ThisiscontentfromElsevier'sDrugInformation
Deutetrabenazine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
6 mg PO twice daily, initially. TITRATION: Increase at weekly intervals in increments of 6 mg/day based on reduction of chorea and tolerability. Administer total daily dosages of 12 mg or more in 2 divided doses. Max: 48 mg/day. Do not exceed 18 mg/dose or 36 mg/day in patients who are poor CYP2D6 metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume the previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
12 mg PO once daily, initially. TITRATION: Increase at weekly intervals in increments of 6 mg/day based on reduction of chorea and tolerability. Max: 48 mg/day. Do not exceed 36 mg/day in patients who are poor CYP2D6 metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
Discontinue tetrabenazine and start deutetrabenazine the next day. Use 6 mg PO once daily for patients taking tetrabenazine 12.5 mg/day; 6 mg PO twice daily for patients taking tetrabenazine 25 mg/day; 9 mg PO twice daily for patients taking tetrabenazine 37.5 mg/day; 12 mg PO twice daily for patients taking tetrabenazine 50 mg/day; 15 mg PO twice daily for patients taking tetrabenazine 62.5 mg/day; 18 mg PO twice daily for patients taking tetrabenazine 75 mg/day; 21 mg PO twice daily for patients taking tetrabenazine 87.5 mg/day; and 24 mg PO twice daily for patients taking tetrabenazine 100 mg/day. TITRATION: Increase at weekly intervals in increments of 6 mg/day based on reduction of chorea and tolerability. Administer total daily dosages of 12 mg or more in 2 divided doses. Max: 48 mg/day. Do not exceed 18 mg/dose or 36 mg/day in patients who are poor CYP2D6 metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
Discontinue tetrabenazine and start deutetrabenazine the next day. Use 6 mg PO once daily for patients taking tetrabenazine 12.5 mg/day; 12 mg PO once daily for patients taking tetrabenazine 25 mg/day; 18 mg PO once daily for patients taking tetrabenazine 37.5 mg/day; 24 mg PO once daily for patients taking tetrabenazine 50 mg/day; 30 mg PO once daily for patients taking tetrabenazine 62.5 mg/day; 36 mg PO once daily for patients taking tetrabenazine 75 mg/day; 42 mg PO once daily for patients taking tetrabenazine 87.5 mg/day; and 48 mg PO once daily for patients taking tetrabenazine 100 mg/day. TITRATION: Increase at weekly intervals by increments of 6 mg/day based on reduction of chorea and tolerability. Max: 48 mg/day. Do not exceed 36 mg/day in patients who are poor CYP2D6 metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
6 mg PO twice daily, initially. TITRATION: Increase at weekly intervals by 6 mg/day based on reduction of tardive dyskinesia and tolerability. Give total daily dosages of 12 mg or more in 2 divided doses. Max: 48 mg/day. Do not exceed 18 mg/dose or 36 mg/day in CYP2D6 poor metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
12 mg PO once daily, initially. TITRATION: Increase at weekly intervals in increments of 6 mg/day based on reduction of tardive dyskinesia and tolerability. Max: 48 mg/day. Do not exceed 36 mg/day in CYP2D6 poor metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: After an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
Discontinue tetrabenazine and start deutetrabenazine the next day. 6 mg PO once daily for patients taking tetrabenazine 12.5 mg/day; 6 mg PO twice daily for patients taking tetrabenazine 25 mg/day; 9 mg PO twice daily for patients taking tetrabenazine 37.5 mg/day; 12 mg PO twice daily for patients taking tetrabenazine 50 mg/day; 15 mg PO twice daily for patients taking tetrabenazine 62.5 mg/day; 18 mg PO twice daily for patients taking tetrabenazine 75 mg/day; 21 mg PO twice daily for patients taking tetrabenazine 87.5 mg/day; and 24 mg PO twice daily for patients taking tetrabenazine 100 mg/day. TITRATION: Increase at weekly intervals by 6 mg/day based on reduction of tardive dyskinesia and tolerability. Give total daily dosages of 12 mg or more in 2 divided doses. Max: 48 mg/day. Do not exceed 18 mg/dose or 36 mg/day in CYP2D6 poor metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: For an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
Discontinue tetrabenazine and start deutetrabenazine the next day. 6 mg PO once daily for patients taking tetrabenazine 12.5 mg/day; 12 mg PO once daily for patients taking tetrabenazine 25 mg/day; 18 mg PO once daily for patients taking tetrabenazine 37.5 mg/day; 24 mg PO once daily for patients taking tetrabenazine 50 mg/day; 30 mg PO once daily for patients taking tetrabenazine 62.5 mg/day; 36 mg PO once daily for patients taking tetrabenazine 75 mg/day; 42 mg PO once daily for patients taking tetrabenazine 87.5 mg/day; 48 mg PO once daily for patients taking tetrabenazine 100 mg/day. TITRATION: Increase at weekly intervals by 6 mg/day based on reduction of tardive dyskinesia and tolerability. Max: 48 mg/day. Do not exceed 36 mg/day in CYP2D6 poor metabolizers. INTERACTIONS: Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. INTERRUPTION OF TREATMENT: For an interruption of more than 1 week, retitrate. For an interruption of less than 1 week, resume previous maintenance dose. DISCONTINUATION: Discontinue treatment without tapering.[61845]
48 mg/day PO; 36 mg/day PO in CYP2D6 poor metabolizers.
