Hemophilia, Adult
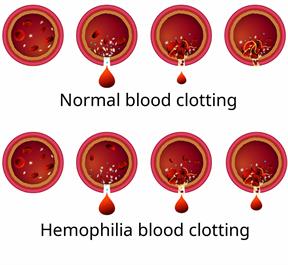
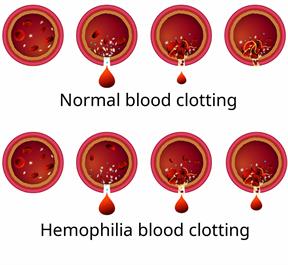
Hemophilia is a bleeding disorder that prevents blood from clotting properly. This means that it is harder for a person's body to stop bleeding. Hemophilia is usually a genetic disorder that a person is born with. A person with hemophilia may have prolonged bleeding after an injury or even without an injury. This occurs because the person has low levels of a type of protein that helps the blood to form clots. These proteins are called clotting factors.
There are different types of hemophilia based on the clotting factor that the person does not have enough of (is
deficient in). The types are:
Hemophilia A. This is the most common type. It is caused by low levels of clotting factor VIII (factor VIII deficiency).
Hemophilia B. This type is caused by low levels of clotting factor IX (factor IX deficiency).
Hemophilia C. This type is caused by low levels of clotting factor XI (factor XI deficiency).
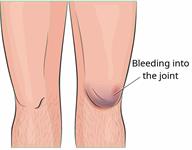
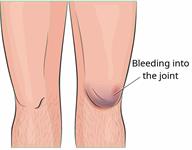
With hemophilia, bleeding can range from mild to severe depending on how much clotting factor the person is missing. Bleeding may occur through the skin, mouth, or nose. It may also happen inside the body, such as in the joints.
What are the causes?
This condition is usually caused by abnormal genes that are passed from parent to child (
inherited).
In rare cases, a person can develop hemophilia without inheriting the hemophilia gene. This can happen if a person develops antibodies that attack clotting factors and keep them from working. An antibody is a type of protein that is part of the body's disease-fighting system (immune system).
What increases the risk?
The following factors may make you more likely to develop this condition:
Having a family history of the disease.
Being male. The disease is much more common in males. Females may be carriers of the disease, but they rarely develop symptoms.
What are the signs or symptoms?
The most common symptoms of this condition are unusual bleeding and bruising. This may occur after an injury, dental work, or a surgery. It may also occur without any obvious cause. Bleeding problems may include:
How is this diagnosed?
This condition may be diagnosed with blood tests. A health care provider may suspect hemophilia in a person who bruises and bleeds easily. Blood tests will be done to measure:
How is this treated?
The main treatment for this condition is replacement of the clotting factor that is missing. You will be given the clotting factor through an IV. How often this is done depends on how severe the hemophilia is. You may be given clotting factor regularly to prevent bleeding, or it may be given to you only when bleeding occurs. You may also be taught to administer the clotting factor to yourself at home. Other treatments may include:
A hormone (desmopressin) that may help to keep blood clots from breaking down. This is used only for mild types of hemophilia A. It stimulates the release of clotting factor VIII. This medicine is given through an IV, by injection, or in a nose spray (intranasal).
A type of medicine (antifibrinolytic medicine) that also helps to keep blood clots from breaking down. This medicine is taken by mouth. It may be given to people who have frequent bleeding from the nose or mouth. It may also be given before dental procedures.
Plasma. Plasma is the liquid part of the blood that helps move platelets and clotting factors throughout the body. This is given through an IV.
Be sure to work with a team of health care providers who specialize in hemophilia. In the United States, these teams are located at hemophilia treatment centers (HTCs). At an HTC, you can get help with home care, education about hemophilia, and support. To find an HTC near you, go to the website of the Centers for Disease Control and Prevention (CDC): www.cdc.gov
Follow these instructions at home:
Medicines
-
Take over-the-counter and prescription medicines only as told by your health care provider.
- Always check with your health care provider before you take any medicines. You will need to avoid over-the-counter medicines that can affect the clotting process. These include:
-
Ask your health care provider before taking over-the-counter medicines, vitamins, herbs, and supplements.
Activity
-
Avoid any activities that your health care provider says are not safe. You may need to avoid or limit activities or contact sports that could result in a fall or injury.
-
Use elbow and knee padding and wear a helmet during athletic or recreational activities as told by your health care provider.
-
Get regular exercise through activities that are recommended by your health care provider.
Safety
-
Use seat belts.
-
Avoid having furniture with sharp corners in the house.
-
Be careful not to cut yourself when using sharp objects or while shaving.
-
Use an electric razor to shave instead of a blade.
- Follow instructions from your health care provider about ways that you can help prevent falls and injuries at home. These may include:
General instructions

-
Tell all your health care providers, including your dentist, that you have hemophilia. There are things that your health care providers can do to prevent or reduce bleeding during and after procedures. For example, medicine can be given during dental procedures to reduce bleeding.
-
Brush your teeth using a soft toothbrush.
-
Wear a medical ID bracelet that says that you have hemophilia. This can help you get the treatment you need in case of an emergency.
-
If you cut yourself, have a nosebleed, or are bleeding for any other reason, apply consistent pressure to the area until the bleeding has stopped completely. This may take several minutes.
-
Stay up to date on all vaccines as directed by your health care provider.
-
Keep all follow-up visits. This is important.
-
World Federation of Hemophilia:
wfh.org
-
Contact a health care provider if:
-
You have bleeding that will not stop.
-
You have any injury to the head.
-
You have any symptoms of bleeding in the brain.
-
You have severe joint pain and swelling.
Summary
-
Hemophilia is a bleeding disorder that prevents blood from clotting properly. It is usually inherited.
-
A person with hemophilia may have prolonged bleeding after an injury or even without an injury.
-
The main treatment for this condition is replacement of the clotting factor that is missing.
-
Wear a medical ID bracelet that says that you have hemophilia. This can help you get the treatment you need in case of an emergency.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.
 The most common symptoms of this condition are unusual bleeding and bruising. This may occur after an injury, dental work, or a surgery. It may also occur without any obvious cause. Bleeding problems may include:
The most common symptoms of this condition are unusual bleeding and bruising. This may occur after an injury, dental work, or a surgery. It may also occur without any obvious cause. Bleeding problems may include: