ThisiscontentfromElsevier'sDrugInformation
Capecitabine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
1,000 mg/m2 or 1,250 mg/m2 PO twice daily on days 1 to 14, repeated every 21 days until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a subset of patients with stage IV breast cancer that was resistant to both paclitaxel and an anthracycline (n = 43) from an open-label, single-arm clinical trial (SO14697), treatment with capecitabine resulted in a partial response rate of 25.6% (no complete responses) for a median duration of 5.1 months; the median time to progression in these patients was 3.4 months and the median survival was 8.4 months. The objective response rate in the overall population of patients who were less resistant to chemotherapy (n = 135) was 18.5% (1 complete response) with a median time to progression of 3 months and median survival of 10.1 months.[44458]
1,000 mg/m2 or 1,250 mg/m2 PO twice daily on days 1 to 14, in combination with docetaxel (75 mg/m2 IV on day 1), every 3 weeks until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] In a multicenter, randomized, open-label, phase 3 trial (SO14999), treatment with capecitabine plus docetaxel significantly improved the time to disease progression (6.1 months vs. 4.2 months), overall survival (14.5 months vs. 11.6 months), and objective response rate (32% vs. 22%) compared to monotherapy with docetaxel in patients with metastatic breast cancer resistant to or recurring during/after anthracycline-based chemotherapy.[44575] [44458]
1,000 mg/m2 PO twice daily on days 1 through 14, in combination with lapatinib (1,250 mg PO once daily on days 1 to 21), repeated every 21 days until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a randomized, phase 3 clinical trial of patients with progressive, locally advanced or metastatic breast cancer, treatment with lapatinib plus capecitabine significantly improved the median time to progression (TTP) by independent assessment compared with capecitabine alone (27.1 weeks vs. 18.6 weeks), with a response rate of 23.7% versus 13.9%; by investigator assessment, the median TTP was 23.9 weeks vs. 18.3 weeks with a response rate of 31.8% vs. 17.4%, respectively. Median progression-free survival (PFS) and overall survival (OS) were decreased in patients with HER2-positive metastatic breast cancer treated with lapatinib plus capecitabine compared with trastuzumab plus capecitabine in a randomized, open-label trial. Patients with HER2-positive metastatic breast cancer receiving first-line treatment with lapatinib plus taxane-based chemotherapy also had a shorter median PFS compared with trastuzumab plus taxane-based chemotherapy in another randomized, open-label trial. Patients should have progressed on trastuzumab and taxane-based therapy prior to treatment with lapatinib and capecitabine.[33192]
1,000 mg/m2 PO twice daily on days 1 to 14, in combination with ixabepilone (40 mg/m2 [maximum BSA, 2.2 m2] IV on day 1), every 3 weeks; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, randomized, open-label clinical trial of patients with anthracycline- and taxane-resistant locally advanced or metastatic breast cancer, treatment with ixabepilone plus capecitabine significantly improved the median progression-free survival (PFS) (5.7 months vs. 4.1 months) and objective response rate (34.7% vs. 14.3%) compared with capecitabine alone; the median duration of response was 6.4 months versus 5.6 months, respectively. There was no significant difference in overall survival (12.9 months vs. 11.1 months).[33563]
750 mg/m2 PO twice daily on days 1 to 14 every 21 days in combination with neratinib (240 mg PO once daily) until disease progression or unacceptable toxicity; alternatively, a 2-week neratinib dose escalation schedule may be given as follows: 120 mg PO once daily on days 1 to 7 (week 1), 160 mg PO once daily on days 8 to 14 (week 2), and 240 mg PO once daily starting on day 15 (week 3 and beyond).[62127] Round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[62127] [44458] Treatment with neratinib plus capecitabine significantly improved median progression-free survival (PFS) (5.6 months vs. 5.5 months) compared with lapatinib plus capecitabine in patients with metastatic HER2-positive breast cancer who had received at least 2 prior anti-HER2 based regimens in the metastatic setting in a randomized, open-label clinical trial (the NALA study). Rates of PFS were more durable in the neratinib plus capecitabine arm at 12 months (29% vs. 15%) and 24 months (12% vs. 3%). The objective response rate was 32.8 months in the neratinib arm for a median duration of 8.5 months compared with 26.7 months in the lapatinib arm for a median duration of 5.6 months. Overall survival was 21 months versus 18.7 months, respectively.[65929]
1,000 mg/m2 PO twice daily on days 1 to 14 of each 21-day cycle in combination with tucatinib (300 mg PO twice daily) and trastuzumab (8 mg/kg IV over 90 minutes on day 1 of cycle 1, followed 3 weeks later by 6 mg/kg IV over 30 minutes repeated every 21 days) until disease progression or unacceptable toxicity; tucatinib and capecitabine can be taken at the same time. Round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. The addition of tucatinib to trastuzumab and capecitabine significantly improved median progression-free survival (PFS) (7.8 months vs. 5.6 months) and overall survival (21.9 months vs. 17.4 months) compared with placebo plus trastuzumab and capecitabine in patients with HER2-positive, unresectable locally advanced or metastatic breast cancer after prior HER2 treatment in a randomized, double-blind clinical trial (HER2CLIMB); all patients had received prior trastuzumab and ado-trastuzumab emtansine and all but 2 patients had prior pertuzumab. The confirmed objective response rate was also significantly improved with the addition of tucatinib (40.6% vs. 22.8%; complete response, 3% vs. 2%) for a median duration of 8.3 months versus 6.3 months, respectively. Patients with brain metastases were eligible for inclusion in the HER2CLIMB study as long as they were neurologically stable and did not require immediate radiation or surgery; patients with leptomeningeal disease were excluded. The median PFS in patients with brain metastases was similar to the overall population (7.6 months vs. 5.4 months).[65295] [65296]
