pregnancy, there was no evidence suggesting a relationship to large categories of major or minor malformations.[48419] Similarly, a large cohort study of pregnancy outcomes in the United States and 5 Nordic countries were compared to assess for the risks of major congenital malformations and cardiac effects in infants exposed to stimulants in utero. Of the 5,571 pregnant people who filled a prescription for amphetamines during the first trimester, 253 (4.54%) were diagnosed with malformations. In infants who were not exposed, 62,966 (3.5%) of the nearly 1.8 million infants developed malformations. After adjusting for underlying psychiatric disorders and other potential confounders, no increased risks were observed for amphetamine use compared to controls.[69191] Animal studies identify long-term neurochemical and behavioral effects in offspring at clinically relevant amphetamine doses.[31563] [62038] [63187] A large cohort study evaluated stimulant use in the second half of pregnancy in 4,693 amphetamine/dextroamphetamine and 786 methylphenidate-exposed pregnancies compared to 2,496,711 unexposed pregnancies. This study found exposure to these medications in utero did not increase the risk of childhood neurodevelopmental disorders after adjustment for confounders, such as demographic characteristics and maternal ADHD or mental health diagnoses.[72097] There is a pregnancy exposure registry that monitors outcomes in pregnant people exposed to ADHD medications. Care teams are encouraged to register patients at https://womensmentalhealth.org/research/pregnancyregistry/adhd-medications/ or by calling 1-866-961-2388.
Stimulant medications are associated with peripheral vasoconstriction or ischemia, including Raynaud phenomenon. Worsening of peripheral vascular disease is possible. Effects on circulation have been observed with therapeutic doses at different times throughout therapy in all age groups. Signs and symptoms are usually intermittent and mild and generally improve after reduction in dose or discontinuation of the drug. However, very rare sequelae include digital skin ulcer and/or soft tissue breakdown. Carefully monitor all individuals for digital changes during treatment with stimulant medications, especially those with pre-existing circulation problems. Instruct individuals to seek immediate medical attention if any new digital numbness, pain, skin discoloration, or temperature sensitivity occur, or if unexplained wounds appear on their fingers or toes. Further clinical evaluation (e.g., rheumatology referral) may be appropriate for individuals taking stimulants who develop signs or symptoms of peripheral vasculopathy.[29332] [31563]
Neonates and infants exposed to this medication in utero are at risk for withdrawal symptoms after delivery. Monitor neonates and infants for symptoms of withdrawal such as feeding difficulties, irritability, agitation, and excessive drowsiness.[31563] [62038] [63187]
Use amphetamine; dextroamphetamine with caution during breast-feeding. FDA-approved product labeling does not recommend breast-feeding in individuals taking amphetamines.[31563] [62038] [63187] However, some experts state that therapeutic dosages can be used during lactation with close monitoring of the child for irritability, insomnia, and poor feeding. Limited data suggest that at typical doses prescribed for medical indications, amphetamines do not cause infant adverse effects. However, the long-term neurodevelopmental effects on infants are unknown.[70364] Dextroamphetamine is present in human milk in small amounts. Limited data indicate a relative infant dose of 2.46% to 7.25% of the maternal weight-adjusted dosage, with a milk to plasma ratio between 2 and 5.2.[70365] Large dosages of amphetamines may interfere with milk production, especially in people without well established lactation.[70364] Methylphenidate, dexmethylphenidate, and serdexmethylphenidate/methylphenidate are alternative options for treatment of ADHD in the breast-feeding individual, as limited data indicates that methylphenidate levels in milk are very low and not detectable in infant serum.[69068]
Amphetamines are non-catecholamine sympathomimetic amines with CNS stimulant activity. Amphetamine and dextroamphetamine stimulate the release of norepinephrine (NE) and other biologic amines from central adrenergic receptors. At higher dosages, they cause release of dopamine (DA) from the mesocorticolimbic system and the nigrostriatal dopamine systems. It is thought that the release of dopamine is responsible for the reinforcing properties of amphetamine. At still higher doses, amphetamine stimulates the release of 5-hydroxytryptamine (5-HT). Finally, amphetamine may act as a direct agonist on central 5-HT receptors. Thus, amphetamine is both a direct and an indirect stimulant. Amphetamines may also inhibit monoamine oxidase (MAO), but this is a minor action. Dextroamphetamine exhibits greater CNS stimulation than racemic- or levo- amphetamine on a weight basis. Amphetamine-induced CNS stimulation produces a decreased sense of fatigue, an increase in motor activity and mental alertness, mild euphoria, and brighter spirits. Lithium may offset amphetamine-induced euphoria.[30000][29332][31563]
Actions in ADHD: The mode of therapeutic action in Attention Deficit Hyperactivity Disorder (ADHD) is not known.[29332][31563] Improved attention spans, decreased distractibility, increased ability to follow directions or complete tasks, and decreased impulsivity and aggression have been noted when stimulants are prescribed for the treatment of ADHD.[54935][61234][63180]
Peripheral actions: In the periphery, the actions of amphetamines are believed to occur through release of norepinephrine from the adrenergic nerve terminals and by a direct stimulant action on alpha- and beta-receptors. Dextroamphetamine has less peripheral activity than racemic amphetamine at normally prescribed dosages. Amphetamines increase systolic and diastolic blood pressure and cause respiratory stimulation and weak bronchodilation. Heart rate typically increases slightly with normal therapeutic doses of stimulants (about 3 to 6 bpm); however, a reflexive decrease in heart rate in response to increased blood pressure can also occur. At high doses, such as in overdoses, amphetamine and its derivatives can cause significant hypertension, tachycardia, arrhythmias, and other serious complications. Amphetamines may produce mydriasis and contraction of the bladder sphincter.[30000][46053][55038][29332][31563]
Revision Date: 10/03/2025, 02:08:56 PMAmphetamine and dextroamphetamine mixed salts are administered orally. Commercially available products contain d-amphetamine and l-amphetamine salts in the ratio of 3:1. Amphetamine; dextroamphetamine is widely distributed throughout the body, including the central nervous system (CNS). Volume of distribution (Vd) increases as body weight increases. Amphetamine is reported to be oxidized at the 4 position of the benzene ring to form 4-hydroxyamphetamine, or on the side chain alpha- or beta- carbons to form alpha-hydroxy-amphetamine or norephedrine, respectively. Norephedrine and 4-hydroxy-amphetamine are both active and each is subsequently oxidized to form 4-hydroxy-norephedrine. Alpha-hydroxy-amphetamine undergoes deamination to form phenylacetone, which ultimately forms benzoic acid and its glucuronide and the glycine conjugate hippuric acid. The specific enzymes involved in amphetamine metabolism have not been described; however, the formation of 4-hydroxy-amphetamine is known to involve CYP2D6. Since CYP2D6 is genetically polymorphic, variations in amphetamine metabolism are a possibility. Children exhibit a higher clearance than adolescents and adults when adjusted for body weight. Under normal conditions, the plasma half-life of amphetamine; dextroamphetamine mixed salts (Adderall and Adderall XR) is roughly 9 to 11 hours in children 6 years and older, 11 to 14 hours in adolescents, and 10 to 13 hours in adults.[29332][31563] In both pediatric and adult patients receiving amphetamine; dextroamphetamine mixed salts (Mydayis), the mean plasma elimination half-life for d-amphetamine ranges from about 10 to 11 hours and l-amphetamine from 10 to 13 hours.[62038]
Amphetamines and their metabolites are excreted in the urine. With normal urine pH, approximately 30% to 40% of the administered dose is recoverable in urine as amphetamine and 50% as alpha-hydroxy-amphetamine (inactive metabolite). Since amphetamine has a pKa of 9.9, urinary recovery of amphetamine is highly dependent on pH and urine flow rates. Alkaline urine pHs result in less ionization and reduced renal elimination of amphetamine. Conversely, acidification of the urine and high urinary flow rates result in increased renal elimination with clearances greater than glomerular filtration rates, indicating the involvement of active secretion. Urinary recovery of amphetamine has been reported to range from 1% to 75% depending on urinary pH. The urinary elimination of amphetamines and their metabolites may be affected by agents that acidify or alkalinize the urinary fluids.[29332][31563][62038]
Possibly affected cytochrome P450 isoenzymes and drug transporters: CYP2D6
The specific enzymes involved in amphetamine metabolism have not been described; however, the formation of 4-hydroxy-amphetamine is known to involve CYP2D6. Because CYP2D6 is genetically polymorphic, variations in amphetamine metabolism are a possibility.[29332][62038] Amphetamines are not an in vitro inhibitor of CYP1A2, CYP2C9, CYP2C19, CYP2D6, or CYP3A, nor an in vitro inducer of CYP1A2, CYP2B6, or CYP3A4/5. Amphetamines are not an in vitro substrate for P-glycoprotein (P-gp).[62038]
Immediate-release tablets
After oral administration, peak plasma concentrations occur approximately 3 hours post-dose. The effect of food on the bioavailability of immediate-release tablets has not been studied.[31563]
Extended-release capsules (Adderall XR)
After oral administration, the maximum systemic absorption of extended-release capsules is completed within 7 hours compared to 3 hours for immediate-release tablets.[29332] In a pharmacokinetic study assessing 51 children with attention-deficit hyperactivity disorder (ADHD), after initial exposure to extended-release 20 mg capsules, mean maximum plasma concentration (Cmax) was 40.1 ng/mL for the d-isomer and 11.89 ng/mL for the l-isomer, consistent with the 3:1 ratio found in the parent compound. At steady state, mean Cmax reported was 47.22 ng/nL and 14.92 ng/nL for the d- and l-isomers, respectively.[51738] Area under the curve (AUC) and Cmax decreases with increases in body weight; children have a higher systemic exposure when compared to adults. However, based upon dose normalization on a mg/kg basis, children show approximately 30% less systemic exposure compared to their adult counterparts. Sprinkling extended-release capsules on applesauce gives comparable plasma concentrations to administration of the intact capsule in the fasted state. Otherwise, food does not affect the extent of absorption of amphetamine, but prolongs Tmax by approximately 2.5 hours. Pharmacokinetic parameters are linear over the normal dosage range.[29332]
Extended-release capsules (Mydayis)
After oral administration, peak plasma concentrations occurred in about 7 to 10 hours in adolescents (13 to 17 years) and about 8 hours in adults (19 to 51 years) for both d-amphetamine and l-amphetamine. Pharmacokinetic parameters are linear over the normal dosage range. Steady-state is achieved between days 7 and 8 of dosing with mean accumulation ratio of 1.6. Body weight is the primary determinant of apparent differences in pharmacokinetics across the age range. Based on dose proportionality, a single dose administered to adolescents would produce about 21% to 31% higher Cmax and AUC for d- and l-amphetamine, compared to the same dose administered to adults. Administration with a high-fat meal does not affect the extent of absorption, but prolongs the Tmax by 5 hours (7 hours at fasted state to 12 hours after a high-fat meal) for d-amphetamine and 4.5 hours (7.5 hours at fasted state to 12 hours after a high-fat meal) for l-amphetamine. Sprinkling on applesauce results in comparable absorption and exposure to the intact capsule taken in the fasted state. The presence of alcohol potentially increases release of amphetamine. At an alcohol concentration of 20% or 40%, in vitro testing showed increases in amphetamine release rate. There is no in vivo study for the effect of alcohol on drug exposure.[62038]
Hepatic dysfunction has the potential to inhibit the elimination of amphetamine and result in prolonged exposures.[29332][31563]
Renal dysfunction has the potential to inhibit the elimination of amphetamine and result in prolonged exposures. Dextroamphetamine is not dialyzable. Use in patients with end-stage renal disease is not recommended.[29332][31563][62038]
Extended-release capsules (Adderall XR)
Children and Adolescents 6 years and older
Children exhibit a higher clearance than adolescents and adults when adjusted for body weight. Under normal conditions, the plasma half-life of amphetamine; dextroamphetamine is roughly 9 to 11 hours in children 6 years and older, 11 to 14 hours in adolescents, and 10 to 13 hours in adults. However, children exhibit higher systemic exposure to amphetamine (based on Cmax and AUC) than adults for a given dose of extended-release amphetamine; dextroamphetamine; this difference is attributed to the higher dose administered to children on a mg/kg basis. Upon dose-normalization on a mg/kg basis, children showed 30% less systemic exposure when compared to adults.[29332]
Extended-release capsules (Mydayis)
Adolescents 13 years and older
Body weight is the primary determinant of apparent pharmacokinetic differences in adolescents (13 to 17 years old) compared to adult patients (19 to 62 years). Based on dose proportionality, a single dose administered to adolescents would produce about 21% to 31% higher Cmax and AUC for d- and l-amphetamine, compared to the same dose administered to adults.[62038]
Systemic exposure to amphetamines is 20% to 30% higher in females as compared to males, but differences diminish when females are given weight-based dosing comparable to male subjects. Gender had no direct effect on the pharmacokinetics of d-amphetamine or l-amphetamine.[29332]
Race does not appear to influence the pharmacokinetics of the amphetamines.[29332][62038]
Available data on the use of prescription amphetamines during human pregnancy have not identified a drug-associated risk of major birth defects and miscarriage. Infants born to individuals taking amphetamines during pregnancy have an increased risk of premature delivery and low birth weight. Amphetamines cause vasoconstriction and may decrease placental perfusion. In addition, amphetamines can stimulate uterine contractions, increasing the risk of premature delivery.[31563] [62038] [63187] Much of the historical data on amphetamine use during pregnancy is derived from studies of illicit use, which may be complicated by comorbid substance abuse or ingestion of higher-than-prescribed doses.[65048] [69068] These studies report increased incidence of premature birth, low birth weight and length, lower occipitofrontal circumference, and neonatal withdrawal symptoms (e.g., abnormal sleep patterns, poor feeding, tremor, agitation, fatigue, hypertonia).[48417] [65048] [69068] However, more recent data demonstrate that risks associated with the use of prescription amphetamines may be lower than initially thought.[69111] Among 671 mother-child pairs enrolled in the Collaborative Perinatal Project who had first trimester exposure to amphetamines and 1,898 mother-child pairs with amphetamine exposures at any time during pregnancy, there was no evidence suggesting a relationship to large categories of major or minor malformations.[48419] Similarly, a large cohort study of pregnancy outcomes in the United States and 5 Nordic countries were compared to assess for the risks of major congenital malformations and cardiac effects in infants exposed to stimulants in utero. Of the 5,571 pregnant people who filled a prescription for amphetamines during the first trimester, 253 (4.54%) were diagnosed with malformations. In infants who were not exposed, 62,966 (3.5%) of the nearly 1.8 million infants developed malformations. After adjusting for underlying psychiatric disorders and other potential confounders, no increased risks were observed for amphetamine use compared to controls.[69191] Animal studies identify long-term neurochemical and behavioral effects in offspring at clinically relevant amphetamine doses.[31563] [62038] [63187] A large cohort study evaluated stimulant use in the second half of pregnancy in 4,693 amphetamine/dextroamphetamine and 786 methylphenidate-exposed pregnancies compared to 2,496,711 unexposed pregnancies. This study found exposure to these medications in utero did not increase the risk of childhood neurodevelopmental disorders after adjustment for confounders, such as demographic characteristics and maternal ADHD or mental health diagnoses.[72097] There is a pregnancy exposure registry that monitors outcomes in pregnant people exposed to ADHD medications. Care teams are encouraged to register patients at https://womensmentalhealth.org/research/pregnancyregistry/adhd-medications/ or by calling 1-866-961-2388.
Use amphetamine; dextroamphetamine with caution during breast-feeding. FDA-approved product labeling does not recommend breast-feeding in individuals taking amphetamines.[31563] [62038] [63187] However, some experts state that therapeutic dosages can be used during lactation with close monitoring of the child for irritability, insomnia, and poor feeding. Limited data suggest that at typical doses prescribed for medical indications, amphetamines do not cause infant adverse effects. However, the long-term neurodevelopmental effects on infants are unknown.[70364] Dextroamphetamine is present in human milk in small amounts. Limited data indicate a relative infant dose of 2.46% to 7.25% of the maternal weight-adjusted dosage, with a milk to plasma ratio between 2 and 5.2.[70365] Large dosages of amphetamines may interfere with milk production, especially in people without well established lactation.[70364] Methylphenidate, dexmethylphenidate, and serdexmethylphenidate/methylphenidate are alternative options for treatment of ADHD in the breast-feeding individual, as limited data indicates that methylphenidate levels in milk are very low and not detectable in infant serum.[69068]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.