ThisiscontentfromElsevier'sDrugInformation
Cyclophosphamide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
1 to 5 mg/kg orally daily for both initial and maintenance dosing. Other oral regimens have been studied. Adjust dosage in response to tumor activity and/or leukopenia. Additionally, drug dosages may need to be reduced when cyclophosphamide is administered in combination with other cytotoxic regimens.[61450]
40 to 50 mg/kg IV (total course dose) in divided doses given over 2 to 5 days. Other regimens include cyclophosphamide 10 to 15 mg/kg IV every 7 to 10 days or cyclophosphamide 3 to 5 mg/kg twice weekly.[61451]
400 mg/m2 daily IV over 1 hour on days 1 to 5 in combination with etoposide 150 mg/m2 daily IV over 2 hours on days 1 to 5 and clofarabine 40 mg/m2 daily IV over 2 hours on days 1 to 5 were given in a clinical study. Clofarabine was administered before cyclophosphamide and etoposide. In patients with a blast count greater than 30 x 109 cells/L, prophylactic steroids were given.[49907] Alternately, etoposide 100 mg/m2 daily IV over 2 hours on days 1 to 5 in combination with cyclophosphamide 440 mg/m2 daily IV over 1 hour on days 1 to 5, and clofarabine 40 mg/m2 daily IV over 2 hours on days 1 to 5 has been studied. Each drug was given daily for 4 days if administered as consolidation treatment.[49910]
40 mg/kg to 50 mg/kg IV in divided doses of a period of 2 to 5 days as an initial recommended dosage by the manufacturer for patients with no hematologic deficiency. Other regimens include 10 mg/kg to 15 mg/kg IV given every 7 to 10 days or 3 mg/kg to 5 mg/kg IV twice weekly. Although effective alone in susceptible malignancies, cyclophosphamide is more frequently used concurrently or sequentially with other antineoplastic agents. Consult the literature or study protocols for specific dosing.[47270]
500 mg/m2 IV in combination with epirubicin (75 mg/m2 IV) and fluorouracil (500 mg/m2 IV) on day 1, every 21 days for 4 cycles (FEC-75).[63560] [63561] Epirubicin dose adjustments for subsequent cycles are recommended by the manufacturer based on nadir platelet counts, ANC, or grade 3 to 4 toxicity.[41751] After completion of 4 cycles of FEC-75, administer paclitaxel 80 mg/m2 IV once weekly in combination with trastuzumab (4 mg/kg IV over 90 minutes on week 1, then 2 mg/kg IV over 30 minutes once weekly), every 21 days for 4 cycles (12 weeks). Surgery should be performed after completion of paclitaxel plus trastuzumab therapy, followed by trastuzumab 6 mg/kg IV every 3 weeks for a total of 52 weeks from the first preoperative dose. In a randomized, phase 3 clinical trial, neoadjuvant treatment with FEC-75 followed by paclitaxel plus trastuzumab (sequential therapy) resulted in similar rates of pathologic complete response (pCR), disease-free survival (DFS), and overall survival (OS) compared with paclitaxel plus trastuzumab followed by FEC-75 plus trastuzumab (concurrent therapy). Sequential therapy was better tolerated and had a lower incidence of cardiac adverse reactions.[63560] [63561]
100 mg/m2 orally on days 1 through 14, in combination with methotrexate 40 mg/m2 IV and fluorouracil 600 mg/m2 IV on day 1 and day 8, repeated every 28 days for 6 cycles.[61185] [47962] [47985] [51607]
500 mg/m2 IV plus doxorubicin (50 mg/m2 IV) then docetaxel (75 mg/m2 IV administered 1 hour later) every 3 weeks for 6 courses. Prophylactic colony stimulating factor support has been recommended to mitigate the risk of hematologic toxicities. Dosages should be adjusted based on toxicity. In an open-label randomized trial, 1,491 patients (stratified based on number of positive lymph nodes) were randomized to receive either docetaxel, doxorubicin, and cyclophosphamide (TAC regimen) or doxorubicin, fluorouracil, and cyclophosphamide (FAC regimen) every 3 weeks for 6 cycles. Results from the second interim analysis (median follow-up 55 months) indicated that the disease-free survival was significantly longer for the TAC regimen versus the FAC regimen. Grade 3 or 4 neutropenia was significantly greater with TAC (65.5% vs. 49.3%) as was febrile neutropenia (24.7% vs. 2.5%).[33124]
500 mg/m2 IV on day 1 in combination with fluorouracil (500 mg/m2 IV) and epirubicin (100 mg/m2 IV) (FEC regimen) every 21 days for 6 cycles. Alternatively, FEC may be administered for 3 cycles, then followed by docetaxel (100 mg/m2 IV) given every 21 days for 3 cycles (FEC-D regimen). A phase 3 trial of 1,944 patients with node-positive breast cancer compared the FEC-D regimen for 3 cycles to FEC for 6 cycles. The primary endpoint, 5-year disease-free survival, was significantly longer in the FEC-D arm (78.4% vs. 73.2 %); overall survival at 5 years was also significantly increased by FEC-D (90.7% vs. 86.7%). Grade 3 or 4 neutropenia and the incidence of nausea/vomiting were higher with FEC, whereas stomatitis, edema, and nail changes were more common with FEC-D.[34268]
A phase 3 study compared docetaxel (75 mg/m2) and cyclophosphamide 600 mg/m2 (TC regimen) given every 21 days for 4 cycles versus doxorubicin (60 mg/m2) and cyclophosphamide 600 mg/m2 (AC regimen) given every 21 days for 4 cycles. The primary endpoint of disease-free survival showed a significant advantage for the TC regimen at 5 years (86% vs. 80%). Extended follow-up after 7 years continued to show a significant benefit for DFS (81% vs. 75%) and overall survival (87% vs. 82%).[35039] Edema, myalgia and arthralgia were seen more frequently with the TC regimen and nausea and vomiting were seen more frequently with the AC regimen. No formal cardiac function comparison was performed.[33123]
600 mg/m2 IV on day 1 in combination with epirubicin 75 mg/m2 IV on day 1, every 3 weeks for 6 cycles. In a phase 3 trial, progression-free survival and overall survival were similar when compared to patients on epirubicin and paclitaxel.[49168]
500 mg/m2 IV on days 1 and 8 in combination with epirubicin 50 mg/m2 IV on days 1 and 8, plus fluorouracil 400 mg/m2 IV on days 1 and 8, every 3 to 4 weeks depending on patient recovery. In a phase 3 clinical trial, treatment was planned for 6 cycles, but was given up to 9 cycles in patients with a partial or complete response.[49142]
Cyclophosphamide has been included in various regimens. Dosages in combination with various other agents include 300 mg/m2 IV on days 1 and 8; 600 mg/m2 IV on day 1; 650 mg/m2 IV on days 1 and 8.
As part of a combination regimen, cyclophosphamide 70 mg/m2 PO every other day with vinblastine, procarbazine, and prednisone (PCVP).
650 mg/m2 IV on day 1 in combination with bleomycin (10 units/m2 IV on day 8), etoposide (100 mg/m2/day IV on days 1, 2, and 3), doxorubicin (25 mg/m2 IV on day 1), vincristine (1.4 mg/m2 (max: 2 mg) IV on day 8), procarbazine (100 mg/m2/day PO on days 1 through 7), and prednisone (40 mg/m2 PO on days 1 through 14). Cycles are repeated every 21 days for up to 8 cycles. Filgrastim was administered beginning on day 8 of each cycle and continued until the leukocyte count returned to normal in some clinical trials.[12501][40572] The escalated dose BEACOPP regimen includes cyclophosphamide 1200 mg/m2 IV on day 1 in combination with bleomycin (10 units/m2 IV on day 8), etoposide (200 mg/m2/day IV on days 1—3), doxorubicin (35 mg/m2 IV on day 1), vincristine (1.4 mg/m2 (max: 2 mg) IV on day 8), procarbazine (100 mg/m2/day PO on days 1 through 7), and prednisone (40 mg/m2 PO on days 1 through 14). Cycles are repeated every 21 days for up to 8 cycles. Filgrastim was administered beginning on day 8 of each cycle and continued until the leukocyte count returned to normal in some clinical trials.[12501][40572] The standard dose BEACOPP and escalated dose BEACOPP regimens have shown benefit for the treatment of advanced Hodgkin lymphoma in clinical trials.[12501][40572][40568] Escalated dose BEACOPP has shown a significantly better freedom from treatment failure at 10 years (82% vs. 70%, p < 0.0001) and overall survival at 10 years (86% vs. 80%, p = 0.0053) compared to standard dose BEACOPP.[49830] A regimen of 4 cycles of escalated dose BEACOPP followed by 4 cycles of standard dose BEACOPP has also been used in patients who achieve a complete response after the initial 4 cycles of escalated dose BEACOPP.[40568]
600 mg/m2 IV on days 1 and 2 in combination with brentuximab vedotin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1; doxorubicin 25 mg/m2 IV on days 1 and 2; vincristine 1.4 mg/m2 IV on day 8; etoposide 125 mg/m2 IV on days 1, 2, and 3; and prednisone 20 mg/m2 PO twice daily on days 1 to 7 repeated every 3 weeks for up to 5 cycles. Administer primary prophylaxis with a granulocyte colony-stimulating factor starting in cycle 1 due to the high incidence of febrile neutropenia.[45378]At a median follow-up time of 42.1 (range, 0.1 to 80.9) months, the 3-year event-free survival rate was significantly improved in patients (median age, 15.6 years; range, 3.4 to 21.99 years) with newly diagnosed, stage IIB with bulk tumor or stage IIIB, IVA, or IVB classic Hodgkin lymphoma who received brentuximab vedotin plus AVEPC compared with doxorubicin, bleomycin, vincristine, etoposide, prednisone, and cyclophosphamide (ABVE-PC) (92.1% vs. 82.5%; hazard ratio = 0.41; 95% CI, 0.25 to 0.67) in a multicenter, randomized, phase 3 trial (n = 587). The 3-year overall survival rates were 99.3% and 98.5% in the brentuximab vedotin plus AVEPC and ABVE-PC arms, respectively.[68172]
Most commonly, cyclophosphamide is given as part of combination regimens with total doses of up to 1,500 mg/m2 IV. In the ProMACE-CytaBOM regimen for Burkitt lymphoma, 650 mg/m2 is given once every 21 days. In the M-BACOD regimen for Burkitt lymphoma, 600 mg/m2 is given once every 21 days.
