ThisiscontentfromElsevier'sDrugInformation
Budesonide; formoterol
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
160 mcg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) or 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth twice daily. Base starting dose on prior asthma therapy and disease severity. Max: 640 mcg budesonide/18 mcg formoterol/day.[32950] [72049]
160 mcg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) or 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth twice daily. Base starting dose on prior asthma therapy and disease severity. Max: 640 mcg budesonide/18 mcg formoterol/day.[32950] [72049]
160 mcg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth twice daily. Max: 320 mcg budesonide/18 mcg formoterol/day.[32950] [72049]
160 mcg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) or 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth once or twice daily. When used as both controller and reliever therapy, the maximum formoterol dose is 54 mcg/day.[66299]
160 mcg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) or 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth once or twice daily. When used as both controller and reliever therapy, the maximum formoterol dose is 54 mcg/day.[66299]
200 mcg budesonide/6 mcg formoterol (1 actuation of 200 mcg budesonide/6 mcg formoterol/actuation, which delivers 80 mcg budesonide/4.5 mcg formoterol per actuation) inhaled by mouth once or twice daily, depending on asthma severity, plus 1 inhalation whenever needed. When used as both a controller and a reliever therapy, the maximum formoterol dose is 72 mcg/day (12 actuations of 200/6 inhaler strength).[69016]
200 mcg budesonide/6 mcg formoterol (1 actuation of 200 mcg budesonide/6 mcg formoterol/actuation, which delivers 80 mcg budesonide/4.5 mcg formoterol per actuation) inhaled by mouth once or twice daily, depending on asthma severity, plus 1 inhalation whenever needed. When used as both a controller and a reliever therapy, the maximum formoterol dose is 72 mcg/day (12 actuations of 200/6 inhaler strength).[69016]
100 mcg budesonide/6 mcg formoterol (1 actuation of 100 mcg budesonide/6 mcg formoterol/actuation, which delivers 80 mcg budesonide/4.5 mcg formoterol per actuation) inhaled by mouth once or twice daily, depending on asthma severity, plus 1 additional inhalation whenever needed. Max: 48 mcg formoterol/day when used as both controller and reliever therapy (8 actuations of 100/6 inhaler strength).[69016]
160 mg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) to 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth as needed in addition to a daily maintenance dose; may repeat dose after 5 minutes if needed. Max: 54 mcg/day of formoterol (12 actuations/day of 4.5 mcg formoterol/actuation).[66299]
160 mg budesonide/9 mcg formoterol (2 actuations of 80 mcg budesonide/4.5 mcg formoterol/actuation) to 320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth as needed in addition to a daily maintenance dose; may repeat dose after 5 minutes if needed. Max: 54 mcg/day of formoterol (12 actuations/day of 4.5 mcg formoterol/actuation).[66299]
200 mcg budesonide/6 mcg formoterol (1 actuation of 200 mcg budesonide/6 mcg formoterol/actuation which delivers 160 mcg budesonide/4.5 formoterol per actuation) inhaled by mouth whenever needed. May provide as anti-inflammatory reliever (AIR) therapy alone or as part of maintenance-and-reliever therapy (MART). Max: 72 mcg/day formoterol, inclusive of reliever and controller therapy (12 actuations of 200/6 inhaler strength).[69016]
200 mcg budesonide/6 mcg formoterol (1 actuation of 200 mcg budesonide/6 mcg formoterol/actuation which delivers 160 mcg budesonide/4.5 formoterol per actuation) inhaled by mouth whenever needed. May provide as anti-inflammatory reliever (AIR) therapy alone or as part of maintenance-and-reliever therapy (MART). Max: 72 mcg/day formoterol, inclusive of reliever and controller therapy (12 actuations of 200/6 inhaler strength).[69016]
100 mcg budesonide/6 mcg formoterol (1 actuation of 100 mcg budesonide/6 mcg formoterol/actuation which delivers 80 mcg budesonide and 4.5 mcg formoterol per actuation) inhaled by mouth whenever needed. Use only as part of a maintenance-and-reliever therapy (MART) regimen. There is inconclusive evidence for using it as an anti-inflammatory reliever (AIR) therapy only in this age group. Max: 48 mcg/day formoterol, inclusive of controller and reliever therapy (8 actuations of 100/6 inhaler strength).[69016]
160 mcg budesonide/4.5 mcg formoterol (1 actuation of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth 5 to 20 minutes before exercise.[56291] [64814] [69016]
320 mcg budesonide/9 mcg formoterol (2 actuations of 160 mcg budesonide/4.5 mcg formoterol/actuation) inhaled by mouth twice daily is the recommended and max dosage.[32950] [72049] Do not use other long-acting beta-agonists (LABAs) concurrently. If taking oral corticosteroids, wean the OCS slowly after transferring to budesonide; formoterol by reducing the daily dose by 2.5 mg prednisone or equivalent on a weekly basis.[32950] [72049]
FDA labeled maximum is 640 mcg of budesonide and 18 mcg of formoterol via oral inhalation/day (4 inhalations/day of FDA-approved products containing 160 mcg budesonide and 4.5 mcg formoterol per actuation). GINA guidance (off-label) for maintenance and reliever therapy (MART) regimens recommends not to exceed 72 mcg/day of formoterol via oral inhalation. NAEPP (off-label) recommends not exceeding 54 mcg/day of formoterol for MART therapy.
FDA labeled maximum is 640 mcg of budesonide and 18 mcg of formoterol via oral inhalation/day (4 inhalations/day of FDA-approved products containing 160 mcg budesonide and 4.5 mcg formoterol per actuation). GINA guidance (off-label) for maintenance and reliever therapy (MART) regimens recommends not to exceed 72 mcg/day of formoterol via oral inhalation. NAEPP (off-label) guidance differs, and recommends not exceeding 54 mcg/day of formoterol for MART therapy.
FDA labeled maximum is 640 mcg of budesonide and 18 mcg of formoterol via oral inhalation/day (4 inhalations/day of FDA-approved products containing 160 mcg budesonide and 4.5 mcg formoterol per actuation). GINA guidance (off-label) for maintenance and reliever therapy (MART) regimens recommends not to exceed 72 mcg/day of formoterol via oral inhalation. NAEPP (off-label) guidance differs, and recommends not exceeding 54 mcg/day of formoterol for MART therapy.
12 years: FDA labeled maximum is 640 mcg of budesonide and 18 mcg of formoterol via oral inhalation/day (4 inhalations/day of FDA-approved products containing 160 mcg budesonide and 4.5 mcg formoterol per actuation). GINA guidance (off-label) for maintenance and reliever therapy (MART) regimens recommends not to exceed 72 mcg/day of formoterol via oral inhalation. NAEPP (off-label) guidance differs, and recommends not exceeding 54 mcg/day of formoterol for MART therapy.
6 to 11 years: FDA labeled maximum is 320 mcg of budesonide and 18 mcg of formoterol via oral inhalation/day (4 inhalations/day of FDA-approved products containing 80 mcg budesonide and 4.5 mcg formoterol per actuation). GINA guidance (off-label) for maintenance and reliever therapy (MART) recommends not to exceed 48 mcg/day of formoterol via oral inhalation. NAEPP has not provided MART dosing guidance for this age group.
1 to 5 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication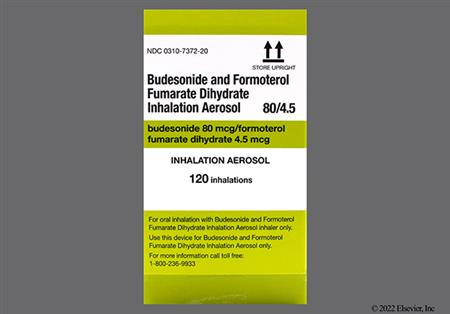


Budesonide; formoterol is a combination of an inhaled corticosteroid (ICS), budesonide, and a long-acting beta-2 agonist (LABA), formoterol. It is administered by oral inhalation twice daily. The combination is indicated for the maintenance treatment of asthma in adult and pediatric patients 6 years and older. Budesonide; formoterol is also indicated for the maintenance treatment of chronic obstructive pulmonary disease (COPD) in adults and to reduce the risk of exacerbations of COPD.[32950][72049] According to the FDA-approved label, budesonide; formoterol is not recommended for acute bronchospasm or acute asthmatic attacks.[32950][32953][72049] However, guidelines have promoted the use of "MART" (maintenance-and-reliever therapy) inhaler dosing strategies for ICS-formoterol and the data are strongest for the budesonide-formoterol inhalers. Budesonide; formoterol may also be used alone for mild asthma (step 1 and 2) in people 12 years and older as antiinflammatory reliever (AIR) therapy. AIR therapy with budesonide-formoterol is more effective than as-needed short-acting beta agonists (SABAs) at reducing severe exacerbations and emergency department visits/hospitalizations in these populations.[69016][66299] According to COPD guidelines, budesonide; formoterol is an option for those patients with stable disease who are already receiving this therapy with no major symptoms or exacerbations. Escalation to triple therapy with an ICS + LABA + long-acting muscarinic antagonist (LAMA) should be considered for COPD patients who have further exacerbations or major symptoms. Budesonide; formoterol may also be appropriate for those patients in areas with limited access to triple therapy. Patients with COPD who have concomitant asthma should be treated with an ICS as part of their COPD regimen.[69470]
For storage information, see the specific product information within the How Supplied section.
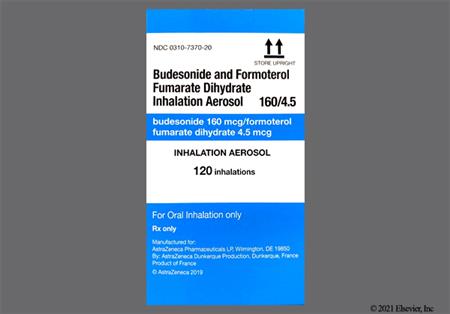
Aerosol pressurized metered-dose Inhalers (pMDIs, e.g., Symbicort, Breyna)
The safety of budesonide; formoterol metered-dose inhaler aerosol (MDI) for asthma was studied in people 12 years or older in three 12-week controlled clinical trials. Studies used the 2 available U.S. strengths of budesonide; formoterol MDI 80/4.5 mcg and 160/4.5 mcg, respectively. The most commonly reported adverse reactions (occurring in 3% or more of recipients) in the 2 dosing groups and at increased incidence vs. placebo included: back pain (3.2%, 1.6%), headache (6.5%, 11.3%), influenza (3.2%, 2.4%), nasal congestion (2.5%, 3.2%), naso-pharyngitis (10.5%, 9.7%), vomiting (1.4%, 3.2%), pharyngo-laryngeal pain (6.1%, 8.9%), sinusitis (5.8%, 4.8%), stomach discomfort (1.1%, 6.5%), and upper respiratory tract infection (7.6%, 10.5%). The safety profile in pediatric patients 6 to 11 years old with asthma was similar to older recipients and side effects occurring in 3% or more of recipients included upper respiratory tract infection, pharyngitis, headache, and rhinitis. In clinical trials for COPD, the most commonly reported adverse reactions (incidence of 3% or more) included naso-pharyngitis (7.3%), bronchitis (5.4%), sinusitis (3.5%), and viral respiratory tract infection (3.5%). Lung infections other than pneumonia (mostly bronchitis) occurred in 7.9% of active MDI recipients. Other adverse reactions reported with budesonide; formoterol MDI use include nausea, muscle cramps, tremor, dizziness, dysphonia, cough, and throat irritation.[32950] [72049]
Budesonide; formoterol, like other products containing inhaled beta-2 agonists, can produce life-threatening paradoxical bronchospasm. In the event of a paradoxical bronchospasm, discontinue budesonide; formoterol immediately and initiate an alternative therapy. Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs in patients with asthma. The exact cause of death is unknown, but cardiac arrest after an unexpected development of a severe acute asthmatic crisis and subsequent hypoxia is suspected.[32950] [72049]
An increase in the need for rescue inhaler use and/or worsening wheezing may occur during therapy with budesonide; formoterol and are symptoms of a deterioration of the underlying respiratory condition, a potentially life-threatening condition. Advise patients not to exceed recommended doses of this medicine, but instead, seek immediate medical attention if such symptoms occur.[32950] [72049] When long-acting beta agonists (LABAs) such as formoterol are used in fixed-dose combination with ICS, data from large clinical trials do not show a significant increase in the risk of serious asthma-related events (hospitalizations, intubations, death) compared with ICS alone.[62717] The use of a LABA as monotherapy to treat asthma, without inhaled corticosteroids [ICS], is associated with an increased risk of asthma-related death. Available data from controlled clinical trials also suggest that use of LABA as monotherapy increases the risk of asthma-related hospitalization in pediatric and adolescent patients.[37481] [41282] These findings are considered a class effect of LABA monotherapy. In most cases, serious acute respiratory events have occurred in patients with severe asthma and/or in patients in whom asthma has been acutely deteriorating, but such events have also occurred in patients with less severe asthma. These findings pertain only to patients who have asthma.[32950] [72049]
Immediate and delayed hypersensitivity reactions, including anaphylactoid reactions, angioedema, bronchospasm, urticaria, exanthema, dermatitis, and pruritus have been reported with budesonide; formoterol use.[32950] [72049]
Formoterol, like other beta2-agonists and sympathomimetic amines, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate (sinus tachycardia), systolic or diastolic blood pressure (hypertension), and/or symptoms or cardiac arrhythmias, such as supraventricular tachycardia (SVT) and extrasystoles (palpitations). Although such effects are uncommon after administration of formoterol at recommended doses, if such effects occur then budesonide; formoterol may need to be discontinued. Beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, QT prolongation, and ST segment depression; the clinical significance of these findings is unknown. Beta2-agonist medications may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation. During long-term safety studies in adolescent and adult patients 12 years of age and older, treated for up to 1 year, no significant or unexpected chemistry, ECG, or Holter monitor assessments occurred. During postmarketing experience, angina pectoris, cardiac arrhythmias (e.g., atrial fibrillation, ventricular extrasystoles, and tachyarrhythmias), palpitations, QT interval prolonged on ECG, increased blood pressure, including hypertension, hypotension, and hypokalemia have been reported with formoterol; budesonide or other products containing formoterol.[32950] [72049]
Orally inhaled budesonide; formoterol has a relatively low risk of hypothalamic-pituitary-adrenal (HPA) suppression when used at recommended doses. Pharmacologic doses of budesonide administered for prolonged periods may, however, result in adrenocortical insufficiency.[32950] [72049] Adrenal suppression and increased intracranial pressure have been reported with the use and/or withdrawal of orally inhaled steroids in pediatric patients.[51792] Local immunosuppression associated with inhaled budesonide use may be manifested as an overgrowth of fungus in the nose, mouth, and throat. Oral candidiasis (thrush) is a well-known adverse reaction of oral inhalation steroid therapy and occurred in 1.4% to 6% of adult patients receiving inhaled budesonide; formoterol during clinical trials.[32950] [72049] Patients who have been previously maintained on 20 mg or more of prednisone (or its equivalent) may be most susceptible, particularly if the systemic corticosteroid has been almost completely discontinued. During this period of HPA suppression, patients may exhibit signs and symptoms of adrenal insufficiency when exposed to stressors such as trauma, surgery, or infectious disease (particularly gastroenteritis), or other conditions associated with severe electrolyte loss. Inhaled corticosteroids provide inadequate systemic glucocorticoid and mineralocorticoid activity for emergencies. Instruct patients to resume oral corticosteroid during severe stress, COPD exacerbation, or asthma attack, and contact their care team.[32950] [72049]
Growth inhibition has been observed in some children following therapy with orally inhaled corticosteroids including budesonide. Growth inhibition has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA) suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients. With orally inhaled corticosteroids, the mean reduction in growth velocity is approximately one centimeter per year (range 0.3 to 1.8 cm per year) and appears to be related to the dose and duration of exposure. In general, the benefits of regular inhaled corticosteroid (ICS) use outweigh the potential risk of relatively small and non-cumulative growth suppression in children with asthma; however, growth should be monitored.[57670] Further study is needed to determine the long-term effects of growth velocity reduction in children, including the impact on final adult height. To minimize the effects of inhaled corticosteroids, each patient should be titrated to the lowest effective dose.[32950] [72049]
Corticosteroids, even orally inhaled doses like budesonide, can induce cataracts and have the potential to induce or worsen ocular hypertension (glaucoma). Although rarely reported during treatment with budesonide; formoterol, patients are encouraged to keep up with routine ophthalmological exams.[32950] [72049]
Behavior disturbances, sleep disturbances, agitation, depression, nervousness, restlessness, and skin bruising (ecchymosis) have been reported with postmarketing use of budesonide; formoterol.[32950] [72049]
Prolonged use (e.g., more than 1 year) of high doses of inhaled corticosteroids, like budesonide, especially when used in combination with frequent courses of systemic corticosteroids, may be associated with reduced bone mineral density (BMD), which may increase the risk of osteopenia or osteoporosis. The clinical significance of small changes in BMD with regard to long-term outcomes, such as fracture, is unknown.[32950] [72049]
Clinically significant changes in blood glucose were seen infrequently during clinical studies with budesonide; formoterol at recommended doses. Hyperglycemia has been reported postmarketing.[32950] [72049]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Budesonide; formoterol is contraindicated for primary treatment of status asthmaticus or other rapidly deteriorating or life-threatening asthma or COPD episodes. Do not initiate or use as reliever therapy for acute symptoms or exacerbations; these require an inhaled short-acting beta agonist (SABA). Increasing SABA use indicates poor control and requires prompt reassessment of the treatment regimen.[32950][41230][62717][72049]
Formoterol, like other beta2-agonists and sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency (coronary artery disease), cardiac arrhythmias, and hypertension. Formoterol can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic or diastolic blood pressure, and cardiac arrhythmias, such as supraventricular tachycardia and extrasystoles. If such effects occur, budesonide; formoterol inhalation may need to be discontinued. In addition, beta-agonists have been reported to produce electrocardiographic changes, such as flattening of the T wave, QT prolongation, and ST segment depression, although the clinical significance of these findings is unknown. Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs. Beta-adrenergic agonist therapies like formoterol may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation.[32950] [72049]
Budesonide; formoterol should be used with caution in people with diabetes mellitus because corticosteroids and beta-2 agonists may aggravate preexisting diabetes mellitus and diabetic ketoacidosis in some patients.[32950] [72049]
Budesonide; formoterol should be used cautiously in patients with glaucoma, cataracts, or other visual disturbance or with a family history of glaucoma. Rare instances of glaucoma, increased intraocular pressure, and cataracts have been reported following the inhaled administration of corticosteroids, including budesonide. Close monitoring of these individuals is warranted.[32950] [72049]
Budesonide; formoterol should be used with caution in patients with hyperthyroidism, a history of seizure disorder, or other unusual responsiveness to sympathomimetic amines.[32950] [72049]
Although inhaled budesonide; formoterol is absorbed systemically to a lesser extent than other corticosteroids, significant amounts can be absorbed when large doses are administered. This can increase the risk for infection. In general, inhaled corticosteroid therapy used with caution, if at all, in patients with active or quiescent tuberculosis infections of the respiratory tract; untreated systemic fungal infection, bacterial infection, viral infection, or a parasitic infection, especially those not adequately controlled by anti-infective agents. Inhaled corticosteroids should be used cautiously, if at all, in patients with an active herpes infection (including ocular herpes simplex). If a patient on immunosuppressant doses of corticosteroids is exposed to chickenpox, therapy with varicella-zoster immune globulin or pooled intramuscular immunoglobulin may be indicated. If a patient is exposed to measles, prophylaxis with pooled intramuscular immunoglobulin may be indicated. Budesonide oral inhalation has been associated with the development of localized infection with Candida albicans in the nose, mouth, and pharynx. If this develops, discontinuation of inhaled budesonide is warranted, and appropriate local therapy should be instituted. Patients who are on long-term budesonide inhalation therapy should receive a periodic evaluation for Candida infection or other adverse effects.[32950] [72049]
Long-term use of orally inhaled corticosteroids, such as budesonide, may affect normal bone metabolism resulting in a loss of bone mineral density or osteopenia. Use budesonide; formoterol with caution in patients with increased risk for osteoporosis such as tobacco use, advanced age, sedentary lifestyle, poor nutrition, family history of osteoporosis, or chronic use of drugs that decrease bone mass. Monitor and treat such patients with the established standards of care.[32950] [72049]
Formal pharmacokinetic studies using budesonide; formoterol inhalation have not been conducted in patients with hepatic impairment. However, since budesonide and formoterol are predominantly cleared by hepatic metabolism, hepatic failure may lead to increased exposure of budesonide and formoterol. Therefore, patients with severe hepatic disease should be closely monitored.[32950] [72049]
There are no adequate and well-controlled studies of budesonide; formoterol during human pregnancy; however, studies of pregnant women taking inhaled budesonide alone have not shown increases in the risk of abnormalities when given during pregnancy. In animal studies, formoterol fumarate has only shown adverse effects when administered systemically at high systemic exposures greatly exceeding the maximum recommended human daily inhalational dose (MRHDID). No teratogenic, embryocidal, or developmental effects were seen in rats that received formoterol inhalation doses up to 375 times the MRHDID. Women with asthma who become pregnant while stabilized on budesonide; formoterol therapy should discuss their asthma management with a qualified health care professional. A review of Swedish registries indicated that in over 2,000 births there was no increased risk for congenital malformations during early pregnancy with budesonide inhalation powder or solution.[32950] [72049] It is known that improved maternal and perinatal outcomes are achieved with optimal control of asthma during pregnancy.[45934] Large studies of women with asthma have confirmed the lack of relationship between the use of inhaled beta-2 agonists and adverse maternal or fetal outcomes; however, less data are available for long-acting beta agonists (LABAs) such as formoterol vs. short-acting beta agonists (SABAs).[45934] However, most inhaled beta-2 agonists, as well as inhaled budesonide, are considered acceptable for use during pregnancy because of the low bioavailability and maternal serum levels after use.[45934] [49764] [63021] According to the 2004 guidelines of the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group, long-acting beta-2 agonists (LABAs), in combination with inhaled corticosteroids (ICS), are one of the preferred treatment options for the long-term control of moderate asthma during pregnancy and lactation; use of medium dose ICS is also a preferred option. Although a preferred LABA is not recommended, the guideline states that more experience is available with salmeterol. Due to the availability of safety information during pregnancy, budesonide is preferred over other ICS.[45934] Infants born to mothers taking substantial corticosteroid doses during pregnancy should be monitored for signs of hypoadrenalism. There are no well-controlled human studies that have investigated the effects of budesonide; formoterol on preterm labor or labor at term. Because of the potential for beta-2 agonist interference with uterine contractility, use of budesonide; formoterol should be restricted to those patients in whom the benefits clearly outweigh the risks.[32950] [72049]
There are no well-controlled human studies of budesonide; formoterol during breast-feeding. Formoterol was excreted in milk in reproductive studies in rats; however, it is unknown whether formoterol is excreted in human milk. Glucocorticoids, such as budesonide, are excreted into human breast milk. Data from a small number (n = 8) of lactating women showed an estimated oral daily dose of budesonide available to the nursing infants which was approximately 0.3% to 1% of the dose inhaled by the mothers. Budesonide plasma concentrations obtained in five of the infants at about 140 minutes after drug administration to the mother and 90 minutes after breast-feeding were below quantifiable levels.[32950] [72049] The amount of inhaled budesonide excreted in breast-milk is minute, and infant exposure is negligible. While not measured, the amount of formoterol absorbed into the maternal bloodstream and excreted into breast-milk after inhalation is expected to be very low; therefore, it is unlikely that nursing infants would be exposed to clinically significant amounts of formoterol via breast milk. Most inhaled bronchodilators are considered acceptable for use during the postpartum period and breast-feeding because of the low bioavailability and maternal serum levels after use.[45934] [63021] The 2004 guidelines of the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group consider a combination of inhaled corticosteroids with long-acting inhaled beta-2 agonists (LABAs) a preferred treatment option for moderate asthma in pregnancy and lactation.[45934]
Budesonide is an antiinflammatory corticosteroid and formoterol is a long-acting, selective beta-agonist; when used together, the combination is more effective than either drug alone.[32950][72049]
Budesonide: In the treatment of asthma, orally inhaled corticosteroids (ICS) are believed to reduce the immediate and late-phase allergic responses associated with allergies and chronic bronchial asthma. Mediators involved in the pathogenesis of asthma include histamine, leukotrienes (slow releasing substance of anaphylaxis, SRS-A), eosinophil chemotactic factor of anaphylaxis (ECF-A), neutrophil chemotactic factor (NCF), cytokines, hydroxyeicosatetraenoic acids, prostaglandin-generating factor of anaphylaxis (PGF-A), prostaglandins, major basic protein, bradykinin, adenosine, peroxides, and superoxide anions. Different cell types are responsible for the release of these mediators, including airway epithelium, eosinophils, basophils, lung parenchyma, lymphocytes, macrophages, mast cells, neutrophils, and platelets. ICS inhibits the release of these mediators as well as inhibit IgE synthesis, attenuate mucous secretion and eicosanoid generation, up-regulate beta-receptors, promote vasoconstriction, and suppress inflammatory cell influx and inflammatory processes. Clinical effects of ICS in treating asthma include a reduction in bronchial hyperresponsiveness to allergens, a decreased number of asthma exacerbations, and an improvement in forced expiratory volume in 1 second (FEV1), peak-flow rate, and respiratory symptoms.
