ThisiscontentfromElsevier'sDrugInformation
Immune Globulin, IVIG
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
General dosing information
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response.[70019]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response.[70019]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration. The target trough is at least 600 mg/dL. The dose may be proportionally adjusted starting with the second infusion using the patient's trough concentration and initial dose.[64039]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration. The target trough is at least 600 mg/dL. The dose may be proportionally adjusted starting with the second infusion using the patient's trough concentration and initial dose.[64039]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[42658] [42661] [70744]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[42658] [42661] [70744]
400 to 800 mg/kg/dose IV every 3 to 4 weeks. The first infusion of Carimune NF in previously untreated agammaglobulinemic or hypogammaglobulinemic patients must be given as a 3% solution; if tolerated, subsequent infusions may be administered at a higher concentration.[42654]
400 to 800 mg/kg/dose IV every 3 to 4 weeks. The first infusion of Carimune NF in previously untreated agammaglobulinemic or hypogammaglobulinemic patients must be given as a 3% solution; if tolerated, subsequent infusions may be administered at a higher concentration.[42654]
300 to 600 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[41552] [42655] [42955] [46250] [51240] [63463]
300 to 600 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[41552] [42655] [42955] [46250] [51240] [63463]
300 to 600 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response.[41553]
300 to 600 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[30276]
300 to 600 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[30276]
200 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[42659]
200 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response and desired IgG trough concentration.[42659]
300 to 800 mg/kg/dose IV every 3 to 4 weeks. Adjust dose and frequency based on clinical response.[72723]
Subcutaneous doses are based on the previously established intravenous IVIG dose. Initially, convert the dose by multiplying the current IVIG dose in grams by 1.37, then divide by the number of weeks between IV doses (e.g., if IVIG is administered every 3 weeks, divide by 3). Start the initial subcutaneous dose approximately 1 week after the last IV infusion and administer weekly. Obtain an IgG trough concentration prior to converting from IV to subcutaneous treatment to guide dosage adjustments. Adjust dose and frequency based primarily on clinical response; desired IgG trough concentration should also be considered. Calculate the difference between the patient's target IgG trough concentration and the actual IgG trough concentration during subcutaneous administration. Use the table provided in the product-specific package insert to adjust the dose based on this difference and the patient's body weight.[42655]
Subcutaneous doses are based on the previously established intravenous IVIG dose. Initially, convert the dose by multiplying the current IVIG dose in grams by 1.37, then divide by the number of weeks between IV doses (e.g., if IVIG is administered every 3 weeks, divide by 3). Start the initial subcutaneous dose approximately 1 week after the last IV infusion and administer weekly. Obtain an IgG trough concentration prior to converting from IV to subcutaneous treatment to guide dosage adjustments. Adjust dose and frequency based primarily on clinical response; desired IgG trough concentration should also be considered. Calculate the difference between the patient's target IgG trough concentration and the actual IgG trough concentration during subcutaneous administration. Use the table provided in the product-specific package insert to adjust the dose based on this difference and the patient's body weight.[42655]
Subcutaneous doses are based on the previously established intravenous IVIG dose. Initially, convert the dose by multiplying the current IVIG dose in grams by 1.37, then divide by the number of weeks between IV doses (e.g., if IVIG is administered every 3 weeks, divide by 3). To convert the calculated initial subcutaneous dose in grams to mL, multiply by 10. Start the initial subcutaneous dose 1 week after the last IV infusion and administer weekly. Obtain an IgG trough concentration prior to converting from IV to subcutaneous treatment to guide dosage adjustments. Adjust dose and frequency based primarily on clinical response; desired IgG trough concentration should also be considered. An IgG trough concentration may be measured as early as 5 weeks after switching from IV to subcutaneous administration. Calculate the difference between the patient's target IgG trough concentration and the actual IgG trough concentration during subcutaneous administration. The projected target trough level is the last IVIG trough level plus 340 mg/dL. Use the table provided in the product-specific package insert to adjust the dose based on this difference and the patient's body weight. To determine whether further dosage adjustments are necessary, monitor IgG trough concentration every 2 to 3 months.[51240] [54820]
Subcutaneous doses are based on the previously established intravenous IVIG dose. Initially, convert the dose by multiplying the current IVIG dose in grams by 1.37, then divide by the number of weeks between IV doses (e.g., if IVIG is administered every 3 weeks, divide by 3). To convert the calculated initial subcutaneous dose in grams to mL, multiply by 10. Start the initial subcutaneous dose 1 week after the last IV infusion and administer weekly. Obtain an IgG trough concentration prior to converting from IV to subcutaneous treatment to guide dosage adjustments. Adjust dose and frequency based primarily on clinical response; desired IgG trough concentration should also be considered. An IgG trough concentration may be measured as early as 5 weeks after switching from IV to subcutaneous administration. Calculate the difference between the patient's target IgG trough concentration and the actual IgG trough concentration during subcutaneous administration. The projected target trough level is the last IVIG trough level plus 340 mg/dL. Use the table provided in the product-specific package insert to adjust the dose based on this difference and the patient's body weight. To determine whether further dosage adjustments are necessary, monitor IgG trough concentration every 2 to 3 months.[51240] [54820]
400 mg/kg/dose IV once daily for 2 to 5 consecutive days. If the platelet count falls to less than 30,000/microliter or clinically significant bleeding manifests after induction therapy, may give 400 mg/kg/dose IV as a single dose. If response is inadequate, may increase the dose to 800 mg/kg/dose to 1 g/kg/dose IV as a single dose.[42654]
400 mg/kg/dose IV once daily for 2 to 5 consecutive days; if the platelet count is adequate (30,000 to 50,000/microliter) after the first 2 doses, therapy may be discontinued. If the platelet count falls to less than 30,000/microliter or clinically significant bleeding manifests after induction therapy, may give 400 mg/kg/dose IV as a single dose. If response is inadequate, may increase the dose to 800 mg/kg/dose to 1 g/kg/dose IV as a single dose.[42654]
1 g/kg/dose IV once daily for 2 consecutive days.[41553]
1 g/kg/dose IV once daily for 2 consecutive days.[41553]
1 g/kg/dose IV as a single dose. If response is inadequate, may give 1 g/kg/dose IV on alternate days for up to 3 doses.[42955]
400 mg/kg/dose IV once daily for 5 consecutive days. Alternatively, 1 g/kg/dose IV once daily for 2 consecutive days; if platelet count is adequate 24 hours after the initial dose, the second dose may be withheld.[46250] [51240]
400 mg/kg/dose IV once daily for 5 consecutive days. Alternatively, 1 g/kg/dose IV once daily for 2 consecutive days; if platelet count is adequate 24 hours after the initial dose, the second dose may be withheld.[46250] [51240]
1 g/kg/dose IV once daily for 2 consecutive days.[42661] [61745] [57655] [63463]
1 g/kg/dose IV once daily for 2 consecutive days.[42659]
1 g/kg/dose IV once daily for 2 consecutive days.[42659]
1 g/kg/dose IV once daily for 2 consecutive days. Alternatively, 400 mg/kg/dose IV once daily for 5 consecutive days.[53269] [53270] [53271] [70050]
2g/kg IV in divided doses over 2 to 5 days.[69025] [70847]
400 mg/kg/dose IV given every 3 to 4 weeks.[42955]
400 mg/kg/dose IV once monthly. Monitor IgG trough concentration every 2 weeks during IVIG therapy, and adjust dose and frequency to maintain a IgG concentration greater than 400 mg/dL. In general, the half-life of IVIG among HCT patients is much shorter than that of healthy patients; larger doses may be required.[51812]
500 mg/kg/dose IV every 3 to 4 weeks.[51812]
500 mg/kg/dose IV once weekly. Monitor IgG trough concentration every 2 weeks during IVIG therapy; adjust dose and frequency to maintain a IgG concentration greater than 400 mg/dL. In general, the half-life of IVIG among HCT patients is much shorter than that of healthy patients; larger doses may be required.[51812]
500 mg/kg/dose IV every 3 to 4 weeks.[51812]
400 mg/kg/dose IV every 2 to 4 weeks.[34361]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[70019]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[70019]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[41552] [42661] [42955] [55005] [63463]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[41552] [42661] [42955] [55005] [63463]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[41553] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 400 mg/kg/dose IV every 3 to 4 weeks, administer at least 400 mg/kg/dose IV as single dose immediately prior to expected exposure.[46250] [51240] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 400 mg/kg/dose IV every 3 to 4 weeks, administer at least 400 mg/kg/dose IV as single dose immediately prior to expected exposure.[46250] [51240] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[42659] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[42659] [55005] [61745]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[30276] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks. If a patient is at risk of future measles exposure and receives less than 530 mg/kg/dose IV every 3 to 4 weeks, increase the dose to at least 530 mg/kg/dose (to provide a serum concentration of 240 milli-International Units/mL of measles antibodies for at least 22 days after infusion).[30276] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks.[30276] [55005]
400 mg/kg/dose IV as a single dose as soon as possible and within 6 days of exposure. This dose should provide a serum concentration more than 240 milli-International Units/mL of measles antibodies for at least 2 weeks.[30276] [55005]
400 mg/kg/dose IV as a single dose as soon as possible after exposure. If a patient is at risk of future measles exposure and receives less than 400 mg/kg/dose IV every 3 to 4 weeks, administer a dose of at least 400 mg/kg/dose IV just prior to the expected measles exposure.[72723]
1,000 mg/kg/dose IV as a single dose or 400 mg/kg/dose IV once daily for 4 consecutive days beginning within 7 days of fever onset. Administer concurrently with moderate- to high-dose aspirin.[42955]
2,000 mg/kg/dose IV as a single dose within 10 days of illness onset but as soon as possible after diagnosis. Administer concurrently with moderate- to high-dose aspirin. Treat children presenting after day 10 of illness if they have unexplained persistent fever or coronary artery abnormalities with ongoing systemic inflammation (e.g., elevated ESR and CRP). Consider a second dose if persistent or recrudescent fever at least 36 hours after completion of the initial IVIG infusion.[61950]
NOTE: Some patients may not require continued maintenance therapy beyond 6 months to maintain therapeutic response. Maintenance therapy beyond 6 months has not been studied.[42655] [51240] [54820] [63463] [42659]
2 g/kg IV loading dose in divided doses over 2 to 5 consecutive days, followed by maintenance dose of 1 g/kg/dose IV every 3 weeks. A maintenance dose range of 0.4 to 1 g/kg/dose IV every 2 to 6 weeks may be considered.[53272] [70243] [70246]
2 g/kg IV loading dose in divided doses over 2 to 5 consecutive days, followed by maintenance dose of 1 g/kg/dose IV every 3 weeks. A maintenance dose range of 0.4 to 1 g/kg/dose IV every 2 to 6 weeks may be considered.[53339] [53340] [53341] [53272] [70243] [70246]
2 g/kg IV loading dose in divided doses over 2 to 4 consecutive days, followed by maintenance dose of 1 g/kg/dose IV administered as a single infusion or as 2 infusions of 500 mg/kg/dose given on 2 consecutive days every 3 weeks.[51240] [54820]
2 g/kg IV loading dose in divided doses over 2 to 5 consecutive days, followed by maintenance dose of 1 g/kg/dose IV administered as a single infusion or in divided doses over 1 to 4 consecutive days every 3 weeks.[42655]
2 g/kg IV loading dose in divided doses over 2 consecutive days, followed by maintenance dose of 1 to 2 g/kg/dose IV in divided doses over 2 consecutive days every 3 weeks.[63463]
2 g/kg IV loading dose in divided doses over 2 to 5 consecutive days, followed by maintenance dose of 1 g/kg/dose IV administered as a single infusion or as 2 infusions of 500 mg/kg/dose given on 2 consecutive days every 3 weeks.[42659]
1 g/kg IV daily for 2 days when there is active bleeding or platelet counts are less than 10 x 109/L was recommended by a panel of 14 clinical and practice guideline experts.[42611] This recommendation was based on data from 4 published randomized controlled trials.[42663] [42665] [42666] [42667] These trials were of mixed quality with only 2 requiring patients to have thrombocytopenia (less than 50 x 109/L) at baseline.[42663] [42667] Additionally, the dosing regimens evaluated in these trials were not standardized, and the trials included a small number of patients (range, 12 to 30 patients). Despite these limitations, the panel deemed the results to be favorable toward IVIG use.
2 g/kg IV divided in equal doses over 2 to 5 consecutive days every 4 weeks.[57655] [68308] [68309] [68311] [68322] [70295]
2 g/kg (Max: 70 g) IV divided in equal doses over 1 to 5 consecutive days every 2 weeks for initial therapy and then every 4 to 6 weeks.[53272] [53273] [53276] [68313] [68314] [68137] [68318] [70295]
2 g/kg IV divided in equal doses over 2 to 5 consecutive days every 4 weeks.[68308] [68309] [68311] [68322] [70295]
2 g/kg (Max: 70 g) IV divided in equal doses over 1 to 5 consecutive days every 2 weeks for initial therapy and then every 4 to 6 weeks.[53272] [53273] [53276] [68313] [68314] [68137] [68318] [70295]
1 g/kg/dose IV once daily for 2 days or 400 mg/kg/dose IV once daily for 5 days within 2 weeks of symptom onset for persons with symptoms of grade 3 severity or higher or symptoms less than grade 3 severity that are progressing and for persons who initially responded to IVIG and are experiencing a relapse of symptoms.[24601] [53272] [64898] [64899]
1 g/kg/dose IV once daily for 2 days or 400 mg/kg/dose IV once daily for 5 days within 2 weeks of symptom onset for persons with symptoms of grade 3 severity or higher or symptoms less than grade 3 severity that are progressing and for persons who initially responded to IVIG and are experiencing a relapse of symptoms.[24601] [53272] [53346]
1 g/kg/dose IV once daily for 1 to 2 days or 0.4 g/kg/dose IV once daily for 5 days.[53272] [61823] [61824] [63192] [63193] [63194] [71494] [71516] [71518]
2 g/kg IV as a single dose or divided over 2 to 5 days.[53272] [53287] [53289] [53290] [71495]
2 g/kg IV as a single dose or divided over 2 to 5 days.[53272] [53286]
0.5 g/kg/dose IV every 2 to 4 weeks or 1 g/kg/dose IV every 2 to 6 weeks.[71494] [71516] [71518]
1 g/kg/dose IV every 4 to 6 weeks.[71495]
0.5 to 1 g/kg/dose IV over 2 hours; may repeat dose in 12 hours if necessary. Therapy is most effective when initiated promptly after diagnosis.[34425] [53293] [53294] [68260] [68261]
A review written by the University Hospital Consortium lists IVIG as an acceptable, first-line agent in the treatment of post-transfusion purpura.[24601] The effects of IVIG were studied in 11 patients with post-transfusion purpura. In the same report, the results of the treatment of an additional 8 patients described in the literature were also summarized. One patient failed therapy due to under dosing and 1 other patient died of CHF. Out of the 17 remaining patients, 16 were determined to have good or excellent results. Five different IVIG preparations were used in the study with no obvious differences in efficacy. The total dose of IVIG per course ranged from 52 to 180 g.[24602] (NOTE: For many clinical conditions, a total dose of 2 g/kg IV divided evenly over 2 to 5 days represents the typical dose.)
2 g/kg IV divided over 2 to 5 consecutive days every 4 weeks.[71628] [71629]
0.5 to 2.4 g/kg/month IV based on clinical response; initial infusion rate is 0.8 mg/kg/minute (Max: 9 mg/kg/minute).[42655]
Efficacy data are limited and variable; dosage regimens vary. 500 to 1,000 mg/kg/dose IV once daily for 1 to 6 days beginning as soon as sepsis is diagnosed is a commonly used dosage range.[53352] [53354] A meta-analyses of 3 prospective, randomized studies reported septic neonates receiving IVIG (n = 55) had a decreased death rate; analyses concluded IVIG administration in addition to conventional therapy increased the survival of early-onset of neonatal sepsis nearly 6-fold.[53352] However, the results from the large International Neonatal Immunotherapy Study (n = 3,493) concluded that IVIG 500 mg/kg/dose IV every 48 hours for 2 doses did not affect the outcomes of suspected or proven neonatal sepsis.[53353] Pediatric guidelines recommend against the routine use of IVIG in patients with septic shock; however, select patients (e.g., those with toxic shock syndrome, necrotizing fasciitis, primary humoral immunodeficiencies, or low immunoglobulin concentrations) may benefit from such treatment.[64985]
2 g/kg IV as a single dose. Efficacy data is limited and variable. Data from a cohort study of 46 pediatric patients suggested those treated with IVIG (n = 21) had improved left ventricular function recovery and survival at 1 year.[53298] Systemic reviews and multi-institutional analyses have failed to prove efficacy or survival benefit.[53300] [53301] [53302] [53303] [66775]
2 g/kg IV as a single dose. Efficacy data is limited and variable. Data from a cohort study of 46 pediatric patients suggested those treated with IVIG (n = 21) had improved left ventricular function recovery and survival at 1 year.[53298] Systemic reviews and multi-institutional analyses have failed to prove efficacy or survival benefit.[53300] [53301] [53302] [53303] [66775]
NOTE: Use only if varicella-zoster immune globulin is unavailable.[70821]
400 mg/kg/dose IV as a single dose administered as soon as possible (preferably within 96 hours), but up to 10 days after exposure in those without evidence of immunity.[34362] [51900] [68723] [70821]
400 mg/kg/dose IV as a single dose administered as soon as possible (preferably within 96 hours), but up to 10 days after exposure in those without evidence of immunity.[34361] [70821]
1 g/kg/dose IV once daily for 2 days or 400 mg/kg/dose IV once daily for 5 days.[53272] [64893] [67800] [67918] [67919] [67920] [67921]
1 g/kg/dose IV once daily for 2 days or 400 mg/kg/dose IV once daily for 5 days.[53272] [67801] [67917]
2 to 3 g/kg IV divided over 1 to 4 days. Total doses ranging from 0.8 to 7.4 g/kg have been reported.[68070] [68088] [68089] [68090]
2 g/kg IV divided over 1 to 4 days. Total doses ranging from 1.5 to 5.8 g/kg have been reported.[53359] [53360] [53361] [53362] [53363] [68093]
200 to 400 mg/kg IV once if tetanus immune globulin is not available.[64478]
200 to 400 mg/kg IV once if tetanus immune globulin is not available.[64478] [70821]
2 g/kg (based on ideal body weight; Max: 100 g/dose) IV as a single dose in combination with low-to-moderate methylprednisolone or equivalent glucocorticoid. The dose may be divided in patients with cardiac dysfunction or fluid overload (1 g/kg IV every 24 hours for 2 doses).[65314] [65707] [65720] [66644] The National Institutes of Health (NIH) treatment guidelines recommend against the routine use of IVIG monotherapy for the treatment of MIS-C, unless glucocorticoid use is contraindicated.[65314]
400 to 500 mg/kg/dose IV once daily for 5 days or 1 g/kg/dose IV once daily for 2 days, then repeat dose every 4 weeks for several months.[60439] [67418] [67419]
400 to 500 mg/kg/dose IV once daily for 5 days or 1 g/kg/dose IV once daily for 2 days, then repeat dose every 4 weeks for several months.[60439] [67418] [67419]
NOTE: Guidelines recommend treatment with aerosolized or systemic ribavirin and IVIG for patients with RSV upper respiratory tract infection disease (URTID) undergoing allogeneic HSCT or recipients of allogeneic HSCT with lower respiratory tract infection disease (LRTID) or risk factors for progression to RSV LRTID and death.[68208] [68226] For solid organ transplant patients, the addition of IVIG and corticosteroids to ribavirin can be considered for lung transplant recipients with URTID or LRTID.[68241]
500 mg/kg/dose IV in combination with aerosolized or systemic ribavirin. Dosing frequency has ranged from one-time to every 48 hours for 5 to 7 doses in clinical studies.[68203] [68202] [68211] [68212] [68223] [68224] [68225] [68240]
400 to 500 mg/kg/dose IV in combination with aerosolized or systemic ribavirin. Dosing frequency has ranged from one-time to every 48 hours for 5 to 7 doses in clinical studies.[68203] [68219] [68220] [68221] [68222]
400 to 500 mg/kg/dose IV once daily for 5 consecutive days.[70696]
Optimal dose has not been established; regimens include 150 to 400 mg/kg/dose IV once daily for 5 days; 1 to 2 g/kg/dose IV as a single dose; or 1 g/kg/dose IV on Day 1, followed by 0.5 g/kg/dose IV once daily for 1 to 2 days.[70821] [71104] [71108] [71109] [71110]
Optimal dose has not been established; regimens include 150 to 400 mg/kg/dose IV once daily for 5 days; 1 to 2 g/kg/dose IV as a single dose; or 1 g/kg/dose IV on Day 1, followed by 0.5 g/kg/dose IV once daily for 1 to 2 days.[70821] [71104] [71108] [71109] [71110]
2 g/kg/dose IV as a single dose or 1 g/kg/dose IV once daily for 2 days or 400 mg/kg/dose IV once daily for 5 days.[72005]
2 g/kg IV as a single dose or divided over 2 to 4 days.[71444] [71445] [71582]
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
To minimize the risk for further acute renal function deterioration or renal failure, use the minimum recommended IVIG dose administered at the minimum concentration available and the minimum practicable intravenous rate. Recommended infusion rates may vary by product. Avoid sucrose-containing IVIG products if possible. If renal deterioration occurs despite adequate volume status, it is recommended to discontinue the IVIG.[42655][42658][64039][70019][72723]
† Off-label indication







Immune globulin IV (IVIG) is an intravenous solution composed primarily of human immunoglobulin G (IgG), with trace amounts of IgA and IgM.[42659][70019][70821][72723] IVIG is derived from the pooled human plasma of thousands of donors, ensuring a diversified collection of antibodies with variable antigen-binding regions.[53218] All samples undergo human immunodeficiency virus (HIV), hepatitis B, and hepatitis C testing.[42659][70019][72723] Although the amount of each IgG subclass is similar to that of human plasma in all IVIG formulations, titers among specific antigens, preparation methods, viral inactivation steps, stabilizing agents, osmolality, and IgA content differ among products. Thus, IVIG products have comparable efficacy but are not pharmaceutically equivalent. IVIG is used for a variety of conditions; its primary indication is as replacement therapy for patients with primary immunodeficiency. It is also used to treat idiopathic thrombocytopenic purpura (ITP), chronic inflammatory demyelinating polyneuropathy (CIDP), Guillain-Barre syndrome, and Kawasaki disease in pediatric patients.[34425][53366][53272][61950][70821] The majority of adverse reactions associated with IVIG are infusion-related; however, serious reactions including acute renal failure, hemolytic anemia, aseptic meningitis syndrome, and thrombotic events have been reported.[53441][70821] Conservative product-specific infusion rates and careful monitoring is essential with IVIG use.[53366]
For storage information, see the specific product information within the How Supplied section.
Preparation
Alyglo, Asceniv, Bivigam, Flebogamma, Gammaplex, Qivigy, Yimmugo
Carimune NF
Gammagard Liquid
Gammagard S/D
Gamunex-C/Gammaked
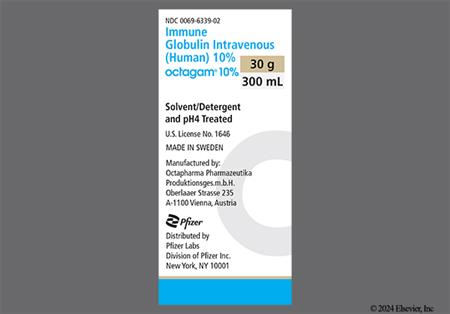
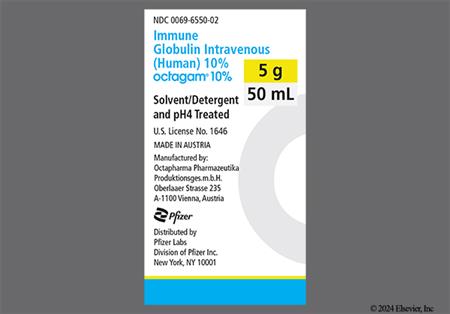
Octagam/Panzyga
Privigen
General Intravenous Administration
Product specific administration
Alyglo
Asceniv
Bivigam
Carimune NF
Flebogamma DIF
Gammagard Liquid
Gammagard S/D
Gammaplex 5% or 10%
Gamunex-C/Gammaked
Octagam 5% or 10%
Panzyga
Privigen
Qivigy
Yimmugo
Preparation (all products)
Subcutaneous Administration
Transfusion-related acute lung injury (TRALI) is a life-threatening and potentially fatal complication of blood product administration; it has rarely been reported after IVIG administration. TRALI is characterized by severe respiratory distress, hypoxemia (hypoxia), fever, normal left ventricular function, and severe non-cardiogenic pulmonary edema. Symptoms typically begin 1 to 2 hours after administration and manifest fully within 1 to 6 hours. The clinical presentation may be subtle or significant. Radiographs show bilateral pulmonary infiltrates without evidence of cardiac compromise or fluid overload. Respiratory support may be necessary. Diuretics are not effective in TRALI as the cause involves microvascular injury, rather than fluid overload. The etiology of TRALI may be attributable to the presence of anti-HLA antibodies and/or anti-granulocyte antibodies in the plasma of multiparous females or donors who have received previous transfusions who serve as donors for the plasma-derived product. Recipients of IVIG should be monitored for pulmonary adverse events. If TRALI is suspected, both the product and the individual need to be tested for the presence of anti-neutrophil and anti-HLA antibodies.[26918] [51240] [53383] [53384] [53385] [70019] [72723]
