ThisiscontentfromElsevier'sDrugInformation
Fluconazole
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
NOTE: For CNS infections caused by Cryptococcus, see Cryptococcus meningitis.
400 to 800 mg PO once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[28674] [60487]
12 mg/kg/dose PO once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[28674] [60487]
9 mg/kg/dose PO once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[28674] [60487]
400 to 800 mg IV once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[60487] [60686]
12 mg/kg/dose IV once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[60487] [60686]
9 mg/kg/dose IV once daily until resolution of all signs and symptoms and CSF and radiologic abnormalities.[60487] [60686]
800 to 1,200 mg PO once daily. Guidelines recommend fluconazole as the preferred therapy. Continue suppressive therapy for lifelong.[34362] [61514]
800 to 1,200 mg PO once daily. Guidelines recommend fluconazole as the preferred therapy. Continue suppressive therapy for lifelong.[34362] [61514]
12 mg/kg/dose (Max: 800 mg/dose) PO once daily.[34361] Guidelines recommend fluconazole as preferred therapy.[61514] For persons living with HIV, fluconazole is recommended for 8 weeks after an initial 2-week course of amphotericin B deoxycholate or liposomal amphotericin B plus flucytosine. If amphotericin B is not tolerated, fluconazole may be given as initial therapy plus flucytosine. If flucytosine is not tolerated, fluconazole may be given as initial therapy plus amphotericin B.[34361] Continue suppressive therapy for lifelong.[34361] [61514]
12 mg/kg/dose (Max: 800 mg/dose) IV once daily.[34361] Guidelines recommend fluconazole as preferred therapy.[61514] For persons living with HIV, fluconazole is recommended for 8 weeks after an initial 2-week course of amphotericin B deoxycholate or liposomal amphotericin B plus flucytosine. If amphotericin B is not tolerated, fluconazole may be given as initial therapy plus flucytosine. If flucytosine is not tolerated, fluconazole may be given as initial therapy plus amphotericin B.[34361] Continue suppressive therapy for lifelong.[34361] [61514]
800 mg PO once daily for at least 12 months and until resolution of abnormal CSF findings in persons who are intolerant to both itraconazole and voriconazole.[34362]
800 mg PO once daily for at least 12 months and until resolution of abnormal CSF findings in persons who are intolerant to both itraconazole and voriconazole.[34362]
800 mg PO once daily for at least 12 months and until resolution of CSF abnormalities.[34215]
NOTE: For CNS infections, see dosage for meningitis.
800 mg PO loading dose on day 1, followed by 400 mg PO once daily as an alternative in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487] The FDA-approved dosage is 400 mg PO once daily.[28674] Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily as an alternative in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily.[28674] Guidelines recommend fluconazole as an alternative only in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[28674] [60487]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily as an alternative in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487] The FDA-approved dosage is 400 mg IV once daily.[60686] Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily as an alternative in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487] [60686]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily.[60686] Guidelines recommend fluconazole as an alternative only in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy in patients who have not been receiving fluconazole prophylaxis. Treat for 2 weeks after documented clearance from the bloodstream and resolution of signs and symptoms for invasive candidiasis without metastatic complications.[60487] [60686]
400 mg PO once daily after initial treatment with lipid amphotericin B or an echinocandin for patients who are unlikely to have a fluconazole-resistant isolate. Treat until lesions resolve on repeat imaging, which is usually several months.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily after initial treatment with lipid amphotericin B or an echinocandin for patients who are unlikely to have a fluconazole-resistant isolate. Treat until lesions resolve on repeat imaging, which is usually several months.[28674] [60487]
400 mg IV once daily after initial treatment with lipid amphotericin B or an echinocandin for patients who are unlikely to have a fluconazole-resistant isolate. Treat until lesions resolve on repeat imaging, which is usually several months.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily after initial treatment with lipid amphotericin B or an echinocandin for patients who are unlikely to have a fluconazole-resistant isolate. Treat until lesions resolve on repeat imaging, which is usually several months.[60487] [60686]
800 mg PO loading dose on day 1, followed by 400 to 800 mg PO once daily for fluconazole-susceptible isolates. Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for fluconazole-susceptible isolates. Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for fluconazole-susceptible isolates. Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
800 mg IV loading dose on day 1, followed by 400 to 800 mg IV once daily for fluconazole-susceptible isolates. Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for fluconazole-susceptible isolates.[60487] [60686] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for fluconazole-susceptible isolates.[60487] [60686] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] Treat for at least 4 to 6 weeks with final duration depending on resolution of lesions.[60487]
100 to 200 mg PO once daily for 7 to 14 days for moderate to severe disease.[60487] The FDA-approved dosage is 200 mg PO loading dose on Day 1, then 100 mg PO once daily for at least 14 days to decrease the likelihood of relapse.[28674]
6 mg/kg/dose (Max: 200 mg/dose) PO loading dose on Day 1, then 3 to 6 mg/kg/dose (Max: 100 mg/dose) PO once daily for 7 to 14 days.[28674] [60487] [70821] A course of at least 14 days may decrease the likelihood of relapse.[28674] [70821]
6 mg/kg/dose PO loading dose on Day 1, then 3 to 6 mg/kg/dose PO once daily for 7 to 14 days.[60487] [70821] A course of at least 14 days may decrease the likelihood of relapse.[28674] [70821]
6 mg/kg/dose PO loading dose on Day 1, then 3 to 6 mg/kg/dose PO once daily for 7 to 14 days.[60487] [70821] A course of at least 14 days may decrease the likelihood of relapse.[28674] [70821]
100 to 200 mg IV once daily for 7 to 14 days for moderate to severe disease.[60487] The FDA-approved dosage is 200 mg IV loading dose on Day 1, then 100 mg IV once daily for at least 14 days to decrease the likelihood of relapse.[60686]
6 mg/kg/dose (Max: 200 mg/dose) IV loading dose on Day 1, then 3 to 6 mg/kg/dose (Max: 100 mg/dose) IV once daily for 7 to 14 days.[60487] [60686] [70821] A course of at least 14 days may decrease the likelihood of relapse.[60686] [70821]
6 mg/kg/dose IV loading dose on Day 1, then 3 to 6 mg/kg/dose IV once daily for 7 to 14 days.[60487] [70821] A course of at least 14 days may decrease the likelihood of relapse.[60686] [70821]
6 mg/kg/dose IV loading dose on Day 1, then 3 to 6 mg/kg/dose IV once daily for 7 to 14 days.[60487] [70821] A course of at least 14 days may decrease the likelihood of relapse.[60686] [70821]
200 mg PO loading dose on Day 1, then 100 to 200 mg PO once daily for 7 to 14 days.[34362] [60487] A course of at least 14 days may decrease the likelihood of relapse.[28674]
200 mg PO loading dose on Day 1, then 100 to 200 mg PO once daily for 7 to 14 days.[34362] [60487] A course of at least 14 days may decrease the likelihood of relapse.[28674]
6 to 12 mg/kg/dose (Max: 200 mg/dose) PO once daily for 7 to 14 days.[34361] [70821] A course of at least 14 days may decrease the likelihood of relapse.[28674]
6 to 12 mg/kg/dose PO once daily for 7 to 14 days.[34361] [70821] A course of at least 14 days may decrease the likelihood of relapse.[28674]
200 mg IV loading dose on Day 1, then 100 mg IV once daily for at least 14 days to decrease the likelihood of relapse.[60686]
200 mg IV loading dose on Day 1, then 100 mg IV once daily for at least 14 days to decrease the likelihood of relapse.[60686]
6 to 12 mg/kg/dose (Max: 200 mg/dose) IV once daily for 7 to 14 days.[34361] [70821] A course of at least 14 days may decrease the likelihood of relapse.[60686]
6 to 12 mg/kg/dose IV once daily for 7 to 14 days.[34361] [70821] A course of at least 14 days may decrease the likelihood of relapse.[60686]
200 to 400 mg PO once daily for 14 to 21 days.[60487] The FDA-approved dosage is 200 mg PO once, then 100 mg PO once daily for a minimum of 3 weeks and for 2 weeks after resolution of symptoms.[28674]
6 mg/kg/dose (Max: 400 mg/dose) PO loading dose on day 1, followed by 3 to 6 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 to 21 days.[60487] [70821] The FDA-approved dosage is 6 mg/kg/dose PO once, then 3 mg/kg/dose PO once daily for a minimum of 3 weeks and for 2 weeks after resolution of symptoms.[28674] Doses up to 12 mg/kg/day (Max: 400 mg/day) PO may be used if clinical condition warrants more aggressive dosing.[28674] [70821]
6 mg/kg/dose PO loading dose on day 1, followed by 3 to 6 mg/kg/dose PO once daily for 14 to 21 days.[60487] [70821] Doses up to 12 mg/kg/day PO may be used if clinical condition warrants more aggressive dosing.[70821]
6 mg/kg/dose PO loading dose on day 1, followed by 3 to 6 mg/kg/dose PO once daily for 14 to 21 days. Doses up to 12 mg/kg/day PO may be used if clinical condition warrants more aggressive dosing.[28674] [60487] [70821]
200 to 400 mg IV once daily for 14 to 21 days.[60487] The FDA-approved dosage is 200 mg IV once, then 100 mg IV once daily for a minimum of 3 weeks and for 2 weeks after resolution of symptoms.[60686]
6 mg/kg/dose (Max: 400 mg/dose) IV loading dose on day 1, followed by 3 to 6 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 to 21 days.[60487] [70821] The FDA-approved dosage is 6 mg/kg/dose IV once, then 3 mg/kg/dose IV once daily for a minimum of 3 weeks and for 2 weeks after resolution of symptoms.[60686] Doses up to 12 mg/kg/day (Max: 400 mg/day) IV may be used if clinical condition warrants more aggressive dosing.[60686] [70821]
6 mg/kg/dose IV loading dose on day 1, followed by 3 to 6 mg/kg/dose IV once daily for 14 to 21 days.[60487] [70821] Doses up to 12 mg/kg/day IV may be used if clinical condition warrants more aggressive dosing.[70821]
6 mg/kg/dose IV loading dose on day 1, followed by 3 to 6 mg/kg/dose IV once daily for 14 to 21 days. Doses up to 12 mg/kg/day IV may be used if clinical condition warrants more aggressive dosing.[60487] [70821]
200 mg PO loading dose on day 1, followed by 100 to 400 mg PO once daily for 14 to 21 days.[28674] [34362] [60487]
200 mg PO loading dose on day 1, followed by 100 to 400 mg PO once daily for 14 to 21 days.[28674] [34362] [60487]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 to 21 days.[34361] [60487]
6 to 12 mg/kg/dose PO once daily for 14 to 21 days.[34361] [60487]
200 mg IV loading dose on day 1, followed by 100 to 400 mg IV once daily for 14 to 21 days.[34362] [60487] [60686]
200 mg IV loading dose on day 1, followed by 100 to 400 mg IV once daily for 14 to 21 days.[34362] [60487] [60686]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 to 21 days.[34361] [60487]
6 to 12 mg/kg/dose IV once daily for 14 to 21 days.[34361] [60487]
400 to 800 mg PO once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [70594]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60294] [60487] [70594]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60294] [60487] [70594]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60294] [60487] [70594]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60294] [60487] [70594]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60294] [60487] [70594]
400 to 800 mg IV once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [70594]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [60686] [70594]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [60686] [70594]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [60686] [70594]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [60686] [70594]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat for at least 6 weeks after valve replacement. When native valve replacement is not possible or for prosthetic valve endocarditis, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60294] [60487] [60686] [70594]
400 to 800 mg PO once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[28674] [60487]
400 to 800 mg IV once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily as step-down therapy after lipid amphotericin B or echinocandin therapy in stable patients with negative blood cultures. Total treatment duration is at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Treat at least 4 to 6 weeks after hardware removal. When hardware removal is not possible, chronic suppressive therapy with fluconazole is recommended after initial treatment.[60487] [60686]
400 to 800 mg PO once daily for at least 2 weeks after candidemia (if present) has cleared.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily for at least 2 weeks after candidemia (if present) has cleared.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for at least 2 weeks after candidemia (if present) has cleared.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for at least 2 weeks after candidemia (if present) has cleared.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for at least 2 weeks after candidemia (if present) has cleared.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for at least 2 weeks after candidemia (if present) has cleared.[28674] [60487]