Formoterol: Similar to other beta-2 agonists, formoterol's mechanism of action involves stimulation of adenyl cyclase leading to the production of cyclic adenosine monophosphate (cAMP) via adenosine triphosphate (ATP). Increased levels of cAMP result in relaxation of the bronchial smooth muscle.Formoterol, like salmeterol, is highly lipophilic. It enters the plasma cell membrane in the form of a depot and is gradually released into the aqueous phase to react with the beta-2 receptor, resulting in a long duration of action. The aqueous phase activity, not demonstrated by salmeterol, is responsible for the rapid onset of action of formoterol. Formoterol has more than a 200-fold greater agonist activity at beta-2 receptors (primarily in the lung) than at beta-1 receptors (primarily in the heart). However, 10% to 50% of the beta receptors in the heart are beta-2 receptors and raise the possibility that even highly selective beta-2 receptor agonists may have adverse cardiovascular effects, such as tachycardia, palpitations, and ischemia. As with other beta-2 agonists, formoterol may possess antiinflammatory activity, but the clinical significance of this effect is unknown.[26424] In vitro studies have demonstrated inhibition of mast cell mediators, such as histamine and leukotrienes, from the human lung.
Revision Date: 10/15/2025, 01:33:00 AMBudesonide; formoterol is administered via oral inhalation. After systemic absorption of the drugs following oral inhalation from the aerosol metered dose inhaler (MDI), the distribution, metabolism and excretion data are as follows:[32950][72049]
Affected Cytochrome P450 isoenzymes and drug transporters: CYP3A4
The main route of metabolism of corticosteroids, including budesonide, is via CYP3A4. After oral administration of a strong inhibitor of CYP3A4, the mean plasma concentration of orally administered budesonide increased. Caution should be exercised when considering the long-term coadministration of strong CYP3A4 inhibitors with budesonide; formoterol.[32950][72049]
Budesonide; formoterol aerosol inhalation is delivered by metered dose inhaler (MDI) via oral inhalation. Absorption pharmacokinetics in healthy subjects are below; Studies in both subjects with asthma and those with COPD have also been performed and are described extensively in the manufacturer labels.[32950][72049]
There are no specific pharmacokinetic data for budesonide; formoterol aerosol inhaler in patients with hepatic impairment. Reduced liver function may affect the elimination of corticosteroids. Budesonide pharmacokinetics was affected by compromised liver function as evidenced by a doubled systemic availability after oral ingestion. The intravenous budesonide pharmacokinetics was, however, similar in patients with cirrhosis and in healthy subjects. Specific data with formoterol is not available, but because formoterol is primarily eliminated via hepatic metabolism, an increased exposure can be expected in people with severe liver impairment.[32950][72049]
No specific data are available regarding the pharmacokinetics of budesonide; formoterol aerosol inhaler in patients with renal impairment.[32950][72049]
Plasma concentrations of budesonide were measured following administration of 4 inhalations of budesonide; formoterol inhaler 160/4.5 strength in a single-dose study in pediatric patients with asthma, 6 to less than 12 years of age. Peak budesonide concentrations of 1.4 nmol/L occurred at 20 minutes post-dose. This study also demonstrated that the total systemic exposure to budesonide from the aerosol inhaler was approximately 30% lower than from inhaled budesonide via a dry powder inhaler that was also evaluated at the same delivered dose. The dose-normalized Cmax and AUC0-inf of budesonide following single dose inhalation in children 6 to less than 12 years of age were numerically lower than that observed in adults. Following 2 inhalations of budesonide; formoterol aerosol inhaler 160/4.5 twice daily treatment, formoterol Cmax and AUC0-6 at steady state in children 6 to less than 12 years of age were comparable to that observed in adults.[32950][72049]
Pharmacokinetic parameters have not been specifically studied in geriatric adults.[32950][72049]
Specific studies to examine the effects of gender on the pharmacokinetics of budesonide; formoterol have not been conducted. Population pharmacokinetic analysis of budesonide; formoterol inhaler pharmacokinetic data indicates that gender does not affect the pharmacokinetics of budesonide and formoterol.[32950][72049]
