ThisiscontentfromElsevier'sDrugInformation
Famotidine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
10 to 20 mg PO twice daily as needed. Max: 40 mg/day.[51488] [51490]
10 to 20 mg PO twice daily as needed. Max: 40 mg/day.[51488] [51490]
20 mg PO twice daily for up to 6 weeks.[51477]
0.5 mg/kg/dose PO twice daily (Max: 40 mg PO twice daily).[44392] [55232] Treat for 6 to 12 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO twice daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO twice daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO once daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO once daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO once daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO once daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
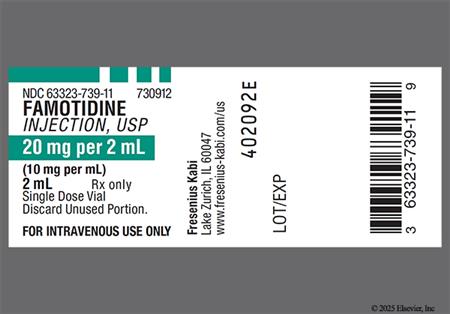
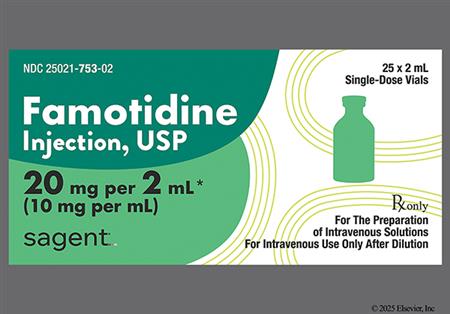
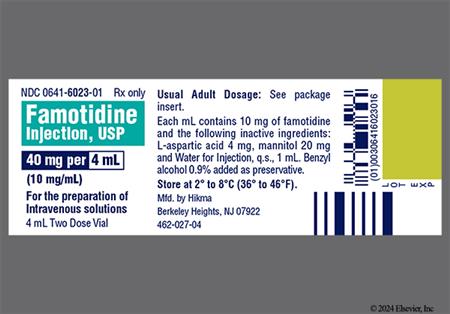
20 mg IV every 12 hours.[51456]
0.25 mg/kg/dose IV every 12 hours initially (Max: 40 mg/day); doses up to 0.5 mg/kg/dose IV every 12 hours have been used.[51456] A dose of 0.5 mg/kg/dose IV every 8 to 12 hours is supported by pharmacokinetic and pharmacodynamic data.[25030]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV twice daily have been used in 1 small study.[51494]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV once daily have been used in 1 small study.[51494]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV once daily have been used in 1 small study.[51494]
20 or 40 mg PO twice daily for up to 12 weeks.[51477]
0.5 mg/kg/dose PO twice daily (Max: 40 mg PO twice daily).[44392] [55232] Treat for 6 to 12 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO twice daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO twice daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO once daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO once daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
0.5 mg/kg/dose PO once daily initially, in addition to conservative measures such as thickened feedings. May increase the dose to 1 mg/kg/dose PO once daily if needed. Treat for up to 8 weeks.[51477] While famotidine may be effective in patients with less severe GERD, proton pump inhibitors (PPIs) offer more rapid symptom relief and better healing.[26115]
20 mg IV every 12 hours.[51456]
0.25 mg/kg/dose IV every 12 hours initially (Max: 40 mg/day); doses up to 0.5 mg/kg/dose IV every 12 hours have been used.[51456] A dose of 0.5 mg/kg/dose IV every 8 to 12 hours is supported by pharmacokinetic and pharmacodynamic data.[25030]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV twice daily have been used in 1 small study.[51494]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV once daily have been used in 1 small study.[51494]
Safety and efficacy have not been established; however, doses of 0.25 to 0.5 mg/kg/dose IV once daily have been used in 1 small study.[51494]
NOTE: For dosing in people with gastric or duodenal ulcers due to H. pylori, see H. pylori eradication indication.
40 mg PO once daily at bedtime. Most individuals with a duodenal ulcer heal within 4 weeks and full-dose therapy is rarely needed for longer than 6 to 8 weeks.
0.5 mg/kg/day PO at bedtime or 0.25 mg/kg/dose PO twice daily initially (Max: 40 mg/day). Doses up to 1 mg/kg/day (Max: 40 mg/day) PO have been used. Individualize treatment duration and dose based on clinical response and/or pH determination (gastric or esophageal) and endoscopy.[44392] In one small study, a treatment duration of 8 weeks was effective for the treatment of gastric or duodenal ulcer.[25029]
20 mg IV every 12 hours.[51456]
0.25 mg/kg/dose IV every 12 hours (Max: 40 mg/day). Titrate to a maximum dosage of 0.5 mg/kg every 12 hours (Max: 40 mg/day) based on clinical response and/or gastric pH determination and endoscopy.[51456]
20 mg PO once daily at bedtime.
20 mg IV every 12 hours.[51456]
20 mg PO every 6 hours, initially. May titrate. Maximum: 160 mg PO every 6 hours per the manufacturer. Clinically, adjust to patient response. Doses as high as 200 mg PO every 6 hours have been reported.[44392]
20 mg IV every 12 hours; titrate the dosage to individual treatment needs.[51456]
40 mg PO twice daily. Data from clinical trials note that only higher doses of H2-blockers are effective at reducing risk for gastric ulceration from NSAIDs.[60443] [60444] In one trial, patients receiving a NSAID for either rheumatoid arthritis or osteoarthritis were given famotidine 20 mg PO twice daily, famotidine 40 mg PO twice daily, or placebo for 24 weeks. The cumulative incidence of gastric ulcer was significantly reduced by famotidine 40 mg but not the lower dose compared to placebo. The cumulative incidence of duodenal ulcer was significantly reduced by both famotidine doses relative to placebo.[24596]
20 mg PO every 12 hours.[67626]
20 mg IV every 12 hours.[26015] [67626]
1 to 2 mg/kg/day IV divided every 8 to 12 hours (Max: 40 mg/day).[51510] [51511] [51981]
10 mg IV bolus, followed by 1.7 mg/hour (40 mg/day) continuous IV infusion.[26015] [67626]
20 mg PO as a single dose given 3 hours prior to the time of surgery, before induction of anesthesia. Alternatively, 40 mg PO the night prior to elective surgery. According to guidelines of the American Society of Anesthesiologists, routine preoperative use is NOT recommended in patients who have no apparent increased risk for pulmonary aspiration.[60445] However, some guidelines recommend an H2-receptor antagonist (PO or IV) for all women presenting for cesarean delivery.[66408]
20 mg IV in the morning prior to surgery, before induction of anesthesia. According to guidelines of the American Society of Anesthesiologists, routine preoperative use is NOT recommended in patients who have no apparent increased risk for pulmonary aspiration.[60445] However, some guidelines recommend an H2-receptor antagonist (PO or IV) for all women presenting for cesarean delivery.[66408]
20 mg IV as a single dose.[69080]
0.25 mg/kg/dose (Max: 20 mg/dose) IV as a single dose.[69080]
20 mg PO as a single dose.[69080]
0.25 mg/kg/dose (Max: 20 mg/dose) PO as a single dose.[69080]
20 to 40 mg PO twice daily for at least 6 months.[69771] [69772]
20 to 40 mg IV twice daily for at least 6 months.[69771] [69772]
40 mg/day PO or IV for active duodenal or benign gastric ulcer; 20 mg/day PO for ulcer maintenance; 40 mg/day PO for GERD; 80 mg/day PO for esophagitis; doses may go as high as 640 mg/day or 800 mg/day (rare) PO or 80 mg/day IV for hypersecretory conditions such as Zollinger-Ellison; 40 mg/day PO for self-medication (OTC).
40 mg/day PO or IV for active duodenal or benign gastric ulcer healing; 20 mg/day PO for ulcer maintenance; 40 mg/day PO for GERD; 80 mg/day PO for esophagitis; doses may go as high as 640 mg/day or 800 mg/day (rare) PO or 80 mg/day IV for hypersecretory conditions such as Zollinger-Ellison; 40 mg/day PO for self-medication (OTC).
1 mg/kg/day PO (Max: 80 mg/day); 1 mg/kg/day IV (Max: 40 mg/day); however, doses up to 2 mg/kg/day IV have been used off-label.
1 mg/kg/day PO (Max: 80 mg/day); 1 mg/kg/day IV (Max: 40 mg/day); however, doses up to 2 mg/kg/day IV have been used off-label.
3 to 11 months: 2 mg/kg/day PO. Safety and efficacy of IV have not been established; however, doses up to 2 mg/kg/day IV have been used off-label.
1 to 2 months: 1 mg/kg/day PO. Safety and efficacy of IV have not been established; however, doses up to 2 mg/kg/day IV have been used off-label.
1 mg/kg/day PO. Safety and efficacy of IV have not been established; however, 0.5 mg/kg/day IV has been used off-label.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
General Recommendations
Pediatrics
The following has been recommended based on a dose of 0.5 to 1 mg/kg/DAY divided every 12 hours in pediatric patients with normal renal function:
GFR 30 to 50 mL/minute/1.73 m2: 0.5 mg/kg/dose every 24 hours.
GFR 10 to 29 mL/minute/1.73 m2: 0.25 mg/kg/dose every 24 hours.
GFR less than 10 mL/minute/1.73 m2: 0.125 mg/kg/dose every 24 hours.[32569]
Intravenous Dosage
Adults
CrCl less than 50 mL/minute: Decrease dose 50% or extend the dosing interval to 36 to 48 hours based on clinical response.[51456]
Pediatrics
The following guidance has been recommended based on a pharmacokinetic study of pediatric patients with stable chronic renal insufficiency (n = 18):
CrCl 50 mL/minute/1.73m2 or more: 0.5 mg/kg/dose (Max: 20 mg) IV every 12 to 24 hours.
CrCl 11 to 49 mL/minute/1.73m2: 0.5 mg/kg/dose (Max: 20 mg) IV every 36 to 48 hours.
