How to Use an Incentive Spirometer
An incentive spirometer is a tool that measures how well you are filling your lungs with each breath. Learning to take long, deep breaths using this tool can help you keep your lungs clear and active. This may help to reverse or lessen your chance of developing breathing (
pulmonary) problems, especially infection. You may be asked to use a spirometer:
If the spirometer includes an indicator to show the highest number that you have reached, your health care provider or respiratory therapist will help you set a goal. Keep a log of your progress as told by your health care provider.
What are the risks?
-
Breathing too quickly may cause dizziness or cause you to pass out. Take your time so you do not get dizzy or light-headed.
-
If you are in pain, you may need to take pain medicine before doing incentive spirometry. It is harder to take a deep breath if you are having pain.
How to use your incentive spirometer
-
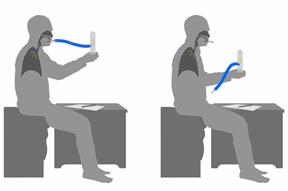
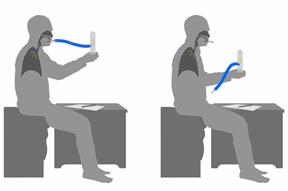
Sit up on the edge of your bed or on a chair.
-
Hold the incentive spirometer so that it is in an upright position.
-
Before you use the spirometer, breathe out normally.
-
Place the mouthpiece in your mouth. Make sure your lips are closed tightly around it.
-
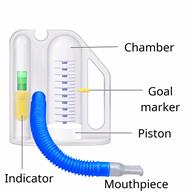
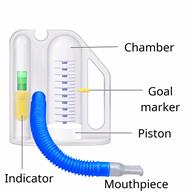
Breathe in slowly and as deeply as you can through your mouth, causing the piston or the ball to rise toward the top of the chamber.
- Hold your breath for 3–5 seconds, or for as long as possible.
-
Remove the mouthpiece from your mouth and breathe out normally. The piston or ball will return to the bottom of the chamber.
- Rest for a few seconds, then repeat the steps 10 or more times.
-
If the spirometer includes a goal marker to show the highest number you have reached (best effort), use this as a goal to work toward during each repetition.
- After each set of 10 deep breaths, cough a few times. This will help to make sure that your lungs are clear.
Contact a health care provider if:
-
You are having difficulty using the spirometer.
-
You have trouble using the spirometer as often as instructed.
-
Your pain medicine is not giving enough relief for you to use the spirometer as told.
-
You have a fever.
-
You develop shortness of breath.
-
You develop a cough with bloody mucus from the lungs.
-
You have fluid or blood coming from an incision site after you cough.
Summary
-
An incentive spirometer is a tool that can help you learn to take long, deep breaths to keep your lungs clear and active.
-
You may be asked to use a spirometer after a surgery, if you have a lung problem or a history of smoking, or if you have been inactive for a long period of time.
-
Use your incentive spirometer as instructed every 1–2 hours while you are awake.
-
If you have an incision on your chest or abdomen, place a pillow or a rolled-up towel firmly against your incision when you cough. This will help to reduce pain.
-
Get help right away if you have shortness of breath, you cough up bloody mucus, or blood comes from your incision when you cough.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.
 An incentive spirometer is a tool that measures how well you are filling your lungs with each breath. Learning to take long, deep breaths using this tool can help you keep your lungs clear and active. This may help to reverse or lessen your chance of developing breathing (pulmonary) problems, especially infection. You may be asked to use a spirometer:
An incentive spirometer is a tool that measures how well you are filling your lungs with each breath. Learning to take long, deep breaths using this tool can help you keep your lungs clear and active. This may help to reverse or lessen your chance of developing breathing (pulmonary) problems, especially infection. You may be asked to use a spirometer: