ThisiscontentfromElsevier'sDrugInformation
Fludrocortisone
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
0.05 to 0.1 mg PO once daily, initially, in combination with another glucocorticoid. Adjust dose based on clinical response (e.g., edema, postural hypotension, salt craving, serum electrolytes) and tolerability. Dose range: 0.05 to 0.2 mg/day. Guidelines recommend mineralocorticoid replacement in all individuals with confirmed aldosterone deficiency.[66494] The FDA-approved dosage is 0.1 mg PO once daily, initially, in combination with another glucocorticoid, preferably cortisone or hydrocortisone. Reduce dose to 0.05 mg PO once daily if transient hypertension develops. Dose range: 0.1 mg PO 3 times/week to 0.2 mg PO once daily.[49507]
0.05 mg PO twice daily, initially, in combination with another glucocorticoid. Adjust dose based on clinical response (e.g., blood pressure, growth, plasma renin activity, serum electrolytes, symptoms of salt cravings, weight gain) and tolerability. Dose range: 0.05 to 0.2 mg/day in 2 divided doses. Guidelines recommend mineralocorticoid replacement in all individuals with confirmed aldosterone deficiency.[66494] [72009]
0.05 mg PO twice daily, initially, in combination with another glucocorticoid. Adjust dose based on clinical response (e.g., blood pressure, growth, plasma renin activity, serum electrolytes, symptoms of salt cravings, weight gain) and tolerability. Dose range: 0.05 to 0.2 mg/day in 2 divided doses. Guidelines recommend mineralocorticoid replacement in all individuals with confirmed aldosterone deficiency. Concurrent administration of sodium chloride supplements is recommended until salt intake from diet is sufficient, usually around the age of 8 to 12 months.[66494] [72009]
0.05 mg PO twice daily, initially, in combination with another glucocorticoid. Adjust dose based on clinical response (e.g., blood pressure, growth, plasma renin activity, serum electrolytes, symptoms of salt cravings, weight gain) and tolerability. Dose range: 0.05 to 0.2 mg/day in 2 divided doses. Guidelines recommend mineralocorticoid replacement in all individuals with confirmed aldosterone deficiency. Concurrent administration of sodium chloride supplements is recommended until salt intake from diet is sufficient, usually around the age of 8 to 12 months.[66494] [72009]
0.05 to 0.2 mg/day PO in 1 or 2 divided doses in combination with another glucocorticosteroid. Adjust dose based on clinical response (e.g., edema, postural hypotension, salt craving, serum electrolytes) and tolerability. Usual dose: 0.1 mg/day.[54123] [71840] The FDA-approved dosage is 0.1 mg PO once daily, initially, in combination with another glucocorticoid, preferably cortisone or hydrocortisone. Reduce dose to 0.05 mg PO once daily if transient hypertension develops. Dose range: 0.1 mg PO 3 times/week to 0.2 mg PO once daily.[49507]
0.01 to 0.2 mg/day PO in 1 or 2 divided doses in combination with another glucocorticosteroid. Adjust dose based on clinical response (e.g., blood pressure, growth, plasma renin activity, serum electrolytes, symptoms of salt cravings, weight gain) and tolerability. Infants may need higher dosing during the first 6 months due to mineralocorticoid resistance. Concurrent administration of sodium chloride supplements is recommended until salt intake from diet is sufficient, usually around the age of 8 to 12 months.[54123] [66494] [71840] [72009]
0.01 to 0.2 mg/day PO in 1 or 2 divided doses in combination with another glucocorticosteroid. Adjust dose based on clinical response (e.g., blood pressure, growth, plasma renin activity, serum electrolytes, symptoms of salt cravings, weight gain) and tolerability. Concurrent administration of sodium chloride supplements is recommended.[54123] [66494] [71840] [72009]
0.1 to 0.2 mg PO once daily.[49507]
0.05 or 0.1 mg PO once daily, initially. May increase the dose as needed based on clinical response and tolerability. Max: 0.2 mg/day. Doses higher than 0.2 mg/day do not improve therapeutic effect.[32679] [32680] [65824] [65825] [66385] [68047] [68048] [68049]
0.1 mg PO once daily, or alternatively, 0.3 mg PO once daily for 7 days, then 0.1 mg PO once daily. May increase the dose as needed based on clinical response and tolerability. Max: 0.2 mg/day.[65825] [71794] [71795]
0.1 mg PO 3 times daily or 0.2 mg PO twice daily for up to 12 days.[58117] [68526] [68527] [68528]
0.1 mg PO once daily, initially. Increase the dose after 5 to 14 days to 0.2 mg PO once daily. Adjust dose based on clinical response and tolerability. Dose range: 0.05 to 0.2 mg/day.[65824] [65825] [71784]
0.1 mg PO once daily, initially. Increase the dose after 5 to 14 days to 0.2 mg PO once daily. Adjust dose based on clinical response and tolerability. Dose range: 0.05 to 0.2 mg/day.[65824] [65825] [71784]
Maintenance therapy usual max: 0.2 mg/day PO.
Maintenance therapy usual max: 0.2 mg/day PO.
Safety and efficacy have not been established, but doses of up to 0.3 mg/day PO have been used.
Safety and efficacy have not been established, but doses of up to 0.3 mg/day PO have been used.
Safety and efficacy have not been established, but doses of up to 0.3 mg/day PO have been used.
Safety and efficacy have not been established, but doses of up to 0.3 mg/day PO have been used.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication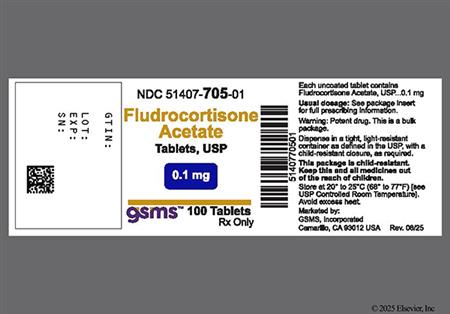


Fludrocortisone is an oral synthetic adrenocortical steroid derived from the substitution of a 9alpha-fluoride on the B ring of hydrocortisone. Fluorination at this position gives rise to potent mineralocorticoid activity. Pharmacologic actions are similar to those of aldosterone, an endogenous mineralocorticoid. The sodium-retaining activity of fludrocortisone is extremely high compared with other adrenocorticoids such as hydrocortisone. Although fludrocortisone has significant glucocorticoid activity, it has no appreciable glucocorticoid effects at usual therapeutic doses. Fludrocortisone is used as mineralocorticoid replacement therapy in patients with adrenocortical insufficiency and salt-losing adrenogenital syndrome. Fludrocortisone was approved by the FDA in 1954.
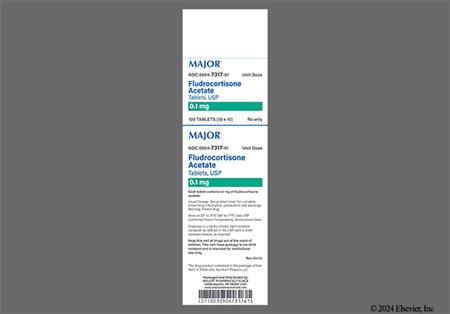
For storage information, see the specific product information within the How Supplied section.
May be administered without regard to meals; however, administer with meals to minimize GI upset.
Fludrocortisone has potent mineralocorticoid properties and as a result, most adverse reactions are due to its mineralocorticoid activity. These adverse effects include fluid imbalance, electrolyte imbalance (particularly hypokalemia), edema, congestive heart failure, cardiomegaly, and hypertension. A fludrocortisone dosage adjustment is recommended if hypertension develops during fludrocortisone therapy in combination with a glucocorticoid for Addison's disease. Hypertension, weight gain, edema, hypokalemia, heart size increase, sinus tachycardia, and suppressed plasma renin activity are clinical signs of overdosage with mineralocorticoids. If the above signs are noted, discontinue fludrocortisone. The symptoms will usually subside within several days; use a reduced fludrocortisone dose for subsequent treatment. To help prevent overdosage, regularly monitor blood pressure and serum electrolytes. A hypokalemic metabolic alkalosis syndrome can also be associated with fludrocortisone therapy and includes nausea and vomiting, orthostatic hypotension, QT prolongation, ST-T wave changes, severe weakness of the extremities, anorexia, and muscle cramps and pain.[49507]
Corticosteroids, like fludrocortisone, have been reported to cause pseudotumor cerebri (increased intracranial pressure) causing papilledema, oculomotor or abducens nerve paralysis, loss of vision, and headache.
Glucocorticoid side effects of fludrocortisone may occur when the drug is used over a prolonged period of time or in conjunction with a glucocorticoid. Corticosteroid therapy, including fludrocortisone, can mask the symptoms of infection and should be avoided during an acute viral, fungal, or bacterial infection. Neutropenia including febrile neutropenia has been reported by recipients of corticosteroids. Immunosuppression is most likely to occur in patients receiving high-dose (e.g., equivalent to 1 mg/kg or more of prednisone daily), systemic corticosteroid therapy for any period of time, particularly in conjunction with corticosteroid sparing drugs (e.g., troleandomycin) and/or concomitant immunosuppressant agents; however, patients receiving moderate dosages of systemic corticosteroids for short periods or low dosages for prolonged periods also may be at risk. Corticosteroids can reactivate tuberculosis and should not be used in patients with a history of active tuberculosis except when chemoprophylaxis is instituted concomitantly. Patients receiving immunosuppressive doses of corticosteroids should be advised to avoid exposure to measles or varicella (chickenpox) and, if exposed to these diseases, to seek medical advice immediately. Monitoring systemic corticosteroid recipients for signs of an opportunistic fungal infection is recommended, as cases of oropharyngeal candidiasis have been reported. Development of Kaposi's sarcoma has also been associated with prolonged administration of corticosteroids. Discontinuation of the corticosteroid may result in clinical improvement.[43319]
Glucocorticoid side effects of fludrocortisone may occur when the drug is used over a prolonged period of time or in conjunction with a glucocorticoid. Ocular effects such as corneal perforation, exophthalmos, posterior subcapsular cataracts, retinopathy, or ocular hypertension, can result from prolonged use of glucocorticoids and could result in glaucoma or ocular nerve damage including optic neuritis. Temporary or permanent visual impairment, including blurred vision and blindness, has been reported with glucocorticoid administration by several routes of administration. Secondary fungal and viral infections of the eye (ocular infection) can be exacerbated by corticosteroid therapy.[49507]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Fludrocortisone increases sodium retention and has the potential to cause edema and other related effects. It should be used with caution in individuals needing sodium restriction, such as those with cardiac disease, congestive heart failure, hypertension, renal impairment, or renal failure. Since fludrocortisone acetate is a potent mineralocorticoid compared to other corticosteroids, both the dosage and the individual's salt intake should be carefully monitored in order to avoid the development of hypertension, edema or weight gain. Periodic monitoring of serum electrolyte concentrations is advised during prolonged therapy; dietary salt restriction and potassium supplementation may be necessary.[49507]
Systemic corticosteroids, including fludrocortisone, may cause dose-dependent immunosuppression and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids may mask symptoms and increase the risk of severe or fatal infectious complications, requiring close monitoring and potential dose adjustment or withdrawal. Systemic fludrocortisone and other corticosteroids may cause severe or fatal infections by reactivating or worsening TB, hepatitis B, amebiasis, Strongyloides, varicella, measles, herpes simplex, and other viral or herpes infections. Avoid using corticosteroids in individuals with cerebral malaria. Screen for hepatitis B before prolonged immunosuppressive therapy; consult specialists and consider antiviral prophylaxis if infection is present. Rule out latent amebiasis in individuals with tropical exposure or unexplained diarrhea. Use caution in individuals with known or suspected Strongyloides infection; prophylactic therapy may be indicated. Fludrocortisone is contraindicated in individuals with systemic fungal infection. Corticosteroids should be used with caution, if at all, in individuals with ocular herpes simplex. Avoid exposing nonimmune corticosteroid-treated individuals to varicella or measles. If exposure occurs, prophylaxis with varicella zoster immune globulin (VZIG) for varicella or immunoglobulin (IG) for measles may be needed. If infection develops, consider antiviral treatment.[49507]
Systemic corticosteroids, such as fludrocortisone, may decrease glucose tolerance, produce hyperglycemia, and aggravate or precipitate diabetes mellitus. This may especially occur in those predisposed to diabetes mellitus. When corticosteroid therapy is necessary in people with diabetes mellitus, changes in insulin, oral antidiabetic agent dosage, and/or diet may be required. Metabolic clearance of systemic corticosteroids is decreased in hypothyroidism and increased in hyperthyroidism. There is an enhanced effect of corticosteroids in people with hypothyroidism. Changes in thyroid disease status may necessitate adjustment in fludrocortisone dosage.[49507]
Systemic corticosteroid use may be associated with neuro-psychiatric effects ranging from euphoria, insomnia, mood swings, personality changes, and severe depression, to frank psychosis. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids, such as in individuals with a mood disorder or psychotic disorder. Inform individuals or caregivers of the potential for mood and behavioral changes with fludrocortisone treatment and encourage them to seek medical attention if psychiatric symptoms develop, especially if depressed mood (depression) or suicidal ideation is suspected.[49507]
Use fludrocortisone with caution in myasthenia gravis. Acute myopathy has been observed in association with high doses of corticosteroids in individuals with disorders of neuromuscular transmission, including myasthenia gravis. The acute myopathy was generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Creatinine kinase levels may be elevated. Recovery may take weeks to years after stopping corticosteroids.[49507]
Corticosteroids decrease bone formation and increase bone resorption both through their effect on calcium regulation (e.g., decreasing absorption and increasing excretion) and inhibition of osteoblast function. This, together with a decrease in the protein matrix of the bone secondary to an increase in protein catabolism, and reduced sex hormone production, may lead to the development of osteopenia and osteoporosis at any age. Use fludrocortisone with caution in individuals with osteoporosis. Special consideration should be given to individuals at increased risk for osteoporosis (e.g., postmenopausal females) before initiating corticosteroid therapy.[49507]
According to the Beers Criteria, systemic corticosteroids are considered potentially inappropriate medications (PIMs) for use in geriatric patients with delirium or at high risk for delirium and should be avoided in these patient populations due to the possibility of new-onset delirium or exacerbation of the current condition. The Beers expert panel recommends that fludrocortisone be prescribed in the lowest effective dose and for the shortest possible duration consistent with the needs of the patient.[63923]
Corticosteroids like fludrocortisone should be used with caution in patients with nonspecific ulcerative colitis if there is a probability of impending GI perforation, GI abscess, or other pyogenic infection. Corticosteroids should also be used cautiously in patients with diverticulitis, fresh intestinal anastomosis, or active or latent peptic ulcer disease.[49507]
Fludrocortisone is classified as FDA pregnancy risk category C.[49507] Studies involving use of fludrocortisone in pregnancy have not been done in humans. Complications, including cleft palate, still birth, and premature abortion, have been reported when corticosteroids were administered during pregnancy. Fludrocortisone acetate should be given to a pregnant woman only if clearly needed. If these drugs must be used during pregnancy, the potential risks should be discussed with the patient. The mother may require additional monitoring to ensure adequate replacement during pregnancy; insufficient treatment of Addison's disease during pregnancy is associated with fetal risks. The usual treatments for Addison's disease are usually continued throughout pregnancy and post-partum, and the mother may require dosage adjustments for proper replacement post-partum as requirements return to pre-pregnancy levels. Infants born to mothers who have taken substantial doses of corticosteroids during pregnancy should be monitored for signs of hypoadrenalism. In addition, maternal treatment with corticosteroids should be carefully documented in the infant's medical records to assist in follow-up.[49507]
Use fludrocortisone with caution in individuals with hepatic cirrhosis; there is an enhanced effect due to decreased metabolism of corticosteroids in these individuals.[49507]
Corticosteroids distribute into breast milk. Because of the risk of hypoadrenalism in the infant, or other potential adverse effects, fludrocortisone should be used cautiously during breast-feeding.[49507]
Endogenous corticosteroids are secreted by the adrenal cortex; their effects are believed to be due to modification of enzymatic activity rather than to a direct hormone-induced action. Fludrocortisone mimics the actions of aldosterone, an endogenous mineralocorticoid. Mineralocorticoids facilitate sodium resorption and promote hydrogen ion and potassium excretion at the level of the distal renal tubule. Small oral doses produce marked sodium retention and increased urinary potassium excretion. Among 5 adults with orthostatic hypotension who took fludrocortisone 0.3—1 mg/day for 10—14 days, the change in sodium balance ranged from +149 mmol to +282 mmol, and the change in plasma volume ranged from 185 ml to 299 mL. The mean recumbent blood pressure increased from 110 +/-6 over 69 +/-3 mmHg to 124 +/-7 over 79 +/-2 mmHg. Although fludrocortisone receipt tended to decrease the signs and symptoms of severe orthostatic hypotension, only incomplete symptomatic relief was obtained in each patient.[32776] Larger doses can inhibit endogenous adrenal cortical secretion, thymic activity, and pituitary corticotropin excretion; promote the deposition of liver glycogen; and, if protein intake is inadequate, induce negative nitrogen balance.
Fludrocortisone receipt (0.2—1 mg/day) for at least a year led to recumbent and standing blood pressure increases in all 7 adults with severe orthostatic hypotension; 5 had idiopathic disease and 2 had orthostatic hypotension associated with diabetes. Average systolic blood pressure values were at least 20 mmHg higher and average diastolic blood pressure values were at least 10 mmHg higher as compared with values before fludrocortisone receipt. Hypertensive retinopathy developed in 2 patients; one of the 2 patients also had x-ray evidence of cardiomegaly and electrocardiographic changes consistent with left ventricular hypertrophy. Although plasma volume increased over the first 10 days of fludrocortisone receipt, the plasma volume decreased to control levels despite further blood pressure increases. Treatment did not affect plasma catecholamines concentrations and did not enhance pressor response to infused norepinephrine in 5 patients who had hyperreactive blood pressure responses to norepinephrine before fludrocortisone receipt. An enhanced pressor response to infused norepinephrine occurred in 2 patients who showed normal blood pressure responses to norepinephrine before fludrocortisone receipt. Hemodynamic data were obtained from 2 patients; hypertension in the recumbent position was related to increases in total peripheral vascular resistance - no appreciable change in either cardiac output or plasma volume was noted.[32776]
Revision Date: 10/13/2025, 08:37:52 AMFludrocortisone is administered orally. The circulating drug binds extensively to the plasma proteins albumin and transcortin, and only the unbound portion of a dose is active. Systemic fludrocortisone is quickly distributed into the kidneys, intestines, skin, liver, and muscle. Fludrocortisone distributes into breast milk and crosses the placenta. Fludrocortisone is metabolized by the liver to inactive metabolites. These inactive metabolites, as well as a small portion of unchanged drug, are excreted in the urine. The biological half-life of fludrocortisone is 18—36 hours.
Fludrocortisone is absorbed rapidly from the GI tract. Peak plasma concentrations are reached within 1.5 hours.
Fludrocortisone is classified as FDA pregnancy risk category C.[49507] Studies involving use of fludrocortisone in pregnancy have not been done in humans. Complications, including cleft palate, still birth, and premature abortion, have been reported when corticosteroids were administered during pregnancy. Fludrocortisone acetate should be given to a pregnant woman only if clearly needed. If these drugs must be used during pregnancy, the potential risks should be discussed with the patient. The mother may require additional monitoring to ensure adequate replacement during pregnancy; insufficient treatment of Addison's disease during pregnancy is associated with fetal risks. The usual treatments for Addison's disease are usually continued throughout pregnancy and post-partum, and the mother may require dosage adjustments for proper replacement post-partum as requirements return to pre-pregnancy levels. Infants born to mothers who have taken substantial doses of corticosteroids during pregnancy should be monitored for signs of hypoadrenalism. In addition, maternal treatment with corticosteroids should be carefully documented in the infant's medical records to assist in follow-up.[49507]
Corticosteroids distribute into breast milk. Because of the risk of hypoadrenalism in the infant, or other potential adverse effects, fludrocortisone should be used cautiously during breast-feeding.[49507]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.