48 mg/day PO; 36 mg/day PO in CYP2D6 poor metabolizers.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Deutetrabenazine is contraindicated in patients with hepatic impairment.[61845]
Specific guidelines for dosage adjustments are not available; the impact of renal impairment on deutetrabenazine has not been studied.[61845]
† Off-label indication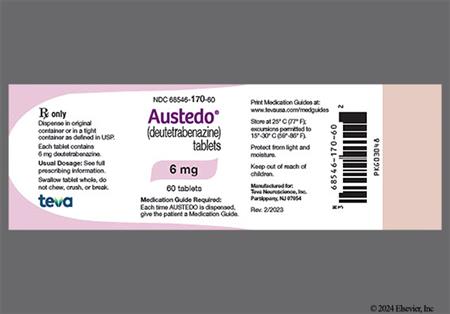







Deutetrabenazine is an oral, vesicular monoamine transporter 2 (VMAT 2) inhibitor indicated for the treatment of tardive dyskinesia and chorea associated with Huntington's disease.[61845] Deutetrabenazine is a deuterated formulation of tetrabenazine. Adverse reactions associated with peak plasma concentrations of tetrabenazine (e.g., somnolence, depression) sometimes limit treatment. The chemical alteration present in deutetrabenazine slows drug metabolism and prolongs therapeutic effect, which decreases dosing requirements and thereby produces lower peak plasma concentrations.[61875] During a placebo-controlled trial of 222 adult patients with tardive dyskinesia, deutetrabenazine dosages of 24 mg/day and 36 mg/day significantly reduced abnormal involuntary movements compared to placebo as measured by the Abnormal Involuntary Movement Scale (AIMS); AIMS total scores improved from baseline to 12 weeks by 1.4, 3.2, and 3.3 units for placebo, deutetrabenazine 24 mg/day, and deutetrabenazine 36 mg/day, respectively. A reduction in abnormal involuntary movements by AIMS was noted as early as 2 weeks into deutetrabenazine therapy. An additional placebo-controlled trial in adults with tardive dyskinesia (n = 113) demonstrated a statistically significant AIMS change with deutetrabenazine compared to placebo (-3 vs. -1.6) from baseline to 12 weeks. The mean deutetrabenazine dosage was 38.3 mg/day. In a 12-week, randomized, double-blind, placebo-controlled trial of 90 patients with chorea associated with Huntington's disease, deutetrabenazine significantly improved motor function as measured by the change from baseline in Total Maximal Chorea Score (-4.4 vs. -1.9; p less than 0.0001). The mean deutetrabenazine dosage after titration was 40 mg/day. Deutetrabenazine use may increase the risk for suicidality in patients with Huntington's disease, and is therefore contraindicated in patients who are suicidal or who have untreated or inadequately treated depression.[61845]
For storage information, see the specific product information within the How Supplied section.