750 mg/m2 IV on day 1 in combination with doxorubicin 50 mg/m2 IV on day 1, vincristine 1.4 mg/m2 IV on day 1 (maximum dosage is 2 mg), and prednisone 50 mg/m2 PO once daily on days 1 to 5, repeated every 21 days. After 3 cycles, patients with a complete response received 3 additional cycles, patients with a partial response received 5 additional cycles, and patients with progressive disease discontinued treatment.[52334]
750 mg/m2 IV on day 1, rituximab 375 mg/m2 IV given on day 1 (or day 0), in combination with doxorubicin 50 mg/m2 IV on day 1, vincristine 1.4 mg/m2 IV (maximum dosage is 2 mg), and prednisone 100 mg/m2 PO on days 1, 2, 3, 4, and 5 (R-CHOP regimen) repeated every 3 weeks for 6 to 8 cycles has been studied in previously untreated and previously treated patients with follicular lymphoma (FL) in randomized, phase 3 trials.[47202] [47203] [47204]
750 mg/m2 IV on day 1, rituximab 375 mg/m2 IV on day 1, doxorubicin 50 mg/m2 IV on day 1, vincristine 1.4 mg/m2 (maximum dosage is 2 mg) IV on day 1, and prednisone 40 or 100 mg/m2 PO daily on days 1, 2, 3, 4, and 5 (R-CHOP) repeated every 21 days for up to 8 cycles in patients aged 60 years and older with previously untreated diffuse large B-cell lymphoma in randomized, clinical trials.[34649][31968] In a randomized, phase 3 study in 632 patients aged 60 years or older (range 60 to 92 years), the 3-year failure-free survival rate was significantly higher with R-CHOP compared with CHOP (53% vs. 46%; hazard ratio [HR] = 0.78; 95% CI, 0.61 to 0.99; p = 0.04) at a median follow-up of 3.5 years. Overall survival (OS) was not significantly improved in the R-CHOP arm (HR = 0.83; 95% CI, 0.63 to 1.09).[34649] In another randomized trial, the median progression-free survival (PFS) (4.8 vs. 1.2 years; p less than 0.0001) and OS (8.4 vs. 3.5 years; p less than 0.0001) times were significantly improved with R-CHOP compared with CHOP in 399 patients aged 60 to 75 years. The 10-year PFS rates were 36.5% and 20.1% in the R-CHOP and CHOP arms, respectively, and the 10-year OS rates were 43.5% and 27.6%, respectively.[47312]
750 mg/m2 IV on day 1 in combination with polatuzumab vedotin 1.8 mg/kg IV, rituximab 375 mg/m2 IV, and doxorubicin 50 mg/m2 IV on day 1 plus prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 repeated every 21 days for 6 cycles has been evaluated in a randomized, double-blind, placebo-controlled, phase 3 trial (n = 879; the POLARIX trial). Rituximab 375 mg/m2 IV was continued for 2 additional cycles of therapy (cycles 7 and 8).[67350]
NOTE: Cyclophosphamide is approved for the treatment of CLL[49678]; however, all components of combination regimens may not have been evaluated by the FDA for the treatment of CLL.
250 mg/m2/day IV on days 1 to 3 in combination with fludarabine 25 mg/m2/day IV on days 1 to 3 repeated every 28 days for up to 6 cycles was evaluated in randomized, phase III studies.[50268] [41970] In 1 study, patients with severe lymphopenia for longer than 7 days received prophylactic antibiotics.[41970] In another study, patients received prophylactic antibiotic therapy with cotrimoxazole for 6 months after treatment and allopurinol daily for 7 days during the first 2 to 3 courses; prophylactic antiviral therapy was recommended.[50268]
150 mg/m2/day PO on days 1 to 5 plus fludarabine 24 mg/m2/day PO on days 1 to 5 repeated every month for up to 6 cycles was evaluated in a randomized, phase III study. Patients received prophylactic antibiotic therapy with cotrimoxazole for 6 months after treatment and allopurinol daily for 7 days during the first 2 to 3 courses; prophylactic antiviral therapy was recommended.[50268] No significant differences in efficacy was found between patients who received PO or IV cyclophosphamide plus fludarabine therapy in a retrospective analysis in 65 patients.[50269]
250 mg/m2/day on days 1 to 3 in combination with fludarabine 25 mg/m2/day on days 1 to 3 and rituximab 375 mg/m2 IV on day 0 (the day prior to fludarabine and cyclophosphamide (FC) on cycle 1, then 500 mg/m2 IV on day 1 on cycles 2 to 6 repeated every 28 days (R-FC) for 6 cycles has been studied in randomized, phase III trials. The addition of rituximab to fludarabine and cyclophosphamide (mean of 5.2 cycles) resulted in a significantly improved progression-free survival (PFS) time (primary endpoint) compared with FC alone (51.8 vs. 32.8 months; p < 0.0001) in 817 previously untreated CLL patients in a multinational, randomized, phase III trial. The 3-year PFS (65% vs. 45% hazard ratio (HR) = 0.56; 95% CI, 0.46 to 0.69) and overall survival (OS) (87% vs. 83%; HR = 0.67; 95% CI, 0.48 to 0.92) rates were also significantly improved with R-FC. Grade 3 or 4 neutropenia and leukopenia occurred significantly more often with R-FC therapy.[41970] The median PFS time (primary endpoint) was 30.6 months with R-FC compared with 20.6 months with FC (HR = 0.65; 95% CI, 0.51 to 0.82; p < 0.001) in another multinational, randomized, phase III trial in 552 CLL patients who had relapsed or refractory disease following 1 prior line of therapy. All patients in this study received tumor lysis and antibiotic/antiviral prophylaxis. At a median follow-up time of 25 months, the median OS was not significantly different between treatment arms (R-FC, median time not reached; FC, 52 months). There were more treatment-related deaths reported with R-FC therapy (19 vs. 14 deaths).[40235]
250 mg/m2/day IV over 30 to 60 minutes on days 1 to 3 plus cladribine repeated every 28 days for a median of 6 cycles[43762] and cyclophosphamide 650 mg/m2 IV on day 1 plus cladribine repeated every 28 days for a median of 3 cycles[50166] were evaluated in 2 randomized, phase III trials. The cladribine dosage was 0.12 mg/kg/day IV on days 1 to 3 in both studies.
650 mg/m2 IV on day 1 in combination with cladribine 0.12 mg/kg/day IV over 2 hours on days 1 to 3 and mitoxantrone 10 mg/m2 IV on day 1 repeated every 28 days for up to 6 cycles (median, 3 cycles) has been evaluated in a randomized, phase III trial.[50166]
600 mg/m2 IV on day 1 in combination with pentostatin (2 mg/m2 or 4 mg/m2 IV on day 1) and rituximab (375 mg/m2 IV on day 1) repeated every 21 days for 6 or 8 cycles has been studied in clinical trials.[36901][50242] The first cycle rituximab administration varied in these studies with 1 study giving rituximab 100 mg/m2 on day 1 and 375 mg/m2 on days 3 and 5 on cycle 1[36901] and another study administering rituximab 100 mg/m2 on day 8 and 275 mg/m2 on day 9 on cycle 1.[50242] Patients received prophylactic antibiotic and/or antiviral therapy in these studies.
200 to 300 mg/m2 IV on day 1 in combination with carmustine, prednisone, and either doxorubicin or cisplatin. As part of the M-2 protocol, cyclophosphamide is given as 10 mg/kg IV on day 1 in combination with vincristine, carmustine, melphalan, and prednisone.
Cyclophosphamide 125 mg/m2 PO on days 1 to 4 has been given in combination with vincristine, melphalan, and prednisone (VMCP regimen).
Total doses of 600 to 1000 mg/m2 IV in combination with doxorubicin, cisplatin, and/or other agents.
100 to 150 mg/m2 PO once daily for 14 days in combination with doxorubicin, cisplatin, fluorouracil, or other agents.
40 mg/kg IV and vincristine (0.05 mg/kg IV) every 3 weeks for 57 weeks. Cyclophosphamide has been used in various combination regimens with doxorubicin, cisplatin, etoposide, and/or vincristine.
Although FDA-approved for AML and CML, cyclophosphamide does not have extensive activity in primary myeloid malignancies and has generally been replaced with more effective agents (e.g., cytarabine/anthracyclines for AML and hydroxyurea/interferon alfa for CML). Cyclophosphamide may be used as part of conditioning regimens prior to bone marrow transplantation (BMT) in patients with AML or CML. Common doses of cyclophosphamide for conditioning regimens include 120 to 200 mg/kg IV divided as 60 mg/kg/day IV for 2 days or 50 mg/kg/day IV for 4 days or 3.6 to 6 g/m2 IV divided over 3 to 4 days. Doses greater than 120 mg/kg over 2 days (i.e., more than 60 mg/kg/day for 2 days) are associated with an increased risk of severe cardiac toxicity.
Methotrexate and dactinomycin are FDA approved for the treatment of trophoblastic disease as components of a multi-drug regimen.[60517] [63445]
600 mg/m2 IV on day 8 in combination with etoposide, methotrexate, leucovorin, actinomycin D, and vincristine (EMA-CO regimen), repeated every 2 to 3 weeks depending on toxicity. Multiple studies have been reported with cure rates ranging from 70% to 90% in women with high-risk gestational trophoblastic disease. Results are typically better in women who receive EMA-CO as primary therapy and in women without metastatic disease. Consider growth-factor support to maintain dose-intensity and prevent hematological toxicity. Complete response is typically defined as 3 consecutive weekly human chorionic gonadotropin (hCG) levels that are undetectable or less than the upper limit of normal. In studies, treatment was continued for 2 to 3 additional courses after complete hCG response.[33966] [33967]
600 mg/m2/day IV on days 1 and 2, or on days 1, 2, and 3 in combination with bleomycin and dactinomycin (BCD regimen) has been incorporated into multiple treatment protocols for osteogenic sarcoma. In the POG-8651 protocol, 106 patients (younger than 30 years old) with previously untreated nonmetastatic high-grade osteogenic sarcoma were randomized to receive multiagent chemotherapy either before or after surgical resection. Multiagent chemotherapy consisted of 3 days of BCD each cycle in sequence with doxorubicin and cisplatin, and high-dose methotrexate. Event-free survival (EFS), the primary endpoint, was not significantly different between the treatment arms and reached 69% at 5 years in the postoperative group.[34600] In a comparison of the Memorial Sloan-Kettering Cancer Center T-10 and T-12 protocols, 73 patients (ages 4.6 to 36.4 years) with previously untreated, high-grade osteogenic sarcoma received BCD on days 1 and 2 of each cycle as part of a multiagent chemotherapy regimen in sequence with doxorubicin and cisplatin, high-dose methotrexate, and surgical resection. The 5-year EFS was 78% and 73% in the T-12 and T-10 protocols, respectively.[34668] The use of BCD alone has also been studied in 8 pediatric patients (ages 9.1 to 16.4 years old) with previously treated metastatic osteogenic sarcoma. Patients received 1 to 5 courses of BCD. No tumor regression could be measured for any of the patients, and progressive tumor enlargement was demonstrated in 2 patients.[34621]
Dosage is not established. In a phase II trial of newly diagnosed metastatic rhabdomyosarcoma, 61 patients younger than 21 years received cyclophosphamide 250 mg/m2/day IV on days 1 to 5 immediately followed by topotecan (0.75 mg/m2/day IV on days 1 to 5) (TC); repeated every 21 days for 2 cycles. To prevent hemorrhagic cystitis, mesna 250 mg/m2/day IV on days 1 to 5 was given immediately prior to cyclophosphamide administration. If objective improvement occurred (CR or PR), patients continued to receive TC in combination with vincristine (VTC) alternating with vincristine, dactinomycin, and cyclophosphamide (VAC) during weeks 6 to 41. The overall response rate to TC was 46% (3% CR, 43% PR, 23% objective improvement, and 10% no response). Of treated patients, 70% were considered responders and received alternating VTC/VAC therapy. After 41 weeks of therapy, 34% achieved a CR. Disease-free survival at 3 years was 10%, while 3-year overall survival was 20%. No unexpected toxicities occurred during treatment.[28682] In a phase III clinical trial, VAC/VTC was compared to VAC in 617 patients with previously untreated intermediate-risk rhabdomyosarcoma. The primary endpoint, failure-free survival (FFS), was not significantly different between the 2 treatment arms (68% VAC/VTG vs. 73% VAC, p = 0.3) when measured at 4 years. In addition, the estimated overall survival (OS) at 4 years was 79% for both treatment groups. Neutropenia occurred more significantly more often in patients who received VAC only (78% vs. 85%, p = 0.04).[43256]
150 mg/m2/day PO days 1 to 7 in combination with doxorubicin (35 mg/m2 IV on day 8) every 21 days for 5 cycles. In a clinical trial, 135 patients with hyperdiploid tumors exhibited a complete response rate of 67%. Patients with diploid tumors or patients with hyperdiploid tumors who had a suboptimal response to treatment were switched to cisplatin and etoposide.[33842]
70 mg/kg/day IV infusion with hydration on days 1 and 2 in combination with doxorubicin and vincristine every 21 days for courses 1, 2, 4, and 6; alternating with cisplatin and etoposide every 21 days for courses 3, 5, and 7. Mesna may be given as 24-hour infusions to start with cyclophosphamide at an equal dose. This dose of cyclophosphamide was studied in 86 patients with high-risk neuroblastoma. Complete responses or very good partial responses were seen in 79% of patients. Comparable response rates were seen between patients who received 5 or 7 cycles of treatment.[33843]
10 mg/kg/day IV on days 1 to 5 in combination with doxorubicin and vincristine given every 21 days for 2 courses; preceded by 2 courses of carboplatin and etoposide. NOTE: Final doses of all agents should be reduced by 30% in neonates (see below). In a study of 52 patients with unresectable localized neuroblastoma, an overall response rate of 66% was observed. Surgical resection was attempted in all patients and considered complete in 66%.[33844]
7 mg/kg/day IV on days 1 to 5 in combination with doxorubicin and vincristine given every 21 days for 2 courses; preceded by 2 courses of carboplatin and etoposide. In a study of 52 patients with unresectable localized neuroblastoma, an overall response rate of 66% was observed. Surgical resection was attempted in all patients and considered complete in 66%.[33844]
Cyclophosphamide has been given in combination with etoposide, carboplatin, and doxorubicin in the following fashion. Cycles 1 and 7: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg/day in children less than 12 kg) plus etoposide 120 mg/m2/day IV on days 1, 2, and 3 (4 mg/kg/day in children less than 12 kg). Cycles 2 and 6: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg/day in children less than 12 kg) plus cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg/day in children less than 12 kg), and doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg/day in children less than 12 kg). Cycles 3 and 5: Cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg/day in children less than 12 kg) plus etoposide 120 mg/m2/day IV on days 1, 2, and 3 (4 mg/kg/day in children less than 12 kg). Cycle 4: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg/day in children less than 12 kg) plus etoposide 120 mg/m2/day IV on days 1, 2, and 3 (4 mg/kg/day in children less than 12 kg), and doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg/day in children less than 12 kg). Cycle 8: Cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg/day in children less than 12 kg) plus doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg/day in children less than 12 kg). All cycles given at 3 week intervals. Patients with favorable biologic features received 4 cycles; if incomplete response after 4 cycles, patients given an additional 4 cycles. Patients with unfavorable biologic features received 8 cycles. Infants younger than 60 days received granulocyte colony-stimulating factor after each cycle.[49848]
Multiple dosage regimens have been studied. Cyclophosphamide 750 mg/m2 IV on day 1 in combination with doxorubicin 40 mg/m2 IV on day 1 and vincristine 1.2 mg/m2 (maximum dose is 2 mg) IV on day 1, every 4 weeks for 4 cycles.[51164] Cyclophosphamide 800 mg/m2 IV on day 1 in combination with doxorubicin 50 mg/m2 IV on day 1 and vincristine 1.4 mg/m2 (maximum dosage is 2 mg) IV on day 1, every 3 to 4 weeks for 4 cycles.[51165] Cyclophosphamide 1,000 mg/m2 IV on day 1 in combination with doxorubicin 40 mg/m2 IV on day 1 and vincristine 1 mg/m2 (maximum dosage is 2 mg) IV on day 1, every 3 weeks for 6 cycles.[51166]
Cyclophosphamide 1,000 mg/m2 IV on day 1 in combination with doxorubicin 45 mg/m2 IV on day 1 and etoposide 100 mg/m2/day IV on days 1, 2, and 3 every 3 weeks for 5 cycles.[51057][50310]
4 g/m2 IV over 6 hours on day 1 along with mesna 3 g/m2 IV, then 500 mg every 3 hours PO/IV for 8 doses and prednisone 2 mg/kg orally on days 1 to 4. At 36 to 48 hours after completion of cyclophosphamide, patients began G-CSF 10 mg/kg subcutaneously per day until recovery.[49936]
Cyclophosphamide 60 mg/kg/day IV on 2 consecutive days (days -7 and -6) in combination with fludarabine 25 mg/m2/day IV for 5 consecutive days (days -5 to -1). Cyclosporine alone or in combination with mycophenolate was used for GVHD prevention. For obese patients (more than 120% ideal body weight), chemotherapy dosing weight was calculated by using the formula: dosing weight = ideal body weight + (actual/ideal weight)/2.[50099]
Fludarabine 30 mg/m2/day IV for 5 consecutive days (days -7 to -3) in combination with cyclophosphamide 1 g/m2/day IV on 3 consecutive days (days -5 to -3). Low dose methotrexate was given in combination with tacrolimus or cyclosporine for the prevention of GVHD. Infection prophylaxis with fluconazole, acyclovir, and TMP/SMX was given per institutional standards.[50307]
Busulfan 1 mg/kg PO 4 times a day on days -7 to -4 (16 mg/kg PO total dose) in combination with cyclophosphamide 60 mg/kg/day IV on days -3 and -2 (120 mg/kg IV total dose). Cyclosporine and prednisone were used for the prevention of GVHD. Cyclophosphamide was dosed on ideal weight, all other agents were dosed on actual weight.[44348]
Doses of 1 to 2 mg/kg/day PO have been given for periods as long as 2 years. Cyclophosphamide is usually used as a second-line agent in patients who have failed other immunosuppressant therapy.
2 mg/kg PO once daily has been recommended in patients who fail initial treatment with prednisone or do not tolerate corticosteroid treatment. Dosage is adjusted according to WBC count. Treatment is indicated in symptomatic patients with a platelet count less than 50,000/mm3.[23970]
500 mg IV every 3 to 4 weeks. Cyclophosphamide has also been used as part of combination chemotherapy with prednisone and etoposide or vincristine with or without procarbazine in patients with severe refractory ITP.[24153]
Initially, 1 to 1.5 mg/kg/day PO; may increase in 25 mg increments every 3 to 4 weeks up to 2 mg/kg/day. Alternatively, 800 to 1,400 mg IV monthly with IV hydration for 6 to 9 months. The goal is to avoid neutropenia. In 1 series, compared with patients who did not receive cyclophosphamide for alveolitis, patients treated with cyclophosphamide had improvement in FVC and diffusing capacity and an increased survival.[26574] In another study, receipt of cyclophosphamide 1 mg/kg/day PO initially, then increased monthly by 25 mg up to 2 mg/kg/day, for 12 months led to a percent of predicted FVC difference of -1 +/- 0.92 from baseline in patients with limited or diffuse systemic scleroderma. In contrast, the percent of predicted FVC difference for placebo recipients was -2.6 +/- 0.9 from baseline. Survival or long-term adverse effects such as malignancy were not determined.[32354]
2 mg/kg/day orally for 8 to 12 weeks; the maximum cumulative dose is 168 mg/kg. Treatment beyond 90 days increases the probability of sterility in males.[49678]
1.5 to 2.5 mg/kg/day PO in combination with other agents; however, doses of less than 1.0 mg/kg/day have not been consistently effective.
0.5 to 1 g/m2 IV monthly for 6 months then every 2 to 3 months in combination with other agents.
Doses of cyclophosphamide 200 mg/kg (total dose) IV or 4 g/m2 IV followed by hematopoietic growth factors and peripheral stem cell transplantation have been studied in small phase I/II trials. Responses have been noted for more than 19 months.[26575] [26576]
1 to 2 mg/kg/day PO in addition to corticosteroids, especially if there is major organ system involvement. Doses can be increased by 25 mg/day every 2 weeks until clinical response or toxicity is seen. Therapy should be continued for 12 to 18 months following complete remission. Early addition of cyclophosphamide is appropriate in Wegener's granulomatosis and polyarteritis nodosa.
0.5 to 1 g/m2 IV monthly in addition to corticosteroids, especially if there is major organ system involvement. Early addition of cyclophosphamide is appropriate in Wegener's granulomatosis and polyarteritis nodosa. Other studies have described lower pulse doses of cyclophosphamide 500 mg IV weekly (250 mg IV in patients with creatinine clearance less than 30 mL/min) in combination with mesna.[24154]
2 mg/kg/day PO to a maximum dose of 150 mg/day PO. Dosing should begin at 25 to 50 mg/day PO. Increase gradually, by 25-mg increments, every 7 to 14 days until the maximum dose is reached. Guidelines suggest treatment should be in combination with corticosteroids and for a minimum duration of 6 months. Objective responses may not be noted until the patient has received 3 months or more of therapy. Exact duration of treatment and need for long-term maintenance should be individualized based on clinical response and tolerance to therapy.[26496]
500 to 1,800 mg IV given every 2 to 4 weeks has been tried in open trials of refractory patients with generally unimpressive results. The poor results in these trials may reflect the late course disease when treatment was started rather than a failure of cyclophosphamide therapy.[26496]
500 mg/m2 IV on day 1 plus doxorubicin 50 mg/m2 IV on day 1 and cisplatin 50 mg/m2 IV on day 1 (with 1 L hydration before and after chemotherapy) repeated every 21 days (PAC regimen) for up to 8 cycles (median of 7 cycles) in patients with previously untreated, unresectable, extensive-stage thymoma [41507] or for 2 or 4 cycles (median of 4 cycles; range, 1-7 cycles) followed by radiotherapy in patients with previously untreated, unresectable, limited-stage thymoma who had stable disease or better[47366] have been evaluated in nonrandomized studies with favorable overall response rates and overall survival rates. Additionally, multimodality treatment with 3 cycles of cyclophosphamide 500 mg/m2 IV on day 1, cisplatin 30 mg/m2/day IV on days 1 to 3, doxorubicin 30 mg/m2/day continuous IV infusion over 24 hours on days 1 to 3, and prednisone 100 mg PO on days 1 to 5 repeated every 3 to 4 weeks followed by surgery and radiation therapy and then consolidation chemotherapy with cyclophosphamide, cisplatin, and doxorubicin given at 80% of the original doses and prednisone (given at 100%) repeated every 3 to 4 weeks for 3 cycles has also been evaluated in another nonrandomized study.[41508]
700 mg/m2 IV on day 4 plus cisplatin 50 mg/m2 IV on day 1, doxorubicin 40 mg/m2 IV on day 1, and vincristine 0.6 mg/m2 IV on day 3 repeated every 3 weeks (median of 5 cycles, range, 3-7 cycles) resulted in a favorable overall response rate in a nonrandomized study of 37 patients.[41511]
100 mg/m2 orally twice daily on days 1 to 5 (total dose of 1,000 mg/m2/cycle) in combination with rituximab 375 mg/m2 IV on day 1 and dexamethasone 20 mg IV on day 1 repeated every 21 days for 6 cycles was evaluated in a single-arm, phase II trial.[61073]
Oral cyclophosphamide in combination with lenalidomide (15 mg PO daily on days 1 to 21) and dexamethasone (40 mg PO on days 1, 8, 15, and 22) repeated every 28 days has been evaluated in nonrandomized, phase 2 studies. Treatment duration, the cyclophosphamide dosage, and thromboprophylaxis recommendations varied in these studies.[61322] [61323] In 1 study, cyclophosphamide (500 mg PO on days 1, 8, and 15), lenalidomide, and dexamethasone therapy was given for a maximum of 9 cycles; treatment was discontinued after cycle 6 if a complete response or partial response/very good partial response plus organ response was obtained. In this study, patients with fluid retention over 3% of body weight despite optimal diuretic use received a lower dose of dexamethasone (20 mg once weekly).[61322] In another study, cycles of cyclophosphamide (300 mg/m2 PO on days 1, 8, and 15), lenalidomide, and dexamethasone were continued until disease progression, unacceptable toxicity, or up to 2 years; however, cyclophosphamide was given for up to a maximum of 12 cycles only.[61323]
300 mg/m2 IV on days 1 and 8 for cycles 1 to 6, then cyclophosphamide 300 mg/m2 IV on day 1 for cycles 7 to 12 in combination with lenalidomide (15 mg PO daily on days 1 to 21 for 12 cycles) and dexamethasone (20 mg PO on days 1, 2, 3, 4, 9, 10, 11, and 12 for cycles 1 to 6; then 20 mg PO on days 1, 2, 3, and 4 for cycles 7 to 12) repeated every 28 days was evaluated in a nonrandomized, phase 2 trial. Maintenance therapy with lenalidomide and dexamethasone was administered for 3 additional years or until disease progression. Patients with cardiac stage III had an upfront dose modification of dexamethasone.[61321]
300 mg/m2 (maximum dose of 500 mg) IV or PO in combination with bortezomib 1.3 mg/m2 subcutaneously and dexamethasone 40 mg IV/PO each given weekly on days 1, 8, 15, and 22 repeated every 28 days for a maximum of 6 cycles (VCd) plus up to 2 years of subcutaneous daratumumab; hyaluronidase (D-VCd) was evaluated in transplant eligible, newly diagnosed light-chain amyloidosis patients in a randomized, phase 3 trial (n = 388; the ANDROMEDA trial). The dose of dexamethasone was reduced to 20 mg in patients older than 70 years or who had a body mass index less than 18.5, hypervolemia, poorly controlled diabetes mellitus, or prior intolerance to steroid therapy. Daratumumab; hyaluronidase was administered as follows: 1,800 mg daratumumab and 30,000 units hyaluronidase subcutaneously weekly on weeks 1 to 8 (8 doses), 1,800 mg daratumumab and 30,000 units hyaluronidase every 2 weeks on weeks 9 to 24 (8 doses), and then 1,800 mg daratumumab and 30,000 units hyaluronidase every 4 weeks starting on week 25 until disease progression or for a maximum of 2 years.[65366] At a median follow-up time of 11.4 (range, 0.03 to 21.3) months, the hematologic complete response (hemCR) rate was significantly improved (53.3% vs. 18.1%; relative risk ratio = 2.9; 95% CI, 2.1 to 4.1; p less than 0.001) in patients who received D-VCd compared with VCd in the ANDROMEDA trial. The median time to hemCR was 60 and 85 days in the D-VCd and VCd arms, respectively.[66968]
2 mg/kg/dose IV once daily may be considered in highly refractory children who have failed to respond to a second IVIG infusion, an extended course of steroids, or infliximab.[17314] [61950]
