Idiopathic Intracranial Hypertension
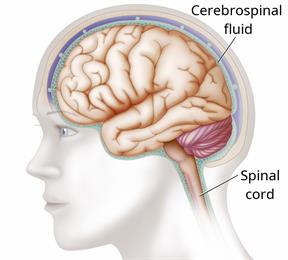
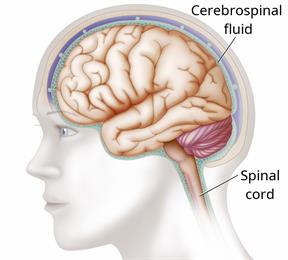
Idiopathic intracranial hypertension (IIH) is a condition that increases pressure around the brain. The fluid that surrounds the brain and spinal cord (cerebrospinal fluid, or CSF) increases and causes the pressure. Idiopathic means that the cause of this condition is not known.
IIH affects the brain and spinal cord. If this condition is not treated, it can cause vision loss or blindness.
What are the causes?
The cause of this condition is not known.
What increases the risk?
The following factors may make you more likely to develop this condition:
Being obese.
Being a person who is female, between the ages of 20 and 50 years old, and who has not gone through menopause.
Taking certain medicines, such as birth control, acne medicines, or steroids.
What are the signs or symptoms?
Symptoms of this condition include:
Headaches. This is the most common symptom.
Brief periods of total blindness.
Double vision, blurred vision, or poor side (peripheral) vision.
Pain in the shoulders or neck.
Nausea and vomiting.
A sound like rushing water or a pulsing sound within the ears (pulsatile tinnitus), or ringing in the ears.
How is this diagnosed?
This condition may be diagnosed based on:
Your symptoms and medical history.
- Imaging tests of the brain, such as:
Diagnostic lumbar puncture. This is a procedure to remove and examine a sample of CSF. This procedure can determine whether your fluid pressure is too high.
An eye exam to check for swelling or nerve damage in the eyes.
How is this treated?
Treatment for this condition depends on the symptoms. The goal of treatment is to decrease the pressure around your brain. Common treatments include:
Weight loss through healthy eating, salt restriction, and exercise, if you are overweight.
Medicines to decrease the production of CSF and lower the pressure within your skull.
Medicines to prevent or treat headaches.
Other treatments may include:
Follow these instructions at home:
-
If you are overweight or obese, work with your health care provider to lose weight.
-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
Ask your health care provider if the medicine prescribed to you requires you to avoid driving or using machinery.
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
-
Keep all follow-up visits. Your health care provider will need to monitor you regularly.
Contact a health care provider if:
- You have changes in your vision, such as:
Double vision.
Blurred vision.
Poor peripheral vision.
- You have any of the following symptoms and they get worse or do not get better:
Headaches.
Nausea.
Vomiting.
Sudden trouble seeing.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.