Immune globulin is derived from human plasma. Based on effective donor screening and product manufacturing processes, IVIG carries an extremely remote risk of transmission of viral infection or disease. A theoretical risk for transmission of Creutzfeldt-Jakob disease also is considered to be extremely remote. Before prescribing IVIG, discuss the risks and benefits of its use with the individual. Infectious events reported during IVIG therapy include bronchitis (6% to 30%), upper respiratory tract infection (6% to 33%), fungal infection (7% to 9%), viral infection (6%), otitis media (7%), urinary tract infection (7% to 11%), vaginal candidiasis (9%), and flu-like syndrome (5% to 6%).[30276] [41552] [41553] [42654] [42655] [42659] [42661] [42955] [46250] [63463] [70019] [72723]
Respiratory adverse events, including cough/increased cough (6% to 54%), dyspnea (5% to 11%; 8% of pediatric patients), epistaxis (5% to 23%), pharyngitis (10% to 41%), nasopharyngitis (22%), rhinitis (5% to 51%), asthma (15% to 29%), pharyngolaryngeal pain (6%), nasal congestion (6% to 52%), sinusitis (2% to 50%), sore throat, rhinorrhea (7% to 17%), sinus congestion, post-nasal drip, sinus pain, respiratory tract congestion (7%), upper respiratory tract infection (8% to 22%), bronchitis (5% to 20%), oropharyngeal pain, cyanosis, throat irritation (6% to 7%), acute otitis media (8% of pediatric patients), tonsillar disorder (8% of pediatric patients), painful respiration, hypoxemia, apnea, hyperventilation, throat tightness, acute respiratory distress syndrome (ARDS), and influenza-like illness (7%), have been reported with the use of immune globulin. Influenza (less than 1%) has also been reported with subcutaneous use in pediatric patients. Wheezing (3% to 14%), dyspnea, and bronchospasm (14% to 29%) may be associated with immune globulin infusion; slowing or stopping the infusion, as well as premedication with acetaminophen and antihistamines may help alleviate these reactions.[30276] [41552] [41553] [42654] [42655] [42659] [42661] [42955] [46250] [51240] [57655] [63463] [64039] [70019] [72723]
Nausea (5% to 67%), vomiting (6% to 42%), and diarrhea (5% to 28%) are commonly reported adverse effects associated with immune globulin. Necrotizing enterocolitis (NEC) has been associated with high-dose immune globulin used for isoimmune hemolytic disease in preterm and term neonates. Other gastrointestinal adverse effects reported include abdominal pain or cramps (15% or less), dyspepsia (6% to 9%), stomach discomfort (6%), gastroenteritis (9% to 22%), gastroesophageal reflux (7%), and toothache (dental pain). Of note, vomiting was reported more frequently in pediatric patients vs. adult patients during clinical trials of immune globulin for primary immunodeficiency. Nausea, vomiting, abdominal pain/cramping, and loss of appetite (anorexia) may be associated with immune globulin infusion; slowing or stopping the infusion as well as premedication with acetaminophen and antihistamines may help alleviate these symptoms.[30276] [41552] [41553] [42654] [42655] [42658] [42659] [42661] [42955] [46250] [51240] [53417] [57655] [64039] [70019] [72723]
Renal dysfunction, including oliguria, anuria, acute renal failure (unspecified), osmotic nephrosis (osmotic nephropathy), acute renal tubular necrosis, proximal tubular nephropathy, and death have been reported in individuals receiving IVIG. Increases in BUN (azotemia) and serum creatinine have been observed as soon as 1 to 2 days after infusion of IVIG. Progression to oliguria and anuria requiring dialysis has been observed; although, some individuals have spontaneously recovered following cessation of treatment. Renal histopathologic examination suggested an osmotic injury to the proximal renal tubules (acute renal tubular necrosis, proximal tubular nephropathy, vacuolar degeneration, and osmotic nephrosis). Renal dysfunction is more common with the use of IVIG products containing sucrose as a stabilizer. Use IVIG with caution in individuals at risk for developing renal dysfunction, including those with any pre-existing degree of renal insufficiency or renal disease, sepsis, paraproteinemia, diabetes mellitus, hypovolemia, dehydration, obesity, age more than 65 years, or concomitant use of nephrotoxic agents. Especially in such individuals, use the minimum recommended dose of IVIG administered at the minimum concentration available and the minimum practicable rate. Ensure individuals are not volume depleted prior to IVIG administration. Monitor renal function, including BUN, serum creatinine, and urine output at baseline and appropriate intervals thereafter. If renal function deteriorates, consider IVIG therapy discontinuation. Dysuria, cystitis, or urinary tract infection was reported in 5% of individuals who received Gammaplex. There are postmarketing reports of renal pain with IVIG therapy.