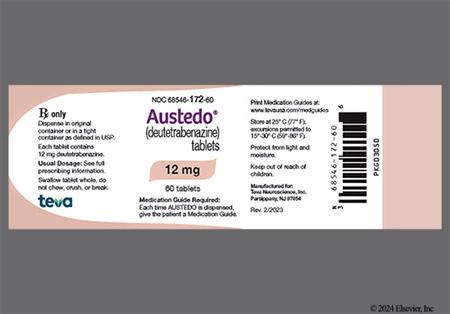
Immediate-release tablets (Austedo):
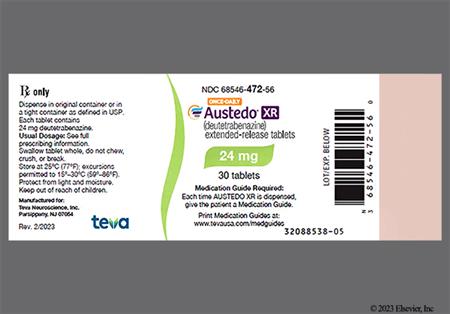
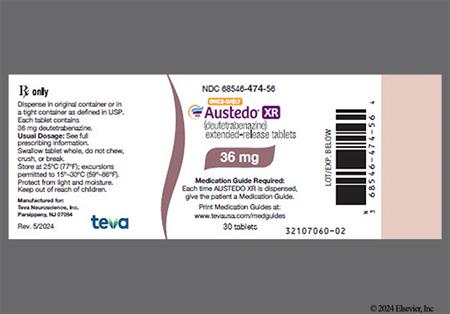
Extended-release tablets (Austedo XR):
Deutetrabenazine use may increase the risk for depression and suicidal ideation; do not use in patients who are suicidal or have untreated or inadequately treated depression. Patients with Huntington's disease are at increased risk for depression and suicidal ideation or behaviors (suicidality). In a placebo-controlled trial of patients with Huntington's disease, suicidal ideation was reported by 2% of deutetrabenazine-treated patients compared to 0% of placebo-treated patients. No suicide attempts or completed suicides were reported. Depression was reported by 4% of patients treated with deutetrabenazine. During placebo-controlled trials of adults with tardive dyskinesia (TD), depression or dysthymic disorder was reported in 2% of deutetrabenazine-treated patients compared to 1% of placebo-treated patients. Use deutetrabenazine with caution in patients with a history of depression or suicidal thoughts or behavior; weigh the risk of suicidality against the need for treatment. Patients or caregivers should report unusual changes in mood, behaviors, or actions promptly to the treating health care professional. If depression or suicidality does not resolve, consider discontinuing treatment with deutetrabenazine. Periodically reevaluate the clinical need for deutetrabenazine.[61845]
Deutetrabenazine may cause pseudoparkinsonism. Reduce the deutetrabenazine dose if a patient develops parkinsonism during treatment; discontinuation may be necessary for some patients. Rigidity may develop as part of the underlying disease process in Huntington's disease; it may be difficult to distinguish between a potential drug-induced adverse reaction and progression of the underlying disease process. Drug-induced parkinsonism may cause more functional disability than untreated chorea in some patients with Huntington's disease. Signs and symptoms of parkinsonism in patients being treated for tardive dyskinesia have included bradykinesia, gait disturbance, and the emergence or worsening of tremor. In most cases, parkinsonism occurred within the first 2 weeks after treatment initiation or dose escalation. In reported cases, parkinsonism resolved after treatment discontinuation.[61845]
Neuroleptic malignant syndrome (NMS) has not been reported with the use of deutetrabenazine; however, NMS has been reported with tetrabenazine (a closely related VMAT2 inhibitor). Be alert for the signs and symptoms of NMS, which include high fever, muscle rigidity, altered mental status, irregular blood pressure, tachycardia, diaphoresis, cardiac dysrhythmia, elevated creatinine phosphokinase, myoglobinuria, rhabdomyolysis, and acute renal failure. If NMS occurs, discontinue deutetrabenazine, and implement intensive symptomatic treatment and medical monitoring. Recurrence of NMS has been reported with reinitiation of drug therapy; if treatment with deutetrabenazine is needed after recovery from NMS, monitor for signs of recurrence.[61845]
Deutetrabenazine may prolong the QT interval, but the degree of QT prolongation is not clinically significant when deutetrabenazine is administered within the recommended dosage range. An exposure-response analysis on QTc prolongation from a study in extensive or intermediate (EM) and poor CYP2D6 metabolizers (PM) showed that a clinically relevant effect can be excluded at exposures after single doses of 24 and 48 mg of deutetrabenazine.[61845]
Deutetrabenazine may increase the risk of akathisia, agitation, and restlessness in patients with Huntington's disease or tardive dyskinesia. In a randomized, placebo-controlled trial in Huntington's disease patients, akathisia, agitation, or restlessness was reported by 4% of patients who received deutetrabenazine compared to 2% of patients who received placebo. Akathisia, agitation, or restlessness was reported by 2% of patients with tardive dyskinesia who received deutetrabenazine compared to 1% of patients who received placebo during randomized, placebo-controlled trials. Agitation led to deutetrabenazine discontinuation in 2% of patients with Huntington's disease. Monitor patients for signs or symptoms of restlessness or agitation, as these symptoms may be indicators of developing akathisia. If akathisia develops, reduce the deutetrabenazine dose; treatment discontinuation may be necessary.[61845]
Drowsiness (somnolence) is a common dose-limiting adverse reaction of deutetrabenazine. Drowsiness was reported in 11% of deutetrabenazine-treated patients compared to 4% of placebo-treated patients in a double-blind, placebo-controlled trial of patients with Huntington's disease. Fatigue occurred in 9% of deutetrabenazine-treated patients compared to 4% of placebo-treated patients. Dizziness (4%) was the most common reaction resulting in dose reduction. Other neurologic adverse reactions observed during the trial include insomnia (7% deutetrabenazine vs. 4% placebo) and anxiety (4% vs. 2%). Contusion occurred in 4% of patients who received deutetrabenazine compared to 2% of patients who received placebo. In tardive dyskinesia studies, insomnia was reported in 4% of deutetrabenazine-treated patients compared to 1% of placebo-treated patients.[61845]
In a 12-week, double-blind, placebo-controlled trial of patients with Huntington's disease, diarrhea occurred in 9% of deutetrabenazine-treated patients compared to 0% of placebo-treated patients. Other gastrointestinal adverse reactions observed during the trial include xerostomia (9% deutetrabenazine vs. 7% placebo) and constipation (4% vs. 2%).[61845]
Urinary tract infection (cystitis) was reported in 7% of deutetrabenazine-treated patients vs. 2% of placebo-treated patients in a double-blind, placebo-controlled study of patients with Huntington's disease. In tardive dyskinesia studies, naso-pharyngitis was reported in 4% of deutetrabenazine-treated patients vs. 2% of placebo-treated patients.[61845]
Serum prolactin concentrations have not been evaluated during deutetrabenazine therapy; however, tetrabenazine, a closely related VMAT2 inhibitor, elevates serum prolactin concentrations in humans. In healthy volunteers, administration of tetrabenazine 25 mg increased peak plasma prolactin concentrations 4- to 5-fold. It is unknown if chronic elevations of prolactin occur with treatment. Patient conditions that may be prolactin-dependent (e.g., breast cancer, amenorrhea, galactorrhea, gynecomastia, and impotence) may develop or worsen. If hyperprolactinemia is suspected, obtain appropriate laboratory testing; consider deutetrabenazine discontinuation.[61845]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Deutetrabenazine is contraindicated in patients with Huntington's disease with active suicidal ideation or who have untreated or inadequately treated depression. Use deutetrabenazine with caution in patients with a history of depression or suicidal thoughts or behavior; weigh the risk of suicidality against the need for chorea treatment. Patients with Huntington's disease are at increased risk for depression and suicidal ideation or behaviors. Deutetrabenazine use may increase the risk for suicidality in patients with Huntington's disease. Report unusual changes in mood, behaviors, or actions promptly to the treating health care professional. If depression or suicidality does not resolve, consider discontinuing treatment with deutetrabenazine. Periodically reevaluate the clinical need for deutetrabenazine.[61845]
Deutetrabenazine may prolong the QT interval, but the degree of QT prolongation is not clinically significant when deutetrabenazine is administered within the recommended dosage range. Avoid using deutetrabenazine in patients with congenital long QT syndrome or a history of cardiac arrhythmias. Certain circumstances may also increase the risk of QT prolongation with deutetrabenazine, including bradycardia, hypokalemia, hypomagnesemia, or concomitant use of other drugs that prolong the QTc interval.[28432] [28457] [56592] [65180] [61845]
Deutetrabenazine is contraindicated for use in patients with hepatic failure or impairment because of the possibility for increased drug exposure and a greater risk of serious adverse reactions. The effect of hepatic impairment on the pharmacokinetics of deutetrabenazine and its primary metabolites has not been studied. In a clinical study of tetrabenazine, a closely related VMAT2 inhibitor, there was a large increase in exposure to tetrabenazine and its active metabolites in patients with hepatic impairment.[61845]
There are no adequate data on the developmental risk associated with deutetrabenazine use during pregnancy. Deutetrabenazine (5, 10, or 30 mg/kg/day) produced no clear adverse effects on embryofetal development when given to rats during the period of organogenesis. However, administration of tetrabenazine, a closely related VMAT2 inhibitor, to rats from organogenesis through lactation resulted in an increase in stillbirths and postnatal mortality.[61845]
Deutetrabenazine has the potential to impair cognitive and motor skills. Sedation is a common dose-limiting side effect of deutetrabenazine. Advise patients to use caution when driving or operating machinery or performing other activities requiring coordination and concentration until they know how deutetrabenazine affects them. The coadministration of alcohol or other CNS depressants may further exacerbate drowsiness associated with the medication.[61845]
Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for deutetrabenazine and any potential adverse effects on the breast-feeding infant from the drug or the mother's underlying condition. There are no data on the presence of deutetrabenazine or its metabolites in human breast milk, the effects on the breast-fed infant, or the effects of the drug on milk production.[61845]
The effect of deutetrabenazine on serum prolactin concentrations has not been evaluated, but it is possible the drug may induce hyperprolactinemia. Tetrabenazine, a closely related VMAT2 inhibitor, can cause hyperprolactinemia. Some human breast cancers may be prolactin-dependent. Therefore, use deutetrabenazine with caution in people who have a history of breast cancer.[61845]
The exact mechanism by which deutetrabenazine exerts its anti-chorea effects is unknown. Deutetrabenazine is a reversible depletor of monoamines (e.g., dopamine, serotonin, norepinephrine, and histamine) from nerve terminals. The major metabolites of deutetrabenazine (alpha-dihydrotetrabenazine [HTBZ] and beta-HTBZ) are reversible inhibitors of vesicular monoamine transporter 2 (VMAT2). Inhibition of VMAT2 results in decreased uptake of monoamines into synaptic vesicles and depletion of monoamine stores.[61845]
Revision Date: 08/26/2025, 07:06:30 PMDeutetrabenazine is administered orally. Protein binding of the major metabolites, alpha-dihydrotetrabenazine (alpha-HTBZ) and beta-dihydrotetrabenazine (beta-HTBZ), ranges from 60% to 68% and 59% to 63%, respectively. Deutetrabenazine is extensively metabolized to alpha-HTBZ and beta-HTBZ, primarily by carbonyl reductase. Alpha-HTBZ and beta-HTBZ are subsequently metabolized by CYP2D6 to form several minor metabolites, with minor contributions from CYP1A2 and CYP3A4/5. The metabolites are primarily renally eliminated. Approximately 75% to 86% and 8% to 11% of a dose is eliminated in the urine and feces, respectively. The half-life of active deuterated alpha-HTBZ, beta-HTBZ, and total alpha-HTBZ metabolites from deutetrabenazine is approximately 12 hours, 7.5 hours, and 9 to 11 hours respectively.[61845]
Affected cytochrome P450 isoenzymes and drug transporters: CYP2D6
In vitro studies indicate that alpha-HTBZ and beta-HTBZ metabolites of deutetrabenazine are substrates for CYP2D6.[61845]
After oral administration of deutetrabenazine, the extent of absorption is at least 80%. Plasma concentrations of deutetrabenazine are generally below detectable limits due to extensive and rapid hepatic metabolism. Peak plasma concentrations of the active metabolites, alpha-HTBZ and beta-HTBZ, are reached within 3 to 4 hours after a dose of the immediate-release formulation. Peak plasma concentrations of active metabolites are reached within approximately 3 hours of administration of the extended-release (ER) formulation, followed by sustained plateaus for several hours. Food has no effect on the AUC of alpha-HTBZ and beta-HTBZ; however, Cmax for the immediate-release formulation is increased by approximately 50% in the presence of food; th eimmediate-release tablets should be given with food. No effect on Cmax was noted with the ER tablet formulation, and the ER tablets may be given with or without food.[61845]
The effect of hepatic impairment on the pharmacokinetics of deutetrabenazine has not been studied. In a clinical study of tetrabenazine, a closely related VMAT2 inhibitor, the exposure to alpha-HTBZ and beta-HTBZ was up to 40% greater in patients with hepatic impairment. The mean tetrabenazine Cmax was up to 190-fold higher in patients with hepatic impairment compared to healthy subjects.[61845]
The effect of renal impairment on the pharmacokinetics of deutetrabenazine has not been studied.[61845]
There is no apparent effect of gender on the pharmacokinetics of alpha-HTBZ and beta-HTBZ of deutetrabenazine.[61845]
CYP2D6 Poor Metabolizers
The pharmacokinetics of deutetrabenazine, alpha-HTBZ, and beta-HTBZ have not been evaluated in patients who do not express CYP2D6. However, it is likely that exposure to alpha-HTBZ and beta-HTBZ would be increased similarly to taking strong CYP2D6 inhibitors, approximately 3-fold.[61845]
There are no adequate data on the developmental risk associated with deutetrabenazine use during pregnancy. Deutetrabenazine (5, 10, or 30 mg/kg/day) produced no clear adverse effects on embryofetal development when given to rats during the period of organogenesis. However, administration of tetrabenazine, a closely related VMAT2 inhibitor, to rats from organogenesis through lactation resulted in an increase in stillbirths and postnatal mortality.[61845]
Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for deutetrabenazine and any potential adverse effects on the breast-feeding infant from the drug or the mother's underlying condition. There are no data on the presence of deutetrabenazine or its metabolites in human breast milk, the effects on the breast-fed infant, or the effects of the drug on milk production.[61845]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.