ThisiscontentfromElsevier'sDrugInformation
Fluorouracil, 5-FU
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
NOTE: Dosage should be based upon body surface area using actual body weight unless patient is obese or has significant fluid retention. In these cases the dose should be based upon the ideal weight or dry weight.
NOTE: Fluorouracil has been given in a large number of different dosages and schedules. The correct dose of fluorouracil will vary from protocol to protocol. Clinicians should consult the appropriate references to verify the dose.
500 mg/m2 IV bolus daily for 5 days on days 1 and 36 beginning 22 to 70 days after surgery; radiation therapy for 6 weeks is begun on day 64 after initiation of 5-FU therapy. 5-FU 225 mg/m2/day IV continuous infusion is given throughout radiation therapy. Then, 5-FU 450 mg/m2 IV bolus daily for 5 days beginning 1 month after radiation (i.e., days 134 to 138) and repeated in 4 weeks (i.e., days 169 to 173). As compared to patients who received bolus injection 5-FU during radiation therapy (5-FU 350 mg/m2/day IV bolus on days 1 to 5; 400 mg/m2 IV bolus on days 36 to 40; 300 mg/m2 IV bolus on days 134 to 138; and 350 mg/m2 IV bolus on days 169 to 173 with radiation therapy beginning on day 64), patients receiving the continuous infusion during radiation therapy had a statistically significant improvement in relapse-free and overall survival rates.[26301]
370 mg/m2 to 420 mg/m2 IV push on days 1, 2, 3, 4, and 5; precede 5-FU administration by leucovorin 20 mg/m2 to 25 mg/m2 IV push on days 1, 2, 3, 4, and 5. Repeat at week 4, week 8, and then every 5 weeks for a total of 6 courses of therapy. In a randomized clinical trial, patients with stage II or III colon cancer post-curative resection received treatment with weekly 5-FU either in combination with low dose leucovorin (Mayo Clinic regimen; n = 984), high dose leucovorin (Roswell Park regimen; n = 981), or levamisole (n = 871). There were no clinically significant differences in 10-year overall survival (OS) (52% vs. 52% vs. 50%) or 10-year disease-free survival (DFS) (49% vs. 47% vs. 45%). Grade 3 or 4 toxicities were reported in 55.6% of those who received the Mayo Clinic regimen, 40.3% of patients treated with Roswell Park, and 44.4% of patients treated with levamisole plus 5-FU.[47421] In a separate study, patients randomized to adjuvant treatment with the Mayo Clinic regimen (n = 158) had improved 5-year relapse-free survival (74% vs. 58%; p = 0.004) and 5-year OS (74% vs. 63%; p = 0.02).[47418]
500 mg/m2 IV bolus on day 1; 1 hour prior to administering 5-FU bolus, give leucovorin 500 mg/m2 IV over 2 hours. Repeat weekly on days 1, 8, 15, 22, 29, and 36 every 8 weeks for 4 to 6 cycles. In a randomized clinical trial, patients with stage II or III colon cancer post-curative resection received treatment with weekly 5-FU either in combination with high dose leucovorin (Roswell Park regimen; n = 981), low dose leucovorin (Mayo Clinic regimen; n = 984), or levamisole (n = 871). There were no clinically significant differences in 10-year overall survival (OS) (52% vs. 52% vs. 50%) or 10-year disease-free survival (DFS) (47% vs. 49% vs. 45%). Grade 3 or 4 toxicities were reported in 40.3% of patients treated with Roswell Park, 55.6% of those who received the Mayo Clinic regimen, and 44.4% of patients treated with levamisole plus 5-FU.[47421] In a separate clinical trial, patients randomized to receive adjuvant treatment with the Roswell Park regimen (n = 519) had improved 3-year DFS (73% vs. 64%; p = 0.0004) and 3-year OS (84% vs. 77%; p = 0.003) compared with those treated with MOF (lomustine, vincristine, 5-FU) (n = 522).[59866]
500 mg/m2 IV bolus on days 1, 8, 15, 22, 29, and 36, preceded on days 1, 15, and 29 by leucovorin 500 mg/m2 IV given concurrently via y-site over 2 hours with oxaliplatin 85 mg/m2 IV. On days 8, 22, and 36, give leucovorin 500 mg/m2 IV over 2 hours alone (without oxaliplatin) prior to 5-FU. The leucovorin infusion should be complete 1 hour prior to administration of 5-FU. Repeat every 8 weeks (56 days) for a total of 3 cycles (24 weeks). After a median 8 years of follow-up, patients with stage II or III colon cancer treated with FLOX (n = 1,247) had significantly improved disease-free survival (DFS) compared with those who received 5-FU/leucovorin alone (FULV; n = 1,245) (HR 0.82; 95% CI, 0.72 to 0.93; p = 0.002) in a randomized, phase III clinical trial. Overall survival was similar between treatment groups (HR 0.88; 95% CI, 0.75 to 1.02; p = 0.08); however, in an unplanned subgroup analysis, age < 70 years may be associated with improved survival (HR 0.8; 95% CI, 0.68 to 0.95; p = 0.013).[59877][59899]
400 mg/m2 IV bolus over 2 to 4 minutes, followed by 5-FU 600 mg/m2 continuous IV infusion (CIV) over 22 hours on day 1 ; precede 5-FU bolus and CIV by oxaliplatin 85 mg/m2 IV, administered concurrently over 2 hours in separate bags via Y-site with leucovorin 200 mg/m2 IV. On day 2, again give leucovorin 200 mg/m2 IV over 2 hours prior to a 5-FU bolus (600 mg/m2 IV) and CIV (600 mg/m2 IV over 22 hours). This 2-day regimen (FOLFOX4) is repeated every 2 weeks for 12 cycles (6 months). Prolongation of the oxaliplatin infusion to 6 hours may mitigate acute toxicities; the infusion time for 5-FU and leucovorin need not be changed. In a multicenter trial, 2,246 patients with stage II or III completely resected colon cancer were randomized to either FOLFOX 4 or infusional 5-FU/LV (De Gramont regimen). At a median follow-up of 81.9 months in the patients with stage III disease, there was a significant improvement in 5-year disease-free survival (DFS) in patients receiving FOLFOX 4 as compared to those receiving infusional 5-FU/LV (73.3% vs. 67.4%; HR 0.80; p = 0.003). The 6-year overall survival (OS) rates were also improved with FOLFOX 4 (78.5% vs. 76%;HR 0.84; p = 0.46). In a subgroup analysis of stage III patients, the 6-year OS rates were improved with FOLFOX 4 (72.9% vs. 68.7%; HR 0.80; p = 0.023). There was no significant difference observed in DFS or OS in patients with stage II disease.[41958] [40864] [20587]
400 mg/m2 IV bolus on day 1, followed by 5-FU 1,200 mg/m2 per day on days 1 and 2 by continuous IV infusion (CIV) (total infusional dose, 2,400 mg/m2 over 46 to 48h); on day 1, precede 5-FU bolus and infusion with leucovorin 400 mg/m2 IV administered concurrently but in separate bags via y-site over 2 hours with oxaliplatin 85 mg/m2 IV. This 2-day regimen (mFOLFOX6) is repeated every 2 weeks for 12 cycles (6 months). Prolongation of the oxaliplatin infusion to 6 hours may mitigate acute toxicities; the infusion time for 5-FU and leucovorin need not be changed. In a multicenter trial, 2,246 patients with stage II or III completely resected colon cancer were randomized to either FOLFOX4 or infusional 5-FU/LV (De Gramont regimen). At a median follow-up of 81.9 months in the patients with stage III disease, there was a significant improvement in 5-year disease-free survival (DFS) in patients receiving FOLFOX4 as compared to those receiving infusional 5-FU/LV (73.3% vs. 67.4%; HR 0.80; p = 0.003). The 6-year overall survival (OS) rates were also improved with FOLFOX4 (78.5% vs. 76%;HR 0.84; p = 0.46). In a subgroup analysis of stage III patients, the 6-year OS rates were improved with FOLFOX4 (72.9% vs. 68.7%; HR 0.80; p = 0.023). There was no significant difference observed in DFS or OS in patients with stage II disease.[40864] [20587] Administering 5-FU 2,400 mg/m2 over 46 to 48 hours (FOLFOX6) provides similar exposure to the daily bolus plus 22 hour 5-FU infusion in FOLFOX4, with increased patient convenience and is preferred.[59867]
500 mg/m2 IV bolus, preceded first by irinotecan 125 mg/m2 IV over 90 minute, and then by leucovorin 20 mg/m2 IV bolus on days 1, 8, 15, and 22, every 6 weeks (IFL), plus bevacizumab 5 mg/kg IV over 30 to 90 minutes every 2 weeks. The sequence of administration is irinotecan, concomitantly with or without bevacizumab, followed by leucovorin, then 5-FU. In a double blind, randomized, placebo-controlled, phase 3 trial, patients who received IFL plus bevacizumab (n = 402) had improved overall survival (OS) (20.3 months vs. 15.6 months; HR 0.66; p < 0.001) and progression-free survival (PFS) (10.6 months vs. 6.2 months; HR 0.54; p < 0.001) compared with patients treated with IFL plus placebo (n = 411). Additionally, the overall response rate (ORR) 45% vs. 35% (p < 0.01) and duration of response 10.4 months vs. 7.1 months, respectively, were also improved with the addition of bevacizumab to IFL.[28177] [59718] [30469] However, IFL has been shown to have increased mortality compared with FOLFIRI in one trial, and is inferior to FOLFOX in another.[41656] [41658] [60896]