825 mg/m2 PO twice daily with concomitant radiation therapy and 1,250 mg/m2 PO twice daily without radiation therapy when administered as part of a peri-operative combination regimen; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] In a multicenter, randomized, open-label clinical trial, patients with stage II to III locally advanced rectal cancer were randomized to adjuvant treatment with capecitabine-based chemoradiotherapy or fluorouracil-based chemoradiotherapy; patients in the capecitabine arm received 2 cycles of capecitabine (1,250 mg/m2 PO twice daily on days 1 to 14, every 21 days) followed by chemoradiotherapy (50.4 Gy plus capecitabine 825 mg/m2), followed by 3 cycles of capecitabine (1,250 mg/m2 PO twice daily on days 1 to 14, every 21 days). After 3 years, the protocol was amended to allow a neoadjuvant cohort in which patients in the capecitabine group received chemoradiotherapy (50.4 Gy plus capecitabine 825 mg/m2 PO twice daily) followed by radical surgery and 5 cycles of capecitabine (1,250 mg/m2 PO twice daily on days 1 to 14, every 21 days). During chemoradiotherapy, radiation and the reduced dose of capecitabine were started on the same day and capecitabine was stopped on the last day of radiotherapy, including weekends. After a median follow-up of 52 months, the 5-year overall survival rate with capecitabine was noninferior to fluorouracil (76% vs. 67%); the 3-year disease-free survival rate was 75% versus 67%, respectively. The numbers of local recurrences were similar in each group (6% vs 7%), but fewer patients treated with capecitabine developed distant metastases (19% vs. 28%).[68392]
1,250 mg/m2 PO twice daily on days 1 to 14, repeated every 21 days for a maximum of 8 cycles. Dosages should be adjusted based on toxicity during treatment cycle; once a dosage is reduced, it should not be increased at a later time. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] After a median follow-up time of 6.9 years, adjuvant treatment with capecitabine was non-inferior to fluorouracil plus leucovorin in patients with previously untreated Dukes' stage C colon cancer in terms of 5-year disease-free survival (59% vs. 55%) and 5-year overall survival (71% vs. 68%).[31340]
1,000 mg/m2 PO twice daily on days 1 to 14 in combination with oxaliplatin (130 mg/m2 IV on day 1), repeated every 21 days for a maximum of 8 cycles; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] Treatment with capecitabine/oxaliplatin (XELOX) improved 7-year disease-free survival compared with fluorouracil/leucovorin in patients with stage III colon cancer in a multicenter, randomized, phase 3 clinical trial (63% vs. 56%; p = 0.004); 7-year overall survival rates were 73% and 67% respectively (p = 0.04). Because alpha levels were not prespecified for testing treatment differences in the final analysis, p values provide only a descriptive statistical measure of a possible difference. In a biomarker analysis, low tumor expression of dihydropyridine dehydrogenase (DPD) may be predictive for XELOX efficacy; no significant associations were observed in the fluorouracil group.[45258] [69445]
1,250 mg/m2 PO twice daily on days 1 to 14, repeated every 21 days until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] Treatment with capecitabine significantly improved the overall response rate (21% vs. 11% to 14%) compared with fluorouracil plus leucovorin in 2 multicenter, randomized clinical trials (SO14695 and SO14796). The median time to progression was not significantly different in either study (4.2 to 4.5 months vs. 4.3 months), and treatment with capecitabine was noninferior to fluorouracil/leucovorin in terms of overall survival (12.5 to 13.3 months vs. 12.1 to 13.4 months).[69447] [46959]
1,000 mg/m2 PO twice daily on days 1 to 14, in combination with oxaliplatin (130 mg/m2 IV on day 1), every 21 days until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] In a multicenter, randomized, phase 3 clinical trial, patients with metastatic colorectal cancer were randomized to treatment with XELOX or fluorouracil/leucovorin/oxaliplatin (FOLFOX4); the protocol was later amended to a 2 x 2 factorial design to allow further randomization to bevacizumab or placebo. Treatment with XELOX was noninferior to FOLFOX4 with regard to the primary outcome of progression-free survival (8 months vs. 8.5 months).[41607] In an exploratory overall survival analysis, the median overall survival was 19 months in the pooled capecitabine/capecitabine-placebo arms compared with 18.9 months in the pooled FOFOX4/FOLFOX4-placebo arms; the study was not powered for formal noninferiority testing for overall survival.[68390]
1,000 mg/m2 PO twice daily on days 1 to 14, in combination with bevacizumab (7.5 mg/kg IV on day 1) and oxaliplatin (130 mg/m2 IV on day 1), every 21 days until disease progression or unacceptable toxicity; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Bevacizumab was administered prior to oxaliplatin on day 1 in the randomized clinical trial. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, randomized, phase 3 clinical trial, patients with metastatic colorectal cancer were randomized to treatment with XELOX or fluorouracil/leucovorin/oxaliplatin (FOLFOX4); the protocol was later amended to a 2 x 2 factorial design to allow further randomization to bevacizumab or placebo. The primary endpoint of median progression-free survival was significantly improved in patients treated with either XELOX or FOLFOX4 plus bevacizumab compared with those who received XELOX or FOLFOX4 alone (9.4 months vs. 8 months), with a median duration of response of 8.45 months versus 7.4 months, respectively. Overall survival, a secondary endpoint, was improved in the bevacizumab arms but did not reach statistical significance (21.3 vs. 19.9 months).[41609] [44458]
Multiple dosage regimens have been studied. Capecitabine 1,250 mg/m2 PO twice daily on days 1 to 14, followed by a 7-day rest period, given in combination with cisplatin 60 mg/m2 IV over 1 hour on day 1, repeated every 21 days until disease progression or unacceptable toxicity. In a phase II trial of 38 patients, capecitabine/cisplatin produced an overall response rate of 21.4%. Grade III or IV neutropenia occurred in 20% of patients.[36002] Another regimen is capecitabine 650 mg/m2 PO twice daily on days 1 to 14, followed by a 7-day rest period, given in combination with gemcitabine 1,000 mg/m2 IV over 30 minutes on days 1 and 8, repeated every 21 days. In phase II trials, this dosage produced an ORR of 29% to 31%.[36003] [36004] Another phase II trial of 43 patients studied capecitabine 1,000 mg/m2 PO twice daily on days 1 to 14, followed by a 7-day rest period, given in combination with cisplatin 60 mg/m2 IV on day 1 and epirubicin 50 mg/m2 IV on day 1, repeated every 21 days until disease progression or unacceptable toxicity.[36005]
1,000 mg/m2 PO twice daily on days 1 to 14, then a 7-day rest period has been given every 21 days. Treatment should be continued until the patient experiences unacceptable toxicity or disease progression. In a phase II study of 41 patients, a partial response was observed in 7.3% of patients and stable disease was achieved in 54% of patients. Grade 3 adverse effects included hand-foot syndrome (27%), abdominal pain (17%), and diarrhea (10%).[34432] In other phase II studies, a higher dose of 1,250 mg/m2 led to the overall response rate in heavily pretreated patients of 3% to 9%.[46087][46088]
1,000 mg/m2 PO twice daily on days 1 to 14 in combination with oxaliplatin 130 mg/m2 IV on day 1, repeated every 3 weeks for 8 cycles. In a phase 3 clinical trial, 1,035 patients with stage II to IIIB gastric cancer were randomized to receive adjuvant capecitabine and oxaliplatin (XELOX) or observation after surgical (D2) resection. The primary endpoint, 3-year disease free survival (DFS), was significantly improved with XELOX (74% vs. 60%, HR 0.56, 95% CI 0.44 to 0.72, p less than 0.0001). At a median follow-up of 34.4 months, the difference in overall survival was not significantly different between the 2 treatment arms (HR 0.74, 95% CI 0.53 to 1.03, p = 0.0775).[45379]
625 mg/m2 PO twice daily on days 1 to 21 of every 21-day cycle for a maximum of 8 cycles has been studied in combination with platinum-containing chemotherapy. Additionally, capecitabine 850 mg/m2 or 1,000 mg/m2 PO twice daily on days 1 to 14 of every 21-day cycle until disease progression or unacceptable toxicity has been studied in combination with oxaliplatin 130 mg/m2 IV on day 1 of each cycle. Round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] [34869] [69456] [69457] [40571]
1,000 mg/m2 PO twice daily on days 1 to 14, in combination with cisplatin (80 mg/m2 IV on day 1) and trastuzumab (8 mg/kg IV on day 1, then 6 mg/kg IV every 21 days thereafter), every 3 weeks until disease progression or unacceptable toxicity. Round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] In a phase 3 trial, patients with inoperable, locally advanced, recurrent, or metastatic adenocarcinoma of the stomach or gastroesophageal junction were randomized to receive 6 cycles of cisplatin and fluorouracil or capecitabine, with or without trastuzumab which was continued until disease progression or unacceptable toxicity. Overall survival (13.5 months vs. 11 months), the primary endpoint, and objective response rate (47% vs. 35%) were significantly increased with the addition of trastuzumab. An updated survival analysis conducted 1 year after the final analysis showed a continued overall survival benefit in the trastuzumab arm (13.1 months vs. 11.7 months). A subgroup analysis revealed an even greater increase in overall survival (18 months vs. 13.2 months) for the trastuzumab arm in patients with high expression of the HER2 protein. Cardiac dysfunction (LVEF decrease of 10% or more from baseline to an absolute value less than 50%) occurred in 5% of patients who received trastuzumab vs. 1.1% of patients who did not receive trastuzumab.[41715] [28061]
830 mg/m2 PO twice daily on days 1 to 21 in combination with gemcitabine (1,000 mg/m2 IV on days 1, 8, and 15), repeated every 28 days until disease progression, unacceptable toxicity, or for a maximum of 6 cycles; round the calculated capecitabine dose to the nearest 150 mg in order to administer whole tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[44458] After a median follow-up of 60 months, patients with ductal adenocarcinoma of the pancreas treated with gemcitabine plus capecitabine after an R0 or R1 resection had significantly prolonged median overall survival compared with those treated with gemcitabine alone in a multicenter, randomized, open-label phase 3 clinical trial (27.7 months vs. 26 months); 5-year survival rates were 20% and 28%, respectively.[69450] In a subgroup analysis after , the magnitude of effect on median overall survival in patients with R0 resection (39.5 months vs. 27.9 months) was significantly greater than in patients with R1 resection (23.7 months vs. 23 months).[62255]
Dosage Adjustments for Treatment-Related Toxicities:
Monotherapy or in Combination with Docetaxel:
NOTE: At the beginning of a treatment cycle, if the patient is receiving capecitabine in combination with docetaxel and a treatment delay is indicated, delay administration of both agents until the requirements for restarting both drugs are met.
Other Nonhematologic Adverse Reactions
Severe Cutaneous Adverse Reactions (SCARs) including Stevens Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN)
Dosage Adjustments for Hematologic Toxicities when used in Combination with Ixabepilone:
NOTE: Follow recommendations for treatment-related toxicity, above, for nonhematologic toxicity.
2,500 mg/m2 PO total daily dose (1,250 mg/m2 PO administered twice daily) on days 1 to 14, every 21 days.
2,500 mg/m2 PO total daily dose (1,250 mg/m2 PO administered twice daily) on days 1 to 14, every 21 days.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Baseline Hepatic Impairment:
In patients with mild to moderate hepatic dysfunction due to liver metastases, no starting dose adjustment is necessary; however, patients should be carefully monitored. Patients with severe hepatic dysfunction have not been studied.[44458]
Treatment-Related Hepatotoxicity:
Baseline Renal Insufficiency:





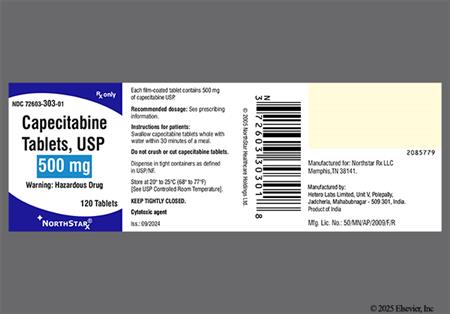
Capecitabine is a prodrug that is metabolized to fluorouracil, an antimetabolite nucleoside inhibitor. It is FDA approved as monotherapy for the adjuvant treatment of stage III colon cancer and for the treatment of unresectable or metastatic colorectal cancer or breast cancer; as a component of a combination chemotherapy regimen for the adjuvant treatment of colorectal cancer or pancreatic cancer and for unresectable or metastatic colorectal cancer, gastric cancer, esophageal cancer, gastroesophageal junction (GEJ) cancer; in combination with docetaxel in progressive advanced or metastatic breast cancer; and as a component of chemoradiotherapy for the perioperative treatment of locally advanced rectal cancer. Capecitabine carries a black box warning for an increased risk of bleeding with concomitant use of oral vitamin K antagonists such as warfarin.[44458]
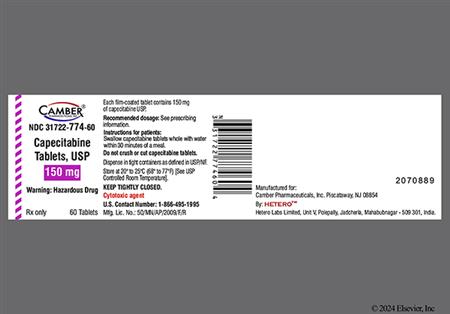
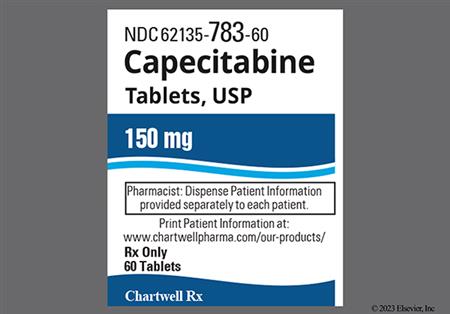
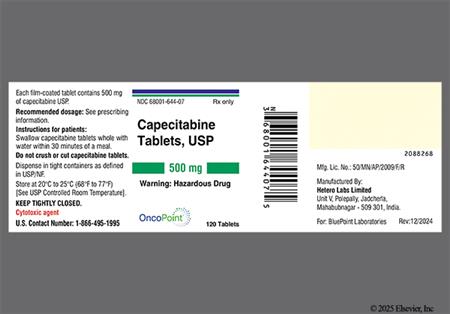
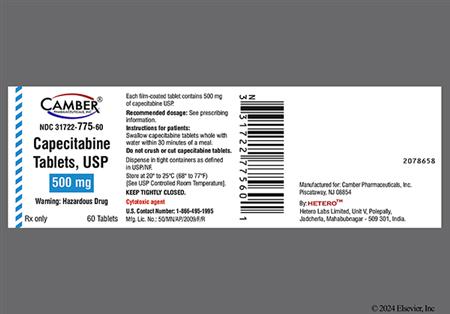
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Emetic Risk
Insomnia, depression, and confusion were each reported in fewer than 10% of patients treated with capecitabine monotherapy in a pooled safety population. A general alteration in mood was also reported in less than 10% of patients who received capecitabine monotherapy in 1 randomized clinical trial.[44458]
Palmar-plantar erythrodysesthesia (hand and foot syndrome) is a dose-limiting toxicity of capecitabine and occurred in 54% to 63% (grade 3 or 4, 11% to 24%) of patients treated with capecitabine as monotherapy or in combination with docetaxel across clinical trials; persistent or severe palmar-plantar erythrodysesthesia can eventually lead to the loss of fingerprints. In patients with metastatic breast or colorectal cancer who received capecitabine monotherapy, the median time to onset of grade 1 to 3 palmar-plantar erythrodysesthesia was 2.6 months (range, 11 days to 1 year). Dermatitis was additionally reported in 27% to 37%; grade 3, 1% of patients treated with capecitabine monotherapy in clinical trials. Additional dermatologic adverse reactions reported in less than 10% of patients treated with capecitabine monotherapy include alopecia, erythema, hyperhidrosis, nail disorder, photosensitivity reaction, pruritus, radiation recall reaction, rash, skin discoloration, and skin ulcer. Nail discoloration and onycholysis were each reported in less than 10% of patients treated with capecitabine and docetaxel in a clinical trial; the addition of capecitabine to docetaxel did not increase the incidence of alopecia (41% vs. 42%; grade 3, 6% vs. 7%) or nail disorders (14% vs. 15%; grade 3, 2% vs. 0%) compared with docetaxel alone. Cutaneous lupus erythematosus (lupus-like symptoms) and severe cutaneous adverse reactions (SCARs) such as Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) have been reported in postmarketing experience with capecitabine; permanently discontinue capecitabine for SCARs.[44458]
Hyperbilirubinemia occurred in 48% of patients with metastatic colorectal cancer treated with capecitabine compared with 17% of those who received fluorouracil/leucovorin in a randomized clinical trial (grade 3 or 4, 23% vs. 6%); the incidence of grade 3 or 4 increases in bilirubin was similar (20%) in another clinical trial of patients with colorectal cancer receiving adjuvant treatment with capecitabine therapy. In a single-arm trial of patients with metastatic breast cancer, hyperbilirubinemia occurred in 22% of patients who received monotherapy (grade 3 or 4, 11%). Hyperbilirubinemia was more common in metastatic breast cancer patients treated with capecitabine plus docetaxel compared with docetaxel alone (20% vs. 6%; grade 3 or 4, 9% vs. 4%). In patients with metastatic breast or colorectal cancer, the incidence of patients who developed grade 3 or 4 hyperbilirubinemia was higher in those with hepatic metastases at baseline compared to those without (23% vs. 12%). The median total bilirubin increased from 8 micromol/liter at baseline to 13 micromol/liter during therapy; the median time to onset for grade 3 or 4 hyperbilirubinemia was 64 days. Of patients with grade 3 or 4 hyperbilirubinemia, 58% (grade 3 or 4, 8%) had both pre- and postbaseline increases in alkaline phosphatase and 19% had only postbaseline increases in alkaline phosphatase; 35% (grade 3 or 4, 3%) had both pre- and postbaseline elevated hepatic enzymes and 28% only had postbaseline transaminitis. Grade 3 or 4 increases in ALT were reported in 1.6% of patients who received capecitabine monotherapy in one noncomparative trial. Hepatic fibrosis, hepatitis, cholestasis, and abnormal liver function tests were also each reported in less than 10% of patients treated with capecitabine monotherapy in a pooled safety population, while jaundice, abnormal liver function tests, hepatic failure, hepatic coma, and hepatotoxicity were reported in less than 10% of patients treated with capecitabine plus docetaxel in 1 clinical trial. Hepatic failure was also reported in postmarketing experience with capecitabine. Increased ALT (75%) and hypoalbuminemia (55%) were more common in pediatric patients compared to adult patients. Monitor patients with hepatic disease more frequently for adverse reactions; an interruption of therapy, dose reduction, or discontinuation of therapy may be necessary if hyperbilirubinemia occurs.[44458]
Cardiotoxicity has been reported with capecitabine treatment, including myocardial infarction/ischemia, angina, dysrhythmias or arrhythmia exacerbation, cardiac arrest, heart failure, cardiomyopathy, ECG changes, and sudden death. Sinus tachycardia, bradycardia, atrial fibrillation, and myocarditis were each reported in less than 10% of patients who received capecitabine monotherapy in a pooled safety population; chest pain was additionally reported in less than 10% of capecitabine-treated patients in 1 randomized clinical trial. Fewer than 10% of breast cancer patients treated with capecitabine plus docetaxel experienced supraventricular tachycardia (SVT) in another randomized clinical trial. Use capecitabine with caution in patients with cardiac disease or a prior history of coronary artery disease. If cardiotoxicity occurs, interrupt therapy with capecitabine as clinically appropriate; the safety of resuming capecitabine therapy after cardiotoxicity has occurred has not been established.[44458]
Bone marrow suppression can occur with capecitabine treatment. Lymphopenia (94%; grade 3 or 4, 59%), anemia (72%; grade 3 or 4, 4%), neutropenia (26%; grade 3 or 4, 4%), and thrombocytopenia (24%; grade 3 or 4, 4%) were reported in a single-arm clinical trial of patients treated with capecitabine. In pooled data from 2 randomized clinical trials, anemia occurred with a similar frequency in patients treated with capecitabine to those who received fluorouracil and leucovorin (80% vs. 79%; grade 3 or 4, 2% to 3% vs. 1% to 2%); however, neutropenia occurred in 13% of patients who received capecitabine compared with 46% of those in the fluorouracil/leucovorin arm (grade 3 or 4, 3% vs. 21%). In another trial, the incidence of grade 3 or 4 decreases from baseline in lymphocytes (13% vs. 13%), hemoglobin (1% vs. 1.2%), and platelets (1% vs. 0.7%) were similar in patients treated with capecitabine compared with fluorouracil/leucovorin; grade 3 or 4 decreases from baseline in neutrophils/granulocytes (2.4% vs. 26%) and neutrophils (2.2% vs. 26%) were again more common in the fluorouracil/leucovorin arm. In a pooled safety population, bone marrow depression, leukopenia, and pancytopenia each occurred in less than 10% of patients who received capecitabine monotherapy. The addition of capecitabine to docetaxel resulted in a similar incidence of lymphopenia (99% vs. 98%; grade 3 or 4, 89% vs. 84%), leukopenia (91% vs. 88%; grade 3 or 4, 61% vs. 75%), neutropenia (86% vs. 87%; grade 3 or 4, 69% vs. 76%), anemia (80% vs. 83%; grade 3 or 4, 10% vs. 5% to 6%), and febrile neutropenia (16% vs. 21%; grade 3 or 4, 16% vs. 21%) compared to those who received docetaxel alone in a randomized clinical trial; thrombocytopenia was reported in 41% versus 23% of patients, respectively (grade 3 or 4, 3% vs. 3%). Agranulocytosis and neutropenic sepsis were each reported in less than 10% of patients who received capecitabine and docetaxel. Lymphopenia (73%), thrombocytopenia (57%), neutropenia (50%), and low hematocrit (50%) were more common in the pediatric population compared to adults. Patients with complete or near complete absence of dihydropyrimidine dehydrogenase (DPD) activity (complete DPD deficiency) are at increased risk for early-onset toxicity and serious or fatal adverse reactions including neutropenia; patients with partial DPD activity (partial DPD deficiency) may also have increased risk of serious or fatal adverse reactions. Do not administer capecitabine to patients with neutrophil counts less than 1,500 cells/mm3 or platelet counts below 100,000 cells/mm3. An interruption of therapy, dose reduction, or discontinuation of therapy is necessary if grade 3 or 4 myelosuppression occurs during the course of treatment.[44458]
