Chronic Bronchitis, Adult
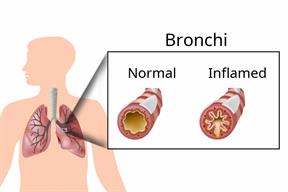
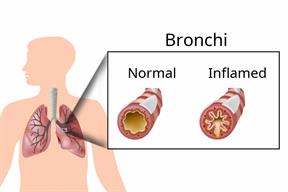
Chronic bronchitis is inflammation inside of the main airways (bronchi) that come off the windpipe (trachea) in the lungs. The swelling causes the airways to narrow and make more mucus than normal. This can make it hard to breathe and may cause coughing or noisy breathing (wheezing). This condition is a type of chronic obstructive pulmonary disease (COPD). Chronic bronchitis is often associated with other chronic respiratory conditions, such as emphysema, asthma, bronchiectasis, or cystic fibrosis.
Chronic bronchitis is a long-term (
chronic) condition. It is defined as a chronic cough with mucus (
sputum) production:
People with chronic bronchitis are more likely to get colds and other infections in the nose, throat, or airways.
What are the causes?
This condition is most often caused by:
A history of smoking.
Exposure to secondhand smoke or a smoky area for a long period of time.
Frequent lung infections.
Long-term exposure to certain fumes or chemicals that irritate the lungs.
What are the signs or symptoms?
Symptoms of chronic bronchitis may include:
A cough that brings up mucus (productive cough).
A whistling sound when you breathe (wheezing).
Shortness of breath.
Chest tightness or soreness.
Fever or chills.
Colds or respiratory infections that go away and return.
How is this diagnosed?
Your health care provider may diagnose this condition based on your signs and symptoms, especially if you have a cough that lasts a long time or keeps coming back.
This condition may be diagnosed based on:
How is this treated?
There is no cure for chronic bronchitis. Treatment may help control your symptoms. This includes:
Drinking fluids. This may help thin your mucus so it is easier to cough up.
Mucus-clearing techniques. Your health care provider will show you which techniques are best for you.
- Medicines such as:
Inhaled medicine (inhaler) to improve air flow in and out of your lungs.
Antibiotics to treat or prevent bacterial lung infections.
Mucus-thinning medicines.
Pulmonary rehabilitation. This is a program that helps you learn how to manage your breathing problem. The program may include exercise, education, counseling, treatment, and support.
Using oxygen therapy, if your blood oxygen level is very low.
Follow these instructions at home:
Medicines
-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
If you were prescribed an antibiotic medicine, take it as told by your health care provider. Do not stop taking the antibiotic even if you start to feel better.
Lifestyle

-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
-
Stay away from other people's smoke (secondhand smoke) and any irritants that make you cough more, such as chemical fumes.
-
Eat a healthy diet and get regular exercise. Talk with your health care provider about what activities are safe for you.
-
Return to normal activities as told by your health care provider. Ask your health care provider what activities are safe for you.
Preventing infections
-
Stay up to date on all immunizations, including the pneumonia and flu vaccines.
-
Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use hand sanitizer.
-
Avoid contact with people who have symptoms of a cold or the flu.
-
Keep your environment free from any known allergens such as dust, mold, pets, and pollen.
General instructions
Contact a health care provider if:
-
Your shortness of breath or coughing gets worse even when you take medicine.
-
Your mucus gets thicker or changes color.
-
You are not able to cough up your mucus.
-
You have a fever.
These symptoms may represent a serious problem that is an emergency. Do not wait to see if the symptoms will go away. Get medical help right away. Call your local emergency services (911 in the U.S.). Do not drive yourself to the hospital.
Summary
-
Chronic bronchitis is inflammation inside of the main airways (bronchi) that come off the windpipe (trachea) in the lungs. The swelling causes the airways to narrow and make more mucus than normal.
-
Chronic bronchitis is a long-term (chronic) condition. It is defined as a chronic cough with mucus (sputum) production for at least 3 months of the year for 2 years in a row.
-
If you were prescribed an antibiotic medicine, take it as told by your health care provider. Do not stop taking the antibiotic even if you start to feel better.
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.