400 mg/m2 IV bolus on day 1, followed by 5-FU 1,200 mg/m2/day on days 1 and 2 by continuous IV infusion (CIV) (total infusional dose, 2,400 mg/m2 over 46 hours) for cycles 1 and 2. If there is no toxicity greater than grade 1, the 5-FU infusion dose may be increased to 3,000 mg/m2 for all subsequent cycles. Prior to 5-FU bolus on day 1, administer irinotecan 180 mg/m2 IV over 90 minutes, administered concomitantly but in separate bags with leucovorin 400 mg/m2 IV over 2 hours. If bevacizumab is included, give bevacizumab 5 mg/kg IV over 30 to 90 minutes every 2 weeks on day 1, concurrently with irinotecan. Repeat this 2-day regimen every 2 weeks until disease progression or unacceptable toxicity. In a multicenter, randomized, phase 3 clinical trial, patients with previously untreated metastatic colorectal cancer (mCRC) who received FOLFIRI (n = 144) had improved progression-free survival (PFS) (7.6 months vs. 5.9 months; HR 1.51; p = 0.004) and overall survival (OS) (23.1 months vs. 17.6 months; p = 0.09) compared with those treated with modified IFL (mIFL; n = 141); overall response rate (ORR) was 47.2% vs. 43.3%, respectively. Patients treated with bevacizumab plus FOLFIRI had PFS of 11.2 months vs. 8.3 months (p = 0.28) and OS of 28 months vs. 19.2 months (HR 1.79; p = 0.037) compared with bevacizumab plus mIFL.[41656] Compared with FOLFOX6, PFS was 8.5 months vs. 8 months (p = 0.26) when FOLFIRI was used as first-line therapy for mCRC and 2.5 months vs. 4.2 months (p = 0.003) as second-line therapy compared with FOLFOX6; OS was 21.5 months for patients treated with first-line FOLFIRI and 20.6 months for patients who received FOLFOX6.[35395] Another dosing schedule of FOLFIRI shown to improve ORR (35% vs. 22%), time to progression (TTP) (6.7 months vs. 4.4 months) and OS (17.4 months vs. 14.1 months; p < 0.05) compared with 5-FU/leucovorin is irinotecan 180 mg/m2 IV over 90 minutes followed by leucovorin 200 mg/m2 IV over 2 hours, and then 5-FU 400 mg/m2 IV bolus and 600 mg/m2 CIV over 22 hours; leucovorin and 5-FU (bolus and CIV) are repeated on day 2. Repeat every 2 weeks until disease progression or unacceptable toxicity.[30469]
400 mg/m2 IV bolus over 2 to 4 minutes, followed by 5-FU 600 mg/m2 continuous IV infusion (CIV) over 22 hours on day 1. Prior to 5-FU bolus on day 1, administer oxaliplatin 85 mg/m2 IV and leucovorin 200 mg/m2 IV (both over 120 minutes via Y-site). If giving FOLFOX4 plus bevacizumab, administer bevacizumab 10 mg/kg IV over 30 to 90 minutes prior to chemotherapy on day 1. On day 2, repeat leucovorin 200 mg/m2 IV over 2 hours followed by 5-FU 400 mg/m2 IV bolus, then 5-FU 600 mg/m2 CIV over 22 hours. The order of administration is (bevacizumab) followed by oxaliplatin and leucovorin, followed by 5-FU. This 2-day regimen is repeated every 2 weeks until disease progression or unacceptable toxicity. Prolongation of the oxaliplatin infusion to 6 hours may mitigate acute toxicities; the infusion time for 5-FU and leucovorin need not be changed. In a multicenter, randomized, open-label clinical trial, previously untreated patients with advanced colorectal cancer who received FOLFOX4 (n = 267) had improved median overall survival compared with irinotecan plus 5FU/LV (IFL; n = 264) (19.4 months vs. 14.6 months; HR 0.65; p < 0.0001). Patients treated with FOLFOX 4 also had improved time to progression (TTP; 8.7 months vs. 6.9 months; HR 0.74; p = 0.0014) and overall response rate (ORR; 45.2% vs. 32.5%; p = 0.008) compared with IFL therapy. In a separate multicenter, randomized, open-label trial, previously treated patients with advanced colorectal cancer who had relapsed or progressed within 6 months of first-line therapy with IFL had improved ORR (9% vs. 0%) and median TTP (4.6 months vs. 2.7 months) after treatment with FOLFOX4 (n = 152) compared with 5FU/LV (n = 151).[41958] In another randomized, open-label, placebo-controlled, phase 3 clinical trial, previously treated patients with metastatic colorectal cancer who received FOLFOX4 plus bevacizumab (n = 286) had improved overall survival (OS) (12.9 months vs. 10.8 months; HR 0.75; p = 0.0011) and progression-free survival (PFS) (7.3 months vs. 4.7 months; HR 0.61; p < 0.0001) compared with those treated with FOLFOX4 alone (n = 291). Additionally, the overall response rate (ORR) was 56% in the FOLFOX4 plus bevacizumab arm compared with 43% in the FOLFOX4 alone arm (p < 0.0001).[28177] [47412] The significance of the effect of bevacizumab on OS is not consistent across clinical trials.[41609]
400 mg/m2 IV bolus on day 1, followed by 5-FU 1,200 mg/m2 per day on days 1 and 2 by continuous IV infusion (CIV) (total infusional dose, 2,400 mg/m2 over 46 to 48 hours). Prior to 5-FU bolus on day 1, administer oxaliplatin 85 mg/m2 IV and leucovorin 400 mg/m2 IV concurrently in separate bags via y-site over 2 hours. If giving mFOLFOX6 plus bevacizumab, administer bevacizumab 5 mg/kg IV over 30 to 90 minutes prior to chemotherapy on day 1; the order of administration is (bevacizumab) followed by oxaliplatin and leucovorin, followed by 5-FU. This 2-day regimen is repeated every 2 weeks until disease progression or unacceptable toxicity. Prolongation of the oxaliplatin infusion to 6 hours may mitigate acute toxicities; the infusion time for 5-FU and leucovorin need not be changed. In 2 sequentially conducted, open-label cohorts (TREE-1 and TREE-2), patients with metastatic or recurrent colorectal cancer without prior therapy for advanced disease were randomized to receive treatment with mFOLFOX6 (n = 50), bFOL (n = 50), CapeOx (n = 50), or the same regimens with bevacizumab (n = 75; n = 74; n = 74, respectively). The primary endpoint of treatment-related grade 3 or 4 adverse events in the first 12 weeks occurred in 59% of patients treated with mFOLFOX6, compared with 36% of those receiving bFOL and 67% of patients who received CapeOx; with the addition of bevacizumab, grade 3 or 4 adverse event rates were 59%, 51%, and 56%, respectively. Overall response rate (ORR), a secondary endpoint, was 41% in patients treated with mFOLFOX6, compared with 20% in those who received bFOL and 27% in patients who received CapeOx; median time to progression (TTP) was 8.7 months vs. 6.9 months vs. 5.9 months, and median overall survival (OS) was 19.2 months vs. 17.9 months vs. 17.2 months, respectively. The addition of bevacizumab improved ORR to 52% vs. 39% vs. 46%, TTP to 9.9 months vs. 8.3 months vs. 10.3 months, and OS to 26.1 months vs. 20.4 months vs. 24.6 months, respectively.[47464] [59895]
1,600 mg/m2 per day on days 1 and 2 as a continuous IV infusion (CIV) over 48 hours (total dose 3,200 mg/m2). Prior to administration of 5-FU on day 1, give irinotecan 165 mg/m2 IV over 1 hour, followed by oxaliplatin 85 mg/m2 IV and levo-leucovorin 200 mg/m2 IV administered concurrently in separate bags via y-site over 2 hours (FOLFOXIRI). Repeat every 2 weeks for up to 12 cycles. The order of administration is irinotecan, followed by oxaliplatin plus leucovorin, followed by 5-FU. In a multicenter, randomized, phase III study of patients with unresectable metastatic colorectal cancer were treated with either FOLFOXIRI or FOLFIRI (n = 244). The primary end point of overall response rate (ORR), was significantly higher in patient who received FOLFOXIRI (60% vs. 34%; p < 0.0001). In addition, progression-free survival (PFS) (9.8 months vs. 6.9 months; p = 0.0006) and overall survival (22.6 months vs. 16.7 months; p = 0.032) were both significantly improved in patients who received FOLFOXIRI. Grade 3 and 4 neutropenia (50% vs. 28%; p < 0.001) and grade 2 and 3 peripheral neurotoxicity (19% vs. 0%; p < 0.001) were significantly worse in the FOLFOXIRI arm.[46110]
400 mg/m2 IV bolus followed by fluorouracil 1,200 mg/m2 per day by continuous IV infusion on days 1 and 2 (total infusional dose, 2,400 mg/m2). Prior to fluorouracil administration on day 1, administer irinotecan (180 mg/m2) concomitantly but in separate bags with leucovorin (400 mg/m2 IV) (FOLFIRI); repeat this 2-day regimen every 2 weeks until disease progression or unacceptable toxicity. Administer FOLFIRI in combination with cetuximab (400 mg/m2 IV on day 1 followed by weekly infusions of cetuximab 250 mg/m2 IV; alternatively, cetuximab may be administered at a dose of 500 mg/m2 IV every 2 weeks). Complete cetuximab administration 1 hour prior to chemotherapy and continue until disease progression or unacceptable toxicity.[51181] In a multicenter, randomized, phase 3 study (the CRYSTAL study), the primary endpoint of median progression-free survival (PFS) was significantly improved with cetuximab plus FOLFIRI (n = 599) compared with FOLFIRI alone (n = 599) (8.9 vs. 8 months; HR 0.851) as first-line treatment in unselected patients with metastatic colorectal cancer. In a retrospective subgroup analysis, the addition of cetuximab to FOLFIRI was found to significantly improve the median PFS (9.9 vs 8.4 months) and overall survival (23.5 vs 20 months) in patients with KRAS wild type disease (n = 666); however, a benefit was not found in patients with KRAS-mutated disease (n = 397).[51189]
400 mg/m2 IV bolus on day 1, followed by 5-FU 1,200 mg/m2 per day on days 1 and 2 by continuous IV infusion (CIV) (total infusional dose, 2,400 mg/m2 over 46 to 48 hours). Prior to 5-FU bolus on day 1, administer oxaliplatin 85 mg/m2 IV and leucovorin 400 mg/m2 IV (concurrently over 120 minutes via Y-site) (mFOLFOX6). This 2-day regimen is repeated every 2 weeks until disease progression or unacceptable toxicity. Additionally, give cetuximab 400 mg/m2 IV over 120 minutes (maximum infusion rate, 10 mg/minute) on cycle 1, day 1, followed by weekly infusions of cetuximab 250 mg/m2 IV over 60 minutes (maximum infusion rate, 10 mg/minute); on day 1 of each 2-week cycle, begin oxaliplatin and leucovorin administration 1 hour after completion of cetuximab (order of administration on day 1 is cetuximab, followed by mFOLFOX6). First-line treatment with cetuximab plus modified FOLFOX (mFOLFOX) 4 or 6 significantly improved objective response rates (ORR) in patients with KRAS WT mCRC in two randomized clinical trials. The benefit to progression-free survival (PFS) was small to nonsignificant, and a benefit to overall survival (OS) was not demonstrated. Skin and gastrointestinal toxicities were increased in patients treated with cetuximab.[60036] [60037] [60038] Total exposure (AUC) to 5-FU was similar when administered as two 22-hour infusions of 600 mg/m2, as in FOLFOX4, or as a single 46-hour infusion of 2,400 mg/m2, as in mFOLFOX6 in a pharmacokinetic study.[59867]
400 mg/m2 IV bolus over 2 to 4 minutes, followed by 5-FU 600 mg/m2 continuous IV infusion (CIV) over 22 hours on day 1. Prior to 5-FU bolus on day 1, administer panitumumab 6 mg/kg IV over 60 minutes (infuse doses greater than 1,000 mg over 90 minutes), followed by oxaliplatin 85 mg/m2 IV and leucovorin 200 mg/m2 IV, administered concurrently in separate bags via y-site over 2 hours. If the first panitumumab infusion is tolerated, subsequent doses of 1,000 mg or less may be infused over 30 to 60 minutes. On day 2, repeat leucovorin 200 mg/m2 IV over 2 hours followed by 5-FU 400 mg/m2 IV bolus, then 5-FU 600 mg/m2 CIV over 22 hours. The order of administration is panitumumab, followed by oxaliplatin and leucovorin, followed by 5-FU. This 2-day regimen is repeated every 2 weeks until disease progression or unacceptable toxicity. In a multicenter, randomized, open-label trial, patients with wild-type KRAS metastatic colorectal cancer who received panitumumab in combination with FOLFOX4 (n = 325) had improved progression-free survival (9.6 months vs. 8 months; p = 0.02) and overall response rate (54% vs. 47%) compared with FOLFOX4 alone (n = 331). An exploratory analysis estimated overall survival to be 23.3 months for combination therapy and 19.4 months with FOLFOX4 alone (HR 0.83; 95% CI, 0.7 to 0.98). In the same study, patients with KRAS mutation-positive tumors had decreased progression-free survival (7.3 months vs. 8.8 months; HR 1.29; 95% CI 1.04 to 1.62) and overall survival (15.5 months vs. 19.3 months; HR 1.24; 95% CI, 0.98 to 1.57) when panitumumab was combined with FOLFOX4, compared with FOLFOX4 alone.[50100] [59908]
400 mg/m2 IV bolus on day 1, followed by 5-FU 1,200 mg/m2 per day on days 1 and 2 by continuous IV infusion (CIV) (total infusional dose, 2,400 mg/m2 over 46 to 48 hours). Prior to 5-FU bolus on day 1, administer panitumumab 6 mg/kg IV over 60 minutes (infuse doses greater than 1,000 mg over 90 minutes), followed by oxaliplatin 85 mg/m2 IV and leucovorin 400 mg/m2 IV, administered concurrently in separate bags via y-site over 2 hours. If the first panitumumab infusion is tolerated, subsequent doses of 1,000 mg or less may be infused over 30 to 60 minutes. The order of administration is panitumumab, followed by oxaliplatin and leucovorin, followed by 5-FU. This 2-day regimen is repeated every 2 weeks until disease progression or unacceptable toxicity. In a randomized, multicenter, open-label phase II clinical trial, panitumumab plus mFOLFOX6 was compared to bevacizumab plus mFOLFOX6 in previously untreated patients with metastatic colorectal cancer (wild type KRAS exon 2). In patients with wild type KRAS (exon 2), the primary endpoint of median progression free survival (PFS) was not significantly improved with the addition of panitumumab to mFOLFOX6 compared with bevacizumab (10.9 months vs. 10.1 months; HR 0.87; p = 0.353). In combination with mFOLFOX6, treatment with panitumumab significantly improved the secondary endpoint of median overall survival (OS) compared with bevacizumab (34.2 months vs. 24.3 months; HR 0.62; p = 0.009); overall response rate (ORR) (57.8% vs. 53.5%) and resection rate (13% vs. 11%) were also improved with panitumumab. In a preplanned extended RAS analysis, panitumumab was associated with a significantly improved median PFS (13 months vs. 9.5 months; p = 0.029) and median OS (41.3 months vs. 28.9 months; p = 0.058) compared with bevacizumab in patients with wild type RAS; ORR was also improved (63.6% vs. 60.5%). Grade 3 or higher adverse events were reported in 91% of patients who received panitumumab and 83% of those treated with bevacizumab.[59907]
1000 mg/m2/day continuous IV for 4 days on days 1—4 and 29—32 in combination with mitomycin (10 mg/m2 IV bolus on days 1 and 29) and radiation therapy has been studied.[27182] [35630] A smaller phase III study has also considered 5-FU 750 mg/m2 IV continuous infusion over 4 days on days 1—4 and 29—32 in combination with mitomycin (15 mg/m2 IV on day 1) and radiotherapy in patients with locally advanced anal cancer.[21310]
Multiple dosage regimens have been studied. 5-fluorouracil (5-FU) 750 mg/m2/day continuous IV infusion (CIVI) on days 1—4 in combination with cisplatin (100 mg/m2 IV on day 1), repeated every 21 days for 2—3 cycles has been given with concomitant radiation (XRT).[35720] Alternately, 5-FU 1000 mg/m2/day has been given as a CIVI on days 1—4 in combination with cisplatin 75 mg/m2 IV over 60 minutes on day 1, repeated every 28 days for 4 cycles.[45529]
NOTE: Dosage should be based upon body surface area using actual body weight unless patient is obese or has significant fluid retention. In these cases the dose should be based upon the ideal weight or dry weight.
As a single agent, fluorouracil 500 mg/m2 IV bolus days 1 through 5 every 28 days has shown response rates of 15% to 35%; however, it is most commonly used in combination with other chemotherapy agents. Common combination regimens include fluorouracil 600 mg/m2 IV bolus on days 1, 8, 29, and 36 with doxorubicin and mitomycin every 8 weeks (FAM); fluorouracil 1,500 mg/m2 IV bolus (1 hour after methotrexate) on day 1 with doxorubicin, methotrexate, and leucovorin every 28 days (FAMTX); fluorouracil 300 mg/m2 IV bolus on days 1 through 5 in combination with doxorubicin and cisplatin every 5 weeks (FAP); or fluorouracil 500 mg/m2 IV bolus days 1 through 3 with etoposide and leucovorin every 21 days (ELF).
200 mg/m2 per day continuous IV infusion on days 1 through 21 in combination with cisplatin 60 mg/m2 IV on day 1 and epirubicin 50 mg/m2 IV on day 1, repeated every 3 weeks (ECF regimen). Treatment should be given for 3 cycles before and 3 cycles after surgical resection. In a phase 3 clinical trial, surgery was performed 3 to 6 weeks after the third cycle of preoperative chemotherapy; postoperative chemotherapy was initiated 6 to 12 weeks after surgery. Overall survival and progression free survival were significantly improved in the ECF arm.[34867]
800 mg/m2 per day continuous IV infusion on days 1 through 5 in combination with cisplatin (80 mg/m2 IV on day 1) and trastuzumab (8 mg/kg IV on day 1, then 6 mg/kg IV every 21 days beginning on day 22); repeat cycles every 3 weeks. Chemotherapy should be continued up to a maximum of 6 cycles; trastuzumab should be continued until disease progression or unacceptable toxicity. In a phase 3 trial, 594 patients with inoperable, locally advanced, recurrent, or metastatic adenocarcinoma of the stomach or gastroesophageal junction were randomized to receive cisplatin and fluorouracil or capecitabine, with or without trastuzumab. Overall survival (13.5 months vs. 11 months), the primary endpoint, and objective response rate (47% vs. 35%) were significantly increased with the addition of trastuzumab. An updated survival analysis conducted 1-year after the final analysis showed a continued overall survival benefit in the trastuzumab arm (13.1 months vs. 11.7 months). In addition, a subgroup analysis revealed an even greater increase in overall survival (18 months vs. 13.2 months) for the trastuzumab arm in patients with high expression of the HER2 protein (FISH-negative and IHC3 +; or, FISH-positive). Cardiac dysfunction (LVEF decrease 10% or more from baseline to an absolute value less than 50%) occurred in 5% of patients who received trastuzumab vs. 1.1% of patients who did not receive trastuzumab.[36110] [41715] [28061]
The FDA-approved dose of fluorouracil for the treatment of pancreatic cancer is 400 mg/m2 IV bolus on day 1, followed by 2,400 mg/m2 continuous IV infusion over 46 hours, every 2 weeks in combination with leucovorin or as a component of a multidrug chemotherapy regimen. Refer to individual treatment protocols for specific dose recommendations.[63817]
2,400 mg/m2 IV continuously over 46 hours every 2 weeks for 12 cycles, in combination with leucovorin (400 mg/m2 IV), oxaliplatin (85 mg/m2 IV), and irinotecan (150 mg/m2 IV). Administer oxaliplatin first, immediately followed by leucovorin and irinotecan; administer fluorouracil last. In a randomized phase 3 trial, adjuvant treatment with mFOLFIRINOX significantly increased both progression-free survival (PFS) and overall survival (OS) compared with gemcitabine monotherapy in patients with pancreatic cancer. In this trial, patients were carefully selected for treatment based on age (younger than 80 years of age), R0 or R1 resection, and a CA 19-9 level of 180 units/mL or less.[64744]
400 mg/m2 IV bolus followed by 2,400 mg/m2 by continuous IV infusion over 46 hours every 2 weeks for up to 6 months, in combination with leucovorin (400 mg/m2 IV), oxaliplatin (85 mg/m2 IV), and irinotecan (180 mg/m2 IV). Administer oxaliplatin first, immediately followed by leucovorin and irinotecan; administer fluorouracil last.[51161]
2,400 mg/m2 by continuous IV infusion over 46 hours, in combination with leucovorin (400 mg/m2 IV), oxaliplatin (60 mg/m2 IV), and liposomal irinotecan (50 mg/m2 IV), every 2 weeks until disease progression or unacceptable toxicity (NALIRIFOX). Administer liposomal irinotecan prior to oxaliplatin, leucovorin, and fluorouracil. Do not substitute liposomal irinotecan with irinotecan HCl. Do not reduce the dose of liposomal irinotecan for patients homozygous for UGT1A1*28 allele. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. First-line treatment with NALIRIFOX significantly improved overall survival (11.1 months vs. 9.2 months) and progression-free survival (7.4 months vs. 5.6 months) compared with gemcitabine plus nab-paclitaxel in patients with metastatic pancreatic adenocarcinoma in a multicenter, randomized, open-label phase 3 clinical trial (NAPOLI-3); the objective response rate was 41.8% vs. 36.2%.[60243] [70338]
2,000 mg/m2 by continuous IV infusion over 24 hours on days 1, 8, 15, and 22, in combination with leucovorin (200 mg/m2 IV) and oxaliplatin (85 mg/m2 IV on days 8 and 22), every 42 days until disease progression or unacceptable toxicity. In a phase 3 trial, 160 patients with pancreatic cancer that progressed while receiving gemcitabine, were randomized to receive fluorouracil and leucovorin with or without oxaliplatin (OFF vs. FF). Overall survival, the primary endpoint, was significantly longer in patients receiving oxaliplatin (26 weeks vs. 13 weeks). Neurologic toxicity and leukopenia occurred more frequently in the oxaliplatin arm.[35050] Initially, this clinical trial randomized patients to receive OFF plus best supportive care (BSC) or BSC alone. Due to the rejection of BSC as an acceptable second-line treatment modality and subsequent poor accrual, the study was amended after the recruitment of 46 patients to OFF vs. FF. Final analysis of OFF vs. BSC revealed a significant improvement in OS (4.83 months vs. 2.3 months).[45671]
2,400 mg/m2 continuous IV infusion over 46 hours in combination with leucovorin (400 mg/m2 IV) and liposomal irinotecan (70 mg/m2 IV), every 2 weeks until disease progression or unacceptable toxicity. Administer fluorouracil after completion of liposomal irinotecan and leucovorin. Do not substitute irinotecan liposome for other drugs containing irinotecan HCl. For patients homozygous for UGT1A1*28 allele, decrease the starting dose for irinotecan liposome to 50 mg/m2, and increase to 70 mg/m2 as tolerated in subsequent cycles. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Treatment with liposomal irinotecan, leucovorin, and fluorouracil significantly improved overall survival (6.2 months vs. 4.2 months) and progression-free survival (3.1 months vs. 1.5 months) compared with leucovorin and fluorouracil alone in patients with metastatic pancreatic adenocarcinoma in a multicenter, randomized, open-label phase 3 clinical trial (NAPOLI-1); the objective response rate was 7.7% vs. 0.8%.[60243] [70337]
According to the manufacturer, the recommended dose of 5-fluorouracil for the treatment of breast cancer is 500 mg/m2 or 600 mg/m2 IV on days 1 and 8, as a component of a cyclophosphamide-based multidrug regimen, every 28 days for 6 cycles.[29028] See individual protocols for specific dosing.
500 mg/m2 IV in combination with epirubicin (75 mg/m2 IV) and cyclophosphamide (500 mg/m2 IV) on day 1, every 21 days for 4 cycles (FEC-75).[63560] [63561] Dose adjustments for subsequent cycles are recommended by the manufacturer based on nadir platelet counts, ANC, or grade 3 to 4 toxicity.[41751] After completion of 4 cycles of FEC-75, administer paclitaxel 80 mg/m2 IV once weekly in combination with trastuzumab (4 mg/kg IV over 90 minutes on week 1, then 2 mg/kg IV over 30 minutes once weekly), every 21 days for 4 cycles (12 weeks). Surgery should be performed after completion of paclitaxel plus trastuzumab therapy, followed by trastuzumab 6 mg/kg IV every 3 weeks for a total of 52 weeks from the first preoperative dose. In a randomized, phase 3 clinical trial, neoadjuvant treatment with FEC-75 followed by paclitaxel plus trastuzumab (sequential therapy) resulted in similar rates of pathologic complete response (pCR), disease-free survival (DFS), and overall survival (OS) compared with paclitaxel plus trastuzumab followed by FEC-75 plus trastuzumab (concurrent therapy). Sequential therapy was better tolerated and had a lower incidence of cardiac adverse reactions.[63560] [63561]
600 mg/m2 IV plus methotrexate 40 mg/m2 IV on days 1 and 8, in combination with cyclophosphamide 100 mg/m2 by mouth on days 1 through 14, repeated every 28 days for 6 cycles.[61185] [47962] [47985] [51607]
500 mg/m2 IV on day 1 in combination with epirubicin (100 mg/m2 IV) and cyclophosphamide (500 mg/m2 IV) (FEC regimen) every 21 days for 6 cycles. Alternatively, FEC may be administered for 3 cycles, then followed by docetaxel (100 mg/m2 IV) given every 21 days for 3 cycles (FEC-D regimen). A phase III trial of 1944 patients with node-positive breast cancer compared the FEC-D regimen for 3 cycles to FEC for 6 cycles. The primary endpoint, 5-year disease-free survival, was significantly longer in the FEC-D arm (78.4% vs. 73.2%, p = 0.012). Overall survival at 5 years was also increased by FEC-D (90.7% vs. 86.7%, p = 0.017). Grade 3/4 neutropenia and the incidence of nausea/vomiting were higher with FEC, while stomatitis, edema, and nail changes were more common with FEC-D.[34268]
400 mg/m2 IV on days 1 and 8 in combination with epirubicin 50 mg/m2 IV on days 1 and 8, plus cyclophosphamide 500 mg/m2 IV on days 1 and 8, every 3 to 4 weeks depending on patient recovery. In a phase III clinical trial, treatment was planned for 6 cycles, but was given up to 9 cycles in patients with a partial or complete response.[49142]
NOTE: Dosage should be based upon body surface area using actual body weight unless patient is obese or has significant fluid retention. In these cases the dose should be based upon the ideal weight or dry weight.
1,000 mg/m2 per day continuous IV infusion on days 1, 2, 3, and 4 in combination with cisplatin (100 mg/m2 IV on day 1), repeated every 3 weeks has been studied. No difference in overall survival was seen when compared to cisplatin and paclitaxel.[36026]
1,000 mg/m2 per day IV over 4 days on days 71 through 74, 99 through 102, and 127 through 130 in combination with cisplatin (80 mg/m2 IV on days 71, 99, and 127); this regimen is preceded by cisplatin (100 mg/m2 IV over 15 to 20 minutes on days 1, 22, and 43) given concurrently with radiation therapy (RT). In a phase 3 trial of 147 patients with advanced nasopharyngeal cancer, chemoradiotherapy significantly improved 3-year progression-free (69% vs. 24%) and overall survival (76% vs. 46%) rates versus RT alone.[20929]
750 mg/m2 per day continuous IV infusion on days 1, 2, 3, 4, and 5 in combination with cisplatin (75 mg/m2 IV over 1 hour) on day 1 immediately before docetaxel (75 mg/m2 IV over 1 hour) on day 1; this regimen is given every 3 weeks for 4 cycles. After completion of chemotherapy, patients should receive radiation therapy. All patients must receive prophylaxis for neutropenic infections, premedication with antiemetics, and appropriate hydration (before and after cisplatin administration). During clinical trials, colony-stimulating factors were recommended during the second and/or subsequent cycles for prophylaxis of febrile neutropenia, documented infections with neutropenia, or neutropenia lasting longer than 7 days. In a randomized trial of 358 patients with inoperable, locally advanced squamous head and neck cancer, patients were treated with the FDA-approved regimen of docetaxel/cisplatin/fluorouracil or cisplatin (100 mg/m2 IV day 1) and fluorouracil (1,000 mg/m2/day continuous IV infusion for 5 days) every 3 weeks for 4 cycles. Progression-free survival (PFS), the primary end-point of the study, was significantly longer in the docetaxel/cisplatin/fluorouracil arm as compared to the cisplatin/fluorouracil (11.4 months vs. 8.3 months) with a median follow-up of 33.7 months. With a follow-up of 51.2 months, the median overall survival also favored patients treated with docetaxel/cisplatin/fluorouracil as compared to those treated with cisplatin/fluorouracil (18.6 months vs. 14.2 months).[28505]
1,000 mg/m2 per day continuous IV infusion on days 1, 2, 3, and 4 in combination with cisplatin (100 mg/m2 IV over 1 hour) on day 1 immediately before docetaxel (75 mg/m2 IV over 30 minutes to 3 hours) on day 1; this regimen is given every 3 weeks for 3 cycles. After completion of chemotherapy, patients should receive chemoradiotherapy. All patients must receive prophylaxis for neutropenic infections, premedication with antiemetics, and appropriate hydration (before and after cisplatin administration).[28505]
600 mg/m2 per day continuous IV infusion on days 1, 2, 3, and 4 in combination with carboplatin (70 mg/m2 per day IV on days 1, 2, 3, and 4). Chemotherapy cycles were started on days 1, 22, and 43 and were administered concurrently with radiotherapy (RT). In a phase 3 trial, 226 patients with stage III or IV squamous cell carcinoma of the oropharynx (no evidence of distant metastasis) were randomized to receive radiotherapy alone or concomitantly with carboplatin/fluorouracil. Overall survival at 5 years was significantly improved in the chemoradiotherapy arm (22.4% vs. 15.8%). The 5-year specific disease free survival rate (26.6% vs. 14.6%) and locoregional control rate (47.6% vs. 24.7%) were also significantly improved with chemoradiotherapy. Hematologic and skin toxicities were more common in chemoradiotherapy arm. In addition, grades 3 and 4 mucositis and poor nutritional status occurred more frequently with concomitant therapy. There were no significant differences in late toxic effects between the arms when assessed at 5 years.[43174] [43119]
1,000 mg/m2 per day continuous IV infusion over 96 hours on days 1, 2, 3, and 4 in combination with carboplatin (300 mg/m2 IV day 1); repeated every 4 weeks. In a phase 3 trial, 277 patients were randomized to receive carboplatin/fluorouracil, cisplatin/fluorouracil, or methotrexate (MTX). An increase in overall response rate was achieved with carboplatin/fluorouracil versus MTX, which was of borderline statistical significance (21% vs. 10%, p = 0.05). The overall response rate was numerically lower with carboplatin/fluorouracil compared to cisplatin/fluorouracil (21% vs. 32%).[43120]
1,000 mg/m2 IV on days 1, 2, 3, and 4 in combination with carboplatin (AUC 5 IV on day 1), repeated every 3 weeks for up to 6 cycles. Administer with cetuximab (400 mg/m2 IV as an initial loading dose on day 1 followed by weekly infusions of cetuximab 250 mg/m2 IV; alternatively, cetuximab may be administered at a dose of 500 mg/m2 IV every 2 weeks). Complete cetuximab administration 1 hour prior to chemotherapy and continue until disease progression or unacceptable toxicity. In a phase 3 trial, 442 patients were randomized to receive platinum (cisplatin or carboplatin) and fluorouracil with or without cetuximab. Overall survival, the primary endpoint, was significantly greater with the addition of cetuximab to chemotherapy compared with chemotherapy alone (10.1 months vs. 7.4 months). Sepsis, hypomagnesemia, grade 3 skin reactions, and grade 3 or 4 infusion reactions occurred more frequently with the addition of cetuximab.[35055]
1,000 mg/m2 IV on days 1, 2, 3, and 4 in combination with cisplatin (100 mg/m2 IV on day 1), repeated every 3 weeks for up to 6 cycles. Administer with cetuximab (400 mg/m2 IV as an initial loading dose on day 1 followed by weekly infusions of cetuximab 250 mg/m2 IV; alternatively, cetuximab may be administered at a dose of 500 mg/m2 IV every 2 weeks). Complete cetuximab administration 1 hour prior to chemotherapy and continue until disease progression or unacceptable toxicity. In a phase 3 trial, 442 patients were randomized to receive platinum (cisplatin or carboplatin) and fluorouracil with or without cetuximab. Overall survival, the primary endpoint, was significantly greater with the addition of cetuximab to chemotherapy compared with chemotherapy alone (10.1 months vs. 7.4 months). Sepsis, hypomagnesemia, grade 3 skin reactions, and grade 3 or 4 infusion reactions occurred more frequently with the addition of cetuximab.[35055]
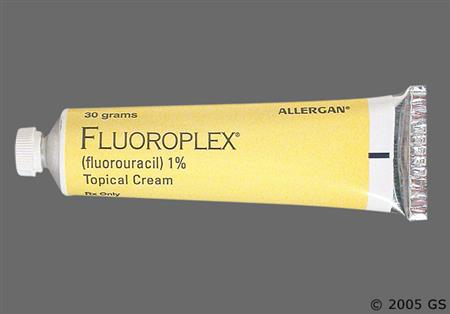
Apply sufficient topical solution or cream to cover affected area; apply twice daily. The 1% preparations are usually used on the head, neck, and chest; the 2% and 5% preparations are used on the hands. A treatment period of at least 2 to 6 weeks is usually required. Increasing the frequency of application and longer period of administration may be required on areas other than the head and neck. Complete healing of the lesions may not be evident for 1 to 2 months following completion of therapy. Close follow-up is recommended.[53825] [53831]
Apply enough cream to cover lesions on face or anterior scalp once daily. Apply at least 10 minutes after thoroughly washing, rinsing, and drying the entire area. May be applied with fingertips, but immediately wash hands after applying. Therapy should continue up to 4 weeks, as tolerated. Continued treatment up to 4 weeks results in greater lesion reduction. In patients treated for 1 week, 74% of the lesions disappeared, with 2 weeks of treatment, the clearance rate is 85%, and following 4 weeks of treatment the clearance rate increased to 90%.[48332]
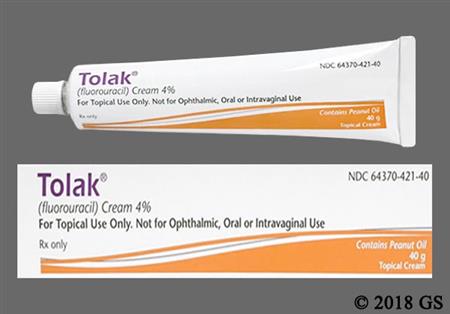
Apply enough cream to cover lesions on face, ears, and/or scalp once daily with a thin film. Apply after thoroughly washing, rinsing, and drying the entire area. May be applied with fingertips to gently massage the medication uniformly into the skin, but immediately wash hands after applying. Therapy should continue up to 4 weeks, as tolerated.[60171]
Apply fluorouracil 5% cream or solution twice daily; use a sufficient amount to cover the lesions. Continue treatment for at least 3 to 6 weeks; complete resolution of lesions may take up to 10 to 12 weeks. In an analysis of 54 patients with a total of 113 superficial basal cell carcinoma lesions, approximately 93% of lesions resolved following treatment with fluorouracil 5% cream or solution. There was 1 failure in 25 lesions treated with fluorouracil 5% solution and 7 failures in 88 lesions treated with fluorouracil 5% cream.[53825]
Apply a thin layer topically to the wart(s) 1 to 2 times daily for 4 to 12 weeks.[51147] [59982] [69965] [69973]
Apply a thin layer topically to the wart(s) 1 to 2 times daily for 4 to 12 weeks.[51147] [59982] [69965] [69973]
Recommended Monitoring
Systemic Therapy
Management of Treatment-Related Toxicities
Interrupt systemic fluorouracil therapy for any of the following; upon resolution or improvement to grade 1 toxicity, resume fluorouracil treatment at a reduced dose.
Interrupt systemic fluorouracil therapy for any of the following; the safety of resuming fluorouracil treatment after resolution or improvement has not been established.
Fluorouracil Dose Adjustments when given in Combination with Irinotecan:
Myelosuppression
ANC 1,000 to 1,499 cells/mm3 or platelets 50,000 to 74,999 cells/mm3
ANC 500 to 999 cells/mm3 or platelets 25,000 to 49,999 cells/mm3
ANC less than 500 cells/mm3 or platelets less than 25,000 cells/mm3
Neutropenic Fever
Diarrhea
2 to 3 stools per day above baseline
4 to 6 stools per day above baseline
7 to 9 stools per day above baseline
Greater than or equal to 10 stools per day above baseline
Other non-hematologic toxicities
Grade 2
Grade 3
Grade 4
The manufacturer recommends a maximum 5-FU dose of 800 mg/day IV; however, higher doses as are routinely given. Intravenous bolus doses of 20—25 mg/kg generally result in severe toxicity or fatalities due to hemorrhagic colitis or bone marrow suppression. By continuous infusion, higher daily doses (i.e., 1—2 g/day) have been given successfully with less hematologic toxicity. Maximum doses are not available for topical products.
The manufacturer recommends a maximum 5-FU dose of 800 mg/day IV; however, higher doses as are routinely given. Intravenous bolus doses of 20—25 mg/kg generally result in severe toxicity or fatalities due to hemorrhagic colitis or bone marrow suppression. By continuous infusion, higher daily doses (i.e., 1—2 g/day) have been given successfully with less hematologic toxicity. Maximum doses are not available for topical products.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
5-FU has been administered to patients with hepatic insufficiency without dose reduction; however, it has been recommended to avoid the use of fluorouracil in patients with elevated serum bilirubin > 5 mg/dL.[53549]
It does not appear that the dosage of fluorouracil, 5-FU, needs to be adjusted in normal patients with renal impairment. Patients with dihydropyrimidine dehydrogenase (DPD) deficiency and renal impairment may require a dosage reduction of 5-FU.
† Off-label indication


















NOTE: The FDA has issued a warning regarding the occurrence of adverse events resulting from name confusion between fluorouracil cream (Carac™) and ketoconazole cream (Kuric™). Use caution when using either one of these products.
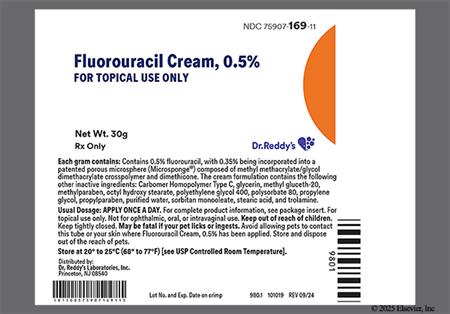
Fluorouracil (5-FU) is a fluorinated pyrimidine and acts as an antimetabolite antineoplastic agent. It differs from the naturally occurring product, uracil, by the addition of a fluoride at position 5. Fluorouracil is a component of chemotherapy regimens for many solid tumors, including breast, colorectal, gastrointestinal, and head and neck cancers. The clinical pharmacology of 5-FU is complex and the pharmacokinetics are complicated by intra- and inter-patient variability, nonlinear elimination, and erratic bioavailability. The toxicities and efficacy of 5-FU differ depending upon the route of administration of the drug. A meta-analysis of 5-FU studies in the treatment of colorectal cancer found that continuous infusion led to a superior response and overall survival rate with a decreased incidence of severe hematologic toxicity as compared to bolus injection. However, there was an increased incidence of hand-foot syndrome with the continuous infusion as compared to the bolus injection.[26296] Fluorouracil commonly is given intravenously but is also used topically for malignant keratoses of the skin. Fluorouracil was approved by the FDA in 1962. In October 2000, a new formulation of fluorouracil cream using a microsponge delivery system (Carac™) was FDA-approved. The new delivery system allows for once daily dosing and a sustained release of fluorouracil.
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Emetic Risk
Extravasation Risk
Patient Counseling
Precipitation:
Intravenous injection:
Intravenous infusion:
NOTE: Ensure correct formulation selection based on indication during prescribing and before administration. Basal cell carcinoma is treated with the 5% formulation.[53825][70287]
Epistaxis was reported in postmarketing experience with the systemic use of fluorouracil.[70470]
Medicinal taste (dysgeusia) and stomatitis have been reported infrequently in patients treated with fluorouracil solution or cream.[53825] [60171] Systemic administration of fluorouracil can cause severe diarrhea; administer fluids, electrolyte replacement, or antidiarrheal treatments as necessary. Mucositis, stomatitis, esophagitis, and pharyngitis, which may lead to mucosal sloughing or oral ulceration, can also occur with systemic fluorouracil treatment; the incidence is higher when administered as an IV bolus compared to continuous infusion. An interruption of therapy and possible dose reduction may be necessary for severe diarrhea or mucositis. GI ulceration (peptic ulcer), nausea, and vomiting have also been reported in postmarketing experiences with fluorouracil. There is an increased risk of acute early-onset toxicities and serious adverse reactions that can result in death (e.g., mucositis, diarrhea) in patients with dihydropyrimidine dehydrogenase (DPD) deficiency.[70470] Only 1 case of serious systemic toxicity associated with DPD deficiency during the topical administration of fluorouracil has been observed in a patient using the 5% cream. Symptoms included severe abdominal pain, bloody diarrhea (GI bleeding), vomiting, fever, and chills. It is unknown whether patients with profound DPD deficiency would develop systemic toxicity with lower concentrations of topical fluorouracil.[48332] [60498] [60499] [53825] [60171]
Leukocytosis has been reported in patients treated with fluorouracil solution or cream; pancytopenia, eosinophilia, thrombocytopenia, and toxic granulation have also occurred infrequently.[53825] [60171] Systemic treatment with fluorouracil can result in severe and potentially fatal bone marrow suppression including neutropenia, thrombocytopenia, and anemia; pancytopenia has been reported in postmarketing experience with systemic use of fluorouracil. The neutrophil nadir typically occurs between 9 and 14 days after administration. Monitor complete blood counts prior to each cycle, or weekly if administered on a weekly or similar schedule, and as needed. An interruption of therapy may be necessary for grade 4 myelosuppression.[70470]
Headache was reported in 3.1% of patients treated with fluorouracil 0.5% cream (n = 257) compared with 2.4% of patients who received vehicle alone (n = 127) in a pooled analysis from two phase 3 studies.[48332] Nystagmus and headache have been reported in postmarketing experience with the systemic use of fluorouracil.[70470]
Ocular irritation was reported in 3.4% to 5.9% of patients treated with fluorouracil cream. Symptoms of ocular irritation were burning, watering (lacrimation), sensitivity, stinging (ocular pain) and ocular pruritus. Conjunctival reaction (conjunctivitis), corneal reaction, and lacrimation have been reported infrequently in patients treated with fluorouracil solution or cream.[48332] [53825] [60171] Lacrimal duct stenosis, visual changes, lacrimation, and photophobia have been reported with the systemic use of fluorouracil.[70470]
Cardiotoxicity including angina, myocardial infarction/ischemia, arrhythmia or arrhythmia exacerbation, and heart failure has been reported with fluorouracil treatment in postmarketing experience; patients receiving fluorouracil via continuous infusion are at increased risk compared to those receiving an IV bolus, as well as patients with CAD. Interrupt fluorouracil therapy if cardiotoxicity occurs; the safety of resuming therapy in patients with cardiotoxicity has not been established.[70470]
In two trials sponsored by the National Cancer Institute for initial treatment of metastatic colorectal cancer, an imbalance in the number of deaths occurring within 60 days of the initiation of treatment was associated with irinotecan, leucovorin, and fluorouracil treatment as compared to fluorouracil and leucovorin (Trial C89803) or oxaliplatin, fluorouracil, and leucovorin therapy (Study N9741). In study N9741 of patients with advanced disease, 12/14 deaths associated with irinotecan, fluorouracil, and leucovorin had several characteristics in common: dehydration (resulting from diarrhea, nausea, and vomiting), neutropenia, and sepsis (alone or in combination with shock), leading to death. Thirteen deaths occurred during the first 6-week cycle or immediately afterward. In the surgical adjuvant study (Trial C89803), 14 deaths in the group assigned to receive irinotecan, fluorouracil, and leucovorin included pulmonary embolism (3 patients), sepsis (3), aspiration (3), myocardial infarction (1), dehydration and neutropenia (1), stroke (1), bowel ischemia or infarct or both (1), and one unknown. Dose modifications to these trials have been made in an attempt to decrease toxicity. Close monitoring of patients receiving the combination of irinotecan, fluorouracil, and leucovorin is warranted.[26489]
Injection site reaction has been associated with IV fluorouracil administration. An erythematous eruption overlying the veins on both arms has been reported in several patients after IV fluorouracil. No superficial phlebitis or extravasation were observed.[25526]
Palmar-plantar erythrodysesthesia (hand and foot syndrome) has been reported with systemic fluorouracil therapy; symptoms may include a tingling sensation, pain, swelling, erythema with tenderness, and desquamation. Palmar-plantar erythrodysesthesia may occur at any time but is generally observed after 8 to 9 weeks of treatment. Prolonged/continuous fluorouracil infusions are more commonly associated with this syndrome compared to bolus injections; patients with previous exposure to chemotherapy may also be at increased risk. An interruption of therapy or dose reduction may be necessary depending on the severity.[70470]
Dermatologic reaction to topical products were the most commonly reported adverse reactions. These included erythema (89.4% to 99%), scaling or xerosis (69% to 95%), crusting (87%), pruritus (85%), stinging or burning (60% to 87%), edema (14.1% to 69%), skin erosion (24.7% to 68%), pain (30.6% to 62.2%), application site reaction (91.8% to 96.5%), skin irritation (up to 2.4%), allergic contact dermatitis, scarring, rash, skin ulcer, inflammation, telangiectasia, alopecia, blistering, skin hyperpigmentation, bullous pemphigoid, ichthyosis, suppuration, swelling, soreness, tenderness, urticaria, and photosensitivity. These adverse events generally increased over the treatment period and diminished to baseline levels weeks after treatment cessation. Xerosis, skin fissures, vein pigmentation, and nail changes including onycholysis have been reported in postmarketing experience with the systemic use of fluorouracil; photosensitivity has also been reported, including erythema and skin hyperpigmentation.[70470] [48332] [53825] [53831] [60171]
Cleft lip/palate was reported in a newborn whose mother used topical fluorouracil as recommended. Additionally, cases of spontaneous fetal abortion (miscarriage) and teratogenesis (specifically, ventricular septal defect) have been reported when fluorouracil was applied to mucous membranes during pregnancy. Multiple birth defects were reported in a fetus of a patient who received IV fluorouracil.[53825]
Emotional upset, insomnia, and irritability occurred infrequently in patients treated with fluorouracil solution or cream.[53825] [60171] Euphoria has also been reported in postmarketing experience with the systemic use of fluorouracil.[70470]
Nasal irritation has been reported infrequently in patients treated with fluorouracil 2% or 5% solution or 5% cream.[53825]
Infection [e.g., common cold virus (up to 4.7%), sinusitis (up to 4.7%)] was reported in patients treated with fluorouracil 0.5% cream; however, the incidence of infection was not greater in the fluorouracil arm compared with the vehicle alone arm.[48332] Herpes simplex viral infection occurred infrequently in patients treated with fluorouracil solution or cream.[53825] [60171]
Generalized allergic reactions including anaphylactoid reactions have been reported in postmarketing experience with the systemic use of fluorouracil.[70470]
Thrombophlebitis (phlebitis) has been reported in postmarketing experience with the systemic use of fluorouracil.[70470]
Encephalopathy related to hyperammonemia in the absence of hepatic disease or other identifiable cause has been reported with fluorouracil therapy in postmarketing experience. Signs or symptoms began within 72 hours after initiation of fluorouracil infusion and included altered mental status, confusion, disorientation, coma, or ataxia with concurrent elevated serum ammonia levels. Symptoms of neurotoxicity mentioned above can also occur without increased ammonia levels; acute cerebellar syndrome has additionally been reported in postmarketing experience. An interruption of fluorouracil is necessary for hyperammonemic encephalopathy or other neurotoxicity; initiate ammonia-lowering therapy for hyperammonemic encephalopathy. The safety of resuming therapy after resolution of hyperammonemic encephalopathy or other neurotoxicity has not been established.[70470]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
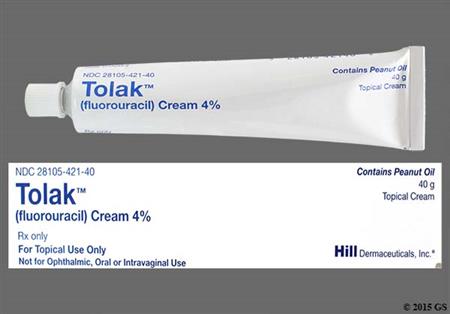
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Topical fluorouracil cream (Tolak) contains peanut oil; discontinue immediately if signs of hypersensitivity occur.[60171]
Some formulations of topical fluorouracil are contraindicated in patients with dihydropyrimidine dehydrogenase deficiency (DPD deficiency); DPD enzyme deficiency can result in shunting of fluorouracil to the anabolic pathway, leading to cytotoxic activity and potential toxicities.[48332] [53825] [53831] [60171] Systemic fluorouracil is not recommended for patients with certain homozygous or compound heterozygous DPYD variants that result in complete DPD deficiency due to an increased risk of acute early-onset toxicities and serious adverse reactions that can result in death (e.g., mucositis, diarrhea, neutropenia, neurotoxicity); patients with partial DPD deficiency may also have an increased risk of serious adverse reactions. Consider testing for DPD deficiency prior to starting therapy if clinically appropriate. There is not an FDA-approved test to detect DPYD mutations; currently available tests may vary in accuracy and design. Hold or permanently discontinue fluorouracil in patients with acute early-onset or unusually severe toxicities, which may indicate near complete or total absence of DPD activity.[70470]
Topical fluorouracil is contraindicated during pregnancy.[48332] [53825] [60498] [60499] Pregnancy should be avoided by females of reproductive potential during treatment with systemic fluorouracil and for up to 3 months after the last dose. Although there are no adequately controlled studies in pregnant women, fluorouracil can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. Women who are pregnant or who become pregnant while receiving fluorouracil should be apprised of the potential hazard to the fetus. When administered as an intraperitoneal injection during organogenesis, malformations including cleft palate, skeletal defects, and deformed paws and tails were observed in mice at doses approximately 0.06 times a human dose of 12 mg/kg for 4 days; delayed growth and malformations including microanophthalmos occurred with a single intraperitoneal dose approximating 0.2 times a human dose of 12 mg/kg to rats during organogenesis. Intramuscular fluorouracil administration to hamsters at lower doses than those used in common treatment regimens had similar results. Fluorouracil administration to monkeys during organogenesis resulted in abortion at doses approximately equal to a human dose of 12 mg/kg; decreasing the dose by half resulted in increased resorptions and decreased fetal body weight.[70470] One birth defect (cleft lip and palate) has been reported in the newborn of a patient using topical fluorouracil as recommended. Miscarriages and birth defects (ventricular septal defects) have been reported when topical fluorouracil was applied to mucous membranes during pregnancy. The amount of fluorouracil absorbed systemically after topical administration to actinic keratoses is minimal.[48332] [53825] [60498] [60499]
Counsel patients about the reproductive risk and contraception requirements during fluorouracil treatment. Fluorouracil can be teratogenic if taken by the mother during pregnancy.[70470] [53825] [48332] [53831] [60171] Females of reproductive potential should avoid pregnancy and use effective contraception during and for up to 3 months after treatment with systemic fluorouracil. Due to the risk of male-mediated teratogenicity, males with female partners of reproductive potential should also use effective contraception during and for up to 3 months after treatment with systemic fluorouracil.[70470] Females of reproductive potential should also use effective contraception during administration of fluorouracil 4% cream (Tolak) and for 1 month after the last dose; recommendations for contraception are not available for other topical formulations.[53825] [48332] [53831] [60171] Females of reproductive potential should undergo pregnancy testing prior to initiation of fluorouracil. Women who become pregnant while receiving fluorouracil should be apprised of the potential hazard to the fetus. Although there are no data regarding the effect of fluorouracil on human fertility, male and female infertility has been observed in animal studies.[70470]
Use systemic fluorouracil with caution in patients with a history of coronary artery disease (CAD). Based on postmarketing reports, fluorouracil can cause cardiotoxicity including angina, myocardial infarction/ischemia, arrhythmia, and heart failure; patients receiving fluorouracil via continuous infusion are at increased risk compared to those receiving an IV bolus, as well as patients with CAD. Interrupt fluorouracil therapy if cardiotoxicity occurs; the safety of resuming therapy in patients with cardiotoxicity has not been established.[70470]
Due to the potential for serious adverse reactions in nursing infants from fluorouracil, a decision should be made whether to discontinue breast-feeding or discontinue the drug, taking into account the importance of the drug to the mother. It is not known whether fluorouracil is present in human milk, although many drugs are excreted in human milk.[70470] [53825] [48332] [60171] [53831]
Fluorouracil (5-FU) is a pyrimidine antimetabolite that inhibits thymidylate synthase (TS) and also interferes with RNA synthesis and function. Fluorouracil also has some effects on DNA.