400 to 800 mg IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for at least 2 weeks after candidemia (if present) has cleared.[60487] [60686]
400 to 800 mg PO once daily.[60294] [60487] [70594]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily.[28674] [60294] [60487] [70594]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily.[28674] [60294] [60487] [70594]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily.[28674] [60294] [60487] [70594]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily.[28674] [60294] [60487] [70594]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily.[28674] [60294] [60487] [70594]
NOTE: Growth of Candida sp. from the respiratory tract typically reflects colonization and rarely requires antifungal therapy. In cases where pneumonia is associated with disseminated infection, treatment is recommended.[60487]
800 mg PO loading dose on day 1, followed by 400 mg PO once daily as an alternative to echinocandin therapy in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487] The FDA-approved dosage is 400 mg PO once daily.[28674]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily as an alternative to echinocandin therapy in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily.[28674] Guidelines recommend fluconazole as an alternative to echinocandin therapy only in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily as an alternative to echinocandin therapy in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487] The FDA-approved dosage is 400 mg IV once daily.[60686]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily as an alternative to echinocandin therapy in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487] [60686]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily.[60686] Guidelines recommend fluconazole as an alternative to echinocandin therapy only in patients who are not critically ill and are unlikely to have a fluconazole-resistant isolate, specifically no prior azole exposure for neutropenic patients.[60487]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
800 mg PO loading dose on day 1, followed by 400 mg PO once daily.[49816] [60487] [66423] The FDA-approved dosage is 50 to 200 mg PO once daily.[28674]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily.[28674] [49816] [60487] [66423]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily.[28674] [49816] [60487] [66423]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] [66423]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] [66423]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] [66423]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487] [66423]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily.[49816] [60487] [66423] The FDA-approved dosage is 50 to 200 mg IV once daily.[60686]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily.[49816] [60487] [60686] [66423]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily.[49816] [60487] [60686] [66423]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686] [66423]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686] [66423]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686] [66423]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686] [66423]
200 mg PO loading dose on day 1, followed by 50 to 100 mg PO once daily for at least 14 days after catheter removal.[61676]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO every 24 to 48 hours for at least 14 days after catheter removal.[53190]
200 mg IV loading dose on day 1, followed by 50 to 100 mg IV once daily for at least 14 days after catheter removal.[61676]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV every 24 to 48 hours for at least 14 days after catheter removal.[53190]
200 mg intraperitoneally every 24 to 48 hours.[61676]
6 to 12 mg/kg/dose (Max: 400 mg/dose) intraperitoneally every 24 to 48 hours.[53190]
200 mg PO loading dose on day 1, followed by 50 to 100 mg PO once daily for at least 14 to 21 days.[66490]
6 mg/kg/dose (Max: 400 mg/dose) PO every 24 to 48 hours for at least 14 to 28 days.[53190]
400 mg PO once daily for 6 to 12 months.[60487]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 to 12 months.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 to 12 months.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
400 mg IV once daily for 6 to 12 months.[60487]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 6 to 12 months.[60487] [60686]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 6 to 12 months.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 6 to 12 months as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
400 mg PO once daily for 6 weeks.[60487]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 weeks.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 weeks.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
400 mg IV once daily for 6 weeks.[60487]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 6 weeks.[60487] [60686]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 6 weeks.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 6 weeks as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
50 to 200 mg PO once daily is the general dosage recommended in the FDA-approved labeling for urinary tract infections.[28674]
50 to 200 mg IV once daily is the general dosage recommended in the FDA-approved labeling for urinary tract infections.[60686]
800 mg PO loading dose on day 1, followed by 400 mg PO once daily for 14 days as an alternative to echinocandin therapy in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
25 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 days as an alternative to echinocandin therapy in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
35 mg/kg (Max: 800 mg/dose) PO loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 days.[28674] Guidelines recommend fluconazole as an alternative to echinocandin therapy only in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily for 14 days is recommended by guidelines as an alternative to echinocandin therapy in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
25 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 days as an alternative to echinocandin therapy in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
35 mg/kg (Max: 800 mg/dose) IV loading dose on day 1, followed by 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 days.[60686] Guidelines recommend fluconazole as an alternative to echinocandin therapy only in patients who are not critically ill and have had no prior azole exposure. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
400 mg PO once daily to complete a 14-day course as stepdown therapy after initial echinocandin or amphotericin B therapy. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily to complete a 14-day course as stepdown therapy after initial echinocandin or amphotericin B therapy. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
400 mg IV once daily to complete a 14-day course as stepdown therapy after initial echinocandin or amphotericin B therapy. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily to complete a 14-day course as stepdown therapy after initial echinocandin or amphotericin B therapy. Candiduria may be the only microbiological documentation of disseminated candidiasis in neutropenic patients; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[28674] [60487]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis. Candiduria may be the only microbiological documentation of disseminated candidiasis in very-low-birth-weight infants; therefore, candiduria should be treated as disseminated candidiasis in these patients.[60487] [60686]
400 mg PO once daily for several days before and after the urologic procedure.[60487]
12 mg/kg/dose (Max: 400 mg/dose) PO once daily for several days before and after the urologic procedure.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
400 mg IV once daily for several days before and after the urologic procedure.[60487]
12 mg/kg/dose (Max: 400 mg/dose) IV once daily for several days before and after the urologic procedure.[60686] [60487]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for several days before and after the urologic procedure as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
200 mg PO once daily for 14 days.[60487]
6 mg/kg/dose (Max: 200 mg/dose) PO once daily for 14 days.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
200 mg IV once daily for 14 days.[60487]
6 mg/kg/dose (Max: 200 mg/dose) IV once daily for 14 days.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
200 to 400 mg PO once daily for 14 days.[60487]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 days.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
200 to 400 mg IV once daily for 14 days.[60487]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 days.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
200 to 400 mg PO once daily for 14 days in addition to surgical removal.[60487]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 14 days in addition to surgical removal.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 12 mg/kg/dose PO once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
25 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
35 mg/kg PO loading dose on day 1, followed by 9 mg/kg/dose PO once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[28674] [60487]
200 to 400 mg IV once daily for 14 days in addition to surgical removal.[60487]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV once daily for 14 days in addition to surgical removal.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 12 mg/kg/dose IV once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
25 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
35 mg/kg IV loading dose on day 1, followed by 9 mg/kg/dose IV once daily for 14 days in addition to surgical removal as an alternative therapy to conventional amphotericin B in patients who have not been receiving fluconazole prophylaxis.[60487] [60686]
400 mg PO once daily during the period of expected neutropenia. Prophylaxis is recommended for individuals who are at high risk of febrile neutropenia or infection, including individuals who are expected to have profound, protracted neutropenia, defined as absolute neutrophil count (ANC) less than 100 cells/mm3 for more than 7 days or other risk factors (e.g., most individuals with acute myeloid leukemia/myelodysplastic syndromes (AML/MDS) or hematopoietic stem-cell transplantation (HSCT) treated with myeloablative conditioning regimens). Prophylaxis is not routinely recommended for individuals with solid tumors.[28674] [49827] [51812] [56105] [64861]
3 to 6 mg/kg/dose (Max: 400 mg/dose) PO once daily during the period of expected neutropenia.[51812] [53050] [53051] [53053] Higher doses (8 mg/kg/day; Max: 400 mg/day) have been reported in pediatric hematopoietic stem-cell transplantation (HSCT) recipients.[31231] For individuals receiving chemotherapy, initiate prophylaxis with induction chemotherapy and continue for the duration of neutropenia. Guidelines for preventing opportunistic infections in HSCT recipients recommend initiating antifungal prophylaxis at the start of conditioning and continuing until engraftment or 7 days after the absolute neutrophil count (ANC) is more than 1,000 cells/mm3.[51812]
3 to 6 mg/kg/dose (Max: 600 mg/dose) PO once daily during the period of expected neutropenia.[51812] [53050] [53051] [53053] Higher doses (8 mg/kg/day; Max: 400 mg/day) have been reported in pediatric hematopoietic stem-cell transplantation (HSCT) recipients.[31231] For individuals receiving chemotherapy, initiate prophylaxis with induction chemotherapy and continue for the duration of neutropenia. Guidelines for preventing opportunistic infections in HSCT recipients recommend initiating antifungal prophylaxis at the start of conditioning and continuing until engraftment or 7 days after the absolute neutrophil count (ANC) is more than 1,000 cells/mm3.[51812]
400 mg IV once daily during the period of expected neutropenia. Prophylaxis is recommended for individuals who are at high risk of febrile neutropenia or infection, including individuals who are expected to have profound, protracted neutropenia, defined as absolute neutrophil count (ANC) less than 100 cells/mm3 for more than 7 days or other risk factors (e.g., most individuals with acute myeloid leukemia/myelodysplastic syndromes (AML/MDS) or hematopoietic stem-cell transplantation (HSCT) treated with myeloablative conditioning regimens). Prophylaxis is not routinely recommended for individuals with solid tumors.[28674] [49827] [51812] [56105] [64861]
3 to 6 mg/kg/dose (Max: 400 mg/dose) IV once daily during the period of expected neutropenia.[51812] [53050] [53051] [53053] Higher doses (8 mg/kg/day; Max: 400 mg/day) have been reported in pediatric hematopoietic stem-cell transplantation (HSCT) recipients.[31231] For individuals receiving chemotherapy, initiate prophylaxis with induction chemotherapy and continue for the duration of neutropenia. Guidelines for preventing opportunistic infections in HSCT recipients recommend initiating antifungal prophylaxis at the start of conditioning and continuing until engraftment or 7 days after the absolute neutrophil count (ANC) is more than 1,000 cells/mm3.[51812]
3 to 6 mg/kg/dose (Max: 600 mg/dose) IV once daily during the period of expected neutropenia.[51812] [53050] [53051] [53053] Higher doses (8 mg/kg/day; Max: 400 mg/day) have been reported in pediatric hematopoietic stem-cell transplantation (HSCT) recipients.[31231] For individuals receiving chemotherapy, initiate prophylaxis with induction chemotherapy and continue for the duration of neutropenia. Guidelines for preventing opportunistic infections in HSCT recipients recommend initiating antifungal prophylaxis at the start of conditioning and continuing until engraftment or 7 days after the absolute neutrophil count (ANC) is more than 1,000 cells/mm3.[51812]
800 mg PO loading dose on day 1, followed by 400 mg PO once daily may be considered for high-risk individuals in ICUs with a high rate of invasive candidiasis (more than 5%).[60487]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily may be considered for high-risk individuals in ICUs with a high rate of invasive candidiasis (more than 5%).[60487]
3 to 6 mg/kg/dose PO twice weekly for 6 weeks in nurseries with high rates (more than 10%) of invasive candidiasis.[60487] Twice weekly regimens have been found to be as effective as more frequent dosage regimens with a lower incidence of cholestasis.[32699] [53058] Guidelines and several published studies limit the use of fluconazole prophylaxis to neonates weighing less than 1,000 g; however, some experts suggest considering prophylaxis for those neonates weighing less than 1,500 g who are at particularly high risk.[53059] [60487]
3 to 6 mg/kg/dose PO twice weekly for 6 weeks in nurseries with high rates (more than 10%) of invasive candidiasis.[60487] Twice weekly regimens have been found to be as effective as more frequent dosage regimens with a lower incidence of cholestasis.[32699] [53058] Although guidelines and several published studies recommend the use of fluconazole prophylaxis for neonates weighing less than 1,000 g, the safety and efficacy of fluconazole for the prophylaxis of invasive candidiasis in premature neonates weighing less than 750 g have not been established.[28674] [53059] [60487] In a prospective, randomized, double-blind, placebo-controlled, multicenter study (n = 361) evaluating fluconazole prophylaxis (6 mg/kg/dose given twice weekly for 6 weeks) in premature neonates weighing less than 750 g, the primary endpoint of death or candidiasis by study day 49 was similar in those who received fluconazole vs. placebo (17.5% vs. 22%; difference, -4.4 (95% CI: -12.6 to 3.8); p = 0.3). Death occurred in approximately 14% of subjects in each group and candidiasis occurred in 3% and 9% of subjects in the fluconazole and placebo groups, respectively.[28674]
3 to 6 mg/kg/dose IV twice weekly for 6 weeks in nurseries with high rates (more than 10%) of invasive candidiasis.[60487] Twice weekly regimens have been found to be as effective as more frequent dosage regimens with a lower incidence of cholestasis.[32699] [53058] Guidelines and several published studies limit the use of fluconazole prophylaxis to neonates weighing less than 1,000 g; however, some experts suggest considering prophylaxis for those neonates weighing less than 1,500 g who are at particularly high risk.[53059] [60487]
3 to 6 mg/kg/dose IV twice weekly for 6 weeks in nurseries with high rates (more than 10%) of invasive candidiasis.[60487] Twice weekly regimens have been found to be as effective as more frequent dosage regimens with a lower incidence of cholestasis.[32699] [53058] Although guidelines and several published studies recommend the use of fluconazole prophylaxis for neonates weighing less than 1,000 g, the safety and efficacy of fluconazole for the prophylaxis of invasive candidiasis in premature neonates weighing less than 750 g have not been established.[53059] [60487] [60686] In a prospective, randomized, double-blind, placebo-controlled, multicenter study (n = 361) evaluating fluconazole prophylaxis (6 mg/kg/dose given twice weekly for 6 weeks) in premature neonates weighing less than 750 g the primary endpoint of death or candidiasis by study day 49 was similar in those who received fluconazole vs. placebo (17.5% vs. 22%; difference, -4.4 (95% CI: -12.6 to 3.8); p = 0.3). Death occurred in approximately 14% of subject in each group and candidiasis occurred in 3% and 9% of subjects in the fluconazole and placebo groups, respectively.[60686]
100 mg PO 3 times weekly may be considered for persons who have recurrent infections.[60487]
100 mg PO once daily or 3 times weekly may be considered for persons who have frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
100 mg PO once daily or 3 times weekly may be considered for persons who have frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
3 to 6 mg/kg/dose (Max: 200 mg/dose) PO once daily may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count or percentage has risen to CDC Immunologic Category 1 or 2. Routine primary candidiasis prophylaxis is not recommended.[34361]
100 to 200 mg PO 3 times weekly may be considered in persons who have recurrent infections.[60487]
100 to 200 mg PO once daily may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
100 to 200 mg PO once daily may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
3 to 6 mg/kg/dose (Max: 200 mg/dose) PO once daily may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count or percentage has risen to CDC Immunologic Category 1 or 2. Routine primary candidiasis prophylaxis is not recommended.[34361]
400 mg IV as a single dose within 60 minutes prior to the surgical incision. Fluconazole is recommended for patients at high risk for Candida infection (e.g., enteric drainage of pancreas) undergoing liver, kidney, or pancreas transplantation. No intraoperative redosing and a duration of prophylaxis less than 24 hours are recommended by guidelines.[53477]
6 mg/kg/dose (Max: 400 mg/dose) IV as a single dose within 60 minutes prior to the surgical incision. Fluconazole is recommended for patients at high risk for Candida infection (e.g., enteric drainage of pancreas) undergoing liver, kidney, or pancreas transplantation. No intraoperative redosing and a duration of prophylaxis less than 24 hours are recommended by guidelines.[53477]
150 mg PO as a single dose.[28674] [34362] [60487] [66938]
150 mg PO as a single dose.[34362] [60487] [66938]
150 mg PO every 3 days for 2 to 3 doses.[60487] [66938]
150 mg PO every 3 days for 2 to 3 doses.[60487] [66938]
100 to 200 mg PO daily for at least 7 days.[34362]
100 to 200 mg PO daily for at least 7 days.[34362]
100 to 200 mg PO every 3 days for a total of 3 doses or daily therapy with oral fluconazole for 10 to 14 days, followed by long-term suppressive therapy.[60487] [66938]
100 to 200 mg PO every 3 days for a total of 3 doses or daily therapy with oral fluconazole for 10 to 14 days, followed by long-term suppressive therapy.[60487] [66938]
100 to 200 mg PO daily for at least 7 days, followed by long-term suppressive therapy.[34362]
100 to 200 mg PO daily for at least 7 days, followed by long-term suppressive therapy.[34362]
150 mg PO once daily on days 1, 4, and 7, followed by oteseconazole therapy for 12 weeks.[34362] [67532]
150 mg PO once daily on days 1, 4, and 7, followed by oteseconazole therapy for 12 weeks.[34362] [67532]
150 mg PO every 72 hours for 3 doses, followed by ibrexafungerp therapy for 6 months.[34362]
150 mg PO every 72 hours for 3 doses, followed by ibrexafungerp therapy for 6 months.[34362]
150 mg PO once monthly plus metronidazole.[66938]
150 mg PO once monthly plus metronidazole.[66938]
NOTE: For CNS infections, see dosage for meningitis.
400 to 800 mg PO once daily for 6 to 12 months in patients unable to take itraconazole.[34215]
NOTE: For CNS disease, see meningitis.
400 mg PO once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[61514] [68001]
400 mg PO once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[34362] [61514] [68001]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[34361] [61514] [68001]
6 to 12 mg/kg/dose PO once daily.[61514]
400 mg IV once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[61514] [68001]
400 mg IV once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[61514] [68001]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV once daily. Duration of treatment varies with disease location and depends on clinical response; treatment may be necessary for 12 months or longer.[34361] [61514] [68001]
6 to 12 mg/kg/dose IV once daily.[61514]
400 mg PO once daily as a preferred therapy. May discontinue therapy in patients who have clinically responded to 3 months or more of antifungal therapy, have a CD4 count of 250 cells/mm3 or more, are virologically suppressed on antiretrovirals, and continued monitoring for recurrence can be performed using serial chest radiograph and coccidioidal serology.[34362] [61514]
400 mg PO once daily as a preferred therapy. May discontinue therapy in patients who have clinically responded to 3 months or more of antifungal therapy, have a CD4 count of 250 cells/mm3 or more, are virologically suppressed on antiretrovirals, and continued monitoring for recurrence can be performed using serial chest radiograph and coccidioidal serology.[34362] [61514]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily. Consider long-term suppressive therapy if CD4 count is less than 250 cells/mm3 or CD4% is less than 15%.[34361] [61514]
6 to 12 mg/kg/dose (Max: 400 mg/dose) IV once daily. Consider long-term suppressive therapy if CD4 count is less than 250 cells/mm3 or CD4% is less than 15%.[34361] [61514]
400 mg PO once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy; discontinuation is dependent on clinical and serological response. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34362] [61514]
400 mg PO once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy; discontinuation is dependent on clinical and serological response. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34362] [61514]
12 mg/kg/dose (Max: 800 mg/dose) PO once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34361] [61514]
400 mg IV once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy; discontinuation is dependent on clinical and serological response. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34362] [61514]
400 mg IV once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy; discontinuation is dependent on clinical and serological response. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34362] [61514]
12 mg/kg/dose (Max: 800 mg/dose) IV once daily after clinical improvement on amphotericin B. Continue therapy for at least 12 months, followed by long-term suppressive therapy. Some experts will also add an azole to amphotericin B during the acute phase of treatment.[34361] [61514]
400 mg PO once daily for asymptomatic persons with a new positive IgM or IgG serologic test and CD4 count less than 250 cells/mm3. Discontinue therapy when CD4 count is 250 cells/mm3 or more with virologic suppression on antivirals. Close clinical follow-up is recommended after discontinuation of antifungal therapy.[34362]
400 mg PO once daily for asymptomatic persons with a new positive IgM or IgG serologic test and CD4 count less than 250 cells/mm3. Discontinue therapy when CD4 count is 250 cells/mm3 or more with virologic suppression on antivirals. Close clinical follow-up is recommended after discontinuation of antifungal therapy.[34362]
200 to 400 mg PO once daily for 6 to 12 months after transplant.[61514] [68001]
400 mg PO once daily for at least 12 months after transplant.[68001]
400 mg PO once daily. Discontinue therapy when have clinical response to 3 months or more of antifungal therapy, a CD4 count of 250 cells/mm3 or more, virological suppression on antiretrovirals, and continued monitoring for recurrence can be performed using serial chest radiograph and coccidioidal serology.[34362]
400 mg PO once daily. Discontinue therapy when have clinical response to 3 months or more of antifungal therapy, a CD4 count of 250 cells/mm3 or more, virological suppression on antiretrovirals, and continued monitoring for recurrence can be performed using serial chest radiograph and coccidioidal serology.[34362]
6 mg/kg/dose (Max: 400 mg/dose) PO once daily. May consider discontinuation of therapy when have clinical response and a CD4 count of 250 cells/mm3 or more or CD4% of 15% or more.[34361]
400 mg PO once daily. Prophylaxis may be lifelong; discontinuation is dependent on clinical and serological response.[34362]
400 mg PO once daily. Prophylaxis may be lifelong; discontinuation is dependent on clinical and serological response.[34362]
6 mg/kg/dose (Max: 400 mg/dose) PO once daily. Prophylaxis is lifelong.[34361]
400 mg PO once daily. Prophylaxis is lifelong.[34362] [61514]
400 mg PO once daily. Prophylaxis is lifelong.[34362] [61514]
6 mg/kg/dose (Max: 400 mg/dose) PO once daily. Prophylaxis is lifelong.[34361] [61514]
800 or 1,200 mg PO once daily plus amphotericin B deoxycholate or liposomal amphotericin B or 1,200 mg PO once daily plus flucytosine for at least 2 weeks as an induction therapy. If the patient is clinically stable and CSF culture is negative at 2 weeks, switch to consolidation therapy of 800 mg PO once daily for at least 8 weeks. If the CSF remains positive in a clinically stable patient after 2 weeks of induction therapy, give 1,200 mg PO once daily either alone or in combination with flucytosine for an additional 2 weeks before starting consolidation therapy of 800 mg PO once daily. The consolidation dose may then be reduced to 400 mg PO once daily in clinically stable patients if the CSF culture is known to be sterile and antiretroviral therapy has been initiated. After at least 8 weeks of consolidation therapy, give 200 mg PO once daily as chronic maintenance therapy. May increase dose to 400 mg PO once daily if fluconazole MIC is 16 mcg/mL or more. Chronic maintenance therapy may be discontinued after at least 1 year from the start of antifungal therapy if patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with suppressed HIV RNA in response to effective antiretroviral therapy. Restart chronic maintenance therapy if CD4 count is less than 100 cells/mm3.[34362] [66807] The FDA-approved dosage is 400 mg PO on day 1, followed by 200 to 400 mg PO once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg PO once daily.[28674]
800 or 1,200 mg PO once daily plus amphotericin B deoxycholate or liposomal amphotericin B or 1,200 mg PO once daily plus flucytosine for at least 2 weeks as an induction therapy. If the patient is clinically stable and CSF culture is negative at 2 weeks, switch to consolidation therapy of 800 mg PO once daily for at least 8 weeks. If the CSF remains positive in a clinically stable patient after 2 weeks of induction therapy, give 1,200 mg PO once daily either alone or in combination with flucytosine for an additional 2 weeks before starting consolidation therapy of 800 mg PO once daily. The consolidation dose may then be reduced to 400 mg PO once daily in clinically stable patients if the CSF culture is known to be sterile and antiretroviral therapy has been initiated. After at least 8 weeks of consolidation therapy, give 200 mg PO once daily as chronic maintenance therapy. May increase dose to 400 mg PO once daily if fluconazole MIC is 16 mcg/mL or more. Chronic maintenance therapy may be discontinued after at least 1 year from the start of antifungal therapy if patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with suppressed HIV RNA in response to effective antiretroviral therapy. Restart chronic maintenance therapy if CD4 count is less than 100 cells/mm3.[34362] [66807] The FDA-approved dosage is 400 mg PO on day 1, followed by 200 to 400 mg PO once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg PO once daily.[28674]
12 mg/kg/dose (Max: 800 mg/dose) PO loading dose on day 1, followed by 10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily plus amphotericin B or flucytosine for at least 2 weeks as an alternate induction therapy, followed by 10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily for at least 8 weeks as consolidation therapy. If induction therapy did not include fluconazole, begin consolidation therapy at 12 mg/kg/dose (Max: 800 mg/dose) PO on day 1, then 10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily. Continue consolidation therapy for at least 8 weeks, followed by 6 mg/kg/dose (Max: 200 mg/dose) PO once daily for at least 1 year as chronic suppressive therapy. Suppressive therapy may be discontinued after at least 1 year on chronic suppressive therapy in children 6 years and older if the patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with an undetectable viral load for more than 3 months on antiretroviral therapy. Restart suppressive therapy if CD4 count is less than 100 cells/mm3.[34361] [66807] The FDA-approved dosage is 12 mg/kg/dose PO on day 1, followed by 6 to 12 mg/kg/dose PO once daily for 10 to 12 weeks after CSF becomes negative, then 6 mg/kg/dose PO once daily.[28674]
12 mg/kg/dose PO loading dose on day 1, followed by 10 to 12 mg/kg/dose PO once daily plus amphotericin B or flucytosine for at least 2 weeks as an alternate induction therapy, followed by 10 to 12 mg/kg/dose PO once daily for at least 8 weeks as consolidation therapy. If induction therapy did not include fluconazole, begin consolidation therapy at 12 mg/kg/dose PO on day 1, then 10 to 12 mg/kg/dose PO once daily. Continue consolidation therapy for at least 8 weeks, followed by 6 mg/kg/dose PO once daily as chronic suppressive therapy.[34361]
1,200 mg IV once daily plus flucytosine for at least 2 weeks as an alternate induction therapy, followed by oral fluconazole consolidation therapy and chronic maintenance therapy.[34362] [66807] The FDA-approved dosage is 400 mg IV on day 1, followed by 200 to 400 mg IV once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg IV once daily.[60686]
1,200 mg IV once daily plus flucytosine for at least 2 weeks as an alternate induction therapy, followed by oral fluconazole consolidation therapy and chronic maintenance therapy.[34362] [66807] The FDA-approved dosage is 400 mg IV on day 1, followed by 200 to 400 mg IV once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg IV once daily.[60686]
12 mg/kg/dose (Max: 800 mg/dose) IV loading dose on day 1, followed by 10 to 12 mg/kg/dose (Max: 800 mg/dose) IV once daily plus amphotericin B or flucytosine for at least 2 weeks as an alternate induction therapy, followed by 10 to 12 mg/kg/dose (Max: 800 mg/dose) IV once daily for at least 8 weeks as consolidation therapy. If induction therapy did not include fluconazole, begin consolidation therapy at 12 mg/kg/dose (Max: 800 mg/dose) IV on day 1, then 10 to 12 mg/kg/dose (Max: 800 mg/dose) IV once daily. Continue consolidation therapy for at least 8 weeks, followed by oral chronic suppressive therapy.[34361] [66807] The FDA-approved dosage is 12 mg/kg/dose IV on day 1, followed by 6 to 12 mg/kg/dose IV once daily for 10 to 12 weeks after CSF becomes negative, then 6 mg/kg/dose IV once daily.[60686]
12 mg/kg/dose IV loading dose on day 1, followed by 10 to 12 mg/kg/dose IV once daily plus amphotericin B or flucytosine for at least 2 weeks as an alternate induction therapy, followed by 10 to 12 mg/kg/dose IV once daily for at least 8 weeks as consolidation therapy. If induction therapy did not include fluconazole, begin consolidation therapy at 12 mg/kg/dose IV on day 1, then 10 to 12 mg/kg/dose IV once daily. Continue consolidation therapy for at least 8 weeks, followed by oral chronic suppressive therapy.[34361]
400 to 800 mg PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 200 to 400 mg PO once daily for 6 to 12 months.[50783] The FDA-approved dosage is 400 mg PO on day 1, followed by 200 to 400 mg PO once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg PO once daily.[28674]
10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 to 12 months.[50783] The FDA-approved dosage is 12 mg/kg/dose PO on day 1, followed by 6 to 12 mg/kg/dose PO once daily for 10 to 12 weeks after CSF becomes negative, then 6 mg/kg/dose PO once daily.[28674]
10 to 12 mg/kg/dose PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose PO once daily for 6 to 12 months.[50783]
400 mg PO once daily for 8 weeks after the initial 4-week course of induction therapy or 800 mg PO once daily for 8 weeks after an initial 2-week course of induction therapy, followed by 200 mg PO once daily for 6 to 12 months.[50783] The FDA-approved dosage is 400 mg PO on day 1, followed by 200 to 400 mg PO once daily for 10 to 12 weeks after CSF becomes negative, then 200 mg PO once daily.[28674]
10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose (Max: 200 mg/dose) PO once daily for 6 to 12 months.[50783] The FDA-approved dosage is 12 mg/kg/dose PO on day 1, followed by 6 to 12 mg/kg/dose PO once daily for 10 to 12 weeks after CSF becomes negative, then 6 mg/kg/dose PO once daily.[28674]
10 to 12 mg/kg/dose PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose PO once daily for 6 to 12 months.[50783]
NOTE: For the treatment of CNS infections, see cryptococcal meningitis.
400 mg PO once daily for 6 to 12 months in combination with antiretroviral therapy. Duration guided by symptom resolution.[34362]
400 mg PO once daily for 6 to 12 months in combination with antiretroviral therapy. Duration guided by symptom resolution.[34362]
12 mg/kg/dose (Max: 600 mg/dose) PO loading dose on day 1, followed by 6 to 12 mg/kg/dose (Max: 600 mg/dose) PO once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, 6 mg/kg/dose (Max: 200 mg/dose) PO once daily for at least 1 year as chronic suppressive therapy. Suppressive therapy may be discontinued after at least 1 year on chronic suppressive therapy in children 6 years and older if the patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with an undetectable viral load for more than 3 months on antiretroviral therapy. Restart suppressive therapy if CD4 count is less than 100 cells/mm3.[34361]
12 mg/kg/dose PO loading dose on day 1, followed by 6 to 12 mg/kg/dose PO once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, 6 mg/kg/dose PO once daily for at least 1 year as chronic suppressive therapy.[34361]
12 mg/kg/dose (Max: 600 mg/dose) IV loading dose on day 1, followed by 6 to 12 mg/kg/dose (Max: 600 mg/dose) IV once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, continue oral chronic suppressive therapy for at least 1 year.[34361]
12 mg/kg/dose IV loading dose on day 1, followed by 6 to 12 mg/kg/dose IV once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, continue oral chronic suppressive therapy for at least 1 year.[34361]
800 to 1,200 mg PO daily for 2 weeks, followed by 400 to 800 mg PO daily for 10 weeks, then 200 mg PO daily for a total of 6 months. Give in combination with antiretroviral therapy.[34362]
800 to 1,200 mg PO daily for 2 weeks, followed by 400 to 800 mg PO daily for 10 weeks, then 200 mg PO daily for a total of 6 months. Give in combination with antiretroviral therapy.[34362]
800 or 1,200 mg PO once daily plus amphotericin B deoxycholate or liposomal amphotericin B or 1,200 mg PO once daily plus flucytosine for at least 2 weeks as an induction therapy, followed by 800 mg PO once daily for at least 8 weeks as consolidation therapy. The consolidation dose may be reduced to 400 mg PO once daily in clinically stable patients if the CSF culture is known to be sterile and antiretroviral therapy has been initiated. After at least 8 weeks of consolidation therapy, give 200 mg PO once daily as chronic maintenance therapy. May increase dose to 400 mg PO once daily if fluconazole MIC is 16 mcg/mL or more. Chronic maintenance therapy may be discontinued after at least 1 year from the start of antifungal therapy if patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with suppressed HIV RNA in response to effective antiretroviral therapy. Restart chronic maintenance therapy if CD4 count is less than 100 cells/mm3.[34362] [66807]
800 or 1,200 mg PO once daily plus amphotericin B deoxycholate or liposomal amphotericin B or 1,200 mg PO once daily plus flucytosine for at least 2 weeks as an induction therapy, followed by 800 mg PO once daily for at least 8 weeks as consolidation therapy. The consolidation dose may be reduced to 400 mg PO once daily in clinically stable patients if the CSF culture is known to be sterile and antiretroviral therapy has been initiated. After at least 8 weeks of consolidation therapy, give 200 mg PO once daily as chronic maintenance therapy. May increase dose to 400 mg PO once daily if fluconazole MIC is 16 mcg/mL or more. Chronic maintenance therapy may be discontinued after at least 1 year from the start of antifungal therapy if patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with suppressed HIV RNA in response to effective antiretroviral therapy. Restart chronic maintenance therapy if CD4 count is less than 100 cells/mm3.[34362] [66807]
12 mg/kg/dose (Max: 600 mg/dose) PO loading dose on day 1, followed by 6 to 12 mg/kg/dose (Max: 600 mg/dose) PO once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, 6 mg/kg/dose (Max: 200 mg/dose) PO once daily for at least 1 year as chronic suppressive therapy. Suppressive therapy may be discontinued after at least 1 year on chronic suppressive therapy in children 6 years and older if the patient remains asymptomatic and the CD4 count is 100 cells/mm3 or more with an undetectable viral load for more than 3 months on antiretroviral therapy. Restart suppressive therapy if CD4 count is less than 100 cells/mm3.[34361]
12 mg/kg/dose PO loading dose on day 1, followed by 6 to 12 mg/kg/dose PO once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, 6 mg/kg/dose PO once daily for at least 1 year as chronic suppressive therapy.[34361]
1,200 mg IV once daily plus flucytosine for at least 2 weeks as an alternate induction therapy, followed by oral fluconazole consolidation therapy and chronic maintenance therapy.[34362] [66807]
1,200 mg IV once daily plus flucytosine for at least 2 weeks as an alternate induction therapy, followed by oral fluconazole consolidation therapy and chronic maintenance therapy.[34362] [66807]
12 mg/kg/dose (Max: 600 mg/dose) IV loading dose on day 1, followed by 6 to 12 mg/kg/dose (Max: 600 mg/dose) IV once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, continue oral chronic suppressive therapy for at least 1 year.[34361]
12 mg/kg/dose IV loading dose on day 1, followed by 6 to 12 mg/kg/dose IV once daily; treatment duration is dependent on site/severity of infection and clinical response. After initial therapy, continue oral chronic suppressive therapy for at least 1 year.[34361]
400 mg PO once daily for 6 to 12 months.[50783]
6 to 12 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 to 12 months.[50783]
6 to 12 mg/kg/dose PO once daily for 6 to 12 months.[50783]
400 to 800 mg PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 200 to 400 mg PO once daily for 6 to 12 months.[50783]
10 to 12 mg/kg/dose (Max: 800 mg/dose) PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose (Max: 400 mg/dose) PO once daily for 6 to 12 months.[50783]
10 to 12 mg/kg/dose PO once daily for 8 weeks after the initial 2-week course of induction therapy, followed by 6 mg/kg/dose PO once daily for 6 to 12 months.[50783]
NOTE: For CNS infections, see meningitis indication.
800 mg PO once daily for at least 12 months as an alternative to itraconazole in patients with CD4 less than 300 cells/mm3.[34362]
800 mg PO once daily for at least 12 months as an alternative to itraconazole in patients with CD4 less than 300 cells/mm3.[34362]
3 to 6 mg/kg/dose (Max: 200 mg/dose) PO once daily for 12 months as an alternative to itraconazole.[34361]
800 mg PO once daily for at least 12 months as an alternative in patients who are intolerant to itraconazole.[34362]
800 mg PO once daily for at least 12 months as an alternative in patients who are intolerant to itraconazole.[34362]
5 to 6 mg/kg/dose (Max: 300 mg/dose) PO twice daily for at least 12 months as an alternative to itraconazole.[34361]
5 to 6 mg/kg/dose (Max: 300 mg/dose) IV twice daily for 12 months as an alternative to itraconazole.[34361]
800 mg PO once daily as an alternative step-down therapy after an amphotericin B product in patients who are intolerant to itraconazole. Continue maintenance therapy for at least 12 months.[34362]
800 mg PO once daily as an alternative step-down therapy after an amphotericin B product in patients who are intolerant to itraconazole. Continue maintenance therapy for at least 12 months.[34362]
400 mg PO once daily as an alternative to itraconazole for patients with severe disseminated or CNS infection after completing at least 12 months of therapy and relapse despite appropriate initial therapy (after reinduction therapy). Consider discontinuation if patients have received treatment for at least 1 year, have negative blood cultures, have a serum or urine Histoplasma antigen below the level of quantification, have an undetectable viral load, and have a CD4 count of more than 150 cells/mm3 on antiretroviral therapy for at least 6 months. Resume secondary prophylaxis if the CD4 count decreases below 150 cells/mm3.[34362]
400 mg PO once daily as an alternative to itraconazole for patients with severe disseminated or CNS infection after completing at least 12 months of therapy and relapse despite appropriate initial therapy (after reinduction therapy). Consider discontinuation if patients have received treatment for at least 1 year, have negative blood cultures, have a serum or urine Histoplasma antigen below the level of quantification, have an undetectable viral load, and have a CD4 count of more than 150 cells/mm3 on antiretroviral therapy for at least 6 months. Resume secondary prophylaxis if the CD4 count decreases below 150 cells/mm3.[34362]
3 to 6 mg/kg/dose (Max: 200 mg/dose) PO once daily as an alternative to itraconazole for patients who remain immunosuppressed and in those who relapse despite appropriate initial therapy. Consider discontinuation if patients have received treatment for at least 1 year, have negative blood cultures, have a serum or urine Histoplasma antigen below the level of quantification, have an undetectable viral load, and have a CD4 percentage greater than 15% at any age or CD4 count of more than 150 cells/mm3 if older than 6 years. Resume secondary prophylaxis if the parameters are not met.[34361]
400 mg PO once weekly as alternative therapy. Recommended for patients with CD4 count less than 100 cells/mm3 who are unable to have antiretroviral therapy (ART) or have treatment failure without access to effective ART options and who reside in the highly endemic regions in northern Thailand, Vietnam, or southern China. May discontinue if the CD4 count is more than 100 cells/mm3 for 6 months or more in response to ART or virologic suppression is achieved for 6 months or more on ART. Restart prophylaxis if CD4 count is less than 100 cells/mm3 and patient still resides in high-risk areas.[34362]
400 mg PO once weekly as alternative therapy. Recommended for patients with CD4 count less than 100 cells/mm3 who are unable to have antiretroviral therapy (ART) or have treatment failure without access to effective ART options and who reside in the highly endemic regions in northern Thailand, Vietnam, or southern China. May discontinue if the CD4 count is more than 100 cells/mm3 for 6 months or more in response to ART or virologic suppression is achieved for 6 months or more on ART. Restart prophylaxis if CD4 count is less than 100 cells/mm3 and patient still resides in high-risk areas.[34362]
400 mg PO once weekly starting 3 days before travel and continuing for 1 week after leaving the endemic area as alternative therapy. Recommended for patients with CD4 count less than 100 cells/mm3 who are unable to have antiretroviral therapy (ART) or have treatment failure without access to effective ART options and who are from countries outside the highly endemic regions in northern Thailand, Vietnam, or southern China and must travel to the region. Restart prophylaxis if CD4 count is less than 100 cells/mm3 and patient still travels to high-risk areas.[34362]
400 mg PO once weekly starting 3 days before travel and continuing for 1 week after leaving the endemic area as alternative therapy. Recommended for patients with CD4 count less than 100 cells/mm3 who are unable to have antiretroviral therapy (ART) or have treatment failure without access to effective ART options and who are from countries outside the highly endemic regions in northern Thailand, Vietnam, or southern China and must travel to the region. Restart prophylaxis if CD4 count is less than 100 cells/mm3 and patient still travels to high-risk areas.[34362]
200 mg PO once daily for 6 weeks. Alternatively for infections due to L. major, 400 mg PO once daily for 6 weeks.[63762]
5 mg/kg/dose (Max: 200 mg/dose) PO once daily for 6 weeks.[63762] [64603] [64604] [64605] [64606] [64607] [70821] Higher doses (8 mg/kg/dose [Max: 400 mg/dose] PO once daily) may be needed for incomplete clinical response or infections due to L. major.[63762] [64606]
100 to 400 mg PO once daily in febrile, immunosuppressed patients as an alternative to an echinocandin or amphotericin B.[57437]
800 mg IV loading dose on day 1, followed by 400 mg IV once daily in febrile, immunosuppressed patients as an alternative to an echinocandin or amphotericin B.[57437]
400 to 800 mg PO once daily for 2 to 4 weeks after all lesions have resolved, usually for a total of 3 to 6 months in patients who cannot tolerate other agents.[50784]
6 mg/kg/dose (Max: 400 mg/dose) PO once daily for 3 to 6 weeks or 8 mg/kg/dose (Max: 400 mg/dose) PO once weekly for 8 to 12 weeks.[34406] [59020] [67612] [67615] [67644] [67645] [67661]
100 to 200 mg PO once weekly for 6 months may be considered for persons who have recurrent infections.[60487] [66938]
100 to 200 mg PO once weekly for 6 months may be considered for persons who have recurrent infections.[60487] [66938]
150 mg PO once weekly may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
150 mg PO once weekly may be considered for persons with frequent or severe recurrences. Discontinuation of secondary prophylaxis is reasonable when the CD4 count is more than 200 cells/mm3 after the start of antiretroviral therapy. Routine primary candidiasis prophylaxis is not recommended.[34362]
400 mg/day PO/IV is FDA-approved maximum; however, doses up to 800 mg PO/IV loading dose and 1,200 mg/day PO/IV maintenance dose have been used off-label.
400 mg/day PO/IV is FDA-approved maximum; however, doses up to 800 mg PO/IV loading dose and 1,200 mg/day PO/IV maintenance dose have been used off-label.
25 mg/kg (35 mg/kg for patients on ECMO) PO/IV loading dose (Max: 800 mg/dose), then 12 mg/kg/day (Max: 400 mg/day) PO/IV is FDA-approved maximum; however, doses up to 1,200 mg/day PO/IV have been used off-label.
25 mg/kg (35 mg/kg for patients on ECMO) PO/IV loading dose (Max: 800 mg/dose), then 12 mg/kg/day (Max: 400 mg/day) PO/IV is FDA-approved maximum; however, doses up to 800 mg/day PO/IV have been used off-label.
25 mg/kg (35 mg/kg for patients on ECMO) PO/IV loading dose, then 12 mg/kg/day PO/IV.
30 weeks gestation and older: 25 mg/kg (35 mg/kg for patients on ECMO) PO/IV loading dose, then 12 mg/kg/day PO/IV.
younger than 30 weeks gestation and 0 to 90 days postnatal age: 25 mg/kg (35 mg/kg for patients on ECMO) PO/IV loading dose, then 9 mg/kg/day PO/IV.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
NOTE: No dosage adjustments are required for single-dose therapy. For multiple-dose regimens, the following adjustments are suggested; further adjustments may be needed depending upon the clinical situation.[28674]
Adults[28674][32569][60686]
CrCl more than 50 mL/minute: No dosage adjustment needed.
CrCl 50 mL/minute or less: Administer usual loading dose, then reduce maintenance dose by 50%.
Infants, Children, and Adolescents [28674][32569][60686]
CrCl more than 50 mL/minute/1.73 m2: No dosage adjustment needed.
CrCl 10 to 50 mL/minute/1.73 m2: Administer usual loading dose, then reduce maintenance dose by 50%.
CrCl less than 10 mL/minute/1.73 m2: Administer usual loading dose, then reduce maintenance dose by 50% and administer every 48 hours.
Neonates† [53038]
Serum creatinine (SCr) less than 1.3 mg/dL: No dosage adjustment needed.
Serum creatinine (SCr) 1.3 mg/dL or more: Consider extending the dosage interval (e.g., every 48 to 72 hours) depending on the degree of renal impairment.