Nausea (34% to 53%; grade 3 or higher, 2% to 4%), vomiting (15% to 37%; grade 3 or higher, 2% to less than 5%), abdominal pain (14% to 35%; grade 3 or higher, 3% to less than 10%), stomatitis (22% to 25%; grade 3 or higher, 2% to 7%), and constipation (15% or less; grade 3 or higher, less than 2%), were reported in patients treated with capecitabine monotherapy across clinical trials; grade 1 or 2 oral discomfort was also reported in capecitabine-treated patients in 1 trial. Less than 10% of patients who received capecitabine monotherapy in a pooled safety population reported abdominal distention, gastric ulcer (peptic ulcer), ileus, and proctalgia. The incidence of stomatitis was higher in a clinical trial of patients who received docetaxel plus capecitabine (67%; grade 3 or higher, 17% to 18%), but the incidence of nausea (45% (grade 3, 7%), vomiting (35%; grade 3 or higher, 5%), abdominal pain (30%; grade 3 or higher, 3% to 4%), constipation (20%; grade 3, 2%), and ileus (less than 10%) were similar to capecitabine monotherapy. Sore throat was additionally reported in 12% (grade 3, 2%) of those who received capecitabine and docetaxel, as well as esophageal ulceration (less than 10%). Patients with complete or near complete absence of dihydropyrimidine dehydrogenase (DPD) activity (complete DPD deficiency) are at increased risk for early-onset toxicity and serious or fatal adverse reactions including mucositis; patients with partial DPD activity (partial DPD deficiency) may also have increased risk of serious or fatal adverse reactions.[44458]
Diarrhea which can sometimes be severe is a dose-limiting toxicity of capecitabine and was reported in 47% to 67% (grade 3 or 4, 12% to 15%) of patients treated with capecitabine as monotherapy or in combination with docetaxel or oxaliplatin in clinical trials; the incidence of diarrhea was higher when used as a component of chemoradiotherapy. Gastroenteritis was reported in less than 10% of patients receiving capecitabine monotherapy in a pooled safety population. An upper GI inflammatory disorder (less than 10%) and a GI motility disorder (10%; grade 3, less than 1%) were reported in a clinical trial of patients with advanced colorectal cancer who received capecitabine monotherapy. Necrotizing enterocolitis (typhlitis) developed in less than 10% of metastatic breast cancer patients treated with capecitabine plus docetaxel; consider typhlitis in patients with fever, neutropenia, and abdominal pain. Patients with complete or near complete absence of dihydropyrimidine dehydrogenase (DPD) activity (complete DPD deficiency) are at increased risk for early-onset toxicity and serious or fatal adverse reactions including diarrhea; patients with partial DPD activity (partial DPD deficiency) may also have increased risk of serious or fatal adverse reactions. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary for grade 2 or higher diarrhea or dehydration.[64032] [44458]
Anorexia or decreased appetite (26% or less; grade 3 or higher, 3% to 4%), dysgeusia (less than 10%), dysphagia (less than 10%), and dyspepsia (14% or less) were reported in patients treated with capecitabine as monotherapy or in combination with docetaxel across clinical trials. Dyspepsia and cachexia were each additionally reported in less than 10% of patients who received capecitabine monotherapy while weight loss and xerostomia were each reported in less than 10% of patients treated with capecitabine plus docetaxel.[44458]
Dehydration was reported in 10% or fewer patients treated with capecitabine as monotherapy or in combination with docetaxel in clinical trials (grade 3, 2% or less). Deaths from severe dehydration have been reported in elderly patients treated with weekly fluorouracil and leucovorin. Renal impairment occurred in less than 10% of patients who received capecitabine in clinical trials, with acute renal failure secondary to dehydration (including fatal outcome) reported in postmarketing experience with capecitabine. Optimize hydration prior to starting therapy. Monitor renal function and hydration status at baseline and as clinically indicated. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary if dehydration or renal impairment occur.[44458]
Fever was reported in 18% or fewer patients treated with capecitabine monotherapy across clinical trials (grade 3 or 4, 1% or less). Various types of infection including bronchitis, fungal infections, influenza-like illnesses, pneumonia, sepsis, and other viral infections have each been reported in less than 10% of patients who received capecitabine monotherapy.[44458]
Fatigue (16% to 42% vs. 16% to 46%; grade 3 or 4, 8% or less vs. 1% to 4%), asthenia (10% vs. 10%; less than 1% vs. 1%), and lethargy (10% vs. 9%; grade 3 or 4, less than 1% vs. less than 1%) occurred with a similar frequency in patients treated with capecitabine monotherapy versus fluorouracil/leucovorin in clinical trials. Muscle weakness was also reported in fewer than 10% of patients who received capecitabine monotherapy in a pooled safety population. The addition of capecitabine to docetaxel in patients with metastatic breast cancer did not increase the incidence of asthenia (26% vs. 25%; grade 3 or 4, 4% to 5% vs. 6%) or fatigue (22% vs. 27%; grade 3 or 4, 4% vs. 6%) compared with docetaxel alone. Weakness was reported in 16% of patients who received capecitabine plus docetaxel compared with 11% of those who received docetaxel alone (grade 3, 2% vs. 2%); lethargy was reported in less than 10% of patients in the capecitabine arm.[44458]
Mild (grade 1 or 2) ocular irritation was reported in 13% to 15% of patients with metastatic breast or colorectal cancer treated with capecitabine monotherapy in 2 clinical trials. Additionally, abnormal vision/visual impairment, conjunctivitis, and keratoconjunctivitis have each been reported in fewer than 10% of patients receiving capecitabine monotherapy. Increased lacrimation was reported in 12% of patients with metastatic breast cancer receiving treatment with capecitabine plus docetaxel compared with 7% (grade 3, less than 1%) of those receiving docetaxel alone; conjunctivitis and eye irritation were also each reported in fewer than 10% of patients in the capecitabine arm. There have been reports of lacrimal duct stenosis and corneal disorders including keratitis in postmarketing experience with capecitabine.[44458]
