ThisiscontentfromElsevier'sDrugInformation
Budesonide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
INHALED DOSAGE RANGES BY PRODUCT
The ranges presented help define low, medium, and high ICS daily dosing according to asthma treatment recommendations.[69016][33558] The NAEPP 2020 focused updates state that ICS ranges from the NAEPP 2007 guidelines need to be updated in future NAEPP guidance.[66299]
Budesonide dry powder inhaler
Children 4 years and younger: Not available
Children 5 years:
Children 6 to 11 years:
Adults, Adolescents, and Children 12 years and older:
Budesonide nebulizer suspension
Infants:
Children 1 to 4 years:
Children 5 years:
Children 6 to 11 years:
Adults, Adolescents, and Children 12 years and older: Not available
360 mcg (2 actuations of 180 mcg/actuation) inhaled by mouth twice daily; 180 mcg (1 actuation of 180 mcg/actuation) twice daily may be appropriate for some patients. Max: 720 mcg (4 actuations of 180 mcg/actuation) twice daily. Titrate to the lowest effective dose once asthma stability is achieved.[34376]
180 mcg (1 actuation of 180 mcg/actuation or 2 actuations of 90 mcg/actuation) inhaled by mouth twice daily; 360 mcg (2 actuations of 180 mcg/actuation) twice daily may be appropriate for some patients. Max: 360 mcg (2 actuations of 180 mcg/actuation) twice daily. Titrate to the lowest effective dose once asthma stability is achieved.[34376]
1 to 2 mg inhaled by nebulizer twice daily, initially. Titrate to the lowest effective dose once asthma stability is achieved. Usual dose: 0.5 to 1 mg inhaled by nebulizer twice daily. Max: 4 mg/day.[65955]
1 to 2 mg inhaled by nebulizer twice daily, initially. Titrate to the lowest effective dose once asthma stability is achieved. Usual dose: 0.5 to 1 mg inhaled by nebulizer twice daily. Max: 4 mg/day.[65955]
0.5 to 1 mg inhaled by nebulizer twice daily, initially. Titrate to the lowest effective dose once asthma stability is achieved. Usual dose: 0.25 to 0.5 mg inhaled by nebulizer twice daily. Max: 2 mg/day.[65955]
0.25 to 1 mg inhaled by nebulizer once daily or 0.25 to 0.5 mg inhaled by nebulizer twice daily. Base starting dose on prior asthma therapy and disease severity. Max: 1 mg/day. If once-daily treatment does not provide adequate control, increase the daily dose and/or administer in divided doses twice daily. Titrate to the lowest effective dose once asthma stability is achieved.[33486] Short-term, high-dose nebulized budesonide can have an early clinical effect by day 2 of treatment.[26690]
0.5 to 1 mg inhaled by nebulizer twice daily, initially. Titrate to the lowest effective dose once asthma stability is achieved. Usual dose: 0.25 to 0.5 mg inhaled by nebulizer twice daily. Max: 2 mg/day.[65955] Limited data from small safety studies used 0.25 to 1 mg/day via nebulizer once daily or in 2 divided doses.[33594] [33595]
180 to 360 mcg (1 to 2 actuations of 180 mcg/actuation) inhaled by mouth as needed whenever a short-acting beta-agonist (SABA) is given.[69016] NAEPP only recommends as-needed inhaled corticosteroid/SABA as an option for patients with mild persistent asthma.[66299]
180 to 360 mcg (1 to 2 actuations of 180 mcg/actuation) inhaled by mouth as needed whenever a short-acting beta-agonist (SABA) is given.[69016] NAEPP only recommends as-needed inhaled corticosteroid/SABA as an option for patients with mild persistent asthma.[66299]
180 mcg (1 actuation of 180 mcg/actuation or 2 actuations of 90 mcg/actuation) as needed whenever a short-acting beta-agonist (SABA) is given.[69016] NAEPP does not recommend intermittent as-needed inhaled corticosteroid/SABA therapy in this age group because therapy has not been adequately studied.[66299]
0.25 to 0.5 mg inhaled by nebulizer as needed whenever a short-acting beta-agonist (SABA) is given.[69016] NAEPP does not recommend intermittent as-needed inhaled corticosteroid/SABA therapy in this age group because therapy has not been adequately studied.[66299]
1 mg inhaled by nebulizer twice daily for 7 days in combination with as-needed short-acting beta-agonist (SABA).[66299]
180 to 360 mcg (1 to 2 oral inhalations of 180 mcg/actuation) twice daily is usual dose range. FDA-approved Max: 4 oral inhalations of 180 mcg/actuation twice daily (720 mcg twice daily).[34376] The efficacy of budesonide in the treatment of EIB has been studied in adults.[56336] Titrate to the lowest effective dose. Regular ICS (controller) use reduces the incidence of EIB.[56291]
180 to 360 mcg (1 to 2 oral inhalations of 180 mcg/actuation) twice daily is the usual dose range. Max: 2 oral inhalations of 180 mcg/actuation twice daily (360 mcg twice daily).[34376] The efficacy of budesonide for EIB has been studied in pediatric patients.[56422] [56423] [56424] Titrate to the lowest effective dose. Regular ICS (controller) use reduces the incidence of EIB.[56291]
The optimal dose for the maintenance treatment of COPD is not established; typical doses of 180 to 360 mcg (1 to 2 actuations of 180 mcg/actuation strength) twice daily may be considered.[50611] Not for the relief of acute bronchospasm; use a short-acting beta-2 agonist (SABA). According to guidelines, inhaled corticosteroid (ICS) in combination with a long-acting beta-2 agonist (LABA) is not recommended for COPD treatment; however, it is an option for those patients with stable disease who are already receiving this therapy with no major symptoms or exacerbations. Escalation to triple therapy with a long-acting muscarinic antagonist (LAMA), a LABA, and an ICS should be considered for patients who have further exacerbations or major symptoms.[69470]
The optimal dose is not established; used for COPD exacerbations. 1 to 2 mg every 6 hours via nebulizer is a common dosage; some studies have used 2 mg twice daily. Reported total daily dose range for acute exacerbations of COPD: 4 to 8 mg/day. Usual Max: 2 mg/dose.[63369] [63370] [63371] Nebulized budesonide for the treatment of exacerbations may be an alternative to oral corticosteroids in some patients.[69470]
2 mg inhaled by nebulizer as a single dose, or alternatively, 1 mg inhaled by nebulizer every 30 minutes for 2 doses.[24066] [25097] [56026] [56027] [56028] [56077] Budesonide is considered an alternative to a single dose of oral dexamethasone, particularly in those unable to take oral medication.[56026] [56027] [59632] [59639] Efficacy has been demonstrated in several studies.[44927] [56029] Most studies have shown comparable efficacy outcomes with dexamethasone for the treatment of croup; however, some studies have shown dexamethasone to be superior to budesonide.[25096] [56030] [56032] The addition of budesonide to dexamethasone therapy has not resulted in an additive benefit.[25097] [56028]
2 sprays (32 mcg/spray) in each nostril once daily. After clinical response has been obtained, decrease to 1 spray in each nostril once daily. If no response after 2 weeks, consult a health care provider.[59312] Prior to non-prescription OTC status, maximum dosages of 256 mcg/day were FDA-approved.[31824]
2 sprays (32 mcg/spray) in each nostril once daily. After clinical response has been obtained, decrease to 1 spray in each nostril once daily. If no response after 2 weeks, consult a health care provider.[59312] Prior to non-prescription OTC status, maximum dosages of 256 mcg/day were FDA-approved.[31824]
Initially, 1 spray (32 mcg/spray) in each nostril once daily. If symptoms do not improve, may increase to 2 sprays in each nostril once daily. After clinical response has been obtained, decrease to 1 spray in each nostril once daily. Non-prescription use in younger children is intended to be assisted by an adult. If the child uses this product for longer than 2 months per year, or, if there is no response to treatment after 2 weeks, consult a pediatrician.[59312] Prior to non-prescription OTC status, maximum dosages of 128 mcg/day were FDA-approved.[31824]
9 mg PO once daily for up to 8 weeks, then 6 mg PO once daily for up to 3 months. Taper to complete cessation if symptom control is still maintained at 3 months. Continued treatment for more than 3 months has not been shown to provide substantial benefit. A repeat 8-week course may be given for recurring episodes of active disease. A Crohn Disease Activity Index (CDAI) less than 150 after 8 weeks of treatment for active disease is recommended before maintenance treatment is initiated.[34979] Guidelines strongly recommend that budesonide not be used to maintain remission of Crohn disease beyond 4 months.[64397]
9 mg PO once daily for up to 8 weeks, then 6 mg PO once daily for 2 weeks.[34979] Repeat courses may be needed if active disease recurs.[56014]
9 mg PO once daily in the morning for up to 8 weeks.[52910] Taper dose based on clinical symptoms, cumulative steroid exposure, and onset of action of alternate therapies; limit use to shortest duration possible.[64393] Guidelines recommend oral budesonide to induce remission in persons with ulcerative colitis; however, guidelines recommend against systemic corticosteroids for the maintenance of remission.[64377] [64393]
2 mg rectally twice daily for 2 weeks, then 2 mg rectally once daily at bedtime for 4 weeks.[58166] Taper dose based on clinical symptoms, cumulative steroid exposure, and onset of action of alternate therapies; limit use to shortest duration possible.[64393]
9 mg PO once daily or on a tapering schedule for 8 weeks has been used in clinical trials. A Cochrane review of IBD and functional bowel disorder trials concluded that budesonide is effective and well-tolerated for inducing and maintaining clinical and histological response in patients with collagenous colitis.[64534] In a placebo-controlled, randomized trial (n = 28), 8 of 14 patients receiving 9 mg/daily were considered responders (p = 0.05), with patients reporting improved stool consistency. Histological findings included a significant decrease in the lamina propria infiltrates in the budesonide group (p is less than 0.001).[33153] Another controlled trial (n = 20) studied a tapering regimen of 9 mg PO for 4 weeks, 6 mg for 2 weeks, and 3 mg for 2 weeks. All 10 patients in the budesonide group experienced a clinical response, and treated patients reported reduced stool weight and frequency; histological inflammation was also significantly improved.[33154]
16 mg PO once daily in the morning for 9 months. When discontinuing therapy, reduce dose to 8 mg PO once daily for the last 2 weeks of therapy. The safety and efficacy of treatment with subsequent courses have not been established.[67192]
3 mg PO 3 times daily, initially. When biochemical remission is achieved, taper dose gradually over 6 months to 3 mg PO once daily or the lowest dose to maintain remission. Guidelines recommend budesonide in combination with azathioprine as first-line therapy in adults who present with autoimmune hepatitis (AIH) who do not have cirrhosis, acute severe AIH, or acute liver failure. May attempt steroid withdrawal while continuing azathioprine.[68993] [68996]
3 mg PO 3 times daily, initially. When biochemical remission is achieved, taper dose gradually over 6 months to 3 mg PO once daily or the lowest dose to maintain remission. Guidelines recommend budesonide in combination with azathioprine as first-line therapy in children who present with autoimmune hepatitis (AIH) who do not have cirrhosis, acute severe AIH, or acute liver failure. May attempt steroid withdrawal while continuing azathioprine.[68993] [68996]
3 mg PO 3 times daily.[69611] [69792] [69793]
3 mg PO 3 times daily.[69611] [69792]
2 mg PO twice daily for 12 weeks.[70334]
2 mg PO twice daily for 12 weeks.[70334]
1 mg PO (swallowed) twice daily for 8 weeks, then reduce dose to the lowest dose that maintains remission. Oral administration of viscous budesonide slurry achieves higher histological remission rates compared vs. oral administration by spraying and swallowing due to longer contact time with the oral mucosa.[55346] [56033] [65816] [70029] [70030] [70042] [70043]
0.5 mg PO (swallowed) twice daily for 8 weeks, then reduce dose to the lowest dose that maintains remission. Oral administration of viscous budesonide slurry achieves higher histological remission rates compared vs. oral administration by spraying and swallowing due to longer contact time with the oral mucosa.[55346] [56033] [65816] [70029] [70042] [70043]
9 mg PO once daily for at least 3 months.[69154] [71087]
3 mg PO 3 times daily for at least 3 months.[71082] [71087]
3 mg PO 3 times daily for at least 3 months.[71082] [71087]
2 mg rectally twice daily for 2 weeks, then 2 mg rectally once daily at bedtime for 4 weeks.[58166] [71542] [71545]
9 mg PO once daily for 8 to 12 weeks, then reduce dose by 3 mg/month until discontinued.[71542] [71547]
2 mg rectally twice daily for 2 weeks, then 2 mg rectally once daily at bedtime for 4 weeks.[58166] [71542] [71545]
9 mg PO once daily for up to 8 weeks. Taper dose based on clinical symptoms, cumulative steroid exposure, and onset of action of alternative therapies.[34979] [71542]
256 mcg/day intranasally; 1,440 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; doses of the nebulizer suspension as high as 8 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC); 9 mg/day PO for delayed release tablets (i.e., Uceris); 16 mg/day PO for delayed release capsules (i.e., Tarpeyo); 4mg/day PO for oral suspension (i.e., Eohilia); 4 mg/day rectally.
256 mcg/day intranasally; 1,440 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; doses of the nebulizer suspension as high as 8 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC); 9 mg/day PO for delayed release tablets (i.e., Uceris); 16 mg/day PO for delayed release capsules (i.e., Tarpeyo); 4mg/day PO for oral suspension (i.e., Eohilia); 4 mg/day rectally.
256 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; nebulizer suspension doses as high as 4 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC); 4 mg/day PO for oral suspension (i.e., Eohilia). Safety and efficacy of delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), and rectal formulations have not been established.
12 years: 256 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; nebulizer suspension doses as high as 4 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC); 4 mg/day PO for oral suspension (i.e., Eohilia). Safety and efficacy of delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), and rectal formulations have not been established.
11 years: 128 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; nebulizer suspension doses as high as 2 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC); 4 mg/day PO for oral suspension (i.e., Eohilia). Safety and efficacy of delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), and rectal formulations have not been established.
9 to 10 years: 128 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; nebulizer suspension doses as high as 2 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC). Safety and efficacy of delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), oral suspension (i.e., Eohilia), and rectal formulations have not been established.
8 years: 128 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; 1 mg/day of the nebulizer suspension is the FDA-approved maximum dosage; however, doses as high as 2 mg/day have been used off-label. 9 mg/day PO for extended release or delayed release capsules (i.e., Ortikos, Entocort EC). Safety and efficacy of delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), oral suspension (i.e., Eohilia), and rectal formulations have not been established.
6 to 7 years: 128 mcg/day intranasally; 720 mcg/day via dry powder inhaler (DPI) is the FDA-approved maximum dosage; 1 mg/day of the nebulizer suspension is the FDA-approved maximum dosage; however, doses as high as 2 mg/day have been used off-label. Safety and efficacy of extended release or delayed release capsules (i.e., Ortikos, Entocort EC), delayed release tablets (i.e., Uceris), delayed release capsules (i.e., Tarpeyo), oral suspension (i.e., Eohilia), and rectal formulations have not been established.
1 to 5 years: 1 mg/day of the nebulizer suspension is the FDA-approved maximum dosage; however, doses as high as 2 mg/day have been used off-label. Safety and efficacy of other formulations have not been established.
Safety and efficacy have not been established; however, doses up to 2 mg/day of the nebulizer suspension have been used off-label.
Nasal or Inhaled products: No dosage adjustment suggested.[59312][33486][34376]
Rectal foam: No dosage adjustment needed. Monitor the patient for signs and symptoms of hypercorticism. Consider drug discontinuation in cases of hypercorticism.[58166]
Oral delayed-release capsules (e.g., Entocort EC)
Mild hepatic impairment (Child-Pugh Class A): No dosage adjustment is needed.
Moderate hepatic impairment (Child-Pugh Class B): Consider a reduced dose of 3 mg once daily. Monitor the patient for signs/symptoms of hypercorticism. Consider drug discontinuation in cases of hypercorticism.
Severe hepatic impairment (Child-Pugh Class C): Avoid use.[34979]
Oral delayed-release capsules or Oral budesonide suspension (e.g., Tarpeyo, Eohilia)
Mild hepatic impairment (Child-Pugh Class A): No dosage adjustment is needed.
Moderate hepatic impairment (Child-Pugh Class B): Monitor the patient for signs and symptoms of hypercorticism. Consider drug discontinuation in cases of hypercorticism.
Severe hepatic impairment (Child-Pugh Class C): Avoid use.[67192][70334]
Oral extended-release capsules (i.e., Ortikos)
Mild hepatic impairment (Child-Pugh Class A): No dosage adjustment is needed.
Moderate or severe hepatic impairment (Child-Pugh Class B or C): Avoid use.[64318]
Oral delayed-release tablet (i.e., Uceris)
Mild hepatic impairment (Child-Pugh Class A): No dosage adjustment is needed.
Moderate or severe hepatic impairment (Child-Pugh Class B or C): Monitor the patient for signs and symptoms of hypercorticism. Consider drug discontinuation in cases of hypercorticism.[52910]
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication































Budesonide is a corticosteroid that is administered via intranasal inhalation, oral inhalation, rectally, or orally. Budesonide has potent glucocorticoid and weak mineralocorticoid activity. Budesonide formulations are used to manage symptoms associated with allergic rhinitis, selected lung diseases, inflammatory bowel disease (Crohn's disease and ulcerative colitis), eosinophilic esophagitis (EoE), or primary immunoglobulin A nephropathy (IgAN) in adults, depending on the formulation chosen. Inhaled budesonide possesses high topical anti-inflammatory activity but low systemic activity. Inhaled corticosteroids (ICS) are the preferred pharmacologic treatment in the long-term management of persistent asthma for most patients.[69016][66299][67192] Maintenance ICS therapy may also decrease the frequency and severity of exercise-induced bronchoconstriction (EIB); short-acting beta-2 agonists (SABAs) also help prevent EIB, but tolerance can develop with regular SABA use.[56291] According to guidelines, budesonide in combination with an inhaled long-acting beta-2 agonist (LABA) is not recommended for COPD treatment; however, it is an option for those patients with stable disease who are already receiving this therapy with no major symptoms or exacerbations. Escalation to triple therapy with a long-acting muscarinic antagonist (LAMA), a LABA, and an ICS should be considered for patients who have further COPD exacerbations or major symptoms. Patients with COPD who have concomitant asthma should be treated with an ICS.[69470] Budesonide nasal spray allows for once-daily dosing for allergic rhinitis. Rhinitis guidelines strongly recommend intranasal corticosteroids as the preferred medication when choosing monotherapy for persistent allergic rhinitis; they may also be offered as first-line therapy for nonallergic rhinitis (NAR) although intranasal antihistamines are strongly recommended as a first-line monotherapy option for NAR.[66102] Oral budesonide has been shown to be superior to placebo and equivalent to prednisolone, but with fewer adverse reactions, in treating active Crohn's disease.[24064][24065] A budesonide oral tablet with a proprietary delivery system (MMX, a multi-matrix system) that delivers medicine to the colon, has been shown to be effective at inducing remission in patients with active, mild to moderate ulcerative colitis.[52909][52910] Several studies also indicate the benefit of oral budesonide in treating microscopic colitis and, specifically, collagenous colitis.[33152] Clinical trials have shown patients with EoE taking oral budesonide suspension for 12 weeks were able to achieve histological remission (38% to 53.1%) and helped improve or eliminated dysphagia symptoms.[70334]
For storage information, see specific product information within the How Supplied section.
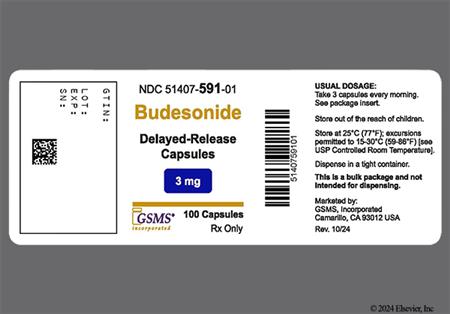
Delayed-release capsules (e.g., Entocort EC and equivalent generics):
Delayed-release capsules (e.g., Tarpeyo):
Extended-release capsules (e.g., Ortikos):
Extended-release tablets (e.g., Uceris):
Extemporaneous compounding instructions for budesonide oral suspension:
Dry powder for inhalation (Pulmicort Flexhaler):
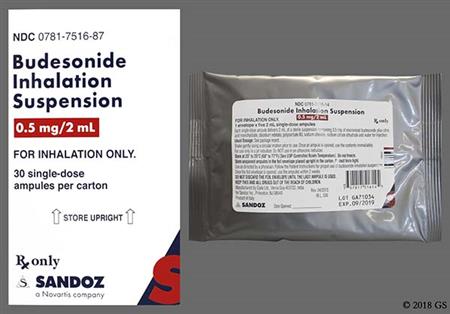
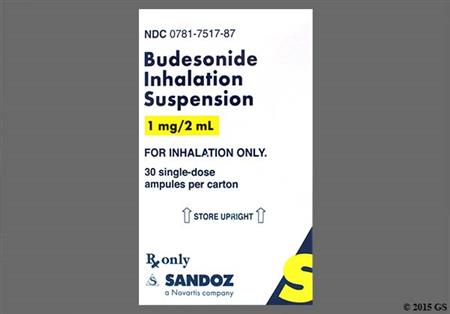
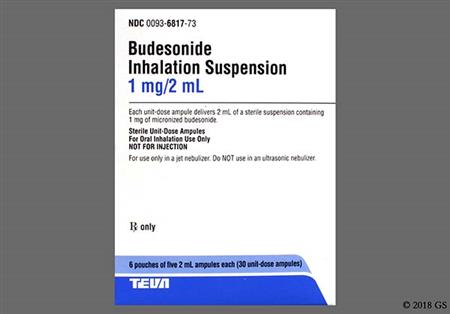
Inhalation suspension for nebulization (Pulmicort Respules):
Rectal Foam
Respiratory infection (8% to 11%), sinusitis (8%), and viral infection (6%) have been reported in adult patients during clinical trials with oral budesonide. Ear infection (unspecified), bronchitis, abscess, rhinitis, dyspnea, and pharynx disorder were reported in less than 5% of adult patients receiving oral budesonide.[34979] [64318] [67192] Respiratory tract infection (including acute sinusitis, sinusitis, nasopharyngitis, respiratory tract infection, viral respiratory infection, upper respiratory tract infection, viral upper respiratory tract infection, and rhinitis) were reported in 13% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE). Throat irritation/oropharyngeal pain (3%) and nasal congestion (less than 2%) were reported in patients receiving oral budesonide suspension for EoE.[70334] Nasal or respiratory adverse events reported during treatment with nasal budesonide include cough (2%), epistaxis (8%), pharyngitis (4%), nasal irritation (2%), sinusitis (3% or more), and bronchospasm (2%).[31824] Respiratory infection (3% to 38%), rhinitis (7% to 12%), cough (5% to 9%), nasopharyngitis (9%), nasal congestion (3%), pharyngitis (3%), allergic rhinitis (2%), viral upper respiratory tract infection (2%), otitis media (1% to 12%), ear infection (2% to 5%), epistaxis (2% to 4%), and viral infection (2% to 5%) were reported by patients receiving budesonide inhalation powder or budesonide inhalation suspension. Chest pain, dysphonia, stridor, otalgia, external ear infection, voice alteration, and cervical lymphadenopathy were also reported in 1% to less than 3% of patients.[33486][34376] Throat irritation and bronchitis has also been reported during postmarketing use of budesonide inhalation powder and suspension.[31824] [33486] [34376] [34979] [52910] [58166] [64318] [70334] Nasal septum perforation, anosmia, pharynx disorders (throat irritation, throat pain, swollen throat, burning throat, itchy throat), and wheezing have been reported with intranasal budesonide during postmarketing experience.[31824] As with other inhaled asthma medications, paradoxical bronchospasm can occur with an immediate increase in wheezing after administration of inhaled beclomethasone that may be life-threatening.[33486] [34376]
Headache (10% to 21%), dizziness (7%), fatigue (2% to 5%), mood changes (2.5% to 6.5%), and insomnia (up to 6.5%) were reported during clinical trials in adult patients with oral budesonide. Agitation, amnesia, confusion, hyperkinesis, nervousness, paresthesias, sleep changes, somnolence or drowsiness, tremor, and vertigo have been reported in less than 5% of adult patients receiving oral budesonide.[34979] [52910] [64318] [67192] Headache/migraine (5%) were reported in adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE). Fatigue, feeling abnormal, depression, irritability, restlessness, and tremor were reported in less than 2% of adult and pediatric patients receiving oral budesonide suspension for EoE.[70334] Insomnia, sleep disorder, and depression were reported in less than 1% of adult patients using budesonide rectal foam.[58166] In pediatric patients (age 12 months to 8 years), hyperkinesia (restlessness), fatigue, and emotional lability was reported in 1% to less than 3% of patients receiving budesonide inhalation suspension.[33486] Headache (3% or more) and migraine (1% to 3%) have been reported in with budesonide inhalation powder and suspension. Psychosis, emotional lability, depression, aggressive reactions, irritability, nervousness, restlessness, anxiety, and headache have been reported in postmarketing experience with budesonide inhalation powder and suspension.[34376] [33486] Mood swings, agitation, confusion, insomnia, nervousness, dizziness, and sleep disorder have been reported in postmarketing experience with oral budesonide.[34979] [64318] Mood swings and dizziness have been reported in postmarketing experience with rectal budesonide.[52910]
Dermatitis (6% or less) was reported in adult patients receiving oral budesonide. Alopecia, eczema (atopic dermatitis), skin disorder, hyperhidrosis, and purpura were reported in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979][64318][67192] Ecchymosis (8%) has been reported in patients receiving nasal budesonide in clinical trials.[31824] In pediatric patients, rash was reported in up to 4% of patients receiving budesonide inhalation suspension (age 12 months to 8 years). Allergic reaction, contact dermatitis, ecchymosis, eczema, pustular rash, pruritus, and purpura occurred in 1% to less than 3% of patients receiving inhaled budesonide power or suspension.[33486] [34376] Anaphylactic reactions, angioedema, bronchospasm, dermatitis, rash, ecchymosis, urticaria, and facial skin irritation have been reported with postmarketing use of budesonide inhalation powder, inhalation suspension, and intranasal budesonide.[33486] [34376] Wheezing or bronchospasm in patients with severe milk protein hypersensitivity has been reported in postmarketing experience with budesonide inhalation powder use.[34376] Anaphylactoid reactions, maculopapular rash, and allergic dermatitis have been reported with oral and rectal budesonide during postmarketing use.[34979] [52910] [58166] [64318] [70334] Discontinue budesonide if such reactions occur.
Budesonide therapy, just like any corticosteroid, has been associated with the development of cataracts, increased ocular pressure or ocular hypertension, and glaucoma. Long-term use of inhaled corticosteroids may increase the risk of these eye problems. Regular eye examinations should be done.[33486] Eye abnormality and abnormal vision/visual impairment was reported in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [64318] In pediatric patients (age: 12 months to 8 years), conjunctivitis (less than 1% to 4%) and ocular infection (unspecified) (1% to less than 3%) were reported in patients receiving budesonide inhalation suspension.[33486] Cataracts, glaucoma, and increased intraocular pressure have been reported during postmarketing experience with budesonide inhalation powder, inhalation suspension, and intranasal budesonide.[31824] [33486] [34376]
Pharmacologic doses of corticosteroids administered for prolonged periods can result in hypothalamic-pituitary-adrenal (HPA) suppression. Adrenocortical insufficiency was reported in 1% more of adult patients taking oral budesonide.[34979] [64318] In a study looking at response to ACTH stimulation in patients receiving oral budesonide 9 mg once daily, the proportion of patient with an abnormal response was 47% at 4 weeks and 79% at 8 weeks.[52910] Adrenal suppression, including adrenal insufficiency, was reported in 2% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334] A decrease in blood cortisol (17%) and adrenal insufficiency (4%) has been reported in adult patients using budesonide rectal foam.[58166] Adrenal insufficiency and withdrawal symptoms may occur after treatment discontinuation or when transitioning from systemic corticosteroids to inhaled corticosteroids. Patients should taper slowly if discontinuing corticosteroids or when transitioning from systemic corticosteroids to inhaled budesonide suspension or dry powder inhaler.[33486] [34376] Symptoms of adrenal insufficiency include tiredness, weakness, nausea and vomiting, and low blood pressure. The severity of glucocorticoid-induced secondary adrenocortical insufficiency varies among individuals and is dependent on the dose, frequency, time of administration, and duration of therapy. Use of inhaled corticosteroids with systemic corticosteroids could increase the likelihood of HPA suppression as compared with a therapeutic dose of either alone.[31824] [33486] [34376] [34979] [52910] [58166] [64318] [70334] Symptoms of hypocorticism and hypercorticism have been reported during postmarketing experience with budesonide inhaled suspension.[33486]
Corticosteroids may cause growth inhibition in pediatric subjects. Data regarding effects on growth are conflicting; the lowest effective dose of any corticosteroid dosage form should be utilized and growth should be routinely monitored during use.[66299] Growth inhibition has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA) suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in children. With orally inhaled corticosteroids, the mean reduction in growth velocity is approximately 1 centimeter/year (range 0.3 to 1.8 centimeter/year) and appears to be related to the dose and duration of exposure. In a study, children 5 to 12 years of age with asthma receiving inhaled budesonide experienced a 1.1 centimeter reduction in growth compared to the placebo group by the end of 1 year. By the end of 4 years, the growth velocities of both groups were similar.[33486] In general, the benefits of regular inhaled corticosteroid use outweigh the potential risk of relatively small and non-cumulative growth suppression in children with asthma; however, growth should be monitored.[57670] Further study is needed to determine the long-term effects of growth velocity reduction in children, including the impact on final adult height. To minimize the effects of inhaled corticosteroids, titrate to the lowest effective dose.[34376] [33486] [34979] [52910] [57670] [58166] [64318] [70334] Growth suppression has been reported with postmarketing experience with budesonide inhalation suspension.[33486]
Arthralgia (2% to 6%) and arthritis (less than 5%) was reported in adult patients receiving oral budesonide.[34979][52910] [64318] [67192] Arthralgia was reported in less than 2% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334] Arthralgia was reported in adult patients receiving budesonide via a dry powder inhaler.[34376] Fracture was reported in 1% to less than 3% of pediatric patients (age 12 months to 8 years) receiving budesonide inhalation suspension during clinical trials.[33486] Prolonged use (e.g., more than 1 year) of high doses of inhaled corticosteroids, such as budesonide, especially when used in combination with frequent courses of systemic corticosteroids, may be associated with skeletal changes and reduced bone mineral density (BMD), which may increase the risk of osteopenia and osteoporosis. The clinical significance of small changes in BMD with regard to long-term outcomes, such as fracture, is unknown. Avascular necrosis of the femoral head and osteoporosis were reported with postmarketing experience with budesonide inhalation suspension.[33486]
Signs and symptoms of hypercorticism (Cushing syndrome) have been reported in adult individuals receiving oral budesonide and included: flushing (less than 5%), acne vulgaris (1% to 15%), bruising easily (5% to 15%), moon face or Cushingoid features (1% to 11%), swollen ankles (2% to 7%), hirsutism (0% to 5%), buffalo hump (1%), skin striae (2% or less), fluid retention (1% to 2%), and face edema (8% or less).[34979] [52910] [64318] [67192] Hirsutism and dermatitis acneiform were reported in less than 2% of adult and pediatric individuals receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334] Acne (less than 1%) and hyperglycemia (less than 1%) has been reported in adult individuals receiving budesonide rectal foam.[58166] Benign increased intracranial pressure has been reported during postmarketing experience with budesonide.[34979] [52910] [58166]
Nausea (5% to 11%), diarrhea (10%), dyspepsia (6% to 7%), abdominal pain (6%), upper abdominal pain (3% to 4%), abdominal distension (2%), flatulence (2% to 6%), constipation (2% or less), vomiting (6%), and weight gain (7% or less) were reported in adult patients receiving oral budesonide during clinical trials. Anus disorder, enteritis, epigastric pain, gastrointestinal fistula, glossitis, hemorrhoids, GI obstruction, tongue edema, tooth disorder, and appetite stimulation were reported in less than 5% of patients.[34979] [52910] [64318] [67192] Gastroenteritis (3%) and erosive esophagitis (2%) were reported in adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE). Xerostomia, dysgeusia, dyspepsia, erosive duodenitis, gastrointestinal motility disorder, esophageal food impaction, and palatal swelling were all reported in less than 2% of patients receiving oral budesonide suspension for EoE.[70334] Nausea (2%) was reported in adult patients using budesonide rectal foam.[58166] Nausea (2%), viral gastroenteritis (2%), dry mouth (1% to less than 3%), and taste perversion/dysgeusia (1% to less than 3%) were reported in adult and pediatric patients receiving budesonide inhalation powder (age 6 years and older).[34376] Gastroenteritis (5%), vomiting (2% to 4%), diarrhea (2% to 4%), abdominal pain (2% to 3%), and anorexia (1% to less than 3%) were reported in pediatric patients receiving budesonide inhalation suspension.[33486] Rectal GI bleeding has been reported during postmarketing experience with oral budesonide tablets.[52910] Pancreatitis has also been reported during postmarketing experience for budesonide.[58166]
Peripheral edema (17%) and hypertension (12% or less) have been reported during clinical trials in adult patients receiving oral budesonide. Palpitations, sinus tachycardia, dependent edema, and chest pain (unspecified) were reported in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [64318] [67192] Palpitations, hypertension, and syncope were reported in less than 2% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334] In pediatric patients, chest pain has been reported in 1% to less than 3% of patient receiving budesonide inhalation suspension.[33486] Syncope has been reported in 1% to less than 3% of pediatric patients using budesonide inhalation powder.[34376] An increase in blood pressure has been reported during postmarketing experience with budesonide.[52910]
In rare cases, persons receiving inhaled budesonide may present with eosinophilia and clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition often treated with systemic corticosteroids. These events have happened most commonly in association with systemic corticosteroid withdrawal in conjunction with the introduction of inhaled corticosteroid therapy. Persons presenting with eosinophilia, vasculitis with granulomas, worsening pulmonary symptoms, and/or neuropathy may have this condition, which may be severe. Similar cases have been reported with the use of other inhaled corticosteroids. A causal relationship to budesonide has not yet been established.[33486] [34376]
Asthenia, influenza or flu-like disorder, malaise, and fever occurred in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [64318] Fever was reported in 3% or more of patients using inhaled budesonide via a dry power inhaler.[34376] Fatigue and flu-like disorder were reported in 1% to less than 3% of pediatric patients (age 12 months to 8 years) receiving budesonide inhalation suspension during clinical trials.[33486] Fever has been reported during postmarketing experience with oral, rectal, and inhaled budesonide.[33486] [58166]
Leukocytosis (increased white blood cell count) was reported in 1% to 6% in adult patients receiving oral budesonide.[67192] [34979] Hypokalemia was reported in less than 5% of patients receiving one oral capsule formulation at incidences greater than with placebo, and greater than 1% of patients receiving other oral formulations.[34979] [64318] Anemia, hematuria, pyuria, increased erythrocyte sedimentation rate, increased alkaline phosphatase, atypical neutrophils, increased c-reactive protein, and adrenal insufficiency where reported in 1% or more of adult patients taking oral budesonide.[34979] [64318] Hyperkalemia, elevated hepatic enzymes (transaminases increased), and dyslipidemia were reported in less than 2% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334]
Gastrointestinal mucosal candidiasis (including esophageal candidiasis, oropharyngeal candidiasis, oral candidiasis) was reported in 8% of adult and pediatric patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE). Fungal skin infection, paronychia, pneumonia, sepsis, and bronchitis were reported in less than 2% of patients receiving oral budesonide suspension for eosinophilic esophagitis (EoE).[70334] Urinary tract infection and thrush have occurred in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [52910] [64318] In clinical studies with intranasal budesonide, the development of localized infections of the nose and pharynx with Candida albicans has occurred.[31824] Oral candidiasis infection was reported in 1% of adult and pediatric patients receiving budesonide inhalation powder (age 6 years and older). Rinsing the mouth after use of budesonide inhalation powder may minimize the incidence of oropharyngeal thrush.[34376] Moniliasis (3% to 4%) was reported in pediatric patients (age 12 months to 8 years) receiving budesonide inhalation suspension during clinical trials. Herpes simplex and infection (unspecified) were reported in 1% to less than 3% of pediatric patients.[33486] Monitor patients on long-term budesonide therapy for signs of infection. Discontinuation of budesonide may be required.[33486] [34376] [34979] [52910] [58166] [64318] [67192] [70334]
Dysuria, increased urinary frequency (micturition frequency), and nocturia were reported in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [64318]
Vaginal bleeding (intermenstrual bleeding) and menstrual irregularity/menstrual disorder has been reported in less than 5% of adult patients receiving oral budesonide during clinical trials.[34979] [64318]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Budesonide inhalation powder contains small amounts of lactose, which contains trace levels of milk protein. Patients with a severe milk protein hypersensitivity may experience an allergic reaction to this product.[34376]
Inhaled budesonide is contraindicated as primary therapy for individuals with status asthmaticus or other types of acute bronchospasm for which intensive therapy is warranted. Caution individuals that budesonide is not to be used as a bronchodilator and is not indicated for relief of acute bronchospasm.[33486][34376]
Systemic corticosteroids, including budesonide, may cause immunosuppression and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Additionally, corticosteroids may mask symptoms and increase the risk of severe or fatal infectious complications in a dose-dependent manner, requiring close monitoring and potential dose adjustment or withdrawal. Systemic budesonide and other corticosteroids may cause severe or fatal infections by reactivating or worsening TB, hepatitis B, amebiasis, Strongyloides, or herpes infections (varicella, measles, herpes simplex), exacerbate systemic fungal disease, and should be avoided in cerebral malaria; screen, monitor, and provide prophylaxis or antiviral/antiparasitic therapy as indicated.[52910] [70334] [67192] These precautions and considerations also apply to budesonide rectal foam and inhalational product use.[58166] [33486] [34376] Administration via the nasal route generally minimizes systemic infection risk. Localized fungal infection of the nose, mouth, and pharynx with Candida albicans has been reported with inhalational or nasal corticosteroid use. Instruct patients to rinse mouth after each use of nasal or inhaled budesonide to minimize risk.[31824] [33486] [34376] Patients using budesonide nasal spray for extended periods (i.e., months) should be examined periodically for evidence of infection or other adverse effects on the nasal mucosa.[31824]
Studies of pregnant women have not shown that inhaled budesonide increases the risk of abnormalities when administered during pregnancy.[31824] [33486] [34376] [46711] A review of Swedish registries of more than 2,000 births indicated that no increased risk for congenital malformations during early pregnancy with budesonide inhalation powder or solution.[46713] Despite adverse effects in animal studies, fetal harm appears remote. Corticosteroid treatment may not be necessary during pregnancy due to a natural increase in corticosteroid production; however, poorly controlled maternal asthma also poses risk to the mother and the fetus. Low-dose inhaled corticosteroids are considered first-line therapy for control of mild persistent asthma during pregnancy according to the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group; of the inhaled corticosteroids, more data are available for budesonide use in pregnancy. Data on the use of medium- to high-dose inhaled corticosteroid use during pregnancy are limited. However, dose titration may be considered for those with moderate to severe persistent asthma, preferably using budesonide. However, there are no data to indicate safety concerns with other inhaled corticosteroids, and maintaining a previously established treatment regimen may be more beneficial to the patient.[31822] Selection of any pharmacologic treatment for asthma control during pregnancy should include the specific needs of the patient, based on an individual evaluation, and consideration of the potential benefits or risks to the fetus. A position statement by the American College of Allergy, Asthma and Immunology also considers budesonide a good choice for pregnant women requiring high doses of inhaled steroids for effective asthma management.[46717] Limited published studies report on the use of oral budesonide in pregnant patients; however, the data are insufficient to inform a drug-associated risk of major birth defects and miscarriage. Oral budesonide products (e.g., Entocort EC, Ortikos, Uceris, Tarpeyo) have been teratogenic and embryocidal in animal studies. At subcutaneous budesonide doses that were 0.3 to 0.5 or 0.03 to 0.05 times the maximum recommended human dose (MRHD) in pregnant rats and rabbits, respectively, fetal loss, decreased pup weights, and skeletal anomalies occurred. There is a natural increase in endogenous corticosteroid production during pregnancy, and many women will require a lower exogenous dose or no corticosteroid treatment at all during pregnancy. Oral budesonide (e.g., Entocort EC, Ortikos, Uceris, Eohilia, Tarpeyo) products should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus. Some studies show an association of adverse pregnancy outcomes in women with Crohn's disease with increased disease activity (increased stool activity and abdominal pain) which can lead to preterm birth and low birth weight infants. Counsel the patients about the importance of controlling the disease.[34979] [64318] IgA nephropathy in pregnancy is associated with adverse maternal outcomes, including increased rates of cesarean section, pregnancy-induced hypertension, pre-eclampsia and preterm delivery, and adverse fetal/neonatal outcomes, including stillbirth and low birth weight. Hypoadrenalism may occur in an infant born to a mother receiving corticosteroids during pregnancy, and the infant should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting.[34979] [52910] [64318] [67192] [70334]
Oral, nasal, rectal, and inhaled forms of budesonide are compatible with breast-feeding. The amount of infant exposure from use of inhaled budesonide by the breast-feeding parent is negligible. Budesonide is excreted into breast milk in small amounts with a relative infant dose (RID) of 0.3%. In addition, budesonide has an oral bioavailability of 10.7%, further limiting total infant exposure.[70364] [70365] Based on data from a small number (n = 8) of breast-feeding women taking inhaled dry powder budesonide 200 to 400 mcg twice daily, approximately 0.3% to 1% of the dose inhaled by the mother is available via breast milk to an exclusively breast-fed infant. Budesonide plasma concentrations obtained in five of the infants in this study about 140 minutes after maternal drug administration and 90 minutes after breast-feeding were below quantifiable levels.[33725] Low-dose inhaled corticosteroids are considered first line therapy for control of mild persistent asthma during pregnancy and lactation according to the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group. Due to greater availability of data, budesonide is considered the preferred agent in this population.[31822] Reviewers and an expert panel consider all inhaled corticosteroids acceptable to use during breast-feeding.[33723] [33724] [31822] Single- and repeated-dose pharmacokinetic studies have shown that maximum plasma budesonide concentrations after a 9 mg oral daily dose are up to 10-times greater than the concentrations measured after inhaled doses of 400 to 800 mcg/day. Assuming that the coefficient of extrapolation between inhaled and oral doses is constant across all doses, it is possible that budesonide exposure to breast-feeding infants after maternal oral ingestion may be up to 10-times higher than exposure to infants after maternally inhaled budesonide.[34979] [52910]
Due to the inhibitory effects of glucocorticoids on wound healing, intranasal budesonide should be avoided in patients with a recent history of oral surgery or nasal surgery, nasal trauma, or nasal septal ulceration until their condition has healed. Intranasal budesonide overuse, improper use, or chronic use might lead to nasal septal perforation; patients who experience recurrent episodes of epistaxis (nosebleeds) or nasal septum discomfort while taking this medication should contact their care team for evaluation. If perforation occurs, the drug should be discontinued until healing is complete.[31824]
Corticosteroids, including budesonide, can decrease bone mineral density (BMD). Monitor patients with increased risk for osteoporosis.[33486] [34376] [34979] [52910] [64318] [67192]
Monitor individuals with hypertension, diabetes mellitus or who have a family history of diabetes, and peptic ulcer disease. Budesonide may exacerbate these conditions.[34979] [52910] [58166] [64318] [67192]
Budesonide undergoes extensive hepatic metabolism. Patients who have moderate hepatic impairment (Class-Pugh B), severe hepatic impairment (Class-Pugh C), or hepatic failure may be at an increased risk of hypercorticism and adrenal axis suppression due to increased budesonide systemic exposure. Avoid use in patients with severe hepatic impairment (Child-Pugh Class C). Monitor for increased signs and/or symptoms of hypercorticism and consider dosage reduction in patients with moderate hepatic impairment (Child-Pugh Class B). No dosage adjustment is suggested for nasal, inhaled, or rectal budesonide. In patients with mild hepatic impairment, no dosage adjustments for oral formulations are recommended; however, avoidance or dosage adjustment is product specific in patients with moderate to severe hepatic disease receiving oral formulations. Monitor all patients on any form of budesonide for signs and symptoms of hypercorticism. Consider discontinuing budesonide if hypercorticism is observed.[34979] [52910] [58166] [64318] [67192] [70334]
Prolonged use of systemic corticosteroids may produce posterior subcapsular cataracts and glaucoma with possible damage to the optic nerves. Rare instances of glaucoma, increased intraocular pressure, and cataracts have been reported after the inhaled or intranasal administration of corticosteroids. Use budesonide with caution in individuals potentially predisposed to these conditions; have individuals using budesonide report any unexplained visual disturbance promptly. Individuals with a change in vision or a history of increased intraocular pressure, glaucoma, or cataracts should be closely monitored during corticosteroid therapy. Consider referral to an ophthalmologist in individuals who develop ocular symptoms or who use budesonide long term.[31824] [34376] [33486] [34979] [52910] [67192] [70334]
There is no special precaution needed for the dosage of inhaled, rectal, or nasal budesonide in older adults.[34376] [59312] [58166] In general, oral budesonide dose selection for a geriatric adult should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy, particularly with chronic use.[34979] [52910] [64318] [67192] According to the Beers Criteria, systemic corticosteroids are considered potentially inappropriate medications (PIMs) for use in geriatric patients with delirium or at high risk for delirium; avoid when possible in these patient populations due to the possibility of new-onset delirium or exacerbation of the current condition. Oral corticosteroids may be required for chronic conditions but should be prescribed in the lowest effective dose and for the shortest possible duration.[63923]
Glucocorticoids are naturally occurring hormones that prevent or suppress inflammation and immune responses when administered at pharmacological doses. In general, glucocorticoids inhibit the activity of a variety of cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, and lymphocytes) and mediators involved in allergic and nonallergic/irritant-mediated inflammation (e.g., histamine, eicosanoids, leukotrienes, and cytokines). At the molecular level, unbound glucocorticoids readily cross cell membranes and bind with high affinity to specific cytoplasmic receptors. Subsequent to binding, transcription and, ultimately, protein synthesis are affected. The result can include inhibition of leukocyte infiltration at the site of inflammation, interference in the function of mediators of inflammatory response, and suppression of humoral immune responses. The anti-inflammatory actions of corticosteroids are thought to involve phospholipase A2 inhibitory proteins, collectively called lipocortins. Lipocortins, in turn, control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes by inhibiting the release of the precursor molecule arachidonic acid. Some of the net effects include reduction in edema or scar tissue as well as a general suppression in immune response. The numerous adverse effects related to corticosteroid use usually depend on the dose administered and the duration of therapy.[30943][50600]
Oral inhaled corticosteroids are believed to reduce the immediate and late-phase allergic responses associated with allergies and chronic bronchial asthma. Proposed mechanisms of action include decreased IgE synthesis, increased number of beta-adrenergic receptors on leukocytes, and decreased arachidonic acid metabolism (which decreases the amount of prostaglandins and leukotrienes released). During an immediate allergic reaction, allergens bridge the IgE antibodies on the surface of mast cells, triggering these cells to release chemotactic substances. Mast cell influx and activation, therefore, is partially responsible for the inflammation and hyperirritability of the oral mucosa. This inflammation can be retarded by administration of adrenocorticoids. Intranasal budesonide provides relief of such symptoms as watery rhinorrhea, nasal congestion, postnasal drip, sneezing, and pharyngeal itching.[30943]
Oral budesonide is a controlled-release formulation that delivers drug locally to disease sites in the terminal ileum and ascending colon. The potential for reduced toxicity results from extensive first pass metabolism of budesonide that lowers systemic bioavailability and subsequently, the frequency of corticosteroid adverse reactions.[34979]
Oral budesonide, when used to treat primary immunoglobulin A nephropathy (IgAN), can modulate the numbers and activity of mucosal B-cells present in the ileum, including the Peyer's patches, through its anti-inflammatory and immunosuppressive effects at the glucocorticoid receptor. These B-cells express glucocorticoid receptors and are responsible for the production of galactose-deficient IgA1 antibodies (Gd-Ag1) causing IgA nephropathy. It has not been established to what extent oral budesonide's efficacy is mediated via local effects in the ileum versus systemic effects.[67192]
The precise mechanism of corticosteroid action on inflammation in eosinophilic esophagitis (EoE) is not known. Corticosteroids have a wide range of inhibitory activities against multiple cell types and mediators involved in allergic inflammation.[70334]