Intermittent hemodialysis
NOTE: A 3-hour hemodialysis session decreases plasma concentrations by approximately 50%.[28674][32569][60686]
Adults and Pediatric patients (FDA-approved labeling)
Administer 100% of the usual daily dose after each dialysis session; on non-dialysis days, administer a reduced dose based on creatinine clearance. Further adjustments may be needed depending upon the clinical situation.[28674][60686]
Adults (alternative)†
200 to 400 mg IV or PO every 48 to 72 hours or 100 to 200 mg IV or PO every 24 hours.[42303]
Pediatric patients (alternative)†
Administer usual loading dose, then reduce maintenance dose by 50% and administer every 48 hours (after dialysis).[32569]
Peritoneal dialysis†
Adults
Administer usual loading dose, then reduce maintenance dose by 50%.[32569]
Pediatric patients
Administer usual loading dose, then reduce maintenance dose by 50% and administer every 48 hours.[32569]
Continuous renal replacement therapy (CRRT)†
NOTE: Various CRRT modalities include continuous venovenous hemofiltration (CVVH), continuous venovenous hemodialysis (CVVHD), continuous venovenous hemodiafiltration (CVVHDF), continuous venovenous high-flux hemodialysis (CVVHFD), continuous arteriovenous hemofiltration (CAVH), continuous arteriovenous hemodialysis (CAVHD), and continuous arteriovenous hemodiafiltration (CAVHDF). Dosing should take into consideration patient-specific factors (e.g., intrinsic renal function), type of infection, the duration of renal replacement therapy, the effluent flow rate, and the replacement solution administered.[42303]
Adults
200 to 400 mg IV or PO every 24 hours has generally been suggested for CRRT.[32569] Specific recommendations for patients receiving CVVH, CVVHD, or CVVHD include the following:
CVVH: 400 to 800 mg IV or PO loading dose, then 200 to 400 mg IV or PO every 24 hours.[34038][42303]
CVVHD or CVVHDF: 400 mg to 800 mg IV or PO every 24 hours. If the dialysate flow rate is 2 L/hour or more and/or if treating relatively resistant organisms, 800 mg IV or PO every 24 hours.[34038][42303]
Pediatric patients
Pediatric recommendations are based on limited study data, mainly derived from adult patients, and extrapolation of CRRT clearance based on fluconazole pharmacokinetic parameters.[67116]
6 mg/kg/dose IV or PO every 24 hours has generally been suggested for CRRT.[32569] Specific recommendations for patients receiving CAVH/CVVH and CAVHD/CVVHD based on dialysate flow rate include the following:
Dialysate flow rate (ultrafiltration rate + dialysis inflow rate) less than 1,500 mL/m2/hour: Administer usual loading dose, then 3 to 12 mg/kg/dose IV or PO every 24 hours.
Dialysate flow rate (ultrafiltration rate + dialysis inflow rate) 1,500 mL/m2/hour or more: Administer usual loading dose, then 6 to 12 mg/kg/dose IV or PO every 24 hours.[67116]
Hybrid hemodialysis†
NOTE: Hybrid treatments include prolonged intermittent renal replacement therapy (PIRRT), sustained low-efficiency dialysis (SLED), slow extended daily dialysis/diafiltration (SLEDD-f), and extended daily dialysis (EDD). Dosing should take into consideration patient-specific factors (e.g., intrinsic renal function), the type of infection, the duration of renal replacement therapy, the ultrafiltration rate, the dialysis flow rate, and how often dialysis sessions occur.[65397]
Adults
800 mg IV loading dose, then 400 mg IV every 12 hours or pre- and post-PIRRT achieved at least a 90% probability of pharmacodynamic target attainment for C. albicans for an 8- to 10-hour PIRRT session. Dosing was studied using 4 different PIRRT setting simulations over 8 to 10 hours/day in a Monte Carlo simulation study using population pharmacokinetic data.[65424]
Pediatric patients
Fluconazole dosing data are not available in pediatric patients receiving hybrid hemodialysis. Based on adult data, dosage adjustments may be necessary.[65424]
† Off-label indication




















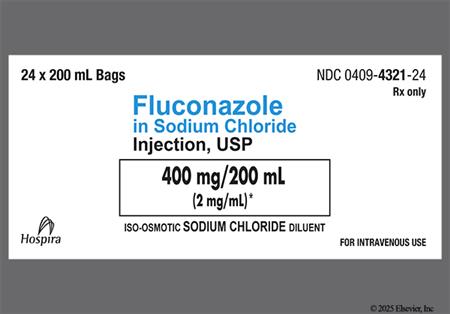
Fluconazole is a synthetic antifungal agent of the triazole class. It is administered orally and intravenously. The antifungal spectrum for fluconazole is broader than that of the imidazole antifungals class, which includes agents such as ketoconazole, miconazole, and clotrimazole. Fluconazole is more resistant to first-pass metabolism and has lower lipophilicity and protein binding than does ketoconazole. Unlike ketoconazole, the oral absorption of fluconazole is not affected by the absence of stomach acid. Fluconazole is approved for the treatment of a variety of infections caused by Candida and for the treatment of cryptococcal meningitis. Additionally, fluconazole is indicated to decrease the incidence of candidiasis in patients undergoing bone marrow transplant who receive chemotherapy and/or radiation therapy.[28674] Fluconazole has been shown equivalent to amphotericin B in the treatment of candidemia in non-neutropenic patients; however, prophylactic use of fluconazole in bone-marrow transplant patients has been associated with increased recovery of C. krusei.[24147][24148]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Reconstitution
Preparation
Intermittent IV Infusion
In comparative clinical trials of fluconazole 150 mg single doses for vaginal candidiasis (n = 448), nausea (7%) and abdominal pain (6%) were among the most common treatment-related adverse reactions associated with fluconazole. Other adverse effects reported included diarrhea (3%), dyspepsia (1%), and dysgeusia (1%). In patients receiving fluconazole for 7 days or more in clinical trials for other indications (n = 4,048), the most frequently reported (1% or more of patients) adverse reactions included nausea (4%), vomiting (2%), abdominal pain (12%), and diarrhea (2%). In children receiving fluconazole in phase II/III clinical trials (n = 577), the most commonly reported adverse reactions were nausea (2%), vomiting (5%), abdominal pain (3%), and diarrhea (2%). Xerostomia has been reported with postmarketing use of fluconazole.[28674]
In patients receiving fluconazole for 7 days or more in clinical trials (n = 4,048), skin rash occurred in approximately 2% of patients. Exfoliative skin disorders, such as Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported in patients taking fluconazole. Fluconazole-associated dermatologic adverse events have resulted in fatal outcomes for patients with serious underlying diseases, such as AIDS or malignancy. Monitor drug recipients for development of a rash. If a rash is observed in a patient being treated for a superficial fungal infection and the rash is attributed to fluconazole, immediately discontinue use of the drug. If a rash develops in a patient being treated for a deep-seated fungal infection, closely monitor the patient and discontinue fluconazole if the lesion progresses. Other dermatologic adverse reactions reported during postmarketing use of the drug include acute generalized exanthematous pustulosis (AGEP), drug reaction with eosinophilia and systemic symptoms (DRESS), and hyperhidrosis (increased sweating).[28674] Fluconazole-induced alopecia has also been reported in postmarketing surveillance. In most cases, the hair loss involved the scalp, but in other cases, substantial loss of facial, leg, axillary, pubic, or chest hair occurred. In 3 patients, scalp hair loss required the use of a wig. In almost all patients, the alopecia resolved after discontinuation or reduction in the dose of fluconazole.[24277] [28674]
Rarely, angioedema and anaphylactoid reactions (including facial edema and pruritus) have been reported with fluconazole in postmarketing experience after single and multiple doses.[28674]
During postmarketing surveillance, rare cases of QT prolongation and torsade de pointes have been reported with fluconazole use. Most of these reports have included seriously ill individuals with multiple confounding risk factors that may have been contributory. Fluconazole prolongs the QT interval through inhibition of cardiac rectifier potassium channel currents.[28674] [60686]
Fluconazole has been associated with rare cases of serious hepatotoxicity. These hepatic reactions have ranged from mild transient elevated hepatic enzymes to clinical hepatitis, cholestasis and fulminant hepatic failure, including fatalities. Instances of fatal hepatic reactions were noted to occur primarily in patients with serious underlying medical conditions (predominantly AIDS or malignancy) and often while taking multiple concomitant medications. Transient hepatic reactions, including hepatitis and jaundice, have occurred among patients with no other identifiable risk factors. Fluconazole hepatotoxicity has usually, but not always, been reversible on discontinuation of therapy. Monitor patients who develop abnormal liver function tests during fluconazole therapy for the development of more severe hepatic injury. Discontinue fluconazole if clinical signs and symptoms consistent with liver disease develop that may be attributable to fluconazole. In 2 comparative trials evaluating the efficacy of fluconazole for the suppression of relapse of cryptococcal meningitis, a statistically significant increase was observed in median aspartate aminotransferase (AST) concentrations from a baseline value of 30 International Units/L to 41 International Units/L in 1 trial and 34 International Units/L to 66 International Units/L in the other trial. The overall rate of serum transaminase elevations of more than 8 times the upper limit of normal was approximately 1% in fluconazole-treated patients in clinical trials. These elevations occurred in patients with severe underlying disease, predominantly AIDS or malignancies, most of whom were receiving multiple concomitant medications, including many known to be hepatotoxic.[28674] Elevated transaminases (alanine aminotransferase (ALT), 5%; AST, 3%) and alkaline phosphatase (2%) have been reported in pediatric patients and were the most common treatment-related laboratory abnormalities in clinical trials.[53061] A higher incidence of cholestasis (direct bilirubin 2 mg/dL or more) was reported in neonates receiving more frequent dosing of fluconazole prophylaxis compared with those receiving less frequent dosing of fluconazole prophylaxis (43% vs. 29%) in a retrospective study (n = 244).[53058]
Leukopenia, including neutropenia and agranulocytosis, and thrombocytopenia have been reported during postmarketing use of fluconazole.[28674]
In comparative clinical trials of fluconazole 150 mg single doses for vaginal candidiasis (n = 448), headache (13%) was among the most common treatment-related adverse reactions associated with fluconazole. Dizziness was reported in 1% of patients receiving fluconazole. In patients receiving fluconazole for 7 days or more in clinical trials for other indications (n = 4,048), headache was reported in 2% of patients receiving fluconazole. Seizures, drowsiness, insomnia, paresthesias, tremor, and vertigo have been reported during postmarketing use of fluconazole.[28674]
Hypokalemia, hypercholesterolemia, and hypertriglyceridemia have been reported during postmarketing use of fluconazole.[28674]
Asthenia, fatigue, fever, malaise, and myalgia have been reported during postmarketing use of fluconazole.[28674]
Reversible cases of adrenocortical insufficiency have been reported in patients receiving fluconazole. Advise patients to report any symptoms of adrenal insufficiency, including long-lasting fatigue, muscle weakness, loss of appetite, weight loss, abdominal pain, nausea, vomiting, or dizziness.[28674]
Anemia and acute renal failure have been reported in postmarketing experience. These events were observed more frequently in persons 65 years of age and older than in younger persons.[28674]
Fluconazole has been associated with teratogenesis when used early in a pregnancy at high doses. Fluconazole produces a characteristic pattern of fetal abnormalities including craniofacial, skeletal and cardiac anomalies, similar to Antley-Bixler syndrome when used during the first trimester. These effects may be dose-dependent. The nature of the observed birth defects suggests that the teratogenic effects may occur before the woman is aware she is pregnant. The exact mechanism is not known.[26025] [28674]
GI perforation, including ileal and small intestinal perforation, was reported at a higher incidence in premature neonates weighing less than 750 g receiving fluconazole prophylaxis (6 mg/kg/dose given twice-weekly for 6 weeks) compared with placebo (7% vs. 4%) in a prospective, randomized, double-blind, multicenter study (n = 361). Other serious adverse reactions reported in the fluconazole vs. placebo groups, respectively, include necrotizing enterocolitis (NEC; 14% vs. 16%), respiratory failure (7% vs. 2%), and bacterial sepsis (5% vs. 7%). The most common fatal serious adverse reactions in the fluconazole vs. placebo groups, respectively, were NEC (5% vs. 5%), neonatal bacterial sepsis (3% vs. 4%), and respiratory failure (2% vs. 0.6%).[28674]
There have been reports of cases of superinfection with Candida species other than C. albicans, which are often inherently not susceptible to fluconazole (e.g., C. krusei). Such cases may require alternative antifungal therapy.[28674] [60686]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Use fluconazole with caution in individuals with hypersensitivity to other azoles; there is no information regarding cross hypersensitivity between fluconazole and other azole antifungal agents.[28674][60686]
Cases of superinfection caused by Candida species other than C. albicans have been reported. These Candida species are often inherently not susceptible to fluconazole and may require treatment with an alternative antifungal therapy.[28674][60686]
Due to the sucrose content, fluconazole oral suspension is not recommended in individuals with hereditary fructose intolerance, glucose-galactose malabsorption, or sucrase-isomaltase deficiency.[28674]
Use fluconazole with caution in people with baseline QT prolongation or who have conditions that may increase the risk of QT prolongation or torsade de pointes, including bradycardia, congenital long QT syndrome, hypocalcemia, hypokalemia, hypomagnesemia, geriatric adults, females, structural abnormalities that interfere with electrical conduction (e.g., cardiomyopathy, coronary artery disease, ischemic heart disease), or in those who have other additional risk factors for QT prolongation or torsade de pointes. The use of other medications that have been associated with QT prolongation or torsade de pointes may further increase risk.[28674] [60686] [65180] [67452] [72115] [72116] [72117] [72118] Concurrent administration of other medications known to prolong the QT interval and which are metabolized by the CYP3A4 enzyme is contraindicated in individuals receiving fluconazole.[28674] [60686]
Use fluconazole with caution in individuals with hepatic failure. Fluconazole has been associated with rare cases of serious hepatotoxicity, including fatalities primarily in individuals with serious underlying medical conditions. In cases of fluconazole-associated hepatotoxicity, no obvious relationship to total daily dose, duration of therapy, sex, or age of the individual has been observed.[28674] [60686]
Use fluconazole with caution in individuals with renal impairment or renal failure. Fluconazole dose adjustments may be needed in individuals with renal impairment who will receive multiple doses. Fluconazole is cleared primarily by renal excretion as unchanged drug.[28674] [60686]
Avoid the use of fluconazole during pregnancy except in patients with severe or potentially life-threatening fungal infections in whom fluconazole may be used if the potential benefit outweighs the possible risk to the fetus. No adequate and well-controlled studies have been conducted in human pregnancy; however, a few case reports have described a pattern of distinct congenital anomalies in infants exposed in utero to high dose maternal fluconazole (400 to 800 mg/day) during most or all of the first trimester; these effects are similar to those observed in animal studies.[28674] The features observed in fluconazole-exposed infants included brachycephaly, abnormal facies, abnormal calvarial development, cleft palate, femoral bowing, thin ribs and long bones, arthrogryposis, and congenital heart disease. The nature of these birth defects suggests that the teratogenic effect may occur early in the first trimester.[26025] Additionally, retrospective epidemiological studies suggest a potential association between the use of low-dose fluconazole (i.e., 150 mg) and increased risk of birth defects and spontaneous abortions.[60495] [60789] Data from the National Birth Defects Prevention Study found an association between maternal exposure to low-dose fluconazole in the first trimester and both cleft lip with cleft palate and d-transposition of the great arteries. Of the 43,247 mothers analyzed, 44 case mothers and 6 control mothers were identified. The majority of cases (n = 36/50; 72%) reported taking fluconazole for vaginal candidiasis and almost all (n = 49/50) reported taking fluconazole for a short duration. Six exposed infants had cleft lip with cleft palate, 4 had an atrial septal defect, and each of the following defects had 3 exposed cases: hypospadias, tetralogy of Fallot, d-transposition of the great arteries, and pulmonary valve stenosis. Fluconazole use was associated with a significant risk for cleft lip with cleft palate (OR 5.53; 95% CI, 1.68 to 18.24) and d-transposition of the great arteries (OR 7.56; 95% CI, 1.22 to 35.45). The increases for the other conditions were not statistically significant.[60789] A large population-based cohort study of U.S. Medicaid data found oral fluconazole use during the first trimester to be associated with musculoskeletal malformations but not with oral clefts or conotruncal malformations. This cohort included 1,969,954 pregnancies, with 37,650 pregnancies exposed to oral fluconazole and 82,090 exposed to topical azoles during the first trimester. The unadjusted relative risk for musculoskeletal malformations with fluconazole vs. unexposed pregnancies was 1.37 (95% CI, 1.19 to 1.58). When comparing oral fluconazole with topical azoles, the unadjusted relative risk for musculoskeletal malformations was 1.4 (95% CI, 1.17 to 1.67). A subanalysis found a 30% increase in risk for musculoskeletal malformations for cumulative fluconazole doses of 150 to 450 mg and an almost 2-fold increase in risk for cumulative doses more than 450 mg. Malformations were defined as deformities of the skull/face/jaw, feet, and/or spine.[65469] A nationwide Danish cohort study also found an association between maternal exposure to oral fluconazole, including doses used to treat vaginal candidiasis, during gestational weeks 7 through 22 and spontaneous abortions. Specifically, 147 spontaneous abortions were reported among 3,315 fluconazole-exposed pregnancies, as compared to 563 spontaneous abortions among the 13,246 unexposed matched control pregnancies. Of these 147 spontaneous abortions, 132 were reported in pregnancies exposed to a fluconazole dose of 150 to 300 mg (n = 2,986 fluconazole-treated persons). These data indicate a statistically significant increase in risk for spontaneous abortion with maternal exposure to fluconazole during gestational weeks 7 through 22 (HR, 1.48; 95% CI, 1.23 to 1.77).[60495] Topical antifungals, administered for a longer duration in persistent or recurrent infections, are recommended for the treatment of vaginal candidiasis during pregnancy.[60741] Guidelines for the prevention of opportunistic infections in persons living with HIV recommend that oral azole antifungals, including fluconazole, not be started during pregnancy and that these agents should be discontinued in persons who become pregnant.[34362] If fluconazole is administered during pregnancy, or if a patient becomes pregnant while taking fluconazole, advise the patient of the potential hazard to the infant.[28674]
Advise individuals to avoid driving or operating machinery or participating in activities requiring coordination and concentration until they know how fluconazole affects them. Fluconazole can cause dizziness or seizures.[28674] [60686]
Counsel females of childbearing potential who are receiving high dose fluconazole (i.e., 400 to 800 mg/day) about the reproductive risk and contraception requirements during treatment. Advise these patients to use effective contraception during treatment and for approximately 1 week (5 to 6 half-lives) after the final dose.[28674] [60686]
Use caution when fluconazole is administered during breast-feeding.[28674] Previous American Academy of Pediatrics (AAP) recommendations considered fluconazole as usually compatible with breast-feeding.[27500] Fluconazole is distributed in human breast milk at concentrations similar to those in the plasma. A case report found breast milk to plasma ratios of 0.46, 0.85, 0.85, and 0.83 at 2, 5, 24, and 48 hours after a single 150 mg dose of fluconazole.[46093] Experts have estimated, based on limited data of concentrations in breast milk, that an exclusively breast-fed child whose mother was receiving fluconazole 200 mg daily would receive a maximum dose of 0.6 mg/kg/day. This is equivalent to 60% of the recommended dose for thrush in newborns younger than 2 weeks of age and 20% of the recommended dose for older newborns and infants.[46094] Another study determined the daily infant fluconazole dose from breast milk (assuming mean milk consumption of 150 mL/kg/day) based on the mean peak milk concentration (2.61 mcg/mL [range: 1.57 to 3.65 mcg/mL] at 5.2 hours post-dose) to be 0.39 mg/kg/day, which is approximately 13% of the recommended pediatric dose for oropharyngeal candidiasis.[28674] Fluconazole has been used successfully to treat mastitis due to yeast resistant to other therapies in breast-feeding persons.[46095] [46096]
Fluconazole is a fungistatic antifungal agent with concentration-independent activity.[53056] Like other azole antifungals, fluconazole exerts its effect by altering the fungal cell membrane. Fluconazole inhibits ergosterol synthesis by interacting with 14-alpha demethylase, a cytochrome P450 enzyme that is needed to convert lanosterol to ergosterol, an essential component of the membrane. Inhibition of ergosterol synthesis results in increased cellular permeability causing leakage of cellular contents. Fluconazole does not appear to have the same activity on human cholesterol synthesis. Other antifungal effects of azole compounds have been proposed and include inhibition of endogenous respiration, interaction with membrane phospholipids, and inhibition of the transformation of yeasts to mycelial forms. Other mechanisms may involve inhibition of purine uptake and impairment of triglyceride and/or phospholipid biosynthesis.[23613][23649]
The Clinical and Laboratory Standards Institute (CLSI) defines minimum inhibitory concentrations (MICs) for C. albicans, C. parapsilosis, and C. tropicalis as susceptible at 2 mcg/mL or less, susceptible dose-dependent (SDD) at 4 mcg/mL, and resistant at 8 mcg/mL or more. For C. glabrata, isolates are defined as SDD at 32 mcg/mL or less and resistant at 64 mcg/mL or more. C. krusei is considered intrinsically resistant to fluconazole.[28674][60487][69089]
The emergence of fungal organisms resistant to fluconazole, especially Candida species, is problematic. Increased frequency of non-Candida albicans species as causes of fungemia has been correlated in epidemiologic studies with the increased use of fluconazole both for prophylaxis and treatment. These non-Candida albicans species are often more resistant to fluconazole. Data indicate the annual incidence of fluconazole-resistant oropharyngeal candidiasis in persons with AIDS is roughly 5%. Consider susceptibility testing of invasive C. albicans isolates for persons with persistent candidemia or progressive disseminated candidiasis, despite fluconazole therapy, and on non-Candidaalbicans isolates (e.g., C. glabrata, C. tropicalis, or C. parapsilosis) from persons with candidemia or invasive disease.[26488]
Revision Date: 10/15/2025, 01:33:00 AMFluconazole is administered orally and intravenously. The pharmacokinetics of both IV and oral fluconazole are similar. Peak serum concentrations and AUC increase in proportion to the dose. Steady-state fluconazole plasma concentrations are achieved within 5 to 10 days at doses within the adult dosage range of 50 to 400 mg/day, and within 2 days when a loading dose of twice the usual daily dosage is given on the first day of therapy. Fluconazole is widely distributed into body tissues and fluids; the apparent volume of distribution approximates that of total body water. Saliva, sputum, nail, blister, and vaginal tissue concentrations are approximately equal to plasma concentrations. Urine and skin concentrations are approximately 10 times that of plasma concentrations. Fluconazole distributes well into the CSF, and achieves CSF concentrations that are 50% to 90% of plasma concentrations, regardless of the degree of meningeal inflammation. Plasma protein binding is low and ranges from 11% to 12%. Fluconazole does not appear to undergo first-pass metabolism. Elimination is mainly renal; about 65% to 80% of a dose is excreted in the urine unchanged and 11% as metabolites. A clearance of approximately 0.23 mL/kg/minute has been reported for adults. Small amounts of fluconazole are excreted in the feces. Plasma elimination half-life in adults with normal renal function is approximately 30 hours (range: 20 to 50 hours).[28674][52683][53005]
Affected cytochrome P450 isoenzymes and drug transporters: CYP2C9, CYP2C19, CYP3A4, UGT2B7
Fluconazole potently inhibits CYP2C19 and moderately inhibits CYP2C9 and CYP3A4. The extent of CYP3A4 inhibition is less than with ketoconazole or itraconazole.[28674][29036][34447] In vitro studies have also shown fluconazole to be a concentration-dependent inhibitor of uridine diphosphoglucuronosyltransferase UGT2B7.[60255][60256]
Fluconazole is well absorbed after oral administration with a bioavailability of approximately 90%. Peak concentrations are reached approximately 1 to 2 hours after administration. Food does not affect the absorption. Bioequivalence has been established between the suspension and tablet formulations.[28674]
Peak concentrations are reached approximately 1 to 2 hours after administration.[60686]
Fluconazole clearance is significantly reduced in patients with renal impairment. A 3-hour hemodialysis session reduces plasma concentrations by approximately 50%.[28674] In a study in 17 children with renal impairment, the elimination half-life of fluconazole was approximately 72 hours in patients requiring peritoneal dialysis (PD) compared with approximately 31 hours in children in the non-PD group (mild renal impairment; mean CrCl 26 mL/minute/1.73 m2).[53009]
Infants, Children, and Adolescents 3 months to 17 years
The clearance of fluconazole is greater in pediatric patients compared to adults. A clearance and elimination half-life of approximately 0.4 to 0.66 mL/kg/minute and 15 to 25 hours, respectively, have been reported in pediatric patients 9 months and older.[28674] Volume of distribution is also greater in children compared with adults. A mean volume of distribution of 0.95 L/kg and 0.7 L/kg has been reported for children and adolescents, respectively. The value in adolescents is similar to what has been reported in adults.[28674][53005][53007][53011]
Neonates and Infants 1 to 2 months
Clearance of fluconazole is prolonged in neonates and young infants compared with children and adults and increases with postnatal age (PNA). In a pharmacokinetic study in premature neonates (gestational age (GA) 26 to 29 weeks), mean total clearance corrected for weight was 0.18 mL/minute/kg (n = 7), 0.33 mL/minute/kg (n = 7), and 0.52 mL/minute/kg (n = 4) at postnatal ages 1 day, 7 days, and 13 days, respectively. Corresponding mean elimination half-lives were 88.6 hours, 67.5 hours, and 55.2 hours, respectively.[32700] In another study in 8 neonates and young infants (GA 35 to 38 weeks; PNA 6 to 59 days), the mean clearance and elimination half-life were 0.29 mL/minute/kg and 54.2 hours, respectively.[28674][53037] Volume of distribution of fluconazole is also greatest in the neonatal period, with values of approximately 1 to 2.25 L/kg reported.[32700][53007][53010][53037] Because of the large volume of distribution and slow elimination, the use of a loading dose on day 1 of therapy is recommended to achieve therapeutic serum concentrations faster. In a study of 13 premature and term patients (median GA of 37 weeks, range: 24 to 39 weeks; median PNA 19 days, range: 5 to 262 days), of the 12 patients who received a 25 mg/kg loading dose, 9 patients achieved an AUC0-24 of more than 400 mg x hour/L in the first 24 hours. A population pharmacokinetic model using data from 55 pediatric patients (GA 23 to 40 weeks, PNA 1 to 88 days) found that a loading dose of 25 mg/kg is necessary to reach target AUC more than 400 mg x hour/L within 24 hours of initiating therapy in patients younger than 3 months.[28674] Additionally, data from a population pharmacokinetic study using Monte Carlo simulations of premature and term neonates revealed that a dose of at least 12 mg/kg/day is necessary to achieve target exposure (AUC/MIC of 50 or more for Candida species with an MIC of 8 mcg/mL or less) in 90% of neonates younger than 30 weeks gestation and 80% of neonates 30 to 40 weeks gestation.[53038] A maintenance dose of 9 mg/kg once daily is recommended in neonates younger than 30 weeks GA and 12 mg/kg once daily is recommended in neonates 30 weeks GA and older.[28674]
Pediatric Patients Receiving Extracorporeal Membrane Oxygenation (ECMO)
A population PK model using data from 21 pediatric patients ages from birth to 17 years supported with ECMO and 19 pediatric non-ECMO patients ages from birth to 2 years found that clearance was related to serum creatinine, while a higher volume of distribution was related to presence of ECMO support. The median volume of distribution was 1.3 L/kg in pediatric patients on ECMO and 0.9 L/kg in those not on ECMO. Simulations suggested that a loading dose of 35 mg/kg is needed to achieve the target AUC0-24 more than 400 mg x hour/L within the first 24 hours in pediatric patients on ECMO.[28674]
Elimination of fluconazole can be impaired in older adults due to expected decrease in renal function. In older adult patients receiving single 50 mg PO doses of fluconazole, the Cmax and AUC of fluconazole were higher than those reported in normal young male volunteers; the mean terminal half-life was 46.2 hours in older adults vs. 30 hours in younger patients. Coadministration with diuretics did not significantly alter the AUC or Cmax of fluconazole. Older adult patients had lower creatinine clearance, lower percentage of drug recovered in urine, and lower fluconazole renal clearance estimates compared to younger volunteers.[28674]
Avoid the use of fluconazole during pregnancy except in patients with severe or potentially life-threatening fungal infections in whom fluconazole may be used if the potential benefit outweighs the possible risk to the fetus. No adequate and well-controlled studies have been conducted in human pregnancy; however, a few case reports have described a pattern of distinct congenital anomalies in infants exposed in utero to high dose maternal fluconazole (400 to 800 mg/day) during most or all of the first trimester; these effects are similar to those observed in animal studies.[28674] The features observed in fluconazole-exposed infants included brachycephaly, abnormal facies, abnormal calvarial development, cleft palate, femoral bowing, thin ribs and long bones, arthrogryposis, and congenital heart disease. The nature of these birth defects suggests that the teratogenic effect may occur early in the first trimester.[26025] Additionally, retrospective epidemiological studies suggest a potential association between the use of low-dose fluconazole (i.e., 150 mg) and increased risk of birth defects and spontaneous abortions.[60495] [60789] Data from the National Birth Defects Prevention Study found an association between maternal exposure to low-dose fluconazole in the first trimester and both cleft lip with cleft palate and d-transposition of the great arteries. Of the 43,247 mothers analyzed, 44 case mothers and 6 control mothers were identified. The majority of cases (n = 36/50; 72%) reported taking fluconazole for vaginal candidiasis and almost all (n = 49/50) reported taking fluconazole for a short duration. Six exposed infants had cleft lip with cleft palate, 4 had an atrial septal defect, and each of the following defects had 3 exposed cases: hypospadias, tetralogy of Fallot, d-transposition of the great arteries, and pulmonary valve stenosis. Fluconazole use was associated with a significant risk for cleft lip with cleft palate (OR 5.53; 95% CI, 1.68 to 18.24) and d-transposition of the great arteries (OR 7.56; 95% CI, 1.22 to 35.45). The increases for the other conditions were not statistically significant.[60789] A large population-based cohort study of U.S. Medicaid data found oral fluconazole use during the first trimester to be associated with musculoskeletal malformations but not with oral clefts or conotruncal malformations. This cohort included 1,969,954 pregnancies, with 37,650 pregnancies exposed to oral fluconazole and 82,090 exposed to topical azoles during the first trimester. The unadjusted relative risk for musculoskeletal malformations with fluconazole vs. unexposed pregnancies was 1.37 (95% CI, 1.19 to 1.58). When comparing oral fluconazole with topical azoles, the unadjusted relative risk for musculoskeletal malformations was 1.4 (95% CI, 1.17 to 1.67). A subanalysis found a 30% increase in risk for musculoskeletal malformations for cumulative fluconazole doses of 150 to 450 mg and an almost 2-fold increase in risk for cumulative doses more than 450 mg. Malformations were defined as deformities of the skull/face/jaw, feet, and/or spine.[65469] A nationwide Danish cohort study also found an association between maternal exposure to oral fluconazole, including doses used to treat vaginal candidiasis, during gestational weeks 7 through 22 and spontaneous abortions. Specifically, 147 spontaneous abortions were reported among 3,315 fluconazole-exposed pregnancies, as compared to 563 spontaneous abortions among the 13,246 unexposed matched control pregnancies. Of these 147 spontaneous abortions, 132 were reported in pregnancies exposed to a fluconazole dose of 150 to 300 mg (n = 2,986 fluconazole-treated persons). These data indicate a statistically significant increase in risk for spontaneous abortion with maternal exposure to fluconazole during gestational weeks 7 through 22 (HR, 1.48; 95% CI, 1.23 to 1.77).[60495] Topical antifungals, administered for a longer duration in persistent or recurrent infections, are recommended for the treatment of vaginal candidiasis during pregnancy.[60741] Guidelines for the prevention of opportunistic infections in persons living with HIV recommend that oral azole antifungals, including fluconazole, not be started during pregnancy and that these agents should be discontinued in persons who become pregnant.[34362] If fluconazole is administered during pregnancy, or if a patient becomes pregnant while taking fluconazole, advise the patient of the potential hazard to the infant.[28674]
Use caution when fluconazole is administered during breast-feeding.[28674] Previous American Academy of Pediatrics (AAP) recommendations considered fluconazole as usually compatible with breast-feeding.[27500] Fluconazole is distributed in human breast milk at concentrations similar to those in the plasma. A case report found breast milk to plasma ratios of 0.46, 0.85, 0.85, and 0.83 at 2, 5, 24, and 48 hours after a single 150 mg dose of fluconazole.[46093] Experts have estimated, based on limited data of concentrations in breast milk, that an exclusively breast-fed child whose mother was receiving fluconazole 200 mg daily would receive a maximum dose of 0.6 mg/kg/day. This is equivalent to 60% of the recommended dose for thrush in newborns younger than 2 weeks of age and 20% of the recommended dose for older newborns and infants.[46094] Another study determined the daily infant fluconazole dose from breast milk (assuming mean milk consumption of 150 mL/kg/day) based on the mean peak milk concentration (2.61 mcg/mL [range: 1.57 to 3.65 mcg/mL] at 5.2 hours post-dose) to be 0.39 mg/kg/day, which is approximately 13% of the recommended pediatric dose for oropharyngeal candidiasis.[28674] Fluconazole has been used successfully to treat mastitis due to yeast resistant to other therapies in breast-feeding persons.[46095] [46096]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.