750 mg/m2 IV on day 1 in combination with brentuximab vedotin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1, doxorubicin 50 mg/m2 IV on day 1, and prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 given every 21 days for 6 to 8 cycles of therapy. The progression-free survival (PFS) time (evaluated via an independent review facility) was significantly improved in patients with CD30-expressing sALCL or peripheral T-cell lymphoma who received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (CHP) compared with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (48.2 months vs. 20.8 months; hazard ratio (HR) = 0.71; 95% CI, 0.54 to 0.93) in a multicenter, randomized, double-blind, phase 3 trial (the ECHELON-2 trial; n = 452). Overall survival was also significantly improved in the brentuximab vedotin-containing arm (HR = 0.66; 95% CI, 0.46 to 0.95). In patients with sALCL (n = 314; anaplastic lymphoma kinase (ALK)-negative sALCL, 48%; ALK-positive sALCL, 22%), the PFS times were 55.7 months and 54.2 months in patients who received brentuximab vedotin plus CHP and CHOP, respectively (HR = 0.59; 95% CI, 0.42 to 0.84).[45378]
750 mg/m2 IV on day 1 in combination with brentuximab vedotin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1, doxorubicin 50 mg/m2 IV on day 1, and prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 given every 21 days for 6 to 8 cycles of therapy. The progression-free survival time (evaluated via an independent review facility) was significantly improved in patients with CD30-expressing systemic anaplastic large-cell lymphoma (sALCL) or PTCL who received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (CHP) compared with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (48.2 months vs. 20.8 months; hazard ratio (HR) = 0.71; 95% CI, 0.54 to 0.93) in a multicenter, randomized, double-blind, phase 3 trial (the ECHELON-2 trial; n = 452). Overall survival was also significantly improved in the brentuximab vedotin-containing arm (HR = 0.66; 95% CI, 0.46 to 0.95). In this trial, 70% of patients had sALCL and 30% of patients had PTCL (e.g., including PTCL not otherwise specified (16%), angioimmunoblastic T-cell lymphoma (12%), adult T-cell leukemia/lymphoma (2%), and enteropathy-associated T-cell lymphoma (less than 1%)).[45378]
600 mg to 1 g/m2 IV as a single dose or once monthly for up to 6 months.[67800] [67918] [67919] [67920] [67921]
500 mg to 1 g/m2 (Max: 1.5 g/dose) IV once monthly for up to 6 months.[67917]
1.5 to 2 mg/kg/dose PO once daily or 50 to 100 mg/day PO in 1 or 2 divided doses for several months.[68308] [68322] [70295]
1.5 to 2 mg/kg/dose PO once daily for several months.[68308] [68313] [68314] [68317] [68322] [70295]
500 to 1,000 mg/m2/dose IV every 4 weeks for several months.[68308] [68311] [68322] [70295]
500 to 1,000 mg/m2/dose IV every 4 weeks for several months.[68308] [68311] [68313] [68314] [68317] [68322] [68338] [68339] [70295]
50 to 100 mg PO once daily or 1 to 2 mg/kg/dose PO once daily.[70696]
50 mg/kg/dose IV once daily for 4 days or 1 g IV once monthly for 4 months. Use ideal body weight to calculate weight-based dose.[70696]
750 to 1,000 mg/m2/dose IV once monthly for 6 months.[70847]
500 mg IV every 2 weeks for 6 doses.[70847] [71743]
500 to 1,000 mg/m2/dose IV once monthly for 6 months.[70847] [71743]
500 mg/m2/dose IV once monthly for 6 months. Increase the dose based on clinical response. Max: 1,500 mg/dose.[65218] [71748]
1 to 1.5 mg/kg/day (Max: 150 mg/day) PO for 2 to 6 months.[71743]
1 mg/kg/day PO for 3 to 6 months.[67356] [71444] [71445]
1.5 mg/kg/day PO for 3 to 6 months.[67356] [71444] [71445]
2 mg/kg/day or less PO for 3 to 6 months.[67356] [71444] [71445]
10 mg/kg/dose (Max: 1,200 mg/dose) IV every 2 weeks for 3 doses, then 10 mg/kg/dose (Max: 1,200 mg/dose) IV every 3 weeks for 3 to 7 doses.[67356] [71444] [71445]
12.5 mg/kg/dose (Max: 1,200 mg/dose) IV every 2 weeks for 3 doses, then 12.5 mg/kg/dose (Max: 1,200 mg/dose) IV every 3 weeks for 3 to 7 doses.[67356] [71444] [71445]
15 mg/kg/dose (Max: 1,200 mg/dose) IV every 2 weeks for 3 doses, then 15 mg/kg/dose (Max: 1,200 mg/dose) IV every 3 weeks for 3 to 7 doses.[67356] [71444] [71445]
15 mg/kg/dose (Max: 1,200 mg/dose) IV every 2 weeks for 3 doses, then 15 mg/kg/dose (Max: 1,200 mg/dose) IV every 3 weeks for 3 to 6 doses.[71444] [71446] Alternatively, 750 mg/m2/dose IV every 4 weeks for 4 to 7 doses.[71446]
2 mg/kg/day or less PO for at least 18 months. Consider longer duration of therapy in individuals with relapsing disease or at high risk for relapse. Max cumulative dose: 36 g.[71444] [71445]
500 mg IV once monthly for at least 18 months. Consider longer duration of therapy in individuals with relapsing disease or at high-risk for relapse. Max cumulative dose: 36 g.[24154] [71444] [71445]
1 to 2 mg/kg/dose PO once daily. Dose range: 50 to 200 mg/day.[71494] [71548] [71549]
1 to 1.5 mg/m2 IV divided over 4 to 5 days once monthly for 6 months, then 1 to 1.5 g/m2 IV divided over 4 to 5 days every 3 months based on clinical response and tolerability.[71550] Alternatively, 0.75 g/m2/dose (Max: 1,500 mg/dose) IV once monthly for 6 months, or 500 mg/m2/dose IV once monthly for 6 months, then 500 mg/m2/dose every other month for a total of 9 doses.[71494] [71551] [71552] Initiate maintenance immunotherapy 4 to 6 weeks after last cycle.[71551]
50 mg/kg/dose IV once daily for 4 days.[71494] [71553] Alternatively, 30 to 50 mg/kg/dose IV once monthly for at least 6 months.[71497]
15 mg/kg/dose IV once daily for 2 days.[71529] [71530] [71531] [71532] [71533] May repeat dose after 2 weeks if the partial pressure of oxygen is less than 60 mmHg and white blood cell count is more than 3,000/mm3.[71532] [71533]
50 mg PO once daily.[71628] [71629]
500 to 750 mg IV once monthly.[71628] [71629]
1 to 2 mg/kg/dose PO once daily, initially. Adjust dose based on clinical response and tolerability. Max: 3 mg/kg/day or 150 mg/day.[71021] [71063]
1 to 2 mg/kg/dose PO once daily, initially. Adjust dose based on clinical response and tolerability. Max: 3 mg/kg/day or 150 mg/day.[71021] [71063]
750 to 1,000 mg/m2/dose IV every 1 to 4 weeks. Adjust dose based on clinical response and tolerability.[71021] [71063] [71697]
750 to 1,000 mg/m2/dose IV every 1 to 4 weeks. Adjust dose based on clinical response and tolerability.[71021] [71063]
Management of Treatment-Related Toxicities
Hematologic Toxicity
Urotoxicity
Oncology: The maximum dose varies and is indication- and protocol-specific.
Oncology: The maximum dose varies and is indication- and protocol-specific.
Oncology: The maximum dose varies and is indication- and protocol-specific.
Oncology: The maximum dose varies and is indication- and protocol-specific.
Baseline Hepatic Impairment
Baseline Renal Impairment










Cyclophosphamide is a bifunctional alkylating agent related to mechlorethamine (nitrogen mustard). It is indicated for the treatment of adult and pediatric patients with various malignant diseases including acute lymphocytic leukemia, breast cancer, malignant lymphomas, ovarian cancer, multiple myeloma, leukemias, mycosis fungoides, neuroblastoma, and retinoblastoma. It is also indicated for the treatment of biopsy proven minimal change nephrotic syndrome in pediatrics patients who failed to adequately respond to or are unable to tolerate adrenocorticosteroid therapy. The safety and effectiveness of cyclophosphamide for the treatment of nephrotic syndrome in adults or other renal disease has not been established. The use of cyclophosphamide is contraindicated in patients with urinary outflow obstruction. Cyclophosphamide was approved by the FDA in 1959.[47270][70002][70001][72651]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Emetic Risk
Pediatrics:
Adults:
Administer routine antiemetic prophylaxis prior to treatment.[67392][67389]
Extravasation Risk
Extemporaneous compounding instructions for cyclophosphamide oral suspension (10 mg/mL)
Extemporaneous compounding instructions for cyclophosphamide oral liquid solution
Visually inspect parenteral products for particulate matter and discoloration prior to administration whenever solution and container permit.
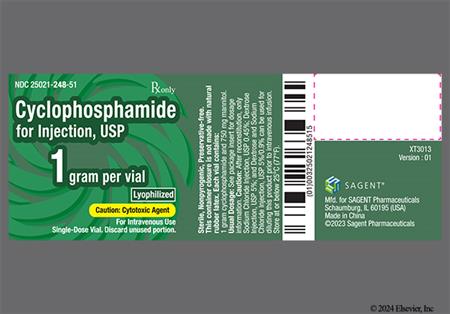
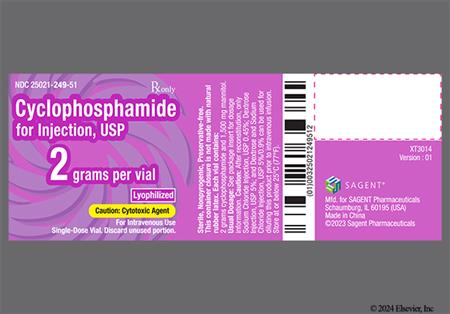
Cyclophosphamide Lyophilized Powder for Injection
NOTE: Do not use cyclophosphamide powder for injection vials if there are signs of melting. Melted cyclophosphamide powder is a clear or yellowish viscous liquid usually found as a connected phase or in droplets in the affected vials.[47270][65782]
Reconstitution
NOTE: Do not reconstitute with Sterile Water for Injection if cyclophosphamide will be administered via direct IV injection due to a resultant hypotonic solution. All reconstituted solutions will have a final concentration of 20 mg/mL.
Dilution
Direct IV Injection or Intravenous Infusion
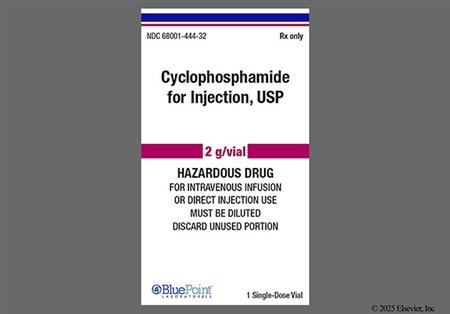
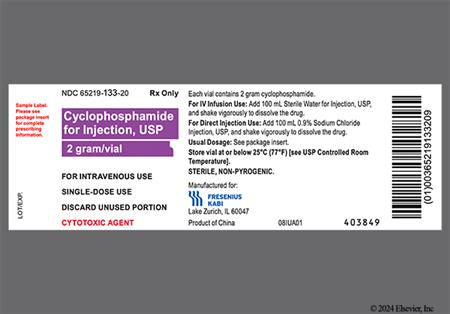
Cyclophosphamide Solution for Injection
Dilution
Direct IV Injection or Intravenous Infusion
Dose-dependent bone marrow suppression (e.g., anemia, leukopenia, neutropenia, thrombocytopenia) is one of the most commonly reported adverse reactions with cyclophosphamide therapy; neutropenic fever and bone marrow failure have also been reported. Leukocyte and platelet nadirs typically occur in weeks 1 and 2 of therapy; blood counts usually normalize after approximately 20 days. Granulocyte colony-stimulating factors may be considered as primary and secondary prophylaxis of neutropenic complications in high-risk patients. Do not administer cyclophosphamide if the neutrophil count is 1,500 cells/mm3 or less or the platelet count is less than 50,000 cells/mm3. An interruption of therapy, dose reduction, or discontinuation of therapy may be necessary.[47270] [70001] [70002] [72651]
Serious and life-threatening infection resulting from severe immunosuppression has been reported in patients receiving cyclophosphamide, including an increase in the risk for and severity of pneumonia or other bacterial (e.g., Pneumocystis jirovecii), fungal, viral, protozoal, or parasitic infections (e.g., Strongyloides), reactivation of latent infections (e.g., viral hepatitis, tuberculosis, herpes zoster), sepsis, and septic shock; an influenza-like illness has also been reported in patients treated with cyclophosphamide in postmarketing experience. Increases in acute-phase reactants such as lactate dehydrogenase and C-reactive protein and multiorgan failure have also been reported. Cyclophosphamide therapy may not be indicated in patients who have an active infection; treatment may need to be interrupted in patients who develop infection.[47270] [70001] [70002] [72651]
Dose-dependent urotoxicity (e.g., bladder ulceration, necrosis, fibrosis, contracture, and secondary cancer) can occur with short-term or long-term use of cyclophosphamide, and may require an interruption of therapy or cystectomy; urotoxicity may be fatal.[47270] [70001] [70002] Early-onset hemorrhagic cystitis occurs within days of cyclophosphamide administration and is usually caused by the toxic metabolite, acrolein. In 20% to 25% of patients who receive high-dose cyclophosphamide, hemorrhagic cystitis can develop weeks to months after treatment; most of these cases are related to reactivation of BK virus. Chronic low-dose cyclophosphamide has also been associated with late-onset hemorrhagic cystitis attributed to BK virus.[65804] Pyelitis, ureteritis, and hematuria have also been reported in patients treated with cyclophosphamide. Aggressive hydration and frequent bladder emptying may reduce the frequency and severity of acute bladder toxicity; administration of mesna has also been used. Discontinue cyclophosphamide therapy in patients who develop severe hemorrhagic cystitis; medical and/or surgical supportive treatment may be required.[47270] [70001] [70002] [72651]
Renal failure, renal tubular necrosis/disorder, renal impairment, toxic nephropathy, ulcerative cystitis, bladder spasm/contracture, nephrogenic diabetes insipidus, and atypical urinary bladder epithelial cells have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Cardiotoxicity, which is dose-dependent, is the dose-limiting toxicity of cyclophosphamide. Transient cardiotoxicity has been reported in up to 45% of patients receiving bone marrow transplantation, typically manifesting as subclinical left ventricular dysfunction; mild arrhythmias and small pleural and pericardial effusions can also occur.[65804] Left ventricular dysfunction has been reported in 7% to 28% of patients treated with cyclophosphamide and appears to be related to a single dose rather than cumulative dosing. High-dose rapid administration of cyclophosphamide may induce lethal acute pericarditis and hemorrhagic myocarditis.[65787] Cardiomyopathy, myocarditis, myopericarditis, pericardial effusion, cardiac tamponade, and congestive heart failure have been reported in postmarketing experience with cyclophosphamide; some cases have been fatal.[47270] [70001] [70002] [72651] Hemorrhagic myocarditis, which is fatal and occurs abruptly within days of cyclophosphamide administration, has been reported in less than 0.1% of patients in transplant centers.[65804]
Cardiac arrest, cardiogenic shock, myocardial hemorrhage, myocardial infarction, bradycardia, palpitations, supraventricular tachycardia (SVT) (e.g., atrial fibrillation and atrial flutter), and ventricular arrhythmia (e.g., severe QT prolongation associated with ventricular tachycardia or ventricular fibrillation) have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651] Arrhythmias may occur in the context of perimyocarditis and congestive heart failure.[65788]
Chest pain (unspecified) has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Pulmonary toxicity including pneumonitis, pulmonary fibrosis, pulmonary veno-occlusive disease and other forms of pulmonary toxicity leading to respiratory failure have been reported during and following treatment with cyclophosphamide. Pneumonitis may develop years after treatment with cyclophosphamide; late onset pneumonitis (greater than 6 months after start of therapy) appears to be associated with increased mortality. Acute respiratory distress syndrome (ARDS), interstitial lung disease as manifested by respiratory failure, bronchiolitis obliterans, organizing pneumonia, allergic alveolitis, pulmonary hemorrhage, bronchospasm, dyspnea, hypoxia, cough, nasal congestion and discomfort, and rhinorrhea have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
New primary malignancy has occurred in patients treated with cyclophosphamide including acute leukemias, lymphomas, myelodysplastic syndrome, sarcomas, thyroid cancer, and urinary tract cancer. Routinely monitor urinalyses for the presence of erythrocytes and other signs of urotoxicity and/or nephrotoxicity; taking measures to prevent hemorrhagic cystitis may reduce the risk of bladder cancer. Renal cell cancer, renal pelvis cancer, sarcoma, thyroid cancer, and ureteric cancer have also been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651] Therapy-related leukemia occurs in approximately 2% of patients treated with chronic cyclophosphamide, usually in patients who received treatment for more than 1 year; the time frame is usually between 3 and 10 years after treatment. Most cases of cyclophosphamide-induced bladder cancer have also been reported in patients who received the drug orally for more than 1 year, with a cumulative dose of more than 20 g as the primary risk factor.[65804]
Sinusoidal obstruction syndrome (SOS), previously termed veno-occlusive disease (VOD), has been reported in patients treated with cyclophosphamide, including some cases with fatal outcome. Risk factors include baseline hepatic disease, abdominal radiation, low performance status, and cytoreductive stem cell transplant conditioning regimens inclusive of cyclophosphamide plus whole-body irradiation, busulfan, or other agents; it has also developed gradually in patients receiving long-term, low-dose cyclophosphamide for immunosuppression. Additional adverse hepatic reactions reported in postmarketing experience with cyclophosphamide include cholestasis, hepatitis (e.g., cholestatic hepatitis and cytolytic hepatitis), and hepatotoxicity with hepatic failure, hepatic encephalopathy, ascites, hepatomegaly, hyperbilirubinemia, and elevated hepatic enzymes. There are also isolated reports of jaundice occurring during therapy.[47270] [70001] [70002] [72651]
Cyclophosphamide may cause impaired wound healing by reducing initial vasodilation and subsequent neovascularization during the proliferative phase of healing. However, although high doses of cyclophosphamide adversely affect wound healing in several animal studies, studies in humans at therapeutic doses did not demonstrate these effects.[47270] [65794] [70001] [70002] [72651]
Hyponatremia associated with increased total body water, acute water intoxication, and syndrome of inappropriate secretion of antidiuretic hormone (SIADH) has been reported in patients receiving cyclophosphamide; some cases were fatal.[47270] [70001] [70002] [72651]
Cyclophosphamide interferes with oogenesis and spermatogenesis and may cause infertility due to gonadal suppression in both sexes. Prepubescent children treated with cyclophosphamide typically develop secondary sexual characteristics normally. Prepubescent girls may have regular menses; however, ovarian fibrosis with complete loss of germ cells has been reported in those who received prolonged cyclophosphamide therapy in late prepubescence. Amenorrhea (transient or permanent), associated with decreased estrogen and increased gonadotropin secretion, develops in some people treated with cyclophosphamide; oligomenorrhea has also been reported. Individuals generally resume regular menses within a few months after cessation of therapy, although ovarian failure and ovarian disorder have also been reported in postmarketing experience with cyclophosphamide. Individuals treated with cyclophosphamide who retain ovarian function are at an increased risk of premature menopause. Oligospermia or azoospermia, increased gonadotropin secretion, and testicular atrophy have occurred in prepubescent and adult individuals who received cyclophosphamide therapy; azoospermia may be reversible in some cases but may be delayed by several years after cessation of therapy. The development of sterility appears to depend on the dose of cyclophosphamide, duration of therapy (greater than 90 days in males), and the state of gonadal function at the time of treatment; it may be irreversible in some patients. The risk of premature menopause with cyclophosphamide increases with age.[47270] [70001] [70002] [72651] The risk for sustained amenorrhea in patients with lupus receiving monthly intermediate-dose cyclophosphamide is 12% for women younger than 25 years old and is greater than 50% for women over 30 years old. However, no ovarian failure was observed in women younger than 26 years old with aplastic anemia after receiving high-dose cyclophosphamide as part of a conditioning regimen for allogeneic bone marrow transplant.[65804]
Teratogenesis including malformations of the skeleton, palate, limbs and eyes as well as miscarriage have been reported after exposure to cyclophosphamide in the first trimester. Fetal growth retardation and additional toxic effects in the newborn include leukopenia, anemia, pancytopenia, severe bone marrow hypoplasia, and gastroenteritis. Fetal death has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Premature labor has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Abdominal pain and diarrhea have commonly been reported in patients treated with cyclophosphamide; there have also been isolated reports of hemorrhagic colitis. Cecitis (typhlitis), constipation, enteritis, and GI bleeding have been reported in postmarketing surveillance of cyclophosphamide.[47270] [65804] [70001] [70002] [72651]