CrCl 10 mL/minute/1.73m2 or less: 0.5 mg/kg/dose (Max: 20 mg) IV every 72 to 96 hours or 0.25 mg/kg/dose (Max: 10 mg) IV every 36 to 48 hours.[51466]
Oral Dosage
Adults and Pediatric patients weighing 40 kg or more (maximum recommended dosage)
Active duodenal or gastric ulcer:
CrCl 30 to 60 mL/minute: 20 mg PO once daily or 40 mg PO every other day.
CrCl less than 30 mL/minute: 10 mg PO once daily or 20 mg PO every other day.
Symptomatic nonerosive GERD:
CrCl 30 to 60 mL/minute: 20 mg PO once daily.
CrCl less than 30 mL/minute: 10 mg PO once daily or 20 mg PO every other day.
Erosive esophagitis diagnosed by endoscopy:
CrCl 30 to 60 mL/minute: 20 mg PO once daily, 40 mg PO once daily, or 40 mg PO every other day.
CrCl less than 30 mL/minute: 10 mg PO once daily, 20 mg PO once daily, or 20 mg PO every other day.
Risk reduction for duodenal ulcer recurrence:
CrCl 30 to 60 mL/minute: 10 mg PO once daily or 20 mg PO every other day.
CrCl less than 30 mL/minute: 10 mg PO every other day.
Pathological hypersecretory conditions: Avoid use.[44392][51477]
Intermittent hemodialysis
Adults
Dose after dialysis.[32569]
Pediatrics
0.125 mg/kg/dose every 24 hours.[32569]
Peritoneal dialysis
Adults
Administer 10% of normal dose.[32569]
Pediatrics
0.125 mg/kg/dose every 24 hours.[32569]
Continuous renal replacement therapy (CRRT)
Adults
Administer 10% to 50% of normal dose.[32569]
Pediatrics
0.5 mg/kg/dose every 24 hours.[32569]
† Off-label indication












































Famotidine is an oral and parenteral histamine type 2-receptor antagonist (H2RA) used in the treatment of gastrointestinal disorders such as peptic ulcer and gastroesophageal reflux disease (GERD). The actions and indications of famotidine differ little from the other H2RAs, except that famotidine is less likely than cimetidine to interact with other drugs.