ThisiscontentfromElsevier'sDrugInformation
Doxorubicin
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628] Doxorubicin 30 mg/m2 slow IV push on day 2 in combination with vinblastine (3 mg/m2 IV on days 2, 15, and 22), methotrexate (30 mg/m2 slow IV push on days 1, 15, and 22), and cisplatin (70 mg/m2 IV on day 2) repeated every 28 days for up to a maximum of 6 cycles (MVAC regimen) has been evaluated in clinical trials.[18793] [36131]
30 mg/m2 IV on day 2 in combination with methotrexate (30 mg/m2 IV on days 1, 15, and 22), cisplatin 70 mg/m2 IV on day 2, and vinblastine (3 mg/m2 IV on days 2, 15, and 22) repeated every 28 days (MVAC regimen) for up to 6 cycles has been evaluated in patients with advanced or metastatic transitional cell carcinoma of the bladder in a long-term analysis of a multicenter, randomized, phase III trial.[44748] Doxorubicin 30 mg/m2 IV on day 1 plus methotrexate (30 mg/m2 IV on days 1, 15, and 22), cisplatin (70 mg/m2 IV on day 1), and vinblastine (3 mg/m2 IV on days 1, 15, and 22) repeated every 4 weeks was studied in another randomized, phase III trial. All patients in this study received granulocyte colony-stimulating factor (G-CSF) following chemotherapy.[44750] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 to 150 mg in 150 mL of normal saline instilled into the bladder. The solution is then retained for at least 30 minutes. Responses of up to 90% have been seen with doses of 50 to 150 mg; however, the duration of response is short. In a comparison trial of intravesical doxorubicin and BCG, the disease-free survival of BCG was significantly longer at 5 years than that of doxorubicin.[25969] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
30 mg/m2 slow IV push on day 2 in combination with vinblastine (3 mg/m2 IV on days 2, 15, and 22), methotrexate (30 mg/m2 slow IV push on days 1, 15, and 22), and cisplatin (70 mg/m2 IV on day 2); give every 28 days for 3 cycles (MVAC regimen).[18788] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
60 mg/m2 as an IV bolus on day 1 repeated every 21 days for 4 cycles of therapy, in combination with cyclophosphamide. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Disease-free survival and overall survival were not significantly different in women with axillary lymph node-positive early breast cancer who received adjuvant doxorubicin hydrochloride-containing regimens (n = 2,157) compared with cyclophosphamide, methotrexate, and fluorouracil (CMF) (n = 1,353) in a meta-analysis of 6 trials conducted by the Early Breast Cancer Trialists Collaborative Group (EBCTCG).[61628] Additionally, a dose-dense regimen of doxorubicin 60 mg/m2 IV plus cyclophosphamide 600 mg/m2 IV on day 1 repeated every 14 days with growth-factor support has been studied.[33122]
60 mg/m2 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 mg/m2 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
25 mg/m2 IV on days 1 and 15 repeated every 28 days in combination with vinblastine, bleomycin, and dacarbazine (ABVD regimen).[40473] A variation of this regimen includes doxorubicin 35 mg/m2 IV on day 8 in combination with mechlorethamine, vincristine, procarbazine, prednisone, bleomycin, and vinblastine (MOPP/ABV hybrid regimen).[40471] [40472] [40473] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Interruption of therapy and/or a dosage reduction may be necessary in patients who develop toxicity or intolerable side effects. Cumulative doxorubicin doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
25 mg/m2 IV on weeks 1, 3, 5, 7, 9, and 11 in combination with mechlorethamine (6 mg/m2 IV on weeks 1, 5, and 9), vinblastine (6 mg/m2 IV on weeks 1, 3, 5, 7, 9, and 11), vincristine (1.4 mg/m2 [Max of 2 mg] IV on weeks 2, 4, 6, 8, 10, and 12), bleomycin (5 units/m2 IV on weeks 2, 4, 6, 8, 10, and 12), etoposide (60 mg/m2 per day IV on 2 consecutive days in weeks 3, 7, and 11), and prednisone (40 mg/m2 PO every other day for 10 weeks then tapered by 10 mg PO every other day between weeks 10 and 12). Total duration of Stanford V regimen is 12 weeks (three 4-week cycles).[40464] [40465] [36931] [40466] [40469] Doses of mechlorethamine, doxorubicin, vinblastine, and etoposide have been reduced to 65% if the absolute neutrophil count (ANC) is less than 1,000 cells/mm3 (treatment delayed if ANC is less than 500 cells/mm3). Prophylactic sulfamethoxazole-trimethoprim, acyclovir, and a H2-blocker were given throughout the treatment period.[40464] G-CSF has also been used to maintain dose intensity as needed after the first dose reduction.[40465] [40469] Alternative prophylactic medications have also been used.[36931] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Interruption of therapy and/or a dosage reduction may be necessary in patients who develop toxicity or intolerable side effects. Cumulative doxorubicin doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
25 mg/m2 IV on day 1 in combination with bleomycin (10 units/m2 IV on day 8), etoposide (100 mg/m2/day IV on days 1, 2, and 3), cyclophosphamide (650 mg/m2 IV on day 1), vincristine (1.4 mg/m2 [Max of 2 mg] IV on day 8), procarbazine (100 mg/m2 per day PO on days 1 to 7), and prednisone (40 mg/m2 PO on days 1 to 14). Cycles are repeated every 21 days for up to 8 cycles. Filgrastim was administered beginning on day 8 of each cycle and continued until the leukocyte count returned to normal in some clinical trials.[12501] [40572] The escalated dose BEACOPP regimen includes doxorubicin 35 mg/m2 IV on day 1 in combination with bleomycin (10 units/m2 IV on day 8), etoposide (200 mg/m2 per day IV on days 1, 2, and 3), cyclophosphamide (1,200 mg/m2 IV on day 1), vincristine (1.4 mg/m2 [Max of 2 mg] IV on day 8), procarbazine (100 mg/m2 per day PO on days 1 to 7), and prednisone (40 mg/m2 PO on days 1 to 14). Cycles are repeated every 21 days for up to 8 cycles. Filgrastim was administered beginning on day 8 of each cycle and continued until the leukocyte count returned to normal in some clinical trials.[12501] [40572] The standard dose BEACOPP and escalated dose BEACOPP regimens have shown benefit for the treatment of advanced Hodgkin lymphoma in clinical trials.[12501] [40572] [40568] Escalated dose BEACOPP has shown a significantly better freedom from treatment failure at 10 years (82% vs. 70%, p < 0.0001) and overall survival at 10 years (86% vs. 80%, p = 0.0053) compared to standard dose BEACOPP.[49830] A regimen of 4 cycles of escalated dose BEACOPP followed by 4 cycles of standard dose BEACOPP has also been used in patients who achieve a complete response after the initial 4 cycles of escalated dose BEACOPP.[40568] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Interruption of therapy and/or a dosage reduction may be necessary in patients who develop toxicity or intolerable side effects. Cumulative doxorubicin doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
25 mg/m2 IV in combination with brentuximab vedotin 1.2 mg/kg IV (not to exceed 120 mg/dose), vinblastine 6 mg/m2 IV, and dacarbazine 375 mg/m2 IV each given on days 1 and 15 repeated every 28 days for up to 6 cycles was evaluated in a randomized, phase III trial. Patients should receive primary prophylaxis with a granulocyte colony-stimulating factor due to the high incidence of febrile neutropenia.[62863] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Interruption of therapy and/or a dosage reduction may be necessary in patients who develop toxicity or intolerable side effects. Cumulative doxorubicin doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
25 mg/m2 IV on days 1 and 2 in combination with brentuximab vedotin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1; vincristine 1.4 mg/m2 IV on day 8; etoposide 125 mg/m2 IV on days 1, 2, and 3; prednisone 20 mg/m2 PO twice daily on days 1 to 7; and cyclophosphamide 600 mg/m2 IV on days 1 and 2 repeated every 3 weeks for up to 5 cycles. Administer primary prophylaxis with a granulocyte colony-stimulating factor starting in cycle 1 due to the high incidence of febrile neutropenia.[45378] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Interruption of therapy and/or a dosage reduction may be necessary in patients who develop toxicity or intolerable side effects. Cumulative doxorubicin doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628] At a median follow-up time of 42.1 (range, 0.1 to 80.9) months, the 3-year event-free survival rate was significantly improved in patients (median age, 15.6 years; range, 3.4 to 21.99 years) with newly diagnosed, stage IIB with bulk tumor or stage IIIB, IVA, or IVB classic Hodgkin lymphoma who received brentuximab vedotin plus AVEPC compared with doxorubicin, bleomycin, vincristine, etoposide, prednisone, and cyclophosphamide (ABVE-PC) (92.1% vs. 82.5%; hazard ratio = 0.41; 95% CI, 0.25 to 0.67) in a multicenter, randomized, phase 3 trial (n = 587). The 3-year overall survival rates were 99.3% and 98.5% in the brentuximab vedotin plus AVEPC and ABVE-PC arms, respectively.[68172]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
Multiple dosage regimens have been studied. Doxorubicin 40 mg/m2 IV on day 1 in combination with cyclophosphamide 750 mg/m2 IV on day 1 and vincristine 1.2 mg/m2 (Max of 2 mg) IV on day 1, every 4 weeks for 4 cycles.[51164] Doxorubicin 50 mg/m2 IV on day 1 in combination with cyclophosphamide 800 mg/m2 IV on day 1 and vincristine 1.4 mg/m2 (Max of 2 mg) IV on day 1, every 3 to 4 weeks for 4 cycles.[51165] Doxorubicin 40 mg/m2 IV on day 1 in combination with cyclophosphamide 1,000 mg/m2 IV on day 1 and vincristine 1 mg/m2 (Max of 2mg) IV on day 1, every 3 weeks for 6 cycles.[51166] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
45 mg/m2 IV on day 1 in combination with cyclophosphamide 1,000 mg/m2 IV on day 1 and etoposide 100 mg/m2 per day IV on days 1, 2, and 3 repeated every 3 weeks for 5 cycles.[51057] [50310] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
45 mg/m2 IV on day 1, given immediately before cisplatin (50 mg/m2) on day 1, then give paclitaxel (160 mg/m2) on day 2; repeated every 21 days. In clinical trials, treatment was continued for up to 7 cycles or until disease progression, and filgrastim (5 mcg/kg) was administered on days 3 to 12. A phase III trial showed an increase in response rate, progression-free survival, and overall survival in patients receiving paclitaxel, doxorubicin, and cisplatin (TAP) compared with cisplatin and doxorubicin alone. Thrombocytopenia and neuropathy were higher in the TAP arm.[33938] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
9 mg/m2 per day IV and vincristine 0.4 mg per day IV on days 1, 2, 3, and 4 plus dexamethasone (VAD regimen) repeated every 4 weeks for 3 to 4 cycles as induction therapy prior to autologous stem-cell transplantation has been studied in previously untreated multiple myeloma patients.[49477] [49478] Doxorubicin and vincristine were administered as a continuous IV infusion over 24 hours per day or as a daily IV infusion.[49477] [49478] Dexamethasone was given as 40 mg PO daily on days 1, 2, 3, and 4; 9, 10, 11, and 12; and 17, 18, 19, and 20 or as 40 mg PO daily days 1, 2, 3, and 4 on all cycles and days 9, 10, 11, and 12 and 17, 18, 19, and 20 on cycles 1 and 2 only.[49478] [49477] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 mg/m2 IV on day 1 in combination with cyclophosphamide 750 mg/m2 IV on day 1, vincristine 1.4 mg/m2 IV on day 1 (Max dose of 2 mg), and prednisone 50 mg/m2 PO once daily on days 1, 2, 3, 4, and 5, repeated every 21 days. After 3 cycles, patients with a complete response received 3 additional cycles, patients with a partial response received 5 additional cycles, and patients with progressive disease discontinued treatment.[52334] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 mg/m2 IV on day 1 in combination with rituximab 375 mg/m2 IV given on day 1 (or day 0), cyclophosphamide 750 mg/m2 IV on day 1, vincristine 1.4 mg/m2 IV (Max dose of 2 mg) on day 1, and prednisone 100 mg/m2 PO on days 1, 2, 3, 4, and 5 (R-CHOP regimen) repeated every 3 weeks for 6 to 8 cycles has been studied in previously untreated and previously treated patients with follicular lymphoma (FL) in randomized, phase III trials.[47202][47203][47204] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 mg/m2 IV on day 1 in combination with rituximab 375 mg/m2 IV on day 1, cyclophosphamide 750 mg/m2 IV on day 1, vincristine 1.4 mg/m2 (Max dose of 2 mg) IV on day 1, and prednisone 40 or 100 mg/m2 per day PO on days 1, 2, 3, 4, and 5 (R-CHOP) repeated every 21 days for up to 8 cycles has been evaluated in patients 60 years of age and older with previously untreated diffuse large B-cell lymphoma in randomized, clinical trials.[34649][31968] In a randomized, phase III study in 632 patients aged 60 years or older (range, 60 to 92 years), the 3-year failure-free survival rate was significantly higher with R-CHOP compared with CHOP (53% vs. 46%; hazard ratio (HR) = 0.78; 95% CI, 0.61 to 0.99; p = 0.04) at a median follow-up of 3.5 years. However, overall survival (OS) was not significantly improved in the R-CHOP arm (HR = 0.83; 95% CI, 0.63 to 1.09).[34649] In another randomized trial, the median progression-free survival (PFS) (4.8 vs. 1.2 years; p < 0.0001) and OS (8.4 vs. 3.5 years; p < 0.0001) times were significantly improved with R-CHOP compared with CHOP in 399 patients aged 60 to 75 years. The 10-year PFS rates were 36.5% and 20.1% in the R-CHOP and CHOP arms, respectively, and the 10-year OS rates were 43.5% and 27.6%, respectively.[47312] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 mg/m2 IV on day 1 in combination with polatuzumab vedotin 1.8 mg/kg IV, rituximab 375 mg/m2 IV, and cyclophosphamide 750 mg/m2 IV on day 1 plus prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 repeated every 21 days for 6 cycles has been evaluated in a randomized, double-blind, placebo-controlled, phase 3 trial (n = 879; the POLARIX trial). Rituximab 375 mg/m2 IV was continued for 2 additional cycles of therapy (cycles 7 and 8).[67350]
Multiple regimens have been studied. Doxorubicin 30 to 45 mg/m2 per day IV for 2 to 3 days monthly as a single agent (may be given daily in divided doses over 2 to 3 days) or 30 to 75 mg/m2 IV in combination with cisplatin or bleomycin, cyclophosphamide, methotrexate, and dactinomycin. Doxorubicin 25 mg/m2 per day IV on days 1, 2, and 3 or 37.5 mg/m2 per day IV on days 1 and 2 in combination with cisplatin, has been incorporated into multiple treatment protocols for osteogenic sarcoma. In the POG-8651 protocol, 106 patients (aged less than 30 years old) with previously untreated nonmetastatic high-grade osteogenic sarcoma were randomized to receive doxorubicin (37.5 mg/m2 per day IV on days 1 and 2) and cisplatin each cycle as part of a multiagent chemotherapy regimen in sequence with BCD (bleomycin, cyclophosphamide, and dactinomycin) and high-dose methotrexate, either before or after surgical resection. Patients also received single-agent doxorubicin (30 mg/m2 per day IV for 3 days) in week 20 of this regimen. Event-free survival (EFS), the primary endpoint, was not significantly different between the treatment arms, and reached 69% at 5 years in the post-operative group.[34600] In a comparison of the Memorial Sloan-Kettering Cancer Center T-10 and T-12 protocols, 73 patients (aged 4.6 to 36.4 years) with previously untreated, high-grade osteogenic sarcoma received doxorubicin (25 mg/m2 per day IV on days 1, 2, and 3) and cisplatin each cycle as part of a multiagent chemotherapy regimen in sequence with BCD, high-dose methotrexate, and surgical resection. The 5-year EFS was 78% and 73% in the T-12 and T-10 protocols, respectively.[34668] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
25 mg/m2 per day IV on days 1, 2, and 3 or 37.5 mg/m2 per day IV on days 1 and 2 in combination with cisplatin has been incorporated into multiple treatment protocols for osteogenic sarcoma. In the POG-8651 protocol, 106 patients (aged less than 30 years old) with previously untreated nonmetastatic high-grade osteogenic sarcoma were randomized to receive doxorubicin (37.5 mg/m2 per day IV on days 1 and 2) and cisplatin each cycle as part of a multiagent chemotherapy regimen in sequence with BCD (bleomycin, cyclophosphamide, and dactinomycin) and high-dose methotrexate, either before or after surgical resection. Patients also received single-agent doxorubicin (30 mg/m2 per day IV for 3 days) in week 20 of this regimen. Event-free survival (EFS), the primary endpoint, was not significantly different between the treatment arms, and reached 69% at 5 years in the post-operative group.[34600] In a comparison of the Memorial Sloan-Kettering Cancer Center T-10 and T-12 protocols, 73 patients (aged 4.6 to 36.4 years) with previously untreated, high-grade osteogenic sarcoma received doxorubicin (25 mg/m2 per day IV on days 1, 2, and 3) and cisplatin each cycle as part of a multiagent chemotherapy regimen in sequence with BCD, high-dose methotrexate, and surgical resection. The 5-year EFS was 78% and 73% in the T-12 and T-10 protocols, respectively.[34668] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628] Single-agent doxorubicin (given as 75 mg/m2 IV over 20 minutes on day 1 OR 25 mg/m2 per day as a continuous 24-hour IV infusion on days 1, 2, and 3) was compared with doxorubicin (25 mg/m2 per day as a IV bolus on days 1, 2, and 3) plus ifosfamide (2.5 grams/m2 per day IV over 4 hour on days 1, 2, 3, and 4) as first-line treatment of locally advanced, unresectable, or metastatic intermediate- or high-grade soft-tissue sarcoma in adult patients (age range, 18 to 63 years) in a multinational, randomized, open-label, phase III trial (n = 445; the EORTC 62012 trial). Patients in the doxorubicin/ifosfamide arm also received mesna (0.5 gram/m2 IV bolus prior to each ifosfamide dose, 1.5 grams/m2 IV over 4 hours given concurrently with each ifosfamide dose, and 1 gram/m2 orally at 2 and 6 hours after each ifosfamide infusion) and pegfilgrastim (6 mg subcutaneously given 24 hours after combination chemotherapy on day 5 of each cycle). Treatment was repeated every 3 weeks until disease progression or unacceptable toxicity, up to a maximum of 6 cycles. The median overall survival time (primary endpoint) was not significantly different with single-agent doxorubicin compared with doxorubicin/ifosfamide therapy (12.8 months vs. 14.3 months; hazard ratio (HR) = 0.83; 95.5% CI, 0.67 to 1.03; p = 0.076) at median follow-up times of 56 and 59 months, respectively. However, the median progression-free survival was significantly higher with doxorubicin/ifosfamide therapy (4.6 months vs. 7.4 months; HR = 0.74; 95.5% CI, 0.6 to 0.9; p = 0.003).[59636]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
15 mg/m2 per day as a continuous IV infusion over 24 hours (CIV) for 4 days in combination with dacarbazine 250 mg/m2 per day CIV for 4 days, ifosfamide 2,000 mg/m2 per day CIV for 3 days, and mesna 2,500 mg/m2 per day CIV for 4 days repeated every 21 days (median of 3 cycles) (MAID regimen) was evaluated in patients with soft-tissue and bone sarcomas in a randomized, phase III trial.[46189] Five cycles of an intensified MAID regimen was compared with 6 cycles of a more standard MAID regimen (dacarbazine 300 mg/m2 per day IV over 1 hour on days 1, 2, and 3 plus doxorubicin 20 mg/m2 per day as an IV bolus or CIV on days 1, 2, and 3; ifosfamide 2.5 grams/m2 per day IV over 3 hours on days 1, 2 and 3; and mesna 2.5 grams/m2 per day CIV on days 1, 2, and 3) in patients with inoperable locally advanced or metastatic soft-tissue sarcoma in another randomized, phase III study.[44784] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
Doxorubicin has been given in combination with carboplatin, cyclophosphamide, and etoposide. In Cycles 1 and 7: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg per day in children less than 12 kg) plus etoposide 120 mg/m2 per day IV on days 1, 2, and 3 (4 mg/kg per day in children less than 12 kg). Cycles 2 and 6: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg per day in children less than 12 kg) plus cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg per day in children less than 12 kg), and doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg per day in children less than 12 kg). Cycles 3 and 5: Cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg per day in children less than 12 kg) plus etoposide 120 mg/m2 per day IV on days 1, 2, and 3 (4 mg/kg/day in children less than 12 kg). Cycle 4: Carboplatin 560 mg/m2 IV on day 1 (18 mg/kg per day in children less than 12 kg) plus etoposide 120 mg/m2 per day IV on days 1, 2, and 3 (4 mg/kg per day in children less than 12 kg), and doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg per day in children less than 12 kg). Cycle 8: Cyclophosphamide 1,000 mg/m2 IV on day 1 (33 mg/kg per day in children less than 12 kg) plus doxorubicin 30 mg/m2 IV on day 1 (1 mg/kg per day in children less than 12 kg). All cycles given at 3 week intervals. Patients with favorable biologic features received 4 cycles; if incomplete response after 4 cycles, patients were given an additional 4 cycles. Patients with unfavorable biologic features received 8 cycles. Infants aged less than 60 days of age received granulocyte colony-stimulating factor after each cycle.[49848] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
60 to 75 mg/m2 IV repeated every 21 days as a single agent; 40 to 75 mg/m2 IV repeated every 21 to 28 days in combination with other chemotherapy agents. Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy. Avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers.[61628]
30 mg/m2 in combination with cisplatin 100 mg/m2, has been administered via intra-arterial administration as a solution or emulsified with the use of Lipiodol. Treatment was repeated every 2 months for at least 3 cycles.[50657] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
50 mg/m2 IV on day 1 plus cisplatin 50 mg/m2 IV on day 1 and cyclophosphamide 500 mg/m2 IV on day 1 (with 1 liter of hydration before and after chemotherapy) repeated every 21 days (PAC regimen) for up to 8 cycles (median of 7 cycles) in patients with previously untreated, unresectable, extensive-stage thymoma or for 2 or 4 cycles (median of 4 cycles; range, 1 to 7 cycles) followed by radiotherapy in patients with previously untreated, unresectable, limited-stage thymoma who had stable disease or better was evaluated in a nonrandomized study.[41507] [47366] Additionally, multimodality treatment with 3 cycles of doxorubicin 30 mg/m2 per day continuous IV infusion over 24 hours on days 1, 2, and 3; cisplatin 30 mg/m2 per day IV on days 1, 2, and 3; cyclophosphamide 500 mg/m2 IV on day 1; and prednisone 100 mg PO on days 1 to 5 repeated every 3 to 4 weeks followed by surgery and radiation therapy and then consolidation chemotherapy with doxorubicin, cisplatin, and cyclophosphamide given at 80% of the original doses and prednisone (given at 100%) repeated every 3 to 4 weeks for 3 cycles was evaluated in another nonrandomized study.[41508] In these studies, overall response rates and overall survival rates were favorable.[41507] [47366] [41508] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
40 mg/m2 IV on day 1 plus cisplatin 50 mg/m2 IV on day 1, vincristine 0.6 mg/m2 IV on day 3, and cyclophosphamide 700 mg/m2 IV on day 4 repeated every 3 weeks (median of 5 cycles; range, 3 to 7 cycles) resulted in a favorable overall response rate in a nonrandomized study of 37 patients.[41511] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
10 mg/m2 IV on day 1 in combination with bleomycin (15 units IV on day 1) and vincristine (1 mg IV on day 1), repeated every 2 weeks.[34595] Alternately, doxorubicin 20 mg/m2 IV on day 1 has been given in combination with bleomycin (10 mg/m2 IV on day 1) and vincristine (1 mg IV on day 1), repeated every 2 weeks for 6 cycles.[21306] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
40 mg/m2 per day IV on days 29 and 30 in combination with ifosfamide 6,000 mg/m2 continuous IV (CIV) over 48 hours on days 1, 29, and 50; mesna 6,000 mg/m2 CIV over 48 hours on days 1, 29, and 50; dactinomycin 0.5 mg/m2 per day IV on days 1, 2, and 3 and 50, 51, and 52; and vincristine 1.5 mg/m2 IV on days 1, 8, 15, and 22. The duration of therapy was dependent on stage at diagnosis (stage I: 16 weeks; II: 26 weeks; III: 40 weeks; IV: 48 weeks).[50231] FDA approved labeling for doxorubicin states to avoid concomitant use with CYP3A4, CYP2D6, and P-glycoprotein inhibitors and inducers and that cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy.[61628]
Doxorubicin 150 mg of 100 to 300 micron beads (given as 2 vials, each 2 mL in volume and containing 75 mg of doxorubicin) via intra-arterial chemoembolization. The maximum dose of doxorubicin was 150 mg/procedure. The beads were mixed with contrast before the procedure and injected slowly in 1 mL aliquots using a "sandwich technique" (i.e., beads then contrast) to identify and minimize reflux.[51160]
Chemoembolization material consisted of mitomycin 10 mg, doxorubicin 50 mg, and cisplatin 100 mg dissolved in sterile contrast (8.5 mL) and diluted with 1.5 mL of sterile water. This was emulsified in a 1:1 ratio with ethiodol. Added to the final aliquot of the emulsion or separately following administration of the emulsion was 0.2 mL of 150- to 250-l polyvinyl alcohol particles. Normal saline at 200 to 300 mL per hour until the completion of the procedure, followed by normal saline at 150 mL per hour for a total of 3 liters. No diuretics were given. Prophylactic antiemetics (ondansetron 24 mg and dexamethasone 10 mg intravenously) and antibiotics (cefazolin 1 g and metronidazole 500 mg) were given.[50654]
50 mg/m2 IV on day 1 in combination with brentuximab vedoin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1, cyclophosphamide 750 mg/m2 IV on day 1, and prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 given every 21 days for 6 to 8 cycles of therapy. The progression-free survival (PFS) time (evaluated via an independent review facility) was significantly improved in patients with CD30-expressing sALCL or peripheral T-cell lymphoma who received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (CHP) compared with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (48.2 months vs. 20.8 months; hazard ratio (HR) = 0.71; 95% CI, 0.54 to 0.93) in a multicenter, randomized, double-blind, phase 3 trial (the ECHELON-2 trial; n = 452). Overall survival was also significantly improved in the brentuximab vedotin-containing arm (HR = 0.66; 95% CI, 0.46 to 0.95). In patients with sALCL (n = 314; anaplastic lymphoma kinase (ALK)-negative sALCL, 48%; ALK-positive sALCL, 22%), the PFS times were 55.7 months and 54.2 months in patients who received brentuximab vedotin plus CHP and CHOP, respectively (HR = 0.59; 95% CI, 0.42 to 0.84).[45378]
50 mg/m2 IV on day 1 in combination with brentuximab vedotin 1.8 mg/kg (not to exceed 180 mg/dose) IV on day 1, cyclophosphamide 750 mg/m2 IV on day 1, and prednisone 100 mg orally daily on days 1, 2, 3, 4, and 5 given every 21 days for 6 to 8 cycles of therapy. The progression-free survival time (evaluated via an independent review facility) was significantly improved in patients with CD30-expressing systemic anaplastic large-cell lymphoma (sALCL) or PTCL who received brentuximab vedotin plus cyclophosphamide, doxorubicin, and prednisone (CHP) compared with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) (48.2 months vs. 20.8 months; hazard ratio (HR) = 0.71; 95% CI, 0.54 to 0.93) in a multicenter, randomized, double-blind, phase 3 trial (the ECHELON-2 trial; n = 452). Overall survival was also significantly improved in the brentuximab vedotin-containing arm (HR = 0.66; 95% CI, 0.46 to 0.95). In this trial, 70% of patients had sALCL and 30% of patients had PTCL (e.g., including PTCL not otherwise specified (16%), angioimmunoblastic T-cell lymphoma (12%), adult T-cell leukemia/lymphoma (2%), and enteropathy-associated T-cell lymphoma (less than 1%))[45378]
Recommended Monitoring
Maximum lifetime cumulative dosage of doxorubicin is 550 mg/m2 IV; 450 mg/m2 IV in patients who have received previous mediastinal radiation.
Maximum lifetime cumulative dosage of doxorubicin is 550 mg/m2 IV; 450 mg/m2 IV in patients who have received previous mediastinal radiation.
Maximum lifetime cumulative dosage of doxorubicin is 550 mg/m2 IV; 450 mg/m2 IV in patients who have received previous mediastinal radiation.
Maximum lifetime cumulative dosage of doxorubicin is 550 mg/m2 IV; 450 mg/m2 IV in patients who have received previous mediastinal radiation. The dose should be based on body weight for children with a BSA < 0.5 m2. Children are more susceptible to cardiotoxicity and require long term follow-up.
Consult individual protocols for hepatic dosage recommendations.
A dosage adjustment is necessary in patients with hepatic impairment as follows:
Serum bilirubin level of 1.2 to 3 mg/dL: decrease dose by 50%.
Serum bilirubin level of 3.1 to 5 mg/dL: decrease dose by 75%.
Severe hepatic impairment (Child-Pugh Class C) or serum bilirubin level greater than 5 mg/dL: use is contraindicated.[61628]
Additional recommendations for hepatic dose adjustments have been described in the literature.[67274]
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication


Doxorubicin is a cytotoxic anthracycline antibiotic that inhibits nucleotide replication by intercalation into DNA and RNA; it is also a topoisomerase II inhibitor. Doxorubicin is indicated for the treatment of acute lymphoblastic leukemia, acute myeloblastic leukemia, Hodgkin lymphoma, non-Hodgkin lymphoma, metastatic breast cancer, metastatic Wilms' tumor, metastatic neuroblastoma, metastatic soft tissue sarcoma, metastatic bone sarcoma, metastatic ovarian cancer, metastatic transitional cell bladder cancer, metastatic thyroid cancer, metastatic gastric cancer, and metastatic lung cancer; it is also indicated for the adjuvant treatment of breast cancer.[61628]
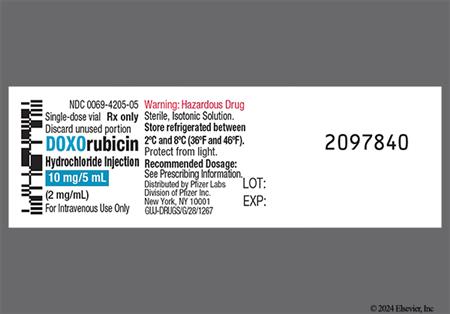
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Emetic Risk
Pediatric patients
Adults
Administer routine antiemetic prophylaxis prior to treatment.[67392][67389]
Extravasation Risk
Patient Counseling
Reconstitution of the Lyophilized Powder Vial
Intravenous (IV) Injection
Continuous IV infusion
Intraarterial Administration
NOTE: Doxorubicin is not approved by the FDA for intraarterial administration.
Hepatic artery chemoembolization:
Bone marrow suppression including reversible, dose-dependent neutropenia has been reported with doxorubicin therapy; blood or platelet transfusions, hospitalization, and death may occur with doxorubicin use. Monitor complete blood counts (CBC) prior to starting doxorubicin; monitor CBC and for signs of clinical complications (e.g., infections, bleeding) during therapy. Septic shock (2%), systemic infection (2%), and severe leukopenia (grade 3, 3.4%; grade 4, 0.3%) and thrombocytopenia (grade 4, 0.1%) were reported in women who received 4 cycles of doxorubicin 60 mg/m2 IV plus cyclophosphamide 600 mg/m2 IV (AC regimen) repeated every 3 weeks for the adjuvant treatment of axillary lymph-node positive breast cancer (n = 1,492). When doxorubicin is given every 3 weeks, the neutrophil count nadir is reached at 10 to 14 days following the dose.[61628]
Cardiotoxicity, including cardiomyopathy, pericarditis, myocarditis, and left ventricular heart failure has been reported with doxorubicin therapy. Assess left ventricular function (e.g., MUGA or echocardiogram) before starting doxorubicin therapy and then regularly during and after therapy; use the same method of assessment at all time points. If the cumulative doxorubicin dose exceeds 300 mg/m2 in a patient that will continue to receive therapy, increase the frequency of cardiac assessment and consider starting dexrazoxane to reduce the incidence and severity of cardiomyopathy. The incidence of cardiotoxicity is highest in patients who exceed the maximum cumulative lifetime dose of 550 mg/m2. Cardiomyopathy may develop during treatment or up to several years after the completion of treatment. The estimated risk of developing cardiomyopathy (when doxorubicin is given every 3 weeks) is 1% to 2% at a cumulative dose of 300 mg/m2, 3% to 5% at a cumulative dose of 400 mg/m2, and 6% to 20% at a cumulative dose of 500 mg/m2. Asymptomatic cardiac dysfunction occurred in 0.2% of women who received 4 cycles of doxorubicin 60 mg/m2 IV plus cyclophosphamide 600 mg/m2 IV (AC regimen) repeated every 3 weeks for the adjuvant treatment of axillary lymph-node positive breast cancer (n = 1,492); transient (0.1%) and symptomatic (0.1%) cardiac dysfunction were also reported. Cardiogenic shock was reported in postmarketing surveillance of doxorubicin.[61628]
Fever and chills have been reported in postmarketing surveillance of doxorubicin.[61628]
Gastrointestinal (GI) adverse events including nausea, mucositis/oral ulceration, stomatitis, necrotizing colitis, typhlitis, gastric erosion/peptic ulcer, GI bleeding, hematochezia, esophagitis, anorexia, abdominal pain, dehydration, diarrhea, hyperpigmentation of the oral mucosa have been reported with doxorubicin therapy. Vomiting for 12 hours or less (34%), vomiting for greater than 12 hours (37%), and intractable vomiting (5%) were reported in women who received 4 cycles of doxorubicin 60 mg/m2 IV plus cyclophosphamide 600 mg/m2 IV (AC regimen) repeated every 3 weeks for the adjuvant treatment of axillary lymph-node positive breast cancer (n = 1,492).[61628]
Alopecia was reported in 92% of women who received 4 cycles of doxorubicin 60 mg/m2 IV plus cyclophosphamide 600 mg/m2 IV (AC regimen) repeated every 3 weeks for the adjuvant treatment of axillary lymph-node positive breast cancer (n = 1,492). Skin hyperpigmentation, nail discoloration/disorder, onycholysis, rash (unspecified), pruritus, photosensitivity, urticaria, acral erythema, and palmar-plantar erythrodysesthesia (hand and foot syndrome) have been reported in postmarketing surveillance of doxorubicin.[61628]
Urine discoloration, specifically red coloration of urine for 1 to 2 days after administration, has been reported with IV doxorubicin use.[61628]
Conjunctivitis, keratitis, and lacrimation have been reported in postmarketing surveillance of doxorubicin.[61628]
Injection site reaction (e.g., extravasation, skin ulcer, severe local tissue necrosis) has been reported with doxorubicin therapy; wide excision of the affected area and skin grafting may be necessary if severe tissue injury occurs. Immediately stop the injection or infusion of doxorubicin if signs or symptoms of extravasation occur. If extravasation occurs or is suspected, apply ice at the site for 15 minutes 4 times daily for 3 days; administer dexrazoxane at the site as soon as possible and within the first 6 hours following extravasation. Extravasation may occur in the absence of typical symptoms (e.g., stinging or burning sensation) or when patients have adequate blood return on aspiration of the infusion needle. If doxorubicin is administered through a peripheral IV line, infuse doxorubicin over 10 minutes or less to minimize the risk of extravasation. Decrease the rate of doxorubicin infusion if erythematous streaking along the vein proximal to the site of infusion or facial flushing occur. Phlebosclerosis and phlebitis/thrombophlebitis have been reported in postmarketing surveillance of doxorubicin.[61628]
Anaphylactoid reactions have been reported in postmarketing surveillance of doxorubicin.[61628]
A radiation recall reaction that may include cutaneous or pulmonary toxicity has been reported in doxorubicin-treated patients who received prior radiation therapy.[61628]
Tumor lysis syndrome (TLS) may occur in patients with rapidly growing tumors who received doxorubicin. Monitor serum electrolytes (e.g., potassium, calcium, phosphorus), uric acid levels, and serum creatinine prior to and during initial treatment. Administer hydration, urine alkalinization, and uric acid lowering therapy (e.g., allopurinol) as necessary to minimize the risk of complications associated with TLS.[61628]
A new primary malignancy, including acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS), has been reported with doxorubicin therapy. In patients who received doxorubicin as adjuvant treatment for breast cancer, the cumulative incidence of secondary malignancy ranged from 0.2% at 5 years to 1.5% at 10 years in 2 separate trials; AML/MDS typically occurred within 1 to 3 years following treatment.[61628]
Doxorubicin may cause gonadal suppression and infertility. Amenorrhea and premature menopause have been reported in females of reproductive potential who received doxorubicin. Ovulation and menstruation may return when therapy is discontinued. The recovery of menses is related to age at treatment. Oligospermia, azoospermia, and spermatogenesis inhibition resulting in permanent loss of fertility have occurred in males treated with doxorubicin. Sperm counts returned to normal levels in some men, sometimes several years after the end of treatment. Gonadal suppression/impairment has been reported in pediatric patients who received doxorubicin as part of intensive chemotherapy; most cases were reversible.[61628]
Elevated hepatic enzymes (i.e., increased ALT and AST levels) have been reported in postmarketing surveillance of doxorubicin. Monitor liver function tests prior to starting doxorubicin and during therapy. A dose reduction is recommended in patients with mild or moderate hepatic disease/impairment (serum bilirubin levels of 1.2 to 5 mg/dL).[61628]
Weight gain has been reported in postmarketing surveillance of doxorubicin.[61628]
Malaise/asthenia has been reported in postmarketing surveillance of doxorubicin.[61628]
Prepubertal growth inhibition/failure have been reported in pediatric patients who received doxorubicin as part of intensive chemotherapy; gonadal impairment was usually reversible.[61628]
Peripheral neuropathy (sensory and motor), seizures, and coma have been reported in postmarketing surveillance of doxorubicin.[61628]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Doxorubicin is contraindication in patients with severe hepatic impairment, including hepatic failure (Child-Pugh class C or serum bilirubin levels greater than 5 mg/dL). Use doxorubicin with caution in patients with mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment (serum bilirubin levels 1.2 to 5 mg/dL); a dose reduction is recommended in these patients. Monitor liver function tests prior to starting doxorubicin and during therapy.[61628]
Doxorubicin is contraindicated in patients with severe myocardial insufficiency or recent (occurring within the past 4 to 6 weeks) myocardial infarction. Use doxorubicin with caution in patients with pre-existing cardiac disease. Cardiotoxicity (e.g., cardiomyopathy, pericarditis, myocarditis, left ventricular heart failure) may develop during doxorubicin therapy or up to several years after completion of treatment. High cumulative anthracycline or anthracenedione doses, concomitant cardiotoxicity medication (e.g., cyclophosphamide, trastuzumab), and prior thoracic radiation therapy may increase the risk of cardiotoxicity. The incidence of cardiotoxicity is highest in patients who exceed the maximum cumulative lifetime dose of 550 mg/m2. Assess left ventricular function (e.g., MUGA or echocardiogram) before starting doxorubicin therapy and then regularly during and after therapy; use the same method of assessment at all time points. If the cumulative doxorubicin dose exceeds 300 mg/m2 in a patient that will continue to receive therapy, increase the frequency of cardiac assessment and consider starting dexrazoxane to reduce the incidence and severity of cardiomyopathy.[61628]
Doxorubicin is contraindicated in patients with severe persistent drug-induced bone marrow suppression. Severe myelosuppression/bone marrow suppression (leukopenia, neutropenia, thrombocytopenia) has been reported with doxorubicin therapy; serious infection, septic shock, blood or platelet transfusions, hospitalization, and death may occur. Monitor complete blood counts (CBC) prior to starting doxorubicin; monitor CBC and for signs of clinical complications (e.g., infection, bleeding) during therapy.[61628]
Extravasation and severe local tissue necrosis have been reported with doxorubicin therapy; wide excision of the affected area and skin grafting may be necessary if severe tissue injury occurs.[61628]
A new primary malignancy, including acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS), has been reported with doxorubicin therapy. In patients who received doxorubicin as adjuvant treatment for breast cancer, the cumulative incidence of secondary malignancy ranged from 0.2% at 5 years to 1.5% at 10 years in 2 separate trials; AML/MDS typically occurred within 1 to 3 years following treatment.[61628]
Use doxorubicin with caution in patients receiving concurrent radiation therapy and in patients who have received prior radiation therapy. Increased toxicity to the myocardium, mucosa, skin, and liver may occur when doxorubicin is used concurrently with radiation therapy. Radiation recall (e.g., cutaneous toxicity, pulmonary toxicity) may occur in patients who receive doxorubicin after prior radiation therapy.[61628]
Doxorubicin is pregnancy category D. It may cause fetal harm when administered to a pregnant woman. Females of reproductive potential should avoid pregnancy during doxorubicin therapy. Apprise the patient of the potential hazard to a fetus if doxorubicin is used during pregnancy or if the patient becomes pregnant while taking doxorubicin. In animal studies in rats and rabbits, doxorubicin was teratogenic (e.g., esophageal and intestinal atresia, tracheo-esophageal fistula, hypoplasia of the urinary bladder, and cardiovascular anomalies) and embryotoxic at doses approximately 0.07-times (based on body surface area) the recommended human dose of 60 mg/m2.[61628]
Counsel patients about the reproductive risk and contraception requirements during doxorubicin treatment. Females of reproductive potential should use effective contraception during and for 6 months after treatment with doxorubicin. Due to male-mediated teratogenicity, men with female partners of reproductive potential should use effective contraception during therapy and for 6 months following the final dose of doxorubicin. Doxorubicin may cause infertility; amenorrhea has been reported in females and oligospermia, azoospermia, and permanent loss of fertility have been reported in males. Sperm counts returned to normal levels in some men who received doxorubicin, sometimes several years after the end of treatment.[61628]
Doxorubicin has been detected in breast milk and should not be administered in breast-feeding women. Peak milk concentrations in 1 patient were approximately 4.4-times greater than plasma concentrations 24 hours after treatment. Doxorubicin was detectable in breast milk up to 72 hours after therapy. Due to the potential for serious adverse reactions in nursing infants from doxorubicin, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.[61628]
Pediatric patients including adolescents, children, and infants are at risk for developing late cardiovascular dysfunction with anthracycline therapy. Pediatric patients should receive long-term, periodic cardiac evaluations after receiving doxorubicin. Risk factors include young age at treatment (especially in children less than 5 years of age), high cumulative doses, and a history of receiving combined modality therapy. Prepubertal growth inhibition/failure and gonadal impairment have been reported in pediatric patients who received doxorubicin as part of intensive chemotherapy; gonadal impairment was usually reversible.[61628] Due to the risk of long-term cardiotoxicity, it has been recommended that patients treated with anthracyclines should undergo screening with electrocardiograms and echocardiograms every 2 years and 24-hour continuous electrocardiograms and radionuclide angiograms every 5 years.[25383]
Doxorubicin is a cytotoxic anthracycline antibiotic derived from Streptomyces peucetius. It prevents the replication of rapidly growing cells by intercalating between base pairs of the DNA/RNA strand and inhibiting DNA and RNA synthesis. Doxorubicin is also a topoisomerase II inhibitor that works by stabilizing the covalently bound form of the topoisomerase II enzyme with DNA causing increased topoisomerase II cross-linked DNA strand breaks.[61628] Several mechanisms of doxorubicin-induced cardiotoxicity have been proposed including iron-catalyzed induction of cardiac oxidative stress, altered calcium homeostasis, impaired gene expression of cardiac proteins, dysregulation of protein degradation by the ubiquitin–proteasome system, induction of mitochondrial DNA lesions, and interference with topoisomerase II. Doxorubicin undergoes one-electron reduction to form oxygen free radical intermediates. In the presence of oxygen and metal catalysts such as iron (Fe2+), doxorubicin undergoes reduction to the semiquone radical. In the presence of oxygen, the semiquone radical can form a superperoxide that in the presence of hydrogen peroxide forms hydroxyl radicals. Mitochondria appear to be an important target for anthracycline-induced cardiotoxicity; anthracyclines are found in high concentrations in the mitochondrial compartment. Doxorubicin binds with high-affinity to cardiolipin, a major phospholipid component of heart mitochondrial inner membranes.[61705]
Revision Date: 10/15/2025, 01:33:00 AMDoxorubicin is administered intravenously (IV). Doxorubicin and its major metabolite, doxorubicinol, are approximately 75% bound to plasma proteins; binding is independent of plasma concentration up to 1.1 mcg/mL. It does not cross the blood brain barrier. In pharmacokinetic analyses of doxorubicin, the steady-state volume of distribution was 809 to 1,214 L/m2, the plasma clearance was 324 to 809 mL/min/m2, and the terminal half-life was 20 to 48 hours. Doxorubicin is primarily excreted in the bile. Following a doxorubicin IV dose, about 40% of the dose is found in the bile and 5% to 12% of the parent drug and its metabolites appear in the urine within 5 days. Less than 3% of the dose is recovered as doxorubicinol in the urine within 7 days. The AUC ratio between doxorubicinol and doxorubicin is about 0.5.
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: CYP2D6, CYP3A4, P-gp
Doxorubicin is metabolized via CYP3A4 and CYP2D6; it is also a P-glycoprotein (P-gp) substrate. Avoid concomitant use with CYP3A4, CYP2D6, or P-gp inhibitors and inducers.[61628]
In cancer patients, doxorubicin exhibits multiphasic disposition after an IV injection. It had dose independent pharmacokinetics in 4 patients receiving doxorubicin 30 to 70 mg/m2.[61628]
The clearance of doxorubicin is reduced in patients with elevated serum bilirubin levels.[61628]
In a pharmacokinetic analysis in pediatric patients (n = 60; age range, 2 months to 20 years), the clearance was 1,443 +/- 114 mL/min/m2) following doxorubicin 10 to 75 mg/m2 IV. The clearance was 1,540 mL/min/m2 in pediatric patients greater than 2 years of age which was increased compared with adult patients. The clearance was 813 mL/min/m2 in patients younger than 2 years of age.[61628]
Gender did not significantly affect doxorubicin pharmacokinetics in a clinical study. A higher median clearance (1,088 vs. 433 mL/min/m2) and a longer half-life (54 vs. 35 hours) were reported in men (n = 6) compared to women (n = 21) who received doxorubicin.[61628]
The systemic clearance of doxorubicin was significantly reduced in obese women with an ideal body weight (IBW) greater than 130% compared with patients with less than 115% of IBW. There was no change in volume of distribution.[61628]
Doxorubicin is pregnancy category D. It may cause fetal harm when administered to a pregnant woman. Females of reproductive potential should avoid pregnancy during doxorubicin therapy. Apprise the patient of the potential hazard to a fetus if doxorubicin is used during pregnancy or if the patient becomes pregnant while taking doxorubicin. In animal studies in rats and rabbits, doxorubicin was teratogenic (e.g., esophageal and intestinal atresia, tracheo-esophageal fistula, hypoplasia of the urinary bladder, and cardiovascular anomalies) and embryotoxic at doses approximately 0.07-times (based on body surface area) the recommended human dose of 60 mg/m2.[61628]
Doxorubicin has been detected in breast milk and should not be administered in breast-feeding women. Peak milk concentrations in 1 patient were approximately 4.4-times greater than plasma concentrations 24 hours after treatment. Doxorubicin was detectable in breast milk up to 72 hours after therapy. Due to the potential for serious adverse reactions in nursing infants from doxorubicin, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.[61628]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.