ThisiscontentfromElsevier'sDrugInformation
Ganciclovir
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
5 mg/kg/dose IV every 12 hours plus IV foscarnet (to stabilize the disease and maximize response). Optimal duration has not been established; however, continue treatment until there is symptomatic improvement and viral eradication.[34213] [34361] [34362] [69330] [69331]
5 mg/kg/dose IV every 12 hours plus IV foscarnet (to stabilize the disease and maximize response). Optimal duration has not been established; however, continue treatment until there is symptomatic improvement and viral eradication.[34213] [34361] [34362] [69330] [69331]
5 mg/kg/dose IV every 12 hours plus IV foscarnet (to stabilize the disease and maximize response). Optimal duration has not been established; however, continue treatment until there is symptomatic improvement and viral eradication.[34213] [34361] [69330] [69331] Follow with secondary prophylaxis (i.e., long-term suppressive therapy) in persons with HIV.[34361]
6 mg/kg/dose IV every 12 hours; dosage adjustments for the development of neutropenia may be required. Change to oral valganciclovir as soon as feasible to complete 6 months of treatment. Treatment for 6 months may result in improved audiologic and neurodevelopmental outcomes.[32656] [34361] [45501] [61213] [69309] [70821]
5 mg/kg/dose IV every 12 hours for at least 3 weeks and until clearance of HHV-6B DNA from blood and CSF. Consider combining with foscarnet.[34213] [72344] [72346] [72347] [72350]
5 mg/kg/dose IV every 12 hours for at least 3 weeks and until clearance of HHV-6B DNA from blood and CSF. Consider combining with foscarnet.[34213] [72344] [72346] [72347] [72350]
5 mg/kg/dose IV every 12 hours.[69333] Treat for 14 to 21 days.[34213] [67800] [69333]
5 mg/kg/dose IV every 12 hours.[52560] Treat for 14 to 21 days.[34213] [67801]
6 mg/kg/dose IV every 12 hours.[52560] Treat for 21 days.[34213] [67801]
6 mg/kg/dose IV every 12 hours.[52560] Treat for 21 days.[34213] [67801]
5 mg/kg/dose IV every 12 hours.[34213] Treat for 10 to 14 days.[34213] [67800]
5 mg/kg/dose IV every 12 hours.[34213] [52560] Treat for 10 to 14 days.[34213] [67801]
6 mg/kg/dose IV every 12 hours.[34213] [52560] Treat for 10 to 14 days.[34213] [67801]
5 mg/kg/dose IV every 12 hours for a minimum of 14 days or until all CNS symptoms have resolved.[34213]
5 mg/kg/dose IV every 12 hours for 14 to 21 days. For immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea), give in combination with intravitreal injections of ganciclovir or foscarnet. Follow induction therapy with chronic maintenance therapy (secondary prophylaxis).[32676] [34362]
5 mg/kg/dose IV every 12 hours for 14 to 21 days. For immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea), give in combination with intravitreal injections of ganciclovir or foscarnet. Follow induction therapy with chronic maintenance therapy (secondary prophylaxis).[34362]
5 to 7.5 mg/kg/dose IV every 12 hours for 14 to 21 days. Consider addition of IV foscarnet for immediate sight-threatening lesions. Although intravitreal injections of foscarnet and ganciclovir are recommended in adults and adolescents, they are not practical for most children. Follow induction therapy with chronic maintenance therapy (secondary prophylaxis).[34361]
2 mg intravitreally once weekly until lesion inactivity is achieved for patients with immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea). Intravitreal injections are given to achieve rapid high intraocular drug concentrations and should be administered in combination with systemic induction therapy.[34362]
2 mg intravitreally once weekly until lesion inactivity is achieved for patients with immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea). Intravitreal injections are given to achieve rapid high intraocular drug concentrations and should be administered in combination with systemic induction therapy.[34362]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease. For immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea), give in combination with intravitreal injections of ganciclovir or foscarnet.[34362] [69330] [69334] [69356] [70682] [70690] [70694] [70698]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease. For immediate sight-threatening lesions, give with intravitreal injections of ganciclovir or foscarnet. For immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea), give in combination with intravitreal injections of ganciclovir or foscarnet.[34362] [69330] [69334] [69356] [70682] [70690] [70694] [70698] [70699] [70700] [70704]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease.[69330] [69334] [69356] [70682] [70694] [70699] [70700] [70704]
2 mg intravitreally once weekly until lesion inactivity is achieved for patients with immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea). Intravitreal injections are given to achieve rapid high intraocular drug concentrations and should be administered in combination with systemic induction therapy.[34362] [70698]
2 mg intravitreally once weekly until lesion inactivity is achieved for patients with immediate sight-threatening lesions (i.e., within 1,500 microns of the fovea). Intravitreal injections are given to achieve rapid high intraocular drug concentrations and should be administered in combination with systemic induction therapy.[34362] [70698]
5 mg/kg/dose IV every 12 hours for 21 to 42 days or until resolution of signs and symptoms; when patient can tolerate PO, switch to oral valganciclovir to complete therapy. Maintenance therapy is usually not necessary, but should be considered after relapse.[34362]
5 mg/kg/dose IV every 12 hours for 21 to 42 days or until resolution of signs and symptoms; when patient can tolerate PO, switch to oral valganciclovir to complete therapy. Maintenance therapy is usually not necessary, but should be considered after relapse.[34362]
5 to 7.5 mg/kg/dose IV every 12 hours for 21 to 42 days or until resolution of signs and symptoms; when patient can tolerate PO, switch to oral valganciclovir to complete therapy. Maintenance therapy is usually not necessary, but should be considered after relapse.[34361] [34362]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease.[69330] [69334] [69356] [70682] [70694]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease.[69330] [69334] [69356] [70682] [70694] [70699] [70700] [70704]
5 mg/kg/dose IV every 12 hours for 14 to 21 days, then 5 mg/kg/dose IV once daily. Optimal duration has not been established.[34362]
5 mg/kg/dose IV every 12 hours for 14 to 21 days, then 5 mg/kg/dose IV once daily. Optimal duration has not been established.[34362]
5 to 7.5 mg/kg/dose IV every 12 hours for 14 to 21 days, then 5 mg/kg/dose IV once daily. Optimal duration has not been established.[34361] [34362]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease.[69330] [69334] [69356] [70682] [70694] Consider the addition of intravenous immune globulin.[69330] [69334] [69356] [70682]
5 mg/kg/dose IV every 12 hours for at least 2 weeks, and until clinical resolution of disease and virologic clearance. Doses up to 10 mg/kg/dose IV every 12 hours have been used for refractory or resistant disease.[69330] [69334] [69356] [70682] [70694] [70699] [70700] [70704] Consider the addition of intravenous immune globulin.[69330] [69334] [69356] [70682] [70700]
NOTE: Treatment is recommended for neonates with moderately to severely symptomatic CMV disease, with or without CNS involvement, and asymptomatic neonates with isolated sensorineural hearing loss.[69309] [70821] Treatment should be initiated within the first 13 weeks following birth.[70821]
NOTE: Oral valganciclovir is the first line drug for the entire treatment course because drug exposure after appropriate dosing of valganciclovir is the same as that achieved with intravenous ganciclovir. However, intravenous ganciclovir can be used initially if an infant is unable to absorb medications reliably from the gastrointestinal tract (i.e., necrotizing enterocolitis or other bowel disorders).[61213] [69309] [70821]
6 mg/kg/dose IV every 12 hours; dosage adjustments for the development of neutropenia may be required. Change to oral valganciclovir as soon as feasible to complete 6 months of treatment. Treatment for 6 months may result in improved audiologic and neurodevelopmental outcomes.[32656] [34361] [45501] [61213] [69309] [70821]
6 mg/kg/dose IV every 12 hours; dosage adjustments for the development of neutropenia may be required. Change to oral valganciclovir as soon as feasible to complete 6 months of treatment. Treatment for 6 months may result in improved audiologic and neurodevelopmental outcomes.[32656] [34361] [45501] [61213] [69309] [70821]
6 mg/kg/dose IV every 12 hours; dosage adjustments for the development of neutropenia may be required. Change to oral valganciclovir as soon as feasible to complete 6 weeks of treatment. Treatment for 6 weeks may result in improved audiologic outcomes.[70821]
6 mg/kg/dose IV every 12 hours; dosage adjustments for the development of neutropenia may be required. Change to oral valganciclovir as soon as feasible to complete 6 weeks of treatment. Treatment for 6 weeks may result in improved audiologic outcomes.[70821]
5 mg/kg/dose IV every 12 hours for 7 to 14 days, then 5 mg/kg/dose IV once daily for 7 days per week or 6 mg/kg/dose IV once daily for 5 days per week through day 100 to 120 post-transplant is the FDA-approved dosage.[32676] [69356] [70694] However, primary prophylaxis with ganciclovir is not routinely recommended in adults due to the risk of myelosuppression and availability of other first-line agents (i.e., letermovir).[70694]
5 mg/kg/dose IV once daily through day 100 post-transplant. Compared with adults, the use of primary prophylaxis with ganciclovir is more common in pediatrics and may be considered in select pediatric HCT recipients.[69356] [70694] [70699] [70700] [70704]
5 mg/kg/dose IV once daily starting within 10 days of transplantation. Continue prophylaxis for 3 to 12 months depending on serostatus, risk level, and specific transplant.[69330] [70682] The FDA-approved dosage is 5 mg/kg/dose IV every 12 hours for 7 to 14 days, then 5 mg/kg/dose IV once daily for 7 days per week or 6 mg/kg/dose IV once daily for 5 days per week.[32676]
5 mg/kg/dose IV once daily starting within 10 days of transplantation. Continue prophylaxis for 3 to 12 months depending on serostatus, risk level, and specific transplant.[69330] [70682] [70704]
5 mg/kg/dose IV every 12 hours for at least 2 weeks and until CMV detection methods are negative or viral load has declined to below a predefined threshold. Alternatively, if viral load is decreasing after 1 to 2 weeks, may change to maintenance dosing of 5 mg/kg/dose IV once daily until CMV detection methods are negative. After discontinuation of preemptive therapy (PET), secondary prophylaxis with valganciclovir or letermovir, or monitoring and PET, is recommended. For recurrent viremia, reinitiation of PET is recommended according to institution-defined viral load thresholds. Typically, the same agent used in the first course of PET can be used for a second course of PET.[69356] [70694]
5 mg/kg/dose IV every 12 hours for at least 2 weeks and until CMV detection methods are negative or viral load has declined to below a predefined threshold. Alternatively, if viral load is decreasing after 1 to 2 weeks, may change to maintenance dosing of 5 mg/kg/dose IV once daily until CMV detection methods are negative. After discontinuation of preemptive therapy (PET), secondary prophylaxis with valganciclovir, or monitoring and PET, is recommended. For recurrent viremia, reinitiation of PET is recommended according to institution-defined viral load thresholds. Typically, the same agent used in the first course of PET can be used for a second course of PET.[69356] [70694] [70699] [70700] [70704]