[44392] Nonprescription (OTC) products are available for the prophylaxis and treatment of heartburn and acid indigestion. Both proton pump inhibitors (PPIs) and H2RAs provide symptom control in non-erosive GERD. However, PPIs are preferred over H2RAs for the healing and maintenance treatment of erosive GERD (i.e., erosive esophagitis) due to superior healing rates. H2RAs may be selected when PPIs are not tolerated, are contraindicated, or are not available.[55326][68019][59478] H2RAs are often used for stress ulcer prophylaxis in critically ill patients; however, evidence for benefit is lacking, and use may increase the risk of adverse reactions such as pneumonia and Clostridioides difficile infection.[64985][65013] Reserve stress ulcer prophylaxis for patients with risk factors for clinically significant gastrointestinal bleeding (e.g., multiple organ dysfunction, prolonged mechanical ventilation, coagulopathy, persistent shock, concomitant corticosteroid therapy).[61770][64985] Famotidine was initially FDA approved in 1986.
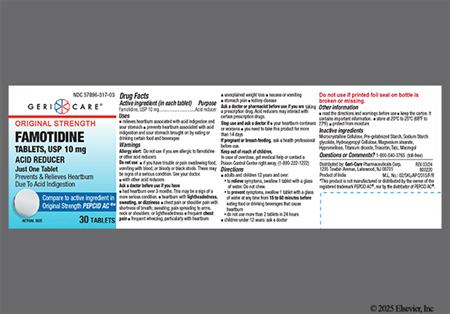
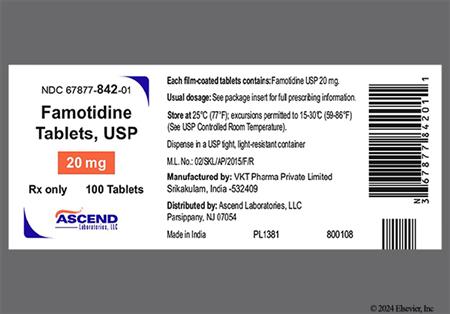
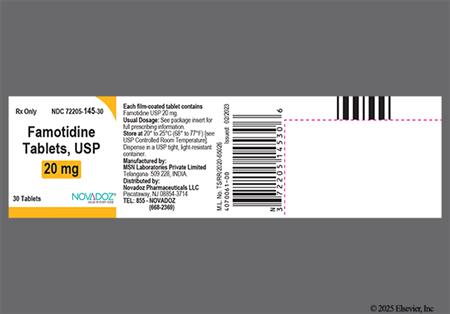
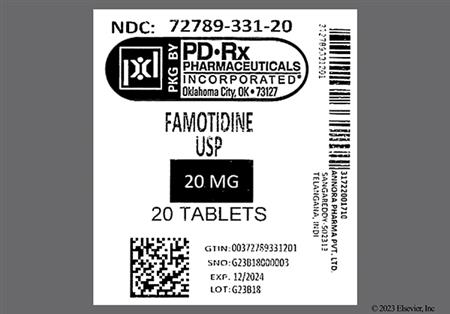
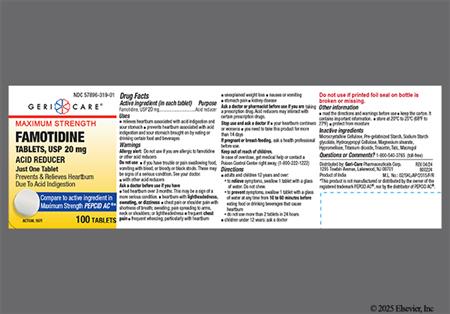
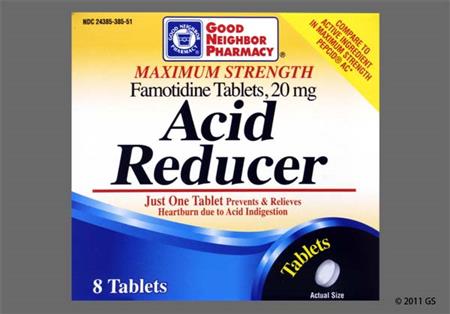
NOTE: Some famotidine 10 mg and 20 mg tablets are marketed as Zantac 360, which may create confusion since the brand name was previously associated with a ranitidine product.[66660]
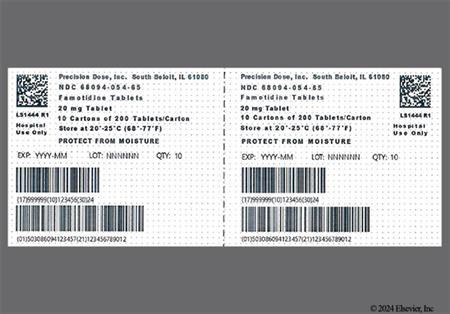
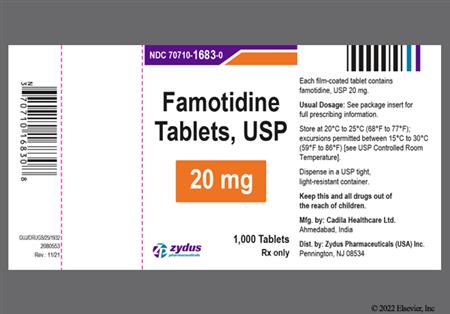
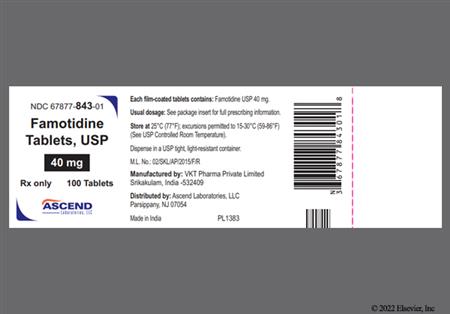
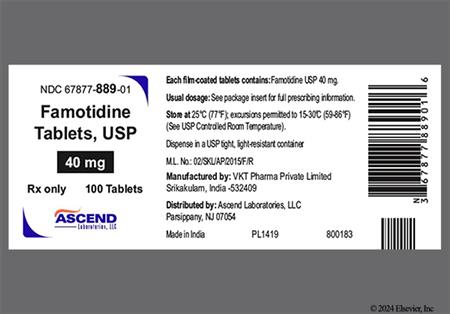
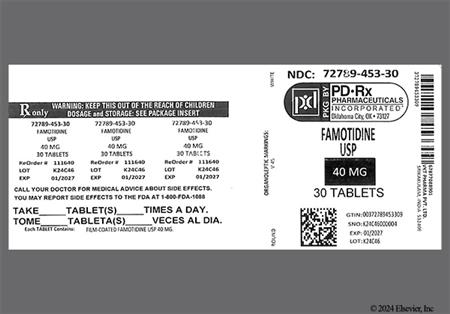
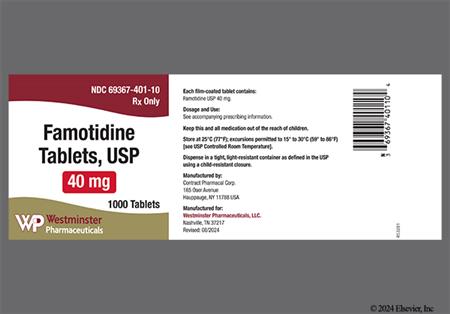
For storage information, see the specific product information within the How Supplied section.
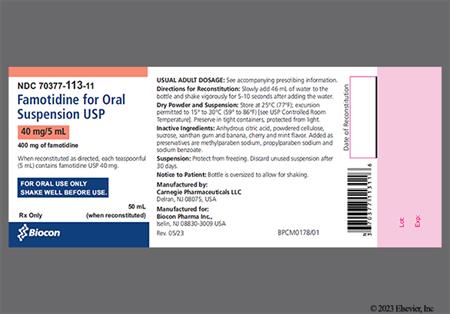
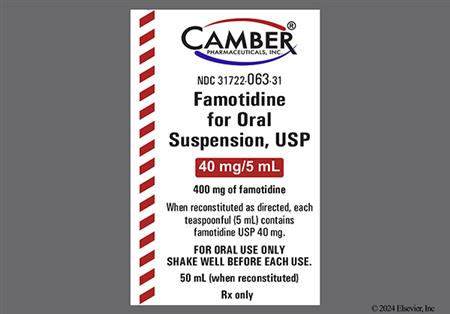
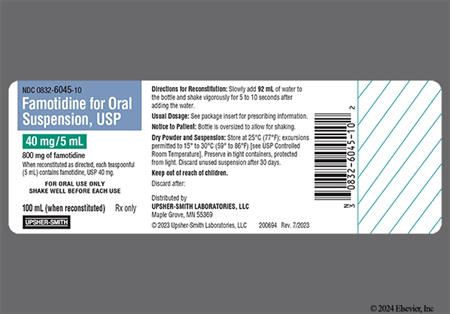
Oral suspension
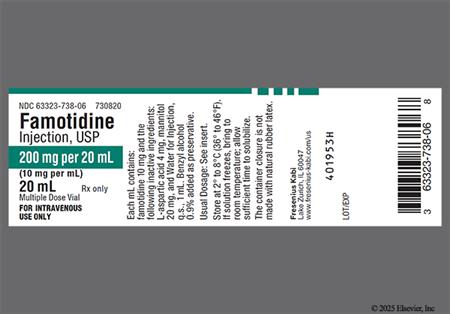
Intermittent IV Injection
Intermittent IV Infusion (vials)
Intermittent IV Infusion (Galaxy containers)
Continuous IV Infusion
Similar to other H2-antagonists, famotidine causes infrequent adverse reactions. In controlled clinical trials, the incidence of adverse reactions in people who received famotidine 40 mg at bedtime was similar to that in the placebo group. The following reactions have occurred in greater than 1% of people and may be causally related to the drug: headache (4.7%), dizziness (1.3%), constipation (1.2%), and diarrhea (1.7%). Other gastrointestinal adverse events reported in clinical trials or post approval include: cholestasis with jaundice, hepatitis, elevated hepatic enzymes, vomiting, nausea, abdominal discomfort, anorexia, dysgeusia (reported as taste disorder), and xerostomia. The relationship between these events and famotidine therapy has been unclear in many cases.[44392]
Reversible mental status changes, including agitation, confusion, delirium, hallucinations, hostility, paranoia, depression, insomnia, and disorientation have been reported rarely following famotidine therapy. Anxiety, libido decrease, paresthesias, and drowsiness have also been reported.[44392] A review of central nervous system reactions to H2-antagonists revealed that the incidence varies widely depending on the specific report, and that no single H2-antagonist is more likely to induce CNS reactions than another.[23494] Central nervous system reactions are more likely to occur in elderly patients and/or those with renal impairment. Seizures have been rarely reported in patients with renal impairment. Additionally, in a clinical study of famotidine in 35 infants < 1 year of age with GERD symptoms, agitation was reported in 5 patients that resolved when famotidine was discontinued.[44392]
Few cases of toxic epidermal necrolysis and Stevens-Johnson syndrome have been reported with famotidine therapy. Anaphylactoid reactions have also been reported. Additional hypersensitivity and dermatological reactions reported for famotidine in clinical trials or post approval include: orbital or facial edema, angioedema, urticaria, rash, conjunctival injection or ocular inflammation, alopecia, acne vulgaris, pruritus, xerosis, and flushing. The relationship between these events and famotidine therapy has been unclear in many cases.[44392]
Increasing evidence suggests a link between acid-suppression therapy and respiratory infection, specifically pneumonia (community- and hospital-acquired). Several mechanisms have been proposed to account for this association. One such mechanism states that gastric pH serves as a barrier against pathogenic colonization of the gastrointestinal tract. An increase in gastric pH allows for bacterial and viral invasion which, in theory, can precipitate respiratory infections.[32661] Another proposed mechanism accounts for the role that gastric acid may have on stimulating the cough reflex that allows for the clearing of infectious agents from the respiratory tract. Finally, the fact that acid-suppressive therapy may impair white blood cell function, which in turn may lead to a depressed immune response to an infection, is listed among possible mechanisms.[35601] Regardless of the mechanism, the use of H2-blockers [32661] and/or PPIs [35601] has been associated with the development of pneumonia. Data from a large epidemiological trial, including 364,683 individuals who developed 5551 first occurrences of community-acquired pneumonia (CAP), suggest an increased risk of developing CAP among users of acid-suppressive therapy compared to those who stopped therapy. After adjusting for confounders, the adjusted relative risk (RR) for CAP among PPI users compared to those who stopped therapy was 1.89 (95% CI, 1.36—2.62). Likewise, users of H2-blockers had an adjusted RR of 1.63 (95% CI, 1.07—2.48) compared to those who stopped therapy.[32661] In a second large cohort trial, including 63,878 hospital admissions, acid-suppressive therapy was ordered in 52% (83% PPI and 23% H2- blocker, with some patients exposed to both) of new admissions. Hospital-acquired pneumonia occurred in 2,219 admissions (3.5%) with a higher incidence recorded among acid-suppressive therapy exposed patients compared to non-exposed patients. A subset analysis found a statistically significant association between PPI use (OR, 1.3; 95% CI, 1.1—1.4) and pneumonia. A non-significant association was found with H2-blockers (OR, 1.2; 95% CI, 0.98—1.4); however, the lack of significance was attributed to the studies lack of power to detect significance for an OR of less than 1.3.[35601] Until more is known about the relationship between acid-suppression and pneumonia, clinicians are encouraged to carefully select patients before empirically initiating acid-suppressive therapy with H2-blockers or PPIs. A causal relationship between the use of famotidine and pneumonia has not been established.
Atrophic gastritis, a precursor for gastric cancer, has been associated with prolonged acid suppression with high dose H2-blockers like famotidine in patients who are H. pylori positive. A 'test and treat' approach for baseline H. pylori infections is recommended for patients with reflux esophagitis on long term acid suppression therapy. Treatment of baseline infection decreases inflammation and may reverse corpus gastritis.[33113]
Cardiovascular adverse events reported for famotidine in clinical trials or post approval include: arrhythmia exacerbation, AV block, and palpitations. The relationship between these events and famotidine therapy has been unclear in many cases. In addition, QT prolongation has been reported in patients with impaired renal function whose dose/dosing interval of famotidine may not have been adjusted appropriately.[44392]
Hematological adverse events have been reported for famotidine in clinical trials or post approval and include few cases of agranulocytosis, pancytopenia, leukopenia, and thrombocytopenia. The relationship between these events and famotidine therapy has been unclear in many cases.[44392]
Miscellaneous adverse events reported for famotidine in clinical trials or post-marketing include: fever, asthenia, fatigue, lethargy, rhabdomyolysis, musculoskeletal pain including muscle cramps, arthralgia, bronchospasm, interstitial pneumonia, and tinnitus. In addition, few cases of impotence (erectile dysfunction) and gynecomastia have been reported; however, in controlled clinical trials, the incidences were not greater than those seen with placebo. The relationship between these events and famotidine therapy has been unclear in many cases.[44392]
Long-term (e.g., generally > 3 years) treatment with acid-suppressing agents can lead to malabsorption of vitamin B12 (cyanocobalamin). One large case-controlled study compared patients with and without an incident diagnosis of vitamin B12 deficiency (n = 25,956 and 184,199, respectively). A correlation was demonstrated between vitamin B12 deficiency and gastric acid-suppression therapy. Patients receiving >= 2 years of a proton pump inhibitor (PPI)(OR, 1.65 [95% CI, 1.58—1.73]) or >= 2 years of a H2-receptor antagonist (OR, 1.25 [95% CI, 1.17—1.34]) were associated with having an increased risk for vitamin B12 deficiency. A dose-dependant relationship was evident, as daily doses > 1.5 PPI pills/day were more strongly associated with vitamin B12 deficiency (OR, 1.95 [95% CI, 1.77—2.15]) compared to daily doses < 0.75 pills/day (OR, 1.63 [95% CI, 1.48—1.78]; p = 0.007 for interaction).[56553] The possibility of cyanocobalamin deficiency and pernicious anemia should be considered if clinical symptoms are observed. Neurological manifestations of pernicious anemia can occur in the absence of hematologic changes.
Symptomatic response to therapy with famotidine does not preclude the presence of gastric cancer. Individuals who have a suboptimal response or early symptomatic relapse after completing therapy should consider evaluation for gastric malignancy.[50742] In the individual who is self-medicating with nonprescription (OTC) formulations, the continuation of heartburn, acid indigestion, or dyspepsia beyond 2 weeks signals the need to consult a health care provider for evaluation.[44392][51488]
Famotidine should be used cautiously in patients with renal impairment or renal failure as there is a close relationship between the drug's elimination half-life and creatinine clearance. Dosages of famotidine should be adjusted in patients with moderate or severe renal impairment. Central nervous system (CNS) adverse reactions, including confusion, delirium, hallucinations, disorientation, agitation, seizures, and lethargy, have been reported in older adults and patients with moderate and severe renal impairment treated with famotidine; in some cases, the dosages were not adjusted as recommended for renal impairment.[50742]
Animal studies and epidemiologic data during pregnancy suggest famotidine use when necessary is not harmful, even though there are no adequate and well-controlled studies evaluating famotidine use in pregnant patients.[20917] [50742] [51456] [51477] In one such study of human data, exposure to H2-blockers, including famotidine, was not associated with an increased risk for congenital malformations (adjusted OR 1.03, 95% CI: 0.80, 1.32); also, no such association was found when therapeutic pregnancy terminations were included in the analysis (adjusted OR 1.17, 95% CI: 0.93, 1.46). Exposure to H2-blockers was not associated with perinatal mortality, premature delivery, low birth weight, or low Apgar scores.[68907] In animal reproduction studies, no adverse development effects were observed with oral famotidine at doses up to approximately 243 and 122 times, respectively, the recommended human dose of 80 mg/day for the treatment of erosive esophagitis.[50742] [51477] Guidelines recommend a trial of lifestyle modifications as first-line therapy for heartburn and gastroesophageal reflux disease (GERD) during pregnancy, followed by antacids if lifestyle adjustments are ineffective. For ongoing symptoms, H2-blockers such as famotidine can be used. Other medications should be reserved for pregnant patients who fail H2-blocker therapy.[68890] Self-medication with H2-blockers (OTC formulations) during pregnancy is not recommended. Pregnant patients should see their health care professional for a proper diagnosis and for treatment recommendations.[45899] Famotidine has been used in limited circumstances at term to prevent acid aspiration during labor; some guidelines recommend an H2-blocker (PO or IV) for all women presenting for cesarean delivery.[66408]
