Blood Clots in a Deep Vein (Deep Vein Thrombosis): What to Know
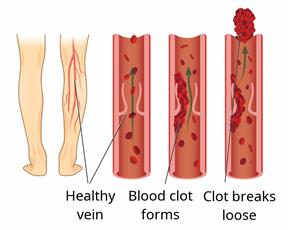
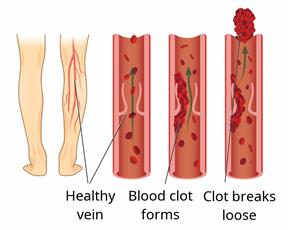
Deep vein thrombosis (DVT) is when a blood clot forms in a deep vein, such as in the arms, lower legs, thighs, or the area between your hip bones (pelvis).
DVT is serious. It can be life-threatening if a blood clot breaks loose and travels to your lungs to cause a blockage (pulmonary embolism). It cause also damage veins in your leg, which can lead to long-term problems, such as:
Pain.
Swelling.
Skin color changes.
Skin ulcers or sores.
What are the causes?
DVT may be caused by:
What increases the risk?
You may be more likely to get a DVT if:
You're older.
You're overweight.
You're pregnant or recently had a baby.
- You take certain medicines, such as:
You smoke or use nicotine or tobacco.
You have or have had a blood vessel disease or heart failure.
You have cancer.
You may also be more at risk if you don't move around enough. This includes if:
You sit or lie down for long periods of time, other than to sleep at night.
You're in the hospital or having major surgery.
You've had a recent bone injury, such as a break.
You've had recent surgery on your legs.
What are the signs or symptoms?
Symptoms may include:
An arm or leg turning warm or red.
Swelling, pain, pressure, or tenderness in an arm or leg.
Pain in your calf or behind your knee.
A leg turning very pale or having other color changes.
If the clot is in your leg, your symptoms may get worse when you stand or walk. In some cases, there are no symptoms.
How is this diagnosed?
You may be diagnosed based on your medical history and an exam. You may also have tests, such as:
Blood tests. These can check how well your blood clots.
Ultrasound. This uses sound waves to make images.
CT venogram. Contrast dye is put into a vein, and X-rays are taken to check for clots. This is helpful for veins in your chest or pelvis.
How is this treated?
Treatment depends on:
The cause of your DVT.
How big the clot is and where it is.
If you have more than one DVT.
Your risk for bleeding or having more clots.
Other health problems you may have.
You may need to:
Take a medicine called a blood thinner to stop more clots from forming or current clots from growing.
Wear compression stockings.
Have medicines put into your vein to break up the clot.
- Have surgery. You may need this if the DVT is very bad or hard to treat. It may be done to:
You may have some treatments for 6 months or longer.
Follow these instructions at home:
If you're taking blood thinners:
- Talk with your health care provider if you have a history of:
Internal bleeding.
Bleeding ulcers.
Strokes.
Cerebral aneurysms.
-
Take your medicines as told. Take them at the same time each day.
-
Talk with your provider before taking any products you can buy at the store.
-
Do not do things that could hurt or bruise you. Be careful to avoid falls.
-
Wear an alert bracelet or carry a card that says you take blood thinners.
-
Be careful when using knives, scissors, or other sharp objects.
-
Use an electric razor instead of a blade.
General instructions
To learn more, go to these websites:
- American Heart Association (AHA) at heart.org. Then:
Click "Search."
Type "venous thromboembolism" in the search field and find the link you need.
- Centers for Disease Control and Prevention (CDC) at cdc.gov. Then:
Click "Search."
Type "venous thromboembolism" in the search field and find the link you need.
Contact a health care provider if:
-
You miss a dose of your blood thinner.
-
You have new bruising.
-
You have new or worse pain, swelling, or redness in an arm or leg.
-
Your arm or leg is numb or tingling and doesn't get better with treatment.
-
Your skin is pale and doesn't get better with treatment.
These symptoms may be an emergency. Call 911 right away.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.