5 mg/kg/dose IV every 12 hours until CMV detection methods are negative or viral load has declined to below a predefined threshold.[69330] [70682]
5 mg/kg/dose IV every 12 hours until CMV detection methods are negative or viral load has declined to below a predefined threshold.[69330] [70682] [70704]
5 mg/kg/dose IV once daily after induction therapy; may switch to oral valganciclovir when the patient is clinically improving and there are no concerns about absorption. The FDA-approved dosage is 6 mg/kg/dose IV once daily for 5 days per week. For patients who experience progression of CMV retinitis while receiving maintenance therapy, re-induction treatment with the same drug used for maintenance followed by reinstitution of maintenance therapy is recommended. For patients with HIV who have had a sustained immune response to highly active antiretroviral therapy (i.e., CD4 counts greater than 100 cells/mm3 for 3 to 6 months), have been on CMV treatment for at least 3 to 6 months, and have no active lesions, secondary CMV retinitis prophylaxis may be discontinued after consultation with an ophthalmologist. Maintenance therapy should be restarted if subsequent CD4 counts drop to less than 100 cells/mm3, as relapse occurs most frequently in those patients whose counts decrease to less than 50 cells/mm3 after stopping treatment. However, because relapses may occur at any CD4 count, all patients who have had maintenance CMV therapy discontinued should continue to undergo regular ophthalmologic monitoring (every 3 months) for early detection of CMV relapse (as well as for immune reconstitution uveitis).[32676] [34362]
5 mg/kg/dose IV once daily after induction therapy; may switch to oral valganciclovir when the patient is clinically improving and there are no concerns about absorption. For patients who experience progression of CMV retinitis while receiving maintenance therapy, re-induction treatment with the same drug used for maintenance followed by reinstitution of maintenance therapy is recommended. For patients with HIV who have had a sustained immune response to highly active antiretroviral therapy (i.e., CD4 counts greater than 100 cells/mm3 for 3 to 6 months), have been on CMV treatment for at least 3 to 6 months, and have no active lesions, secondary CMV retinitis prophylaxis may be discontinued after consultation with an ophthalmologist. Maintenance therapy should be restarted if subsequent CD4 counts drop to less than 100 cells/mm3, as relapse occurs most frequently in those patients whose counts decrease to less than 50 cells/mm3 after stopping treatment. However, because relapses may occur at any CD4 count, all patients who have had maintenance CMV therapy discontinued should continue to undergo regular ophthalmologic monitoring (every 3 months) for early detection of CMV relapse (as well as for immune reconstitution uveitis).[34362]
5 mg/kg/dose IV once daily after induction therapy; may switch to oral valganciclovir for older children who can receive the adult dose based on BSA when the patient is clinically improving and there are no concerns about absorption. For patients who experience progression of CMV retinitis while receiving maintenance therapy, re-induction treatment with the same drug used for maintenance followed by reinstitution of maintenance therapy is recommended. Discontinuation of secondary prophylaxis may be considered in children who have received at least 6 months of highly active antiretroviral therapy with a sustained increase (more than 6 months) in CD4 percentage of at least 15% (pediatric patients younger than 5 years) or CD4 count more than 100 cells/mm3 (children 6 years and older). For retinitis, the decision to discontinue secondary prophylaxis should be made in consultation with an ophthalmologist. Routine follow-up (every 3 to 6 months) with an ophthalmologist is recommended. Restart maintenance therapy if CD4 percentage is less than 15% in pediatric patients younger than 5 years or if CD4 count is less than 100 cells/mm3 in children 6 years and older.[34361]
5 mg/kg/dose IV every 12 hours plus ganciclovir intravitreal injection and/or foscarnet intravitreal injection. The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34362]
5 mg/kg/dose IV every 12 hours plus ganciclovir intravitreal injection and/or foscarnet intravitreal injection. The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34362]
5 mg/kg/dose IV every 12 hours plus IV foscarnet plus ganciclovir intravitreal injection and/or foscarnet intravitreal injection. The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34361]
2 mg/0.05 mL intravitreal injection twice weekly, with or without foscarnet intravitreal injection, in combination with systemic therapy (i.e., ganciclovir or acyclovir). The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34362]
2 mg/0.05 mL intravitreal injection twice weekly, with or without foscarnet intravitreal injection, in combination with systemic therapy (i.e., ganciclovir or acyclovir). The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34362]
2 mg/0.05 mL intravitreal injection twice weekly, with or without foscarnet intravitreal injection, in combination with systemic therapy (i.e., acyclovir or ganciclovir plus foscarnet). The optimal duration has not been defined; duration should be determined clinically in consultation with an ophthalmologist.[34361]
5 mg/kg/dose IV every 12 hours for 3 weeks is recommended by the HIV guidelines.[34361] [34362]
5 mg/kg/dose IV every 12 hours may be useful as an adjunct to chemotherapy and antiretroviral therapy.[34361] [34362]
NOTE: Ganciclovir ophthalmic gel is an FDA-designated orphan drug for this indication.
1 drop in the affected eye(s) 5 times daily, approximately every 3 hours while awake, until corneal ulcer heals, then 1 drop in the affected eye(s) 3 times daily for 7 days.[36875]
1 drop in the affected eye(s) 5 times daily, approximately every 3 hours while awake, until corneal ulcer heals, then 1 drop in the affected eye(s) 3 times daily for 7 days.[36875]
2 mg/0.05 mL intravitreal injections given twice weekly until evidence of treatment response. Administer in combination with 10 to 14 days of IV acyclovir, then at least 14 weeks of oral valacyclovir is recommended by the HIV guidelines. Involvement of an experienced ophthalmologist is recommended.[34362]
2 mg/0.05 mL intravitreal injections given twice weekly until evidence of treatment response. Administer in combination with 10 to 14 days of IV acyclovir, then at least 14 weeks of oral valacyclovir is recommended by the HIV guidelines. Involvement of an experienced ophthalmologist is recommended.[34362]
NOTE: For CNS disease, see encephalitis.
5 mg/kg/dose IV every 12 hours. The American Academy of Pediatrics (AAP) recommends ganciclovir as the first line alternative when IV acyclovir is unavailable for herpes simplex/varicella zoster infections in immunocompromised hosts and patients unable to tolerate oral acyclovir or valacyclovir.[52560]
6 mg/kg/dose IV every 12 hours. The American Academy of Pediatrics (AAP) recommends ganciclovir as the first line alternative when IV acyclovir is unavailable in suspected or proven neonatal herpes simplex disease or herpes simplex/varicella zoster infections in immunocompromised hosts.[52560]
6 mg/kg/dose IV every 12 hours. The American Academy of Pediatrics (AAP) recommends ganciclovir as the first line alternative when IV acyclovir is unavailable in cases of suspected or proven neonatal herpes simplex disease.[52560]
10 mg/kg/day IV is FDA-approved maximum; however, doses up to 20 mg/kg/day IV have been used off-label; 5 drops/day ophthalmic gel in each affected eye.
10 mg/kg/day IV is FDA-approved maximum; however, doses up to 20 mg/kg/day IV have been used off-label; 5 drops/day ophthalmic gel in each affected eye.
Safety and efficacy have not been established for IV dosing; however, doses up to 20 mg/kg/day IV have been used off-label; 5 drops/day ophthalmic gel in each affected eye.
2 to 12 years: Safety and efficacy have not been established for IV dosing; however, doses up to 20 mg/kg/day IV have been used off-label; 5 drops/day ophthalmic gel in each affected eye.
1 year: Safety and efficacy have not been established; however, doses up to 20 mg/kg/day IV have been used off-label.
Safety and efficacy have not been established; however, doses up to 20 mg/kg/day IV have been used off-label.
Safety and efficacy have not been established; however, doses of 12 mg/kg/day IV have been used off-label.
No dosage adjustment necessary.
Modify dosage for intravenous induction therapy and maintenance therapy based on creatinine clearance (CrCl).
Adults:
Intravenous dosage adjustments (induction)
CrCl 70 mL/minute or more: no dosage adjustment needed.
CrCl 50 to 69 mL/minute: 2.5 mg/kg/dose IV every 12 hours.
CrCl 25 to 49 mL/minute: 2.5 mg/kg/dose IV every 24 hours.
CrCl 10 to 24 mL/minute: 1.25 mg/kg/dose IV every 24 hours.
CrCl less than 10 mL/minute: 1.25 mg/kg/dose IV 3 times a week after hemodialysis.
Intravenous dosage adjustments (maintenance)
CrCl 70 mL/minute or more: no dosage adjustment needed.
CrCl 50 to 69 mL/minute: 2.5 mg/kg/dose IV every 24 hours.
CrCl 25 to 49 mL/minute: 1.25 mg/kg/dose IV every 24 hours.
CrCl 10 to 24 mL/minute: 0.625 mg/kg/dose IV every 24 hours.
CrCl less than 10 mL/minute: 0.625 mg/kg/dose IV 3 times a week after hemodialysis.
Intermittent hemodialysis or Peritoneal dialysis
1.25 mg/kg/dose IV 3 times per week. Give all doses after dialysis sessions.[32569]
Continuous renal replacement therapy
Intravenous dosage adjustments (induction): 2.5 mg/kg/dose IV every 24 hours.
Intravenous dosage adjustments (maintenance): 1.25 mg/kg/dose IV every 24 hours.[32569]
Pediatrics:
Intravenous dosage adjustments (induction)
GFR 30 to 50 mL/minute/1.73 m2: 2.5 mg/kg/dose IV every 24 hours.
GFR 10 to 29 mL/minute/1.73 m2: 1.25 mg/kg/dose IV every 24 hours.
GFR less than 10 mL/minute/1.73 m2: 1.25 mg/kg/dose IV 3 times a week.[32569]
Intravenous dosage adjustments (maintenance)
GFR 30 to 50 mL/minute/1.73 m2: 1.25 mg/kg/dose IV every 24 hours.
GFR 10 to 29 mL/minute/1.73 m2: 0.625 mg/kg/dose IV every 24 hours.
GFR less than 10 mL/minute/1.73 m2: 0.625 mg/kg/dose IV 3 times a week.[32569]
Intermittent hemodialysis or Peritoneal dialysis
Give all doses after dialysis sessions.
Intravenous dosage adjustments (induction): 1.25 mg/kg/dose IV 3 times per week.
Intravenous dosage adjustments (maintenance): 0.625 mg/kg/dose IV 3 times per week.[32569]
Continuous renal replacement therapy
Intravenous dosage adjustments (induction): 2.5 mg/kg/dose IV every 24 hours.
Intravenous dosage adjustments (maintenance): 1.25 mg/kg/dose IV every 24 hours.[32569]
† Off-label indication


Ganciclovir is a synthetic, purine nucleoside analog used for the treatment and prevention of cytomegalovirus (CMV) infections. An ophthalmic gel is used for the treatment of herpetic keratitis.[32676] In addition, ganciclovir has been shown to be active against other viruses, including herpes simplex, varicella zoster, and human herpesvirus 6 and 8.[34362] Hematologic toxicity is common with systemic ganciclovir administration; dosage adjustments for neutropenia or thrombocytopenia may be required. The FDA originally approved intravenous ganciclovir in June 1989. Ganciclovir ophthalmic gel (Virgan) was given an orphan drug designation for acute herpetic keratitis in April 2007 and was granted full approval (Zirgan) in September of 2009.[36875][32676] Ganciclovir oral capsules and intraocular implant were withdrawn from the US market in 2013.
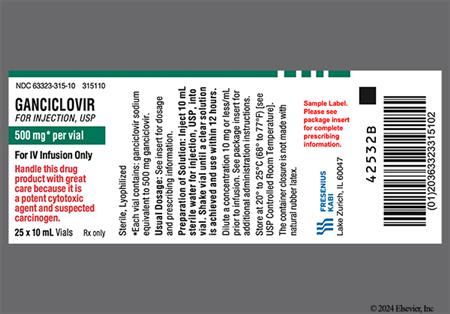
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Reconstitution
Dilution
Premixed IV solution
Intermittent IV Infusion
Intravitreal Injection†
NOTE: Ganciclovir is not approved by the FDA for intravitreal administration.
Ganciclovir can cause significant bone marrow suppression. Anemia (2% to 26%), neutropenia (3% to 29%), pancytopenia, leukopenia (29% to 41%), thrombocytopenia (3% to 57%), and bone marrow failure can all occur. In addition, hemolytic anemia, agranulocytosis, and granulocytopenia have been noted during postmarketing reports.[32676] Related symptoms can include unusual bleeding or bruising. Both granulocytopenia and thrombocytopenia are usually reversible and respond to a dose reduction. Use of the drug is not recommended in patients with neutropenia defined as an absolute neutrophil count (ANC) less than 500 cells/mm3, anemia with hemoglobin less than 8 g/dL, or thrombocytopenia with a platelet count less than 25,000 cells/mm3. In neonates, ganciclovir therapy has been resumed when ANC is 750 cells/mm3 or more; then after treatment re-initiation, the dose is reduced to one-half if subsequent ANC is less than 500/mm3, and therapy discontinued if neutropenia persisted while on the reduced dose.[32656] The incidence of hematologic reactions may be higher in bone marrow transplant patients and less in other transplant patients. The hematologic toxicity usually develops within the early weeks of therapy and is generally dose-related and reversible, but occasionally it can be prolonged or irreversible. Blood counts usually begin to recover within 3 to 7 days of discontinuing the drug. Colony-stimulating factors have been shown to increase neutrophil counts in patients receiving ganciclovir.[32676]
The most common gastrointestinal adverse effects of systemic ganciclovir include abdominal pain, anorexia (14% to 15%), diarrhea (41% to 44%), nausea, vomiting (13%), dysgeusia, and flatulence. Other GI-related adverse events include aphthous stomatitis, constipation, dyspepsia, eructation, GI perforation, pancreatitis, weight loss, and xerostomia (dry mouth). Intestinal ulceration was noted during postmarketing surveillance.[32676]
Adverse CNS effects are fairly common during systemic ganciclovir therapy and include abnormal dreams, anxiety, confusion, depression, dizziness, headache, insomnia, drowsiness and fatigue, dysphagia, hypoesthesia, abnormal thinking, paresthesias, peripheral neuropathy (8% to 9%), tremor, or more serious reactions such as seizures.[32676] Very few cases of ganciclovir-induced seizures have been reported.[23647] Other adverse events noted during postmarketing surveillance include dysesthesia, dysphasia, aphasia, encephalopathy, extrapyramidal reaction, facial palsies or cranial nerve palsies, hallucinations, increased intracranial pressure, irritability, loss of memory and memory impairment, oculomotor nerve paralysis, and stroke.[32676] Some CNS adverse effects have been caused by opportunistic infection rather than by the drug.
Systemic ganciclovir is moderately nephrotoxic. Mild to moderate increases in serum creatinine have been reported during therapy. In general, this adverse reaction occurs during the first week of therapy and is reversible. If renal function worsens during therapy, the ganciclovir dosage should be reduced since ganciclovir is extensively eliminated unchanged via glomerular filtration. Individuals receiving ganciclovir following transplantation seem to have a higher incidence of nephrotoxicity as compared to individuals treated for CMV retinitis. Between 12% to 58% of individuals may experience serum creatinine concentrations of 1.5 to 2.4 mg/dL; serum creatinine concentrations of 2.5 mg/dL or more may be seen in up to 20% of patients. Renal failure (unspecified), decreased creatinine clearance, abnormal renal function, hematuria, increased urinary frequency, and urinary retention have also been reported with ganciclovir therapy. Hemolytic uremic syndrome and renal tubular disorder were noted in postmarketing reports.[32676]
Dermatologic and allergic adverse effects reported during ganciclovir therapy include alopecia, hyperhidrosis (11% to 12%), pruritus (5% to 6%), dermatitis, rash (unspecified), urticaria, and xerosis (dry skin). Phlebitis or injection site reaction (e.g., local inflammation, pain) can occur with IV ganciclovir. Rash, pruritus, or urticaria may indicate hypersensitivity to ganciclovir. Allergic reaction, anaphylactoid reactions, exfoliative dermatitis, and Stevens-Johnson syndrome have been noted in postmarketing reports.[32676]
Ganciclovir is considered a potential carcinogen in humans and may cause a new primary malignancy. Ganciclovir has been associated with clastogenesis during in vitro testing at doses 2.8- to 10-times the normal human dose but not at doses comparable to human exposure. Tumors have developed in mice treated with approximately one-tenth to 1.4 times the human dose. Most tumors were of epithelial or vascular origin, although histiocytic sarcoma of the liver was reported. Tumors appeared in some tissues for which there is no human counterpart.[32676]
Animal and limited human data indicate that ganciclovir may cause temporary or permanent spermatogenesis inhibition and subsequent infertility in males and suppression of fertility in females. Effects on spermatogenesis were reversible at lower doses and irreversible at higher doses. In addition, ganciclovir causes teratogenesis in animals and should not be used during pregnancy. Advise women of childbearing potential about the necessity of using effective contraception during treatment. Females should use effective contraception during and for at least 30 days after treatment with ganciclovir. Males must practice barrier contraception during and for at least 90 days after treatment with ganciclovir.[28463] [32676]
Infection (9% to 13%), sepsis (4% to 15%), catheter-related infection (4% to 9%), and catheter-related sepsis (1% to 8%) were reported during ganciclovir clinical trials. Other, less frequently reported infections included cellulitis, influenza, upper respiratory tract infections, urinary tract infections, and candida infections including oral candidiasis.[32676]
General adverse events associated with the use of systemic ganciclovir include fever (38% to 48%), chills (7% to 10%), enlarged abdomen, asthenia, chest pain (unspecified), congenital anomaly, edema, malaise, unspecified pain, testicular hypotrophy/testicular atrophy, and potentially fatal multiple organ failure.[32676]
Elevated hepatic enzymes were reported with the use of systemic ganciclovir. Hepatic failure, cholelithiasis, cholestasis, and hepatitis were noted during postmarketing reports.[32676]
Tinnitus, otalgia, and hearing loss (deafness) were reported with the use of systemic ganciclovir. Loss of the sense of smell (anosmia) was noted during postmarketing reports.[32676]
Increased cough and dyspnea were reported with systemic ganciclovir. Bronchospasm and pulmonary fibrosis were noted during postmarketing reports.[32676]
Arthralgia, muscle cramps, muscle spasms, back pain, myalgia, and myasthenia have been reported with the use of systemic ganciclovir. Other adverse events noted during postmarketing surveillance include arthritis, myelopathy, and rhabdomyolysis.[32676]
Hypertension, hypotension, arrhythmia exacerbation, and peripheral vasodilation were reported with the use of systemic ganciclovir. Other cardiovascular adverse events reported during postmarketing surveillance include cardiac arrest, cardiac conduction abnormalities, peripheral ischemia, torsade de pointes, vasculitis, and ventricular tachycardia.[32676]
Retinal detachment may occur with systemic (8% to 11% of adults) administration of ganciclovir; however, the precise relationship to the drug is not clear. Retinal detachment has occurred in patients with CMV retinitis both before and after initiation of ganciclovir therapy.[32676] Adverse reactions associated with administration of ganciclovir ophthalmic gel include blurred vision (60%), ocular irritation (20%), punctate keratitis (5%), and conjunctival hyperemia (5%).[36875] Other ocular reactions noted with systemic ganciclovir include abnormal vision or visual impairment, ocular pain, conjunctivitis, macular edema, and vitreous disorder. Xerophthalmia and cataracts were noted in postmarketing reports with systemic ganciclovir.[32676]
Metabolic adverse events noted during postmarketing surveillance with ganciclovir include metabolic acidosis, hypertriglyceridemia, hypercalcemia, hyponatremia, and syndrome of inappropriate antidiuretic hormone secretion (SIADH).[32676]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. It is also contraindicated in patients who have experienced a clinically significant hypersensitivity reaction to valganciclovir.[32676][61771] Although not specifically contraindicated by the manufacturer, ganciclovir ophthalmic gel should be used with extreme caution in these patients as well. Because of similar chemical structures and possible cross-sensitivity, ganciclovir should not be used in patients with hypersensitivity to famciclovir, penciclovir, acyclovir, or valacyclovir. Alternative agents such as foscarnet or cidofovir may be suitable since they are not structurally related to these antivirals.
The use of systemic ganciclovir has been associated with hematologic toxicity including granulocytopenia, anemia, thrombocytopenia, and pancytopenia. The frequency and severity of these events vary widely in different patient populations. Use caution when administering ganciclovir to patients with preexisting cytopenias (anemia, neutropenia, thrombocytopenia, pancytopenia) and in patients receiving radiation therapy, chemotherapy, or other myelosuppressive medications. Complete blood counts with differential and platelet counts should be performed frequently in all patients, especially in patients in whom ganciclovir or other nucleoside analogs have previously resulted in cytopenias or in whom the baseline absolute neutrophil counts (ANC) are less than 1,000 cells/mm3. Avoid use of the drug in patients with an ANC less than 500 cells/mm3, hemoglobin less than 8 g/dL, or platelet count less than 25,000 cells/mm3.[32676] [61771]
Dose adjustments are required when administering systemic ganciclovir to patients with renal impairment, including those with renal failure and who are on dialysis. Ensure patients remain adequately hydrated and monitor renal function during therapy. Increased serum creatinine concentrations have been observed in geriatric drug recipients and in transplant patients receiving concomitant nephrotoxic medications.[32676] [61771]
Although human data are not available, the development of new primary malignancy is a potential risk to consider during ganciclovir therapy based on animal mutagenic and carcinogenic data. Ensure proper handling and disposal procedures for cytotoxic drugs are followed.[32676] [61771]
Ganciclovir is associated with reproductive risk. The drug can be teratogenic if taken by the father near the time of conception (male-mediated teratogenicity) or by the mother during pregnancy. Discuss contraception requirements with the patient. Females should use effective contraception during and for at least 30 days after treatment with ganciclovir. Males must use a condom during and for at least 90 days after treatment. Females of reproductive potential should undergo pregnancy testing prior to initiation of ganciclovir. In addition, based on animal and limited human data, ganciclovir may cause temporary or permanent inhibition of spermatogenesis and subsequent infertility. Animal studies also indicate that suppression of fertility in females may occur.[32676]
There are no adequate and well-controlled human studies evaluating use of ganciclovir during pregnancy; however, based on data from animal studies, ganciclovir may be teratogenic or embryotoxic at doses recommended for human use. If considering use of ganciclovir in a pregnant female, consider that most maternal CMV infections are subclinical or may be associated with mononucleosis-like syndrome. However, in immunocompromised patients, CMV infections are often symptomatic and associated with significant morbidity and mortality. Also consider that the risk and severity of congenital CMV infection appear to be higher in infants born to mother with primary CMV infection than in those born to mothers with reactivation of the disease. Of the newborns who are infected with CMV, only 10% are symptomatic at birth and the mortality rate among symptomatic infants is about 10%; however, approximately 50% to 90% of the surviving infants may experience significant problems, including sensorineural hearing loss, mental retardation, and other neurologic defects. It is not known if topically administered ophthalmic ganciclovir could result in significant systemic absorption; therefore, the manufacturer recommends the administration of ophthalmic ganciclovir to pregnant women only if the potential benefit to the mother outweighs the potential risk to the fetus.[32676] [36875] [61771]
It is not known if ganciclovir is excreted into breast milk. Due to the potential for serious adverse reactions in nursing infants, the manufacturer recommends instructing mothers to stop or not to start breast-feeding if they are receiving ganciclovir. Additionally, ganciclovir may be used to treat infections in patients with HIV and the Centers for Disease Control and Prevention (CDC) recommends that in the US, HIV-infected mothers not breast-feed their infants to avoid the risk of postnatal transmission of HIV. It is not known if topically administered ophthalmic ganciclovir could result in sufficient systemic absorption to produce detectable quantities in breast milk; therefore, the manufacturer recommends caution if ophthalmic ganciclovir is administered to breast-feeding women. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested or administered drug, health care providers are encouraged to report the adverse effect to the FDA.[32676] [36875] [46675]
Ganciclovir is a synthetic analog of 2'-deoxyguanosine and inhibits the replication of human cytomegalovirus (CMV). In CMV-infected cells, ganciclovir is initially phosphorylated to ganciclovir monophosphate by the viral protein kinase pUL97. Further phosphorylation by protein kinases produces ganciclovir triphosphate. Ganciclovir triphosphate inhibits viral DNA synthesis by competitive inhibition of viral DNA polymerases and incorporation into viral DNA resulting in eventual termination of viral DNA elongation. Since phosphorylation is dependent upon viral protein kinases, ganciclovir is preferentially metabolized in virus-infected cells. Ganciclovir triphosphate concentrations may be 100-fold greater in CMV-infected cells than in uninfected cells. As sensitivity tests vary due to many factors, the concentration of ganciclovir to inhibit the growth of virus in cell culture by 50% (IC50) ranges from 0.02—3.48 mcg/mL. Ganciclovir inhibits mammalian cell proliferation (CIC50) in vitro at higher concentrations ranging from 30—725 mcg/mL; however, bone marrow cells are more sensitive (CIC50 0.028—0.7 mcg/mL).
Resistance to ganciclovir may occur after prolonged treatment with valganciclovir by selection of mutations in either the viral protein kinase (UL97) and/or in the viral polymerase gene (UL54). Virus with mutations in the UL97 gene is resistant to ganciclovir alone, whereas virus with mutations in the UL54 gene may show cross-resistance to other antiviral agents with a similar mechanism of action. The current definition of CMV resistance to ganciclovir in vitro is IC50 >= 1.5 mcg/mL. CMV resistance to ganciclovir has been observed in individuals with AIDS and CMV retinitis who have never received ganciclovir therapy.
Revision Date: 08/20/2025, 01:32:00 AMGanciclovir is administered intravenously, by topical ophthalmic administration, and by intravitreal injection. Ganciclovir crosses the blood-brain barrier, producing CSF concentrations that average about 40% (range 24% to 70%) of plasma concentrations. Ganciclovir crosses the placenta. It is not known if ganciclovir is excreted into breast milk. Protein binding is roughly 1% to 2%. Ganciclovir undergoes little or no metabolism. Ganciclovir is excreted primarily in the urine, with about 90% excreted unchanged by glomerular filtration and active tubular secretion.[32676]
Affected cytochrome P450 isoenzymes: none
Following IV administration of ganciclovir, distribution into body tissues and fluids is extensive including significant intraocular penetration. The half-life in patients with normal renal function is about 3.5 hours following IV administration.[32676]
Ophthalmic Route
Minimal systemic exposure is expected with topical ophthalmic administration of ganciclovir gel.[36875]
Half-life of ganciclovir increases in patients with impaired renal function. Patients with an estimated creatinine clearance < 25 mL/minute achieved a mean half-life of 10.7 hours. Hemodialysis reduces ganciclovir concentrations by about 50%.[32676]
The pharmacokinetics of IV ganciclovir in pediatric patients are similar to those seen in adults.
Infants, Children, and Adolescents
The Cmax, systemic clearance, and half-life of ganciclovir in 10 infants and children (9 months to 12 years of age) after doses of 5 mg/kg IV were 7.9 mcg/mL, 4.7 mL/minute/kg, and 2.4 hours, respectively.[32676]
Neonates
The Cmax, systemic clearance, and half-life of ganciclovir in 27 neonates (2 to 49 days postnatal age, gestational age not specified) after doses of 4 to 6 mg/kg IV were 5.5 to 7 mcg/mL, 3.14 to 3.56 mL/minute/kg, and 2.4 hours, respectively.[32676]
There are no adequate and well-controlled human studies evaluating use of ganciclovir during pregnancy; however, based on data from animal studies, ganciclovir may be teratogenic or embryotoxic at doses recommended for human use. If considering use of ganciclovir in a pregnant female, consider that most maternal CMV infections are subclinical or may be associated with mononucleosis-like syndrome. However, in immunocompromised patients, CMV infections are often symptomatic and associated with significant morbidity and mortality. Also consider that the risk and severity of congenital CMV infection appear to be higher in infants born to mother with primary CMV infection than in those born to mothers with reactivation of the disease. Of the newborns who are infected with CMV, only 10% are symptomatic at birth and the mortality rate among symptomatic infants is about 10%; however, approximately 50% to 90% of the surviving infants may experience significant problems, including sensorineural hearing loss, mental retardation, and other neurologic defects. It is not known if topically administered ophthalmic ganciclovir could result in significant systemic absorption; therefore, the manufacturer recommends the administration of ophthalmic ganciclovir to pregnant women only if the potential benefit to the mother outweighs the potential risk to the fetus.[32676] [36875] [61771]
It is not known if ganciclovir is excreted into breast milk. Due to the potential for serious adverse reactions in nursing infants, the manufacturer recommends instructing mothers to stop or not to start breast-feeding if they are receiving ganciclovir. Additionally, ganciclovir may be used to treat infections in patients with HIV and the Centers for Disease Control and Prevention (CDC) recommends that in the US, HIV-infected mothers not breast-feed their infants to avoid the risk of postnatal transmission of HIV. It is not known if topically administered ophthalmic ganciclovir could result in sufficient systemic absorption to produce detectable quantities in breast milk; therefore, the manufacturer recommends caution if ophthalmic ganciclovir is administered to breast-feeding women. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested or administered drug, health care providers are encouraged to report the adverse effect to the FDA.[32676] [36875] [46675]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.