Specific studies to examine the effects of race on the pharmacokinetics of budesonide; formoterol have not been conducted. No conclusions can be drawn on the effect of race due to the low number of non-Caucasians evaluated for pharmacokinetic studies..[32950][72049]
There are no adequate and well-controlled studies of budesonide; formoterol during human pregnancy; however, studies of pregnant women taking inhaled budesonide alone have not shown increases in the risk of abnormalities when given during pregnancy. In animal studies, formoterol fumarate has only shown adverse effects when administered systemically at high systemic exposures greatly exceeding the maximum recommended human daily inhalational dose (MRHDID). No teratogenic, embryocidal, or developmental effects were seen in rats that received formoterol inhalation doses up to 375 times the MRHDID. Women with asthma who become pregnant while stabilized on budesonide; formoterol therapy should discuss their asthma management with a qualified health care professional. A review of Swedish registries indicated that in over 2,000 births there was no increased risk for congenital malformations during early pregnancy with budesonide inhalation powder or solution.[32950] [72049] It is known that improved maternal and perinatal outcomes are achieved with optimal control of asthma during pregnancy.[45934] Large studies of women with asthma have confirmed the lack of relationship between the use of inhaled beta-2 agonists and adverse maternal or fetal outcomes; however, less data are available for long-acting beta agonists (LABAs) such as formoterol vs. short-acting beta agonists (SABAs).[45934] However, most inhaled beta-2 agonists, as well as inhaled budesonide, are considered acceptable for use during pregnancy because of the low bioavailability and maternal serum levels after use.[45934] [49764] [63021] According to the 2004 guidelines of the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group, long-acting beta-2 agonists (LABAs), in combination with inhaled corticosteroids (ICS), are one of the preferred treatment options for the long-term control of moderate asthma during pregnancy and lactation; use of medium dose ICS is also a preferred option. Although a preferred LABA is not recommended, the guideline states that more experience is available with salmeterol. Due to the availability of safety information during pregnancy, budesonide is preferred over other ICS.[45934] Infants born to mothers taking substantial corticosteroid doses during pregnancy should be monitored for signs of hypoadrenalism. There are no well-controlled human studies that have investigated the effects of budesonide; formoterol on preterm labor or labor at term. Because of the potential for beta-2 agonist interference with uterine contractility, use of budesonide; formoterol should be restricted to those patients in whom the benefits clearly outweigh the risks.[32950] [72049]
There are no well-controlled human studies of budesonide; formoterol during breast-feeding. Formoterol was excreted in milk in reproductive studies in rats; however, it is unknown whether formoterol is excreted in human milk. Glucocorticoids, such as budesonide, are excreted into human breast milk. Data from a small number (n = 8) of lactating women showed an estimated oral daily dose of budesonide available to the nursing infants which was approximately 0.3% to 1% of the dose inhaled by the mothers. Budesonide plasma concentrations obtained in five of the infants at about 140 minutes after drug administration to the mother and 90 minutes after breast-feeding were below quantifiable levels.[32950] [72049] The amount of inhaled budesonide excreted in breast-milk is minute, and infant exposure is negligible. While not measured, the amount of formoterol absorbed into the maternal bloodstream and excreted into breast-milk after inhalation is expected to be very low; therefore, it is unlikely that nursing infants would be exposed to clinically significant amounts of formoterol via breast milk. Most inhaled bronchodilators are considered acceptable for use during the postpartum period and breast-feeding because of the low bioavailability and maternal serum levels after use.[45934] [63021] The 2004 guidelines of the National Asthma Education and Prevention Program (NAEPP) Asthma and Pregnancy Working Group consider a combination of inhaled corticosteroids with long-acting inhaled beta-2 agonists (LABAs) a preferred treatment option for moderate asthma in pregnancy and lactation.[45934]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.