Nausea and vomiting commonly occur with cyclophosphamide treatment if antiemetic prophylaxis is not employed. After a single dose of cyclophosphamide 1,500 mg/m2 or more, greater than 90% of patients will experience emesis. At doses of less than 1,500 mg/m2, the incidence of vomiting is 30% to 90%. In pediatric patients receiving combination chemotherapy that includes cyclophosphamide doses greater than 400 mg/m2 along with other specific chemotherapy agents, the incidence of nausea and vomiting is greater than 90%.[47270] [63197] [67392] [70001] [70002] [72651]
Anorexia has commonly been reported with cyclophosphamide treatment. Dysgeusia, hypogeusia, and parosmia have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
There have been isolated reports of oral ulceration in patients treated with cyclophosphamide. Mucosal inflammation, oropharyngeal pain, parotid gland inflammation (parotitis), and stomatitis have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Acute pancreatitis has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Hearing loss (deafness), impaired hearing, and tinnitus have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Visual impairment, conjunctivitis, and increased lacrimation have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Anaphylactic shock and hypersensitivity reactions have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Arthralgia, muscle cramps/spasms, myalgia, myelopathy, and rhabdomyolysis have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Hyperglycemia and hypoglycemia have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Alopecia is common in patients treated with cyclophosphamide. A skin rash occasionally occurs during treatment, while skin hyperpigmentation and nail changes can also occur. Toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema, erythema multiforme, palmar-plantar erythrodysesthesia (hand and foot syndrome), radiation recall reaction, toxic skin eruption, scleroderma, urticaria, dermatitis, blisters, pruritus, and hyperhidrosis have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Tremor, encephalopathy, seizures/convulsions, dizziness, and neurotoxicity (manifested as reversible posterior leukoencephalopathy syndrome) have all been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Peripheral neuropathy, polyneuropathy, neuralgia, dysesthesia, hypoesthesia, and paresthesias have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Confusion has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Tumor lysis syndrome (TLS) and hyperuricemia have been reported in patients with rapidly growing tumors in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Pulmonary embolism, venous thrombosis, and peripheral ischemia have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Asthenia, malaise, and fatigue have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Fever and chills have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Disseminated intravascular coagulation (DIC) has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Hemolytic uremic syndrome with thrombotic microangiopathy has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Pleural effusion has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Fluid retention, edema, and facial swelling have been reported in postmarketing surveillance of cyclophosphamide. Facial swelling may be dependent on the rate of infusion.[47270] [70001] [70002] [72651]
Pulmonary edema has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Hypertension and hypotension have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Pulmonary hypertension has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Headache has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Both flushing and hot flashes have been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Vasculitis has been reported in postmarketing surveillance of cyclophosphamide.[47270] [70001] [70002] [72651]
Infusion/injection site reactions including thrombosis, necrosis, phlebitis, inflammation, pain, swelling, and erythema have been reported in postmarketing experience with cyclophosphamide.[47270] [70001] [70002] [72651]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Cross-sensitivity with other alkylating agents is possible with cyclophosphamide.[47270][70001][70002]
Cyclophosphamide is contraindicated in individuals with urinary tract obstruction; use cyclophosphamide with caution, if at all, in individuals with an active urinary tract infection (UTI). Urotoxicity (e.g., bladder ulceration, necrosis, fibrosis, contracture, and secondary cancer) which may be fatal can occur with short-term or long-term use of cyclophosphamide and may require an interruption of therapy or cystectomy. Regularly monitor urinary sediment for the presence of erythrocytes and other signs of urotoxicity and/or nephrotoxicity. Aggressive hydration with forced diuresis and frequent bladder emptying can reduce the frequency and severity of bladder toxicity; mesna has been used to prevent severe bladder toxicity. Discontinue cyclophosphamide if severe hemorrhagic cystitis occurs.[47270] [70001] [70002] [72651]
Do not start therapy with cyclophosphamide until patients have recovered from drug-induced bone marrow suppression including neutropenia (ANC 1,500 cells/mm3 or less) and thrombocytopenia (platelets less than 50,000 cells/mm3). Cyclophosphamide can cause severe myelosuppression and bone marrow failure, which may be worse in patients receiving concomitant chemotherapy and/or radiation therapy. Monitor complete blood counts at baseline and during treatment. An interruption of therapy and/or dose reduction or discontinuation of therapy may be necessary if hematologic toxicity occurs. Consider primary and secondary prophylaxis with a granulocyte colony-stimulating factor in patients who have an increased risk of neutropenic complications; antimicrobial prophylaxis may also be indicated.[47270] [70001] [70002] [72651]
Use cyclophosphamide with caution in patients with an active infection; treatment can result in myelosuppression which may increase the severity of an infection and impede recovery.[47270] [70001] [70002] [72651]
Use cyclophosphamide with caution in patients with a history of cardiac disease and other risk factors for cardiotoxicity including heart failure, coronary artery disease, uncontrolled hypertension, thoracic radiation therapy, and previous treatment with other cardiotoxic agents.[72136] Geriatric patients (patients 65 years or older) and patients receiving high doses of cyclophosphamide are also at increased risk for cardiotoxicity. Cardiotoxicity including myocarditis, myopericarditis, pericardial effusion, cardiac tamponade, and congestive heart failure have been reported with cyclophosphamide use. Cardiac arrhythmias including supraventricular arrhythmias (e.g., atrial fibrillation, atrial flutter) and ventricular arrhythmias (e.g., QT prolongation associated with ventricular tachyarrhythmia) have also occurred following cyclophosphamide-containing therapy. Monitor patients with risk factors for cardiotoxicity and with pre-existing cardiac disease.[47270] [70001] [70002] [72651]
Use cyclophosphamide with caution in patients who have a history of pre-existing pulmonary disease; pneumonitis/interstitial lung disease, pulmonary fibrosis, pulmonary veno-occlusive disease, and other forms of pulmonary toxicity have been reported in patients treated with cyclophosphamide. Monitor patients for new or worsening respiratory symptoms including fever, cough, or dyspnea.[47270] [70001] [70002] [72140] [72651]
Patients with severe hepatic impairment (Child-Pugh class C; total bilirubin greater than 3 times the upper limit of normal (ULN) and any AST) or hepatic failure may have decreased efficacy of cyclophosphamide due to reduced conversion to its active 4-hyroxyl metabolite; monitor these patients for treatment efficacy. When administering IV cyclophosphamide, consider the alcohol content of the specific product in patients with hepatic impairment. Additionally, patients with hepatic impairment including hepatic failure (as well as those who have received prior abdominal radiation therapy and those with a low performance status) may be at increased risk for veno-occlusive disease in patients receiving cyclophosphamide.[47270] [70001] [70002] [72651]
Notify the anesthesiologist if a patient has been treated with cyclophosphamide within 10 days of a planned procedure or major surgery requiring general anesthesia. Cyclophosphamide causes a marked and persistent inhibition of cholinesterase activity; prolonged apnea may occur with concurrent depolarizing muscle relaxants (e.g., succinylcholine). Cyclophosphamide may also cause impaired wound healing.[65782] [69997] [70001] [70002] [72651]
Advise individuals of reproductive potential to avoid pregnancy during cyclophosphamide treatment and for up to 1 year after the last dose. Although there are no adequately controlled studies in pregnant people, cyclophosphamide can cause fetal harm or death when administered during pregnancy based on human case reports, its mechanism of action, and animal studies. Individuals who are pregnant or who become pregnant while receiving cyclophosphamide should be apprised of the potential hazard to the fetus. Malformations of the skeleton, palate, limbs, and eyes as well as miscarriage have been reported after human fetal exposure to cyclophosphamide in the first trimester. Fetal growth retardation and toxic effects in the newborn (e.g., leukopenia, anemia, pancytopenia, severe bone marrow hypoplasia, and gastroenteritis) have also been reported after exposure to cyclophosphamide during pregnancy. When administered to pregnant animals (mice, rats, rabbits, and monkeys) during organogenesis at doses at or below the dose used in humans based on body surface area, multiple malformations occurred including neural tube defects, limb and digit defects and other skeletal anomalies, cleft lip and palate, and reduced skeletal ossification. Animal data suggest the risk of failed pregnancy and malformations may persist as long as oocytes and follicles that were exposed to cyclophosphamide during any of their maturation phases exist; the exact duration in humans is not known, but may be longer than 12 months.[47270] [70001] [70002]
Advise patients to use caution when driving or operating machinery or performing other dangerous duties or activities requiring coordination and concentration immediately after a cyclophosphamide infusion. Cyclophosphamide solution for injection contains ethanol to dissolve the active ingredients; take this into account for patients in whom ethanol ingestion should be avoided or minimized, including pediatric patients. The amount of alcohol varies between products; consult individual product labeling for alcohol content. Monitor patients for signs of alcohol intoxication during and after treatment.[61451] [65780] [69997] [71492] [71513] [71514] [72651]
Counsel people about the reproductive risk and contraception requirements during cyclophosphamide treatment. Cyclophosphamide can be teratogenic if taken during pregnancy. Individuals of reproductive potential should avoid pregnancy and use effective contraception during and for at least 1 year after treatment with cyclophosphamide; these individuals should undergo pregnancy testing prior to initiation of cyclophosphamide. Due to the risk of male-mediated teratogenicity, individuals with partners of reproductive potential should use effective contraception during and for 4 months after treatment with cyclophosphamide. People who become pregnant while receiving cyclophosphamide should be apprised of the potential hazard to the fetus. Cyclophosphamide interferes with oogenesis and spermatogenesis and may cause infertility in both sexes. Prepubescent children treated with cyclophosphamide typically develop secondary sexual characteristics normally. Prepubescent girls may have regular menses; however, ovarian fibrosis with complete loss of germ cells has been reported in those who received prolonged cyclophosphamide therapy in late prepubescence. Amenorrhea (transient or permanent), associated with decreased estrogen and increased gonadotropin secretion, develops in some people treated with cyclophosphamide; oligomenorrhea has also been reported. Individuals generally resume regular menses within a few months after cessation of therapy. Individuals treated with cyclophosphamide who retain ovarian function are at an increased risk of premature menopause. Oligospermia or azoospermia, increased gonadotropin secretion, and testicular atrophy have occurred in prepubescent and adult individuals who received cyclophosphamide therapy; azoospermia may be reversible in some cases but may be delayed by several years after cessation of therapy. The development of sterility appears to depend on the dose of cyclophosphamide, duration of therapy (greater than 90 days in males), and the state of gonadal function at the time of treatment; it may be irreversible in some patients. The risk of premature menopause with cyclophosphamide increases with age.[47270] [70001] [70002]
Due to the potential for serious adverse reactions in nursing infants from cyclophosphamide, advise individuals to discontinue breast-feeding during treatment and for 1 week after the final dose. Cyclophosphamide is present in human milk. Neutropenia, thrombocytopenia, low hemoglobin, and diarrhea have been reported in infants breast-fed by people receiving treatment with cyclophosphamide.[47270] [70001] [70002]
Some formulations of cyclophosphamide solution for injection are not indicated for use in neonates, infants, or children due to the alcohol and propylene glycol content; other cyclophosphamide products may have a different amount of alcohol or no alcohol. Check the specific product labeling to verify the appropriateness of use in pediatric patients. The systemic exposure to alcohol may be increased due to alcohol and propylene glycol being metabolized by the same enzymes, which may be particularly significant in pediatric patients.[47270] [70001] [70002]
Cyclophosphamide is a synthetic alkylating agent that is chemically related to the nitrogen mustards.[47270][70001][70002][72651] It is an inactive prodrug that requires activation to release the active metabolite, phosphoramide mustard. Hydroxylation of cyclophosphamide by the cytochrome P450 system generates 4-hydroxycyclophosphamide, which coexists in equilibrium with its tautomer, aldophosphamide. These metabolites are able to freely diffuse into cells, where aldophosphamide is decomposed into 2 compounds, phosphoramide mustard and acrolein. Phosphoramide mustard produces interstrand and intrastand DNA crosslinks, responsible for the cytotoxic properties of cyclophosphamide. Acrolein is the cause of hemorrhagic cystitis.[65804] Cyclophosphamide causes immunosuppression via lymphopenia (both B-cells and T-cells) and selective suppression of B-lymphocyte activity. Decreased immunoglobulin secretion has been described in patients treated with low-dose cyclophosphamide for autoimmune diseases.[25001] Cyclophosphamide also influences T-lymphocyte activity, although the exact mechanism has not been established. Cyclophosphamide can suppress some T-cell function (e.g., graft-versus-host response and delayed hypersensitivity). In addition, cyclophosphamide (or an activated analog, 4-hydroperoxycyclophosphamide) can enhance the immune response by inhibiting suppressor T-cells. Some studies have shown that cyclophosphamide can increase the efficacy of certain immunotherapy regimens by decreasing tumor-induced suppressor T-cells. Other data suggest that cyclophosphamide induces release of factors that enhance tumor-specific T-cells, specifically type I interferons.[25331]
Revision Date: 10/03/2025, 02:01:25 PMCyclophosphamide is administered orally and intravenously. It is approximately 20% protein-bound, with no dose-dependent changes in protein binding; some metabolites are protein-bound to an extent greater than 60%. The cyclophosphamide volume of distribution approximates total body water and is approximately 30 to 50 liters; it has an elimination half-life of 3 to 12 hours, with total body clearance ranging from 4 to 5.6 liters/hour. Cyclophosphamide appears to induce its own metabolism, which results in an increase in the total clearance, increased formation of the active 4-hydroxycyclophosphamide metabolite, and shortened half-life values following repeated administration at 12- to 24-hour intervals. Cyclophosphamide is primarily excreted as metabolites, with 10% to 20% excreted as unchanged drug in the urine and 4% in the bile following IV administration.[47270][70001][70002][72651]
Affected cytochrome P450 isoenzymes: CYP2A6, CYP2B6, CYP3A, CYP2C9, CYP2C19
Cyclophosphamide is a prodrug that is primarily (75%) biotransformed in the liver to both therapeutically active (N-hydroxylated) and therapeutically inactive but neurotoxic (N-dechlorethylated) metabolites.[27058][47270] CYP2B6 is primarily responsible for metabolism to the active alkylating metabolites, 4-hydroxycyclophosphamide and aldophosphamide; CYP2A6, CYP3A, CYP2C9, and CYP2C19 also contribute to cyclophosphamide metabolism. Aldophosphamide and 4-hydroxycyclophosphamide undergo oxidation by aldehyde dehydrogenases to form inactive metabolites carboxyphosphamide and 4-ketocyclophosphamide, respectively. Aldophosphamide can also undergo beta-elimination to form active metabolites phosphoramide mustard and acrolein, which is urotoxic. This spontaneous conversion can be catalyzed by albumin and other proteins.[47270][70001][70002][72651] The N-dechloroethylation process for cyclophosphamide appears catalyzed primarily by CYP3A4.[27058] Less than 5% of cyclophosphamide may be directly detoxified by side chain oxidation, leading to the formation of inactive metabolites 2-dechloroethylcyclophosphamide (neurotoxic). At high doses, the fraction of parent compound cleared by 4-hydroxylation is reduced, resulting in non-linear elimination of cyclophosphamide in patients.[47270][70001][70002][72651]
Peak concentrations of cyclophosphamide occurred 1 hour after oral administration (Tmax). The AUC ratio for cyclophosphamide after oral and IV administration (AUCPO to AUCIV) ranged from 0.87 to 0.96.[70001][70002]
Pharmacokinetics are linear over the dose range used clinically. When administered at a dose of 4 g/m2 IV over 90 minutes (approximately 2 times the recommended dose), cyclophosphamide exhibited saturable elimination in parallel with first-order renal elimination.[47270][72651]
The mean total body clearance of cyclophosphamide was 45 liters/kg (+/- 8.6 liters/kg) in patients with severe hepatic impairment (mean bilirubin 3.5 mg/dL and mean AST 90 international units/liter), which is a 40% decrease compared to those with normal hepatic function (mean bilirubin 0.5 mg/dL and mean AST 10 international units/liter). The elimination half-life was 12.5 hours (+/- 1 hour) in patients with severe hepatic impairment, representing a 64% increase from the control group. Patients with severe hepatic impairment have reduced conversion of cyclophosphamide to the active 4-hydroxyl metabolite, potentially reducing efficacy.[47270][70001][70002][72651]
Systemic exposure to cyclophosphamide increases as renal function decreases. Following a 1-hour IV infusion, the mean dose-corrected AUC increased by 38% in patients with moderate renal impairment (CrCl 25 to 50 mL/min) and by 64% to 77% in patients with severe renal impairment (CrCl 10 to 24 mL/min) compared to the control group (CrCl 80 mL/min or higher). Cyclophosphamide is dialyzable. In four patients on long-term hemodialysis, the dialysis clearance of cyclophosphamide averaged 104 mL/min (calculated by arterial venous difference and actual drug recovery in dialysate); this is in the range of the metabolic clearance of 95 mL/min for cyclophosphamide. A mean of 37% of the administered dose was removed during a 4-hour hemodialysis period. The elimination half-life of cyclophosphamide was 3.3 hours during hemodialysis, which is a 49% reduction from that reported for uremic patients (6.5 hours). Cyclophosphamide exposure increased by 23% in patients receiving hemodialysis (CrCl less than 10 mL/min) compared to controls (CrCl 80 mL/min or higher).[47270][65782][70002][70001][72651]
Advise individuals of reproductive potential to avoid pregnancy during cyclophosphamide treatment and for up to 1 year after the last dose. Although there are no adequately controlled studies in pregnant people, cyclophosphamide can cause fetal harm or death when administered during pregnancy based on human case reports, its mechanism of action, and animal studies. Individuals who are pregnant or who become pregnant while receiving cyclophosphamide should be apprised of the potential hazard to the fetus. Malformations of the skeleton, palate, limbs, and eyes as well as miscarriage have been reported after human fetal exposure to cyclophosphamide in the first trimester. Fetal growth retardation and toxic effects in the newborn (e.g., leukopenia, anemia, pancytopenia, severe bone marrow hypoplasia, and gastroenteritis) have also been reported after exposure to cyclophosphamide during pregnancy. When administered to pregnant animals (mice, rats, rabbits, and monkeys) during organogenesis at doses at or below the dose used in humans based on body surface area, multiple malformations occurred including neural tube defects, limb and digit defects and other skeletal anomalies, cleft lip and palate, and reduced skeletal ossification. Animal data suggest the risk of failed pregnancy and malformations may persist as long as oocytes and follicles that were exposed to cyclophosphamide during any of their maturation phases exist; the exact duration in humans is not known, but may be longer than 12 months.[47270] [70001] [70002]
Due to the potential for serious adverse reactions in nursing infants from cyclophosphamide, advise individuals to discontinue breast-feeding during treatment and for 1 week after the final dose. Cyclophosphamide is present in human milk. Neutropenia, thrombocytopenia, low hemoglobin, and diarrhea have been reported in infants breast-fed by people receiving treatment with cyclophosphamide.[47270] [70001] [70002]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.