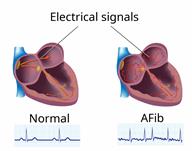
Atrial Fibrillation
Atrial fibrillation (AFib) is a type of irregular or rapid heartbeat (arrhythmia). In AFib, the top part of the heart (atria) beats in an irregular pattern. This makes the heart unable to pump blood normally and effectively.
The goal of treatment is to prevent blood clots from forming, control your heart rate, or restore your heartbeat to a normal rhythm. If this condition is not treated, it can cause serious problems, such as a weakened heart muscle (cardiomyopathy) or a stroke.
What are the causes?
This condition is often caused by medical conditions that damage the heart's electrical system. These include:
High blood pressure (hypertension). This is the most common cause.
Certain heart problems or conditions, such as heart failure, coronary artery disease, heart valve problems, or heart surgery.
Diabetes.
Overactive thyroid (hyperthyroidism).
Chronic kidney disease.
Certain lung conditions, such as emphysema, pneumonia, or COPD.
Obstructive sleep apnea.
In some cases, the cause of this condition is not known.
What increases the risk?
This condition is more likely to develop in:
Older adults.
Athletes who do endurance exercise.
People who have a family history of AFib.
Males.
People who are Caucasian.
People who are obese.
People who smoke or misuse alcohol.
What are the signs or symptoms?
Symptoms of this condition include:
Fast or irregular heartbeats (palpitations).
Discomfort or pain in your chest.
Shortness of breath.
Sudden light-headedness or weakness.
Tiring easily during exercise or activity.
Syncope (fainting).
Sweating.
In some cases, there are no symptoms.
How is this diagnosed?
Your health care provider may detect AFib when taking your pulse. If detected, this condition may be diagnosed with:
An electrocardiogram (ECG) to check electrical signals of the heart.
An ambulatory cardiac monitor to record your heart's activity for a few days.
A transthoracic echocardiogram (TTE) to create pictures of your heart.
A transesophageal echocardiogram (TEE) to create even clearer pictures of your heart.
A stress test to check your blood supply while you exercise.
Imaging tests, such as a CT scan or chest X-ray.
Blood tests.
How is this treated?
Treatment depends on underlying conditions and how you feel when you get AFib. This condition may be treated with:
Medicines to prevent blood clots or to treat heart rate or heart rhythm problems.
Electrical cardioversion to reset the heart's rhythm.
A pacemaker to correct abnormal heart rhythm.
Ablation to remove the heart tissue that sends abnormal signals.
Left atrial appendage closure to seal the area where blood clots can form.
In some cases, underlying conditions will be treated.
Follow these instructions at home:
Medicines
Lifestyle
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your provider.
-
Eat heart-healthy foods. Talk with a food expert (dietitian) to make an eating plan that is right for you.
-
Exercise regularly as told by your provider.
-
Do not drink alcohol.
-
Lose weight if you are overweight.
General instructions
-
If you have obstructive sleep apnea, manage your condition as told by your provider.
-
Do not use diet pills unless your provider approves. Diet pills can make heart problems worse.
-
Keep all follow-up visits. Your provider will want to check your heart rate and rhythm regularly.
Contact a health care provider if:
-
You notice a change in the rate, rhythm, or strength of your heartbeat.
-
You are taking a blood thinner and you notice more bruising.
-
You tire more easily when you exercise or do heavy work.
-
You have a sudden change in weight.

-
You have chest pain.
-
You have trouble breathing.
-
You have side effects of blood thinners, such as blood in your vomit, poop (stool), or pee (urine), or bleeding that does not stop.
- You have any symptoms of a stroke. "BE FAST" is an easy way to remember the main warning signs of a stroke:
B - Balance. Signs are dizziness, sudden trouble walking, or loss of balance.
E - Eyes. Signs are trouble seeing or a sudden change in vision.
F - Face. Signs are sudden weakness or numbness of the face, or the face or eyelid drooping on one side.
A - Arms. Signs are weakness or numbness in an arm. This happens suddenly and usually on one side of the body.
S - Speech.Signs are sudden trouble speaking, slurred speech, or trouble understanding what people say.
T - Time. Time to call emergency services. Write down what time symptoms started.
- Other signs of a stroke, such as:
These symptoms may be an emergency. Get help right away. Call 911.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.
 This condition is often caused by medical conditions that damage the heart's electrical system. These include:
This condition is often caused by medical conditions that damage the heart's electrical system. These include: