ThisiscontentfromElsevier'sDrugInformation
Evolocumab
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
General Dosing Information
140 mg subcutaneously every 2 weeks or 420 mg subcutaneously once monthly. If switching dosage regimens, administer the first dose of the new regimen on the next scheduled date of the previous regimen.[60127]
140 mg subcutaneously every 2 weeks or 420 mg subcutaneously once monthly. If switching dosage regimens, administer the first dose of the new regimen on the next scheduled date of the previous regimen.[60127]
420 mg subcutaneously once monthly. Increase to 420 mg subcutaneously every 2 weeks if a clinically meaningful response is not attained in 12 weeks.[60127]
420 mg subcutaneously once monthly. Increase to 420 mg subcutaneously every 2 weeks if a clinically meaningful response is not attained in 12 weeks.[60127]
420 mg subcutaneously once monthly or every 2 weeks to correspond with apheresis schedule (administer after apheresis session is complete). For those initiated on monthly dosing, increase to 420 mg subcutaneously every 2 weeks if a clinically meaningful response is not attained in 12 weeks.[60127]
420 mg subcutaneously once monthly or every 2 weeks to correspond with apheresis schedule (administer after apheresis session is complete). For those initiated on monthly dosing, increase to 420 mg subcutaneously every 2 weeks if a clinically meaningful response is not attained in 12 weeks.[60127]
140 mg subcutaneously every 2 weeks or 420 mg subcutaneously once monthly. If switching dosage regimens, administer the first dose of the new regimen on the next scheduled date of the previous regimen.[60127]
420 mg/dose subcutaneously once monthly for most indications or every 2 weeks for homozygous familial hypercholesterolemia (HoFH).
420 mg/dose subcutaneously once monthly for most indications or every 2 weeks for homozygous familial hypercholesterolemia (HoFH).
420 mg/dose subcutaneously once monthly for heterozygous familial hypercholesterolemia (HeFH) or every 2 weeks for homozygous familial hypercholesterolemia (HoFH).
10 to 12 years: 420 mg/dose subcutaneously once monthly for heterozygous familial hypercholesterolemia (HeFH) or every 2 weeks for homozygous familial hypercholesterolemia (HoFH).
1 to 9 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Mild to moderate hepatic impairment (Child-Pugh A or B): No dosage adjustment is needed.
Severe hepatic impairment: Specific guidelines for dosage adjustments are not available.[60127]
No dosage adjustment is needed.[60127]
† Off-label indication

Evolocumab is a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor indicated as an adjunct to diet and exercise for the treatment of primary hypercholesterolemia, including heterozygous familial hypercholesterolemia (HeFH), and for the treatment of homozygous familial hypercholesterolemia (HoFH). Additionally, evolocumab is also indicated to reduce the risk of myocardial infarction, stroke, and coronary revascularization in individuals at increased risk for these events. During various clinical trials, evolocumab produced negative mean differences from placebo from baseline in LDL-C ranging from 31% to 71%.[60127] Evolocumab is recommended as second-line therapy in addition to maximally tolerated statin therapy in individuals with clinical atherosclerotic cardiovascular disease (ASCVD) and comorbidities that still require 25% or greater LDL-C reduction. Factors to consider include cost, benefit of ASCVD risk reduction, dosing frequency requirements, and administration by subcutaneous injection.[63783] Evolocumab was FDA-approved in 2015.[60127]
For storage information, see the specific product information within the How Supplied section.
Single-use prefilled syringe administration
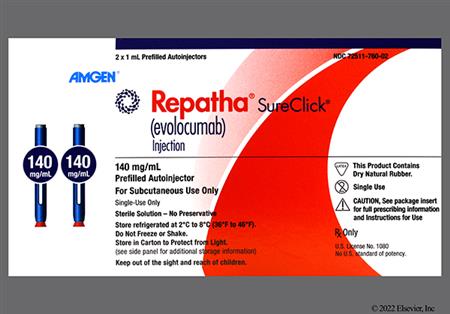
Single-use SureClick autoinjector administration
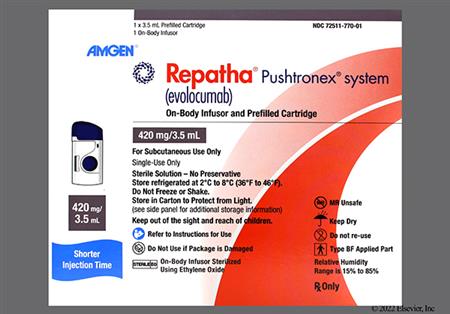
Single-use on-body infusor with prefilled cartridge (Pushtronex system) administration
Naso-pharyngitis (4% to 12%), upper respiratory tract infection (2% to 9%), influenza (1% to 9%), cough (1% to 5%), urinary tract infection (1% to 5%), and sinusitis (4%) were reported in evolocumab-treated patients during clinical trials. Influenza-like illness has been reported with postmarketing use of evolocumab.[60127]
Hypersensitivity reactions were reported in 5% of patients receiving evolocumab during clinical trials. The most common reactions included rash (1%), eczema (0.4%), erythema (0.4%), and urticaria (0.4%). Angioedema has been reported with postmarketing use. If signs or symptoms of serious hypersensitivity reactions, anaphylaxis, or anaphylactoid reactions occur, discontinue evolocumab treatment, treat with standard of care, and monitor until symptoms resolve.[60127]
Diarrhea (3%), gastroenteritis (3% to 6%), and nausea (2%) were reported in evolocumab-treated patients during clinical trials. Oropharyngeal pain was reported in 7% of pediatric patients.[60127]
Back pain (2% to 6%), arthralgia (2%), myalgia (4%), muscle cramps/spasms (1%), musculoskeletal pain (3%), fatigue (2%), and contusion (1%) were reported in evolocumab-treated patients during clinical trials.[60127]
Injection site reaction, including erythema, pain, and bruising, was reported in 3% to 6% of evolocumab-treated patients during clinical trials.[60127]
Hypertension (3%), headache (4%), and dizziness (4%) were reported in evolocumab-treated patients during clinical trials. Headache was reported in 11% of pediatric patients.[60127]
Antibody formation may occur with evolocumab. In a pool of placebo- and active-controlled clinical trials, 0.3% of adult patients treated with at least 1 dose of evolocumab tested positive for binding antibody development. Patients who tested positive for binding antibodies were tested for neutralizing antibodies, and none of the patients were positive for neutralizing antibodies. The development of anti-evolocumab antibodies was not detected in pediatric clinical trials. There is no evidence that the presence of anti-drug antibodies impacts the pharmacokinetics, clinical response, or safety of evolocumab.[60127]
Hyperglycemia (reported as diabetes mellitus) was reported in 9% of adult patients receiving evolocumab and 8% of those receiving placebo during the cardiovascular outcomes trial. The incidence of new-onset diabetes mellitus during the trial was approximately 8% in both groups.[60127]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. The evolocumab prefilled single-dose autoinjector and prefilled single-dose syringe formulations that contain dry natural rubber (a derivative of latex) in the needle cover may cause an allergic reaction in individuals with latex hypersensitivity. Instruct individuals to inform their healthcare provider if they are sensitive to latex. Consider prescribing a formulation of evolocumab that does not contain dry natural rubber for individuals that are sensitive to latex.[60127]
Do not expose the Pushtronex system, a single-use on-body infuser for evolocumab, to a magnetic resonance environment, such as magnetic resonance imaging (MRI).[60127]
Available data from clinical trials and postmarketing reports on the use of evolocumab in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or other adverse maternal or fetal outcomes. No effects on pregnancy or neonatal or infant development were observed when monkeys were given evolocumab from organogenesis through parturition at dose exposures up to 12 times the maximum recommended human dose. Measurable evolocumab serum concentrations were observed in infant monkeys at birth at comparable concentrations in maternal serum, indicating that evolocumab, like other IgG antibodies, crosses the placental barrier. Monoclonal antibodies are transported across the placenta in increasing amounts especially near term; therefore, there is a potential for evolocumab to be transmitted from mother to the developing fetus. Before administering evolocumab to a pregnant woman, consider the benefits and risks of treatment to the mother and the possible risks to the fetus. There is a pregnancy exposure registry that monitors outcomes in pregnant patients exposed to evolocumab; information about the registry can be obtained at mothertobaby.org-ongoinf-study/repatha or by calling 1-800-772-6436.[60127]
There are no data on the presence of evolocumab in human milk, the effects on the breast-fed child, or the effects on milk production. Human IgG is present in human milk, but data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts. Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for evolocumab and any potential adverse effects on the breast-fed child from evolocumab or from the underlying maternal condition.[60127]
Evolocumab is a human monoclonal IgG2 antibody that binds to and inhibits proprotein convertase subtilisin/kexin type 9 (PCSK9) binding to low-density lipoprotein receptors (LDLR). PCSK9 binds to LDLR on the hepatocyte surface to promote LDLR degradation within the liver. LDLR is the primary receptor that clears circulating LDL; with evolocumab inhibiting the binding of PCSK9 to LDLR, the number of LDLRs available to clear LDL increases, thereby lowering LDL-C concentrations.[60127]
Revision Date: 09/02/2025, 01:36:44 PMEvolocumab is administered subcutaneously. The Vd following a single subcutaneous dose of 420 mg was 3.3 L. At low concentrations, evolocumab is eliminated primarily via saturable binding to proprotein convertase subtilisin/kexin type 9 (PCSK9). At higher concentrations, evolocumab is eliminated mainly through a non-saturable proteolytic pathway. The estimated effective half-life of evolocumab is 11 to 17 days. Maximum LDL-C reduction occurred 2 weeks after a single dose of 140 mg and 3 weeks after a single dose of 420 mg.[60127]
Affected cytochrome P450 isoenzymes and drug transporters: none
The absolute bioavailability after subcutaneous administration is 72%. The median Tmax after administration of single doses of 140 mg or 420 mg to adult patients is 3 to 4 days. Maximum suppression of free circulating PCSK9 occurs within 4 hours after a single subcutaneous dose of evolocumab 140 mg or 420 mg and returns to baseline once evolocumab concentrations are undetectable. Evolocumab exhibits non-linear pharmacokinetics. Following administration of a subcutaneous dose of 140 mg and 420 mg to healthy adults, the mean Cmax was 18.6 mcg/mL and 59 mcg/mL, respectively. An approximate 2- to 3-fold accumulation is observed in trough serum concentrations after 140 mg doses administered every 2 weeks (Cmin 7.21) or 420 mg doses administered monthly (Cmin 11.2). Steady state is reached within 12 weeks of dosing.[60127]
The mean Cmax and AUC are lower (20% to 30% and 40% to 50%, respectively) in patients with mild and moderate hepatic impairment. Evolocumab has not been studied in patients with severe hepatic impairment.[60127]
Since monoclonal antibodies are not known to be eliminated via renal pathways, renal function is not expected to impact the pharmacokinetics of evolocumab. In a clinical trial of 18 adult patients with either normal renal function (eGFR 90 mL/minute/1.73 m2 or more; n = 6), severe renal impairment (eGFR less than 30 mL/minute/1.73 m2; n = 6), or end-stage renal disease (ESRD) receiving hemodialysis (n = 6), exposure to evolocumab after a single 140 mg subcutaneous dose was decreased in patients with severe renal impairment or ESRD receiving hemodialysis. Reductions in PCSK9 concentrations in patients with severe renal impairment or ESRD receiving hemodialysis were similar to those with normal renal function.[60127]
Children and Adolescents 10 to 17 years
Mean trough serum concentrations of evolocumab were 22.4 mcg/mL and 25.8 mcg/mL over Week 12 and Week 24 time points, respectively, during clinical trials in 103 pediatric patients with heterozygous familial hypercholesteremia (HeFH). Mean trough serum concentrations of evolocumab were 20.3 mcg/mL and 17.6 mcg/mL over Week 12 and Week 80 time points, respectively, during clinical trials in 12 pediatric patients with homozygous familial hypercholesteremia (HoFH).[60127]
Age was not shown to have an effect on the pharmacokinetics of evolocumab.[60127]
Gender was not shown to have an effect on the pharmacokinetics of evolocumab.[60127]
Race was not shown to have an effect on the pharmacokinetics of evolocumab.[60127]
Evolocumab exposure has been found to decrease with increasing body weight; however, these differences are not clinically meaningful.[60127]
Available data from clinical trials and postmarketing reports on the use of evolocumab in pregnant women are insufficient to evaluate for a drug-associated risk of major birth defects, miscarriage, or other adverse maternal or fetal outcomes. No effects on pregnancy or neonatal or infant development were observed when monkeys were given evolocumab from organogenesis through parturition at dose exposures up to 12 times the maximum recommended human dose. Measurable evolocumab serum concentrations were observed in infant monkeys at birth at comparable concentrations in maternal serum, indicating that evolocumab, like other IgG antibodies, crosses the placental barrier. Monoclonal antibodies are transported across the placenta in increasing amounts especially near term; therefore, there is a potential for evolocumab to be transmitted from mother to the developing fetus. Before administering evolocumab to a pregnant woman, consider the benefits and risks of treatment to the mother and the possible risks to the fetus. There is a pregnancy exposure registry that monitors outcomes in pregnant patients exposed to evolocumab; information about the registry can be obtained at mothertobaby.org-ongoinf-study/repatha or by calling 1-800-772-6436.[60127]
There are no data on the presence of evolocumab in human milk, the effects on the breast-fed child, or the effects on milk production. Human IgG is present in human milk, but data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts. Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for evolocumab and any potential adverse effects on the breast-fed child from evolocumab or from the underlying maternal condition.[60127]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.