•RNA-related effects: Formation of fluorouracil monophosphate (FUMP) occurs through two different pathways. FUMP may be formed as the result of direct transfer of a ribose sugar from phosphoribosylpyrophosphate (PPRP) to 5-FU via orotic acid phosphoribosyltransferase (OPRTase). In the second pathway, a ribose sugar is added to 5-FU by uridine phosphorylase forming fluorouridine (FUrd). FUrd undergoes phosphorylation by uridine kinase to form fluorouracil monophosphate (FUMP). Flurouridine diphosphate (FUDP) and flurouridine triphosphate (FUTP) are formed due to the sequential activity of pyrimidine monophosphate kinase and pyrimidine diphosphate kinase on FUMP. The FUTP is then incorporated into RNA and inhibits RNA activity and synthesis.
•DNA-related effects: Fluorouracil can be converted to fluorodeoxyuridine (FdUrd) by thymidine phosphorylase and then fluorodeoxyuridine monophosphate (FdUMP) by thymidine kinase. As a secondary pathway, FdUMP may be formed indirectly by the conversion of FUDP to fluorodeoxyuridine diphosphate (FdUDP) and then to FdUMP. FdUMP forms a tight, but reversible, covalent bond with thymidylate synthase (TS) in the presence of methylenetetrahydrofolate (CH2-THF), a natural reduced folate. Binding of FdUMP to TS inhibits the formation of thymidylate from uracil. Thymidylate is the necessary precursor of thymidine triphosphate (dTTP), one of four deoxyribonucleotides required for synthesis of DNA. Thus, a deficiency of thymidylate leads to depletion of dTTP. Both FdUMP and FdUDP may be converted to fluorodeoxyuridine (FdUTP), which can be incorporated into DNA by DNA polymerase in place of dTTP. When given in combination with leucovorin, the DNA-effects of 5-FU are enhanced through stabilization of the ternary complex of TS, FdUMP, and CH2-THF.
•Cytotoxicity: During the first 24 hours after drug exposure, S-phase cytotoxicity is noted, probably due to 5-FU-induced DNA effects. After 24 hours, cytotoxicity occurs primarily in the G1-phase of the cell cycle probably due to incorporation of 5-FU into RNA. The selectivity of 5-FU for rapidly dividing cells is due to the higher concentrations of thymidylate synthase (TS) in dividing cells, up to 20-fold, versus non-proliferating cells.
Resistance to 5-FU therapy may be due to a variety of mechanisms due to the complex effects of 5-FU. Deletion or decreased activity of various activating enzymes, decreased availability of cofactors (i.e., PRPP), competition with natural substrates (i.e., uracil triphosphate and dTTP), and increased activity of enzymes associated with the catabolism of 5-FU to inactive compounds (i.e., dihydropryrimidine dehydrogenase) may all play a role in the development of chemotherapy resistance.
Revision Date: 10/07/2025, 07:41:13 PMFluorouracil (5-FU) is administered topically or parenterally. Due to low and inconsistent oral bioavailability, 5-FU is not given orally. The drug distributes widely throughout the body tissues and crosses the blood-brain barrier to a significant degree. CSF concentrations can be sustained for several hours. Fluorouracil also distributes well into ascites and pleural effusions; delayed elimination from these fluid reservoirs could prolong toxicity. Fluorouracil exhibits nonlinear kinetics. With increasing IV doses of 5-FU, hepatic extraction ratio is decreased, bioavailability and AUC are increased, total-body clearance is decreased, and elimination half-life is increased. Although changes in 5-FU clearance or AUC with increasing 5-FU dose may be linear over a certain dose range, with higher doses the decrease in clearance and increase in AUC may change disproportionately. This nonlinearity probably represents saturation of metabolic processes at higher drug concentrations. A small portion of fluorouracil is converted to active metabolites (FdUMP, FUTP) in the tissues; the rest (85%) is catabolized via dihydropryrimidine dehydrogenase (DPD), the initial rate-limiting step, and other enzymes to the dihydropyrimidine form. DPD is widely distributed through out the body including the liver, gastrointestinal mucosa, and peripheral white blood cells. The liver is the major site of 5-FU catabolism. However, during continuous infusion of 5-FU the clearance of 5-FU exceeds liver blood flow indicating significant extrahepatic metabolism. DPD plays a critical role in determining the amount of 5-FU available for anabolism, and therefore, may in part determine the efficacy and/or toxicity of 5-FU therapy. DPD follows a circadian pattern and exhibits significant interpatient variability in terms of activity. The circadian variation of DPD levels is associated with an inverse circadian pattern in plasma 5-FU patterns. Individuals with low or nonexistent DPD activity experience severe toxicity when treated with conventional doses of 5-FU. It also appears this interpatient variability in DPD activity is responsible for the variable bioavailability following oral administration of 5-FU.[26297] Following IV administration of fluorouracil, the mean elimination half-life from plasma is 16 minutes (range: 8—20 minutes) and is dose dependent. In contrast to the parent compound, the intracellular nucleotides FdUMP and FUTP have prolonged half-lives. A small amount of unchanged 5-FU and primarily its metabolites are eliminated via the biliary and renal systems. Seven to 20 percent of 5-FU is renally excreted unchanged.[29028]
After a 12 hour application of 1 g of topical fluorouracil, 5-FU to the head and neck, approximately 6% of the dose was absorbed systemically.[53825] In a multiple-dose pharmacokinetic study in which 10 patients received the 0.5% topical cream at a dose of 1 g once daily (Carac) and 10 patients received the 5% topical cream (Efudex) at a dose of 1 g twice daily, 3 patients receiving the 0.5% cream and 9 patients receiving the 5% cream had measurable plasma concentrations. However, only 1 patient receiving the 0.5% cream and 6 patients receiving the 5% cream had sufficient data points to calculate mean pharmacokinetic parameters. The Tmax occurred at about 1 hour in both groups. The Cmax for the 0.5% cream (n = 1) was 0.77 ng/mL and AUC was 2.8 ng x hr/mL. The Cmax for the 5% cream (n = 6) was 11.49 +/- 8.24 ng/mL and the AUC was 22.39 +/- 7.89 ng x hr/mL.[48332] In a study of the 4% topical cream (Tolak, n = 21) in patients with at least 3 actinic keratosis lesions (4 mm or greater in diameter), steady state plasma concentrations were obtained at 1, 2, 4, 6, 8, 10, 12, 16, and 24 hours after the last dose of a 4-week regimen. Eight patients had undetectable plasma concentrations (lower limit of 1 ng/mL) in all plasma samples. In patients with detectable 5-FU concentrations, the highest concentration was generally observed at 1 hour after the administered dose with a mean observed maximum concentration of 3.66 +/- 1.58 ng/mL and a range of 1.11 to 7.35 ng/mL.[60171]
Regional Administration
Following hepatic artery infusion (HAI) of 5-FU, 19—51% of the infused dose was cleared during first-pass hepatic metabolism. Systemic exposure of 5-FU following HAI has been reported to be 12—52% that of after IV administration; systemic exposure increases with increasing 5-FU doses. 5-FU may be given by the intraperitoneal route. The advantage of regional administration is that low molecular weight products, such as 5-FU, are absorbed primarily through the portal circulation, passing through the liver before reaching the systemic circulation.
Fluorouracil has been administered to patients with hepatic insufficiency without dose reduction; however, dose reduction may be prudent in patients with serum bilirubin > 5 mg/dl and poor performance status.
Patients with renal insufficiency and normal activity of DPD do not require 5-FU dosage adjustments.
Topical fluorouracil is contraindicated during pregnancy.[48332] [53825] [60498] [60499] Pregnancy should be avoided by females of reproductive potential during treatment with systemic fluorouracil and for up to 3 months after the last dose. Although there are no adequately controlled studies in pregnant women, fluorouracil can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. Women who are pregnant or who become pregnant while receiving fluorouracil should be apprised of the potential hazard to the fetus. When administered as an intraperitoneal injection during organogenesis, malformations including cleft palate, skeletal defects, and deformed paws and tails were observed in mice at doses approximately 0.06 times a human dose of 12 mg/kg for 4 days; delayed growth and malformations including microanophthalmos occurred with a single intraperitoneal dose approximating 0.2 times a human dose of 12 mg/kg to rats during organogenesis. Intramuscular fluorouracil administration to hamsters at lower doses than those used in common treatment regimens had similar results. Fluorouracil administration to monkeys during organogenesis resulted in abortion at doses approximately equal to a human dose of 12 mg/kg; decreasing the dose by half resulted in increased resorptions and decreased fetal body weight.[70470] One birth defect (cleft lip and palate) has been reported in the newborn of a patient using topical fluorouracil as recommended. Miscarriages and birth defects (ventricular septal defects) have been reported when topical fluorouracil was applied to mucous membranes during pregnancy. The amount of fluorouracil absorbed systemically after topical administration to actinic keratoses is minimal.[48332] [53825] [60498] [60499]
Due to the potential for serious adverse reactions in nursing infants from fluorouracil, a decision should be made whether to discontinue breast-feeding or discontinue the drug, taking into account the importance of the drug to the mother. It is not known whether fluorouracil is present in human milk, although many drugs are excreted in human milk.[70470] [53825] [48332] [60171] [53831]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.