Hypercalcemia and hypocalcemia have been reported in patients with metastatic colorectal cancer treated with capecitabine monotherapy in a randomized clinical trial, including grade 3 or 4 decreases (2.3%) and increases (1.1%) from baseline in calcium levels. Hypokalemia, hypomagnesemia, and hypertriglyceridemia were also each reported in fewer than 10% of patients receiving capecitabine monotherapy in a pooled safety population. Hypokalemia (68%), hypocalcemia (48%), hypophosphatemia (45%), and hyponatremia (45%) were more common in pediatric patients compared to adult patients.[44458]
Hemorrhage (bleeding), coagulopathy, and epistaxis were each reported in less than 10% of patients treated with capecitabine monotherapy in a pooled safety population; GI bleeding was additionally reported in less than 10% of patients treated with capecitabine monotherapy in 1 randomized clinical trial. Hemorrhagic diarrhea, decreased prothrombin, and epistaxis were also reported in less than 10% of patients treated with capecitabine plus docetaxel in a randomized clinical trial.[44458]
Musculoskeletal adverse reactions reported with capecitabine treatment when administered as monotherapy or in combination with docetaxel include arthralgia (15% or less; grade 3, 2% or less), arthritis (less than 10%), back pain (12% or less; grade 3, 2% or less), myalgia (15 or less%; grade 3, 2% or less), noncardiac chest pain (unspecified) (less than 10%), generalized pain (12% or less; grade 3, 1% or less), limb pain (13% or less; grade 3, less than 1%), and myalgia (less than 10%). Bone pain was reported in fewer than 10% of patients with metastatic breast cancer treated with capecitabine plus docetaxel in 1 randomized clinical trial.[44458]
Headache (15% or less; grade 3, 3% or less), dizziness (12% or less), and vertigo (less than 10%) have been reported in patients treated with capecitabine as monotherapy or in combination with docetaxel across clinical trials; migraine was additionally reported in fewer than 10% of patients treated with capecitabine plus docetaxel in 1 randomized clinical trial.[44458]
Paresthesias (12% to 21%; grade 3, 1% or less), peripheral neuropathy (10% or less), hypoesthesia (less than 10%), and polyneuropathy (less than 10%) were reported in patients treated with capecitabine monotherapy across clinical trials. Patients with complete or near complete absence of dihydropyrimidine dehydrogenase (DPD) activity (complete DPD deficiency) are at increased risk for early-onset toxicity and serious or fatal adverse reactions including neurotoxicity; patients with partial DPD activity (partial DPD deficiency) may also have increased risk of serious or fatal adverse reactions.[44458]
Edema was reported in 15% or fewer patients treated with capecitabine monotherapy across clinical trials (grade 3, 1%). The addition of capecitabine to docetaxel did not increase the incidence of edema compared to docetaxel alone in 1 randomized clinical trial (33% vs. 34%; grade 3 or 4, less than 2% vs. less than 4%). Lymphedema was reported in less than 10% of patients treated with capecitabine as monotherapy or in combination with docetaxel in clinical trials.[44458]
Dyspnea (14% or less; grade 3, less than 3%), cough (13% or less; grade 3, 1% or less), respiratory distress (less than 10%), and a nonspecific pharyngeal disorder (less than 10%) were reported in patients treated with capecitabine as monotherapy or in combination with docetaxel in clinical trials. Pleural effusion and rhinorrhea each occurred in fewer than 10% of patients with metastatic breast cancer treated with capecitabine plus docetaxel in 1 clinical trial.[44458]
Venous thrombosis and pulmonary embolism were each reported in less than 10% of patients treated with capecitabine monotherapy in clinical trials. Venous phlebitis and thrombophlebitis were each reported in less than 10% of metastatic breast cancer patients who received capecitabine plus docetaxel in 1 clinical trial.[44458]
Hot flashes were reported in less than 10% of patients treated with capecitabine monotherapy in a pooled safety population. Flushing was also reported in less than 10% of patients with metastatic breast cancer treated with capecitabine plus docetaxel in 1 clinical trial.[44458]
Ataxia, impaired balance, encephalopathy, syncope, and tremor were each reported in less than 10% of patients treated with capecitabine monotherapy across clinical trials. Toxic leukoencephalopathy was reported in postmarketing experience with capecitabine therapy.[44458]
Hypotension and hypertension were each reported in less than 10% of patients treated with capecitabine monotherapy in a pooled safety population.[44458]
Thirst (polydipsia) was reported in less than 10% of patients receiving capecitabine monotherapy for the treatment of colorectal cancer or breast cancer in clinical trials.[44458]
Dysarthria and dysphasia were each reported in less than 10% of patients receiving capecitabine monotherapy in a pooled safety population.[44458]
Angioedema has been reported with capecitabine use in postmarketing experience.[44458]
Optimize hydration prior to starting therapy with capecitabine. Diarrhea, sometimes severe, has been reported with capecitabine therapy. Carefully monitor patients with severe diarrhea and administer standard antidiarrheal treatments (e.g., loperamide) if necessary. Dehydration can occur with capecitabine therapy and patients with anorexia, asthenia, nausea/vomiting, or diarrhea may be at increased risk. Monitor hydration status and renal function at baseline and as clinically indicated. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary for grade 2 or higher diarrhea or dehydration.[44458]
Use capecitabine with caution in patients with renal impairment; a dose reduction is necessary for patients with creatinine clearance (CrCl) 30 to 50 mL/min, and capecitabine has not been studied in patients with CrCl less than 30 mL/min. Serious cases of renal failure, some fatal, can occur with capecitabine treatment. Optimize hydration prior to starting therapy. Monitor renal function at baseline and as clinically indicated. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary if renal impairment or renal failure occurs.[44458]
Bone marrow suppression can occur with capecitabine treatment. Monitor complete blood counts at baseline and prior to each cycle. Do not administer capecitabine to patients with neutrophil counts less than 1,500 cells/mm3 or platelet counts below 100,000 cells/mm3. An interruption of therapy, dose reduction, or discontinuation of therapy is necessary if grade 3 or 4 myelosuppression occurs during the course of treatment.[44458]
Monitor the INR more frequently in patients receiving concomitant capecitabine and vitamin K antagonist anticoagulant therapy and adjust the anticoagulant dose as clinically appropriate. Clinically significant increases in PT and INR and/or bleeding events, including fatalities, have been reported in patients taking capecitabine concomitantly with oral vitamin K antagonists such as warfarin, occurring within several days and up to several months after initiating capecitabine therapy; patients included those with and without liver metastases, as well as those who were on stable doses of oral vitamin K antagonists at the time capecitabine was introduced.[44458]
Avoid capecitabine in patients with certain homozygous or compound heterozygous variants in the DPYD gene that result in complete dihydropyrimidine dehydrogenase deficiency (DPD deficiency) due to an increased risk of acute early-onset toxicities and serious, including fatal, adverse reactions (e.g., mucositis, diarrhea, neutropenia, and neurotoxicity); patients with partial DPD deficiency may also have an increased risk of serious, or fatal, adverse reactions. Capecitabine has not been proven safe for patients with complete DPD deficiency at any dose; for patients with partial DPD deficiency, individualize the capecitabine dose and modify dose based on tolerability and intent of treatment. Test for DPD deficiency prior to starting therapy unless immediate treatment is necessary. There is not an FDA-approved test to detect DPYD mutations; currently available tests may vary in accuracy and design. Hold or permanently discontinue capecitabine in patients with acute early-onset or unusually severe toxicities, which may indicate near complete or total absence of DPD activity.[44458]
Use capecitabine with caution in patients with cardiac disease or a prior history of coronary artery disease. Capecitabine therapy has been associated with cardiotoxicity including myocardial infarction, angina, dysrhythmias, cardiac arrest, cardiac failure, electrocardiogram changes, cardiomyopathy, and sudden death; patients with a history of coronary artery disease may be at increased risk. If cardiotoxicity occurs, interrupt therapy with capecitabine as clinically appropriate; the safety of resuming capecitabine therapy after cardiotoxicity has occurred has not been established.[44458]
Monitor patients with hepatic disease more frequently for adverse reactions. Capecitabine exposure increases in patients with mild to moderate hepatic impairment, while the effect of severe hepatic impairment on the safety and pharmacokinetics of capecitabine is unknown. Hyperbilirubinemia has been reported with capecitabine treatment and is more common in patients with hepatic metastases at baseline; an interruption of therapy, dose reduction, or discontinuation of therapy may be necessary if hyperbilirubinemia occurs.[44458]
Monitor geriatric patients (65 years or older) for an increased incidence of capecitabine-related gastrointestinal adverse reactions compared to younger patients. Deaths from severe enterocolitis, diarrhea, and dehydration have been reported in elderly patients receiving weekly leucovorin and fluorouracil in clinical trials.[44458]
Severe cutaneous adverse reactions (SCARs) (serious rash and skin disease) have been reported with capecitabine therapy including toxic epidermal necrolysis (TEN) and Stevens Johnson syndrome (SJS), which can be fatal. Palmar-plantar erythrodysesthesia (hand and foot syndrome) has also occurred with capecitabine treatment; persistent or severe hand and foot syndrome can lead to loss of fingerprints, which could impact patient identification. Monitor patients for new or worsening skin conditions. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary for skin toxicity, depending on the severity of the reaction. Permanently discontinue capecitabine for SCARs.[44458]
Pregnancy should be avoided by females of reproductive potential during capecitabine treatment and for at least 6 months after the last dose. Although there are no adequately controlled studies in pregnant women, capecitabine can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. Women who are pregnant or who become pregnant while receiving capecitabine should be apprised of the potential hazard to the fetus. When capecitabine was given to pregnant animals during organogenesis, teratogenesis and embryolethality were observed in mice and embryolethality in monkeys at 0.2 and 0.6 times the exposure (AUC), respectively, in patients receiving the recommended dose. Teratogenic malformations in mice included cleft palate, anophthalmia, microphthalmia, oligodactyly, polydactyly, syndactyly, kinky tail, and dilation of cerebral ventricles.[44458]
Counsel patients about the reproductive risk and contraception requirements during capecitabine treatment. Capecitabine can be teratogenic if taken by the mother during pregnancy. Females should avoid pregnancy and use effective contraception during and for at least 6 months after treatment with capecitabine. Females of reproductive potential should undergo pregnancy testing prior to initiation of capecitabine. Due to the risk of male-mediated teratogenicity, males with female partners of reproductive potential should use effective contraception during treatment and for 3 months after the last dose. Women who become pregnant while receiving capecitabine should be apprised of the potential hazard to the fetus. Although there are no data regarding the effect of capecitabine on human fertility, male and female infertility has been observed in animal studies.[44458]
Due to the potential for serious adverse reactions in nursing infants from capecitabine, advise women to discontinue breast-feeding during treatment and for 1 week after the final dose. It is not known whether capecitabine is present in human milk, although many drugs are excreted in human milk.[44458]
Capecitabine is converted into fluorouracil by a series of enzymatic reactions. One of the enzymes involved in this activation process, thymidine phosphorylase is expressed in higher concentrations in some human carcinomas compared to normal tissues, which may result in higher intra-tumor concentrations of fluorouracil. Both normal and tumor cells metabolize fluorouracil to 5-fluoro-2-deoxyuridine monophosphate (FdUMP) and 5-fluorouridine triphosphate (FUTP). FdUMP and the folate cofactor, 5,10-methylenetetrahydrofolate, bind to thymidylate synthase (TS) to form a covalently bound ternary complex. This binding inhibits the formation of thymidylate from uracil. Thymidylate is the necessary precursor of thymidine triphosphate (dTTP), one of four deoxyribonucleotides required for synthesis of DNA. Thus, a deficiency of thymidylate leads to depletion of dTTP, which inhibits cell division. Also, nuclear transcriptional enzymes can mistakenly incorporate FUTP in place of uridine triphosphate (UTP) during synthesis of RNA. Thus, RNA processing and protein synthesis are also disrupted.[44458]
Revision Date: 10/20/2025, 09:11:32 AMCapecitabine is administered orally. Plasma protein binding of capecitabine and its metabolites is less than 60% and is not concentration-dependent; the primary protein involved is human albumin (35%). The elimination half-lives of capecitabine and fluorouracil were approximately 0.75 hours. After administration of radiolabeled capecitabine, 96% of the administered dose was recovered in urine (3% as unchanged drug and 57% as the inactive metabolite alpha-fluoro-beta-alanine [FBAL]) and 2.6% in feces.[44458]
Affected cytochrome P450 (CYP) isoenzymes and drug transporters: CYP2C9
Capecitabine is a prodrug that is metabolized to fluorouracil. It is hydrolyzed by carboxylesterase and to 5'-deoxy-5-fluorocytidine (5'-DFCR), which is then converted to 5'-deoxy-5-fluorouridine (5'-DFUR) by cytidine deaminase. 5'-DFUR is subsequently hydrolyzed by thymidine phosphorylase to fluorouracil. More than 80% of fluorouracil is metabolized by dihydropyrimidine dehydrogenase (DPD) to 5-fluoro-5, 6-dihydro-fluorouracil (FUH2). The pyrimidine ring of FUH2 is then cleaved by dihydropyrimidinase to yield 5-fluoro-ureido-propionic acid (FUPA), which is then cleaved by beta-ureido-propionase to FBAL. Capecitabine is a weak inhibitor of CYP2C9.[44458]
Peak blood concentrations (Tmax) of capecitabine are achieved at a median of 1.5 hours after dosing, with peak fluorouracil levels occurring at a median of 2 hours; food delayed the Tmax of both capecitabine and fluorouracil by 1.5 hours. Food also reduces the extent of absorption of capecitabine, with mean Cmax and AUC decreased by 60% and 34%, respectively; the mean Cmax and AUC of fluorouracil were also reduced by 37% and 12%, respectively. The AUC of capecitabine and its metabolite, 5'-DFCR, are dose-proportional over a dosage range of 500 to 3,500 mg/m2 per day. However, increases in the AUC of 5'-DFUR and fluorouracil are greater than proportional to the increase in dose. The interpatient variability in Cmax and AUC of fluorouracil is greater than 85%. Following oral administration of capecitabine 7 days before surgery in patients with colorectal cancer, the median ratio of fluorouracil concentration in colorectal tumors to adjacent tissues was 2.9 (range, 0.9 to 8).[44458]
Administration of an aluminum hydroxide- or magnesium hydroxide-containing antacid immediately after a dose of capecitabine increased the Cmax and AUC of capecitabine by 35% and 16%, respectively; the Cmax and AUC of 5'DRCR were increased by 22% and 18%, respectively. The antacids did not have an observable effect on the Cmax or AUC of 5'-DFUR, fluorouracil, or FBAL.[44458]
The AUC and Cmax of capecitabine increased by 60% in patients with mild to moderate hepatic dysfunction compared to patients with normal hepatic function; the AUC and Cmax of fluorouracil were not affected. The effect of severe hepatic dysfunction on capecitabine pharmacokinetics is not known.[44458]
The AUC of capecitabine and its inactive metabolites 5'-DFUR and FBAL increased by 25%, 42%, and 85%, respectively, in patients with moderate renal impairment (CrCl 30 to 50 mL/min) compared to patients with a CrCl greater than 80 mL/min; there was no relevant change to the AUC of fluorouracil in these patients. The AUC of capecitabine and fluorouracil increased by 25% and 24%, respectively, in patients with severe renal impairment (CrCl less than 30 mL/min); the AUC of inactive metabolites 5'-DFUR and FBAL increased by 71% and 258% in these patients, respectively. Although no clinical experience using dialysis has been reported, dialysis may be of benefit in reducing circulating concentrations of the metabolite 5'-DFUR.[44458]
Age (range, 27 to 86 years) did not have a clinically meaningful effect on the pharmacokinetics of 5'-DFUR or fluorouracil; however, a 20% increase in age results in a 15% increase in the AUC of FBAL.[44458]
Gender did not have a clinically meaningful effect on the pharmacokinetics of 5'-DFUR, fluorouracil, or FBAL.[44458]
Race (White, Black, Other) did not have a clinically meaningful effect on the pharmacokinetics of 5'-DFUR, fluorouracil, or FBAL. However, in a separate study, Japanese patients (n = 18) had approximately a 36% lower Cmax and 24% lower AUC for capecitabine than White patients (n = 22); the Cmax and AUC for FBAL were also approximately 25% and 34% lower in Japanese patients compared with White patients, respectively. The clinical significance of these differences is unknown. There were no clinically significant differences in exposure to other metabolites (5'-DFCR, 5'-DFUR, and fluorouracil).[44458]
Approximately 3% to 5% of White populations have a partial DPD deficiency and 0.2% of White populations have complete DPD deficiency; DPD deficiency is estimated to be more prevalent in Black populations. There is insufficient information available to estimate the prevalence of DPD deficiency in other populations. Partial or complete DPD deficiency is associated with an increased risk of acute early-onset toxicities and serious adverse reactions.[44458]
Pregnancy should be avoided by females of reproductive potential during capecitabine treatment and for at least 6 months after the last dose. Although there are no adequately controlled studies in pregnant women, capecitabine can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. Women who are pregnant or who become pregnant while receiving capecitabine should be apprised of the potential hazard to the fetus. When capecitabine was given to pregnant animals during organogenesis, teratogenesis and embryolethality were observed in mice and embryolethality in monkeys at 0.2 and 0.6 times the exposure (AUC), respectively, in patients receiving the recommended dose. Teratogenic malformations in mice included cleft palate, anophthalmia, microphthalmia, oligodactyly, polydactyly, syndactyly, kinky tail, and dilation of cerebral ventricles.[44458]
Due to the potential for serious adverse reactions in nursing infants from capecitabine, advise women to discontinue breast-feeding during treatment and for 1 week after the final dose. It is not known whether capecitabine is present in human milk, although many drugs are excreted in human milk.[44458]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.