Famotidine is compatible with breast-feeding. Famotidine passes into human milk in minimal amounts with a relative infant dose of 1.9%. This small amount of infant famotidine exposure through breast milk is unlikely to be harmful.[70364] [70365] If heartburn or gastroesophageal reflux disease symptoms persist after delivery, antacids and sucralfate are also safe to use due to minimal breast milk passage. According to guidelines, if heartburn/gastroesophageal reflux (GERD) symptoms persist after delivery, antacids and sucralfate are safe to use during lactation because they are not concentrated in breast milk. H2-blockers are excreted in breast milk, but cimetidine and famotidine are considered safe for use during lactation and may be used if symptoms persist despite antacid use.[45899] [68890]
No special precautions have been advised for famotidine use in geriatric adults vs. younger adults, but dosage adjustments are necessary in older adults with reduced renal function. If critically ill, the older adults in some uncontrolled studies have appeared to be more likely to exhibit central nervous system (CNS) reactions to the H2-antagonists.[50742] According to the Beers Criteria, H2-receptor antagonists are considered potentially inappropriate medications (PIMs) in geriatric patients with delirium/high risk of delirium (potential for new-onset or worsening delirium) and should be avoided in this patient population. Dosage reduction of H2-receptor antagonists is recommended in geriatric adults with a creatinine clearance less than 50 mL/minute due to the potential for mental status changes.[63923]
Famotidine injection multidose vials contain benzyl alcohol as a preservative and should be avoided in neonates. There have been reports of fatal 'gasping syndrome' in neonates (less than 1 month of age) after the administration of parenteral solutions containing the preservative benzyl alcohol at dosages more than 99 mg/kg/day. The minimum amount of benzyl alcohol to cause toxicity is unknown. Therefore, use preservative-free famotidine injectable formulations in neonates.[51456]
Famotidine competitively inhibits the binding of histamine to H2-receptors on the gastric basolateral membrane of parietal cells, reducing basal and nocturnal gastric acid secretions. The drug also decreases the gastric acid response to stimuli such as food, caffeine, insulin, betazole, or pentagastrin. Famotidine reduces the total volume of gastric juice, thus indirectly decreasing pepsin secretion. The drug does not appear to alter gastric motility, gastric emptying, esophageal pressures, biliary secretions, or pancreatic secretions. Famotidine may aid in gastromucosal healing, and it may protect the mucosa from the irritant effects caused by aspirin and nonsteroidal antiinflammatory agents.
Revision Date: 10/15/2025, 01:33:00 AMFamotidine is administered orally and parenterally. Plasma protein binding is approximately 15% to 20%. There is no cumulative effect with repeat doses; plasma concentrations after multiple doses are similar to those after single doses. Famotidine undergoes minimal first-pass metabolism. The majority (65 to 70%) of a famotidine dose is excreted in the urine; 30 to 35% of the dose is metabolized by the liver. The S-oxide metabolite is the only 1 identified in humans. Famotidine elimination half-life is 2.5 to 3.5 hours in adults with normal renal function.[44392][51477]
Affected cytochrome P450 isoenzymes and drug transporters: OAT1, OAT3
I In vitro studies indicate that famotidine is a substrate for OAT1 and OAT3. Following coadministration of probenecid (1,500 mg), an inhibitor of OAT1 and OAT3, with a single dose of famotidine 20 mg PO in 8 healthy subjects, the serum AUC0-10h of famotidine increased from 424 to 768 ng x hour/mL and the maximum serum concentration (Cmax) increased from 73 to 113 ng/mL. Renal clearance, urinary excretion rate and amount of famotidine excreted unchanged in urine were decreased. The clinical relevance of this interaction is unknown.[56579] Famotidine is considered a weak CYP1A2 inhibitor, but drug interactions due to this activity have not been studied clinically. Although not studied clinically, famotidine may lead to substantial increases in blood concentrations of tizanidine, a CYP1A2 substrate. No data have confirmed or refuted a potential interaction.[50742] Other formal studies in man, animal models and in vitro have signaled no significant interference with the disposition of compounds metabolized by the cytochrome P450 hepatic microsomal isoenzyme system. Compounds tested in man include warfarin, theophylline, phenytoin, diazepam, aminopyrine and antipyrine. Indocyanine green as an index of hepatic drug extraction has been tested, and no significant effects have been found.[51456] An in vitro study showed that famotidine is an inhibitor of MATE-1. However, no clinically significant interaction with metformin, a substrate for MATE-1, was observed.[50742]
Bioavailability of famotidine is approximately 40% to 45% in adults. Famotidine tablets and oral suspension are bioequivalent. Food may slightly increase and antacids may slightly decrease the bioavailability of famotidine; however, the effects are considered clinically insignificant. The onset of action is usually within 1 hour after oral administration with maximum effects occurring within 1 to 3 hours depending on the dose. The duration of action is roughly 10 to 12 hours. Twenty-five to 30% of an oral dose is excreted in urine as unchanged drug.[44392][51477]
Sixty-five to 70% of an intravenous dose of famotidine is excreted in urine as unchanged drug.[51456]
In adult patients with severe renal impairment (creatinine clearance less than 30 mL/minute), the systemic exposure (AUC) of famotidine increased at least 5-fold. In adult patients with moderate renal impairment (creatinine clearance between 30 to 60 mL/minute), the AUC of famotidine increased at least 2-fold.[44392][51477]
Children and Adolescents
The mean oral bioavailability in 8 pediatric patients 11 to 15 years of age was 50%. The mean half-life was 2 to 3.4 hours in pediatric patients 1 to 15 years of age.[44392] [51456] [51477]
Neonates and Infants
After a single administration of 0.5 mg/kg orally in patients from birth to 12 months of age, the bioavailability was approximately 42%. The AUC increased 1.4-fold after a single oral dose of 1 mg/kg compared to 0.5 mg/kg and 2.7-fold after multiple oral doses of 1 mg/kg compared to 0.5 mg/kg. The half-life was 5.82 in infants birth to 12 months of age. Plasma clearance was reduced, and elimination half-life was prolonged in pediatric patients from birth to 3 months of age compared to older pediatric patients. After intravenous administration of 0.5 mg/kg, total clearance was 0.13 +/- 0.06 L/hour/kg, 0.21 +/- 0.06 L/hour/kg, and 0.49 +/- 0.17 L/hour/kg in pediatric patients younger than 1 month of age, younger than 3 months of age, and 4 to 12 months of age, respectively. Elimination half-life was 10.5 hours, 8.1 hours, and 4.5 hours in pediatric patients younger than 1 month of age, younger than 3 months of age, and 4 to 12 months of age, respectively. The duration of acid suppression was longer in pediatric patients from birth to 3 months of age compared to older pediatric patients.[44392] [51456] [51477]
There are no clinically significant age-related changes in famotidine pharmacokinetics in elderly patients versus younger adults. However, in elderly patients with decreased renal function, the clearance of famotidine may be reduced.[44392][51477]
Animal studies and epidemiologic data during pregnancy suggest famotidine use when necessary is not harmful, even though there are no adequate and well-controlled studies evaluating famotidine use in pregnant patients.[20917] [50742] [51456] [51477] In one such study of human data, exposure to H2-blockers, including famotidine, was not associated with an increased risk for congenital malformations (adjusted OR 1.03, 95% CI: 0.80, 1.32); also, no such association was found when therapeutic pregnancy terminations were included in the analysis (adjusted OR 1.17, 95% CI: 0.93, 1.46). Exposure to H2-blockers was not associated with perinatal mortality, premature delivery, low birth weight, or low Apgar scores.[68907] In animal reproduction studies, no adverse development effects were observed with oral famotidine at doses up to approximately 243 and 122 times, respectively, the recommended human dose of 80 mg/day for the treatment of erosive esophagitis.[50742] [51477] Guidelines recommend a trial of lifestyle modifications as first-line therapy for heartburn and gastroesophageal reflux disease (GERD) during pregnancy, followed by antacids if lifestyle adjustments are ineffective. For ongoing symptoms, H2-blockers such as famotidine can be used. Other medications should be reserved for pregnant patients who fail H2-blocker therapy.[68890] Self-medication with H2-blockers (OTC formulations) during pregnancy is not recommended. Pregnant patients should see their health care professional for a proper diagnosis and for treatment recommendations.[45899] Famotidine has been used in limited circumstances at term to prevent acid aspiration during labor; some guidelines recommend an H2-blocker (PO or IV) for all women presenting for cesarean delivery.[66408]
Famotidine is compatible with breast-feeding. Famotidine passes into human milk in minimal amounts with a relative infant dose of 1.9%. This small amount of infant famotidine exposure through breast milk is unlikely to be harmful.[70364] [70365] If heartburn or gastroesophageal reflux disease symptoms persist after delivery, antacids and sucralfate are also safe to use due to minimal breast milk passage. According to guidelines, if heartburn/gastroesophageal reflux (GERD) symptoms persist after delivery, antacids and sucralfate are safe to use during lactation because they are not concentrated in breast milk. H2-blockers are excreted in breast milk, but cimetidine and famotidine are considered safe for use during lactation and may be used if symptoms persist despite antacid use.[45899] [68890]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.