Revision Date: 10/15/2025, 01:33:00 AMBudesonide is administered orally, by nasal inhalation, by oral inhalation, and by nebulization. The volume of distribution is approximately 2 to 4 L/kg. The mean volume of distribution of oral budesonide suspension is 1,886 L. The drug is roughly 85% to 90% bound to plasma proteins. Protein binding is constant over the concentration range (1 to 230 nmol/L or 0.43 to 99 ng/mL). Budesonide shows little or no binding to corticosteroid binding globulin and the drug rapidly equilibrates with red blood cells in a concentration independent manner with a blood/plasma ratio of about 0.8. Limited data show distribution into breast milk of 0.39 and 0.78 nmol/L after dry powder oral inhalational administration of 400 mcg/day or 800 mcg/day, respectively. In vitro data show that metabolism occurs rapidly and primarily via CYP3A4. Oral budesonide has a high plasma clearance, 0.9 to 1.8 L/minute approaching the estimated liver blood flow, suggesting the budesonide is a high hepatic clearance medication. Budesonide undergoes approximately 80% to 90% first-pass metabolism to two inactive metabolites: 16-alpha-hydroxyprednisolone (24%) and 6-beta-hydroxybudesonide (5%). Budesonide is excreted in urine and feces in the form of metabolites. The plasma elimination half-life, after administration of intravenous doses or oral budesonide suspension, ranges between 2 and 3.6 hours. The half-life of oral budesonide delayed release capsules is 5 to 6.8 hours.[31824][34979][34376][33486][52910][58166][64318][67192][70334]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4, P-glycoprotein (P-gp)
In vitro data show that metabolism of budesonide occurs primarily by CYP3A4. Inhibitors of CYP3A4 may increase budesonide exposure and, conversely, CYP3A4 inducers may reduce budesonide plasma levels. Budesonide is also a substrate and inhibitor of P-glycoprotein transport.[34354][31824][34979][34376][33486][52910][64318][67192]
Intranasal Route
Intranasal Administration (Rhinocort Aqua): Compared to budesonide administered intravenously, approximately 34% of an intranasal dose reaches the systemic circulation via the nasal mucosa. After nasal administration of a single dose (128 mcg), the mean peak plasma concentration of approximately 0.3 nmol/L occurs about 0.5 hours post-dose.[31824]
Rectal Route
In a population pharmacokinetic analysis in patients with distal ulcerative colitis, the estimated exposure (AUC) following administration of budesonide rectal foam (Uceris) 2 mg rectally twice daily was 4.31 ng x hour/mL with a CV of 64% in the target patient population.[58166]
Reduced liver function may affect the elimination of corticosteroids.[31824][33486] Systemic exposure of orally administered budesonide increases up to 3.5-fold in patients with moderate liver impairment or with hepatic cirrhosis compared to healthy controls while patients with mild hepatic impairment had an approximately 1.4 fold-higher AUC. The Cmax values demonstrated similar increases. Patients with mild liver disease appear to be minimally affected.[34979][52910][64318][67192]
Patients with severe renal disease have not been evaluated. Intact budesonide is not excreted renally. Although budesonide metabolites are renally excreted (60%), their activity is negligible. An enhanced risk of adverse effects in renally compromised patients is not expected.[34979][52910][58166][67192]
Some differences have been noted between budesonide pharmacokinetics in pediatric and adult patients; these differences vary by dosage formulation. The plasma half-life may be slightly shorter in pediatric patients aged 10 to 14 years (1.5 hours) versus adult patients (2 hours) after receiving intravenous budesonide.
The pharmacokinetic parameters of budesonide in geriatric patients have not been assessed. No differences in safety or efficacy due to age have been identified.[31824][34979][34376][67192]
No differences in pharmacokinetics of budesonide due to gender have been identified.[31824][34979][34376][67192]
No differences in pharmacokinetics of budesonide due to race have been identified.[33486][67192]
Studies of pregnant women have not shown that inhaled budesonide increases the risk of abnormalities when administered during pregnancy.[31824] [33486] [34376] [46711] A review of Swedish registries of more than 2,000 births indicated that no increased risk for congenital malformations during early pregnancy with budesonide inhalation powder or solution.[46713] Despite adverse effects in animal studies, fetal harm appears remote. Corticosteroid treatment may not be necessary during pregnancy due to a natural increase in corticosteroid production; however, poorly controlled maternal asthma also poses risk to the mother and the fetus. Low-dose inhaled corticosteroids are considered first-line therapy for control of mild persistent asthma during pregnancy according to the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group; of the inhaled corticosteroids, more data are available for budesonide use in pregnancy. Data on the use of medium- to high-dose inhaled corticosteroid use during pregnancy are limited. However, dose titration may be considered for those with moderate to severe persistent asthma, preferably using budesonide. However, there are no data to indicate safety concerns with other inhaled corticosteroids, and maintaining a previously established treatment regimen may be more beneficial to the patient.[31822] Selection of any pharmacologic treatment for asthma control during pregnancy should include the specific needs of the patient, based on an individual evaluation, and consideration of the potential benefits or risks to the fetus. A position statement by the American College of Allergy, Asthma and Immunology also considers budesonide a good choice for pregnant women requiring high doses of inhaled steroids for effective asthma management.[46717] Limited published studies report on the use of oral budesonide in pregnant patients; however, the data are insufficient to inform a drug-associated risk of major birth defects and miscarriage. Oral budesonide products (e.g., Entocort EC, Ortikos, Uceris, Tarpeyo) have been teratogenic and embryocidal in animal studies. At subcutaneous budesonide doses that were 0.3 to 0.5 or 0.03 to 0.05 times the maximum recommended human dose (MRHD) in pregnant rats and rabbits, respectively, fetal loss, decreased pup weights, and skeletal anomalies occurred. There is a natural increase in endogenous corticosteroid production during pregnancy, and many women will require a lower exogenous dose or no corticosteroid treatment at all during pregnancy. Oral budesonide (e.g., Entocort EC, Ortikos, Uceris, Eohilia, Tarpeyo) products should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus. Some studies show an association of adverse pregnancy outcomes in women with Crohn's disease with increased disease activity (increased stool activity and abdominal pain) which can lead to preterm birth and low birth weight infants. Counsel the patients about the importance of controlling the disease.[34979] [64318] IgA nephropathy in pregnancy is associated with adverse maternal outcomes, including increased rates of cesarean section, pregnancy-induced hypertension, pre-eclampsia and preterm delivery, and adverse fetal/neonatal outcomes, including stillbirth and low birth weight. Hypoadrenalism may occur in an infant born to a mother receiving corticosteroids during pregnancy, and the infant should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting.[34979] [52910] [64318] [67192] [70334]
Oral, nasal, rectal, and inhaled forms of budesonide are compatible with breast-feeding. The amount of infant exposure from use of inhaled budesonide by the breast-feeding parent is negligible. Budesonide is excreted into breast milk in small amounts with a relative infant dose (RID) of 0.3%. In addition, budesonide has an oral bioavailability of 10.7%, further limiting total infant exposure.[70364] [70365] Based on data from a small number (n = 8) of breast-feeding women taking inhaled dry powder budesonide 200 to 400 mcg twice daily, approximately 0.3% to 1% of the dose inhaled by the mother is available via breast milk to an exclusively breast-fed infant. Budesonide plasma concentrations obtained in five of the infants in this study about 140 minutes after maternal drug administration and 90 minutes after breast-feeding were below quantifiable levels.[33725] Low-dose inhaled corticosteroids are considered first line therapy for control of mild persistent asthma during pregnancy and lactation according to the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group. Due to greater availability of data, budesonide is considered the preferred agent in this population.[31822] Reviewers and an expert panel consider all inhaled corticosteroids acceptable to use during breast-feeding.[33723] [33724] [31822] Single- and repeated-dose pharmacokinetic studies have shown that maximum plasma budesonide concentrations after a 9 mg oral daily dose are up to 10-times greater than the concentrations measured after inhaled doses of 400 to 800 mcg/day. Assuming that the coefficient of extrapolation between inhaled and oral doses is constant across all doses, it is possible that budesonide exposure to breast-feeding infants after maternal oral ingestion may be up to 10-times higher than exposure to infants after maternally inhaled budesonide.[34979] [52910]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.