[30276] [39573] [41552] [41553] [46250] [42654] [42655] [42659] [42661] [42955] [51240] [57655] [70019] [72723]
Nervous system or psychiatric adverse events have been reported during the use of immune globulin. Headache (8% to 92%), dizziness (4% to 13%), and anxiety may be associated with the immune globulin infusion; slowing or stopping the infusion, as well as premedication with acetaminophen and antihistamines may help alleviate these symptoms. Other adverse events reported with immune globulin use include insomnia (6% to 9%), agitation, migraine (6% to 7%), restlessness, tremor, hypoesthesia, paresthesias, coma, encephalopathy, loss of consciousness, confusion, nervousness, depression (6%), dysarthria (speech disorder), lethargy, and seizures.[30276] [41552] [41553] [46250] [42654] [42655] [42658] [42659] [42661] [42955] [46250] [51240] [57655] [61745] [70019] [72723]
Aseptic meningitis syndrome (AMS) may rarely occur after IVIG therapy. Signs and symptoms appear within several hours to 2 days and include severe head pain, nuchal rigidity, drowsiness, pyrexia, photophobia, painful eye movements, and emesis. AMS may be more frequent after high-dose (more than 1,000 to 2,000 mg/kg/dose) or rapid-infusion IVIG treatment. Individuals with a history of migraine may be at higher risk for this complication of IVIG. Individuals presenting with signs and symptoms should undergo a thorough neurological evaluation, including cerebrospinal fluid (CSF) studies; the CSF is often positive for pleocytosis and elevated protein levels, with negative culture results. Discontinuation of IVIG treatment may result in remission of AMS within several days without sequelae.[23788] [30276] [41552] [41553] [46250] [42654] [42655] [42659] [42661] [42955] [57655] [70019] [72723] Cerebral edema has also been reported with IVIG therapy in postmarketing surveillance.[42659]
Thrombotic events, such as thromboembolism, myocardial infarction, cerebrovascular accident (stroke), transient ischemic attack, thrombophlebitis, deep vein thrombosis, vena cava thrombosis, arterial thrombosis, retinal thrombosis, and pulmonary embolism, have been reported with IVIG. Signs and symptoms of thrombosis include numbness or weakness (paresis) on one side of the body, pain, swelling, discoloration, and/or warmth of the arms or legs, unexplained shortness of breath, and unexplained tachycardia. Additional adverse events associated with thrombosis include chest pain (unspecified) (5% to 15%), pallor, decreased heart rate, vascular collapse, myocardial infarction, and cardiac arrest. Thrombosis may occur regardless of the route of administration and in the absence of known risk factors; however, individuals at highest risk for thrombotic events include age more than 65 years, those with multiple cardiovascular risk factors, impaired cardiac output, coagulation disorders, prolonged periods of immobilization, diabetes mellitus, obesity, thrombophilic disorders, a history of vascular disease, a history of atherosclerosis, a history of a previous thromboembolic event, use of estrogens, indwelling catheters, and/or known or suspected hyperviscosity. Ensure that individuals are not volume depleted prior to the initiation of IVIG. For individuals judged to be at risk for developing thrombotic events, use the minimum recommended dose of IVIG administered at the minimum concentration available and the minimum practicable rate. Monitor all individuals receiving IVIG during and after each infusion and encourage individuals to report any signs and symptoms of thrombosis.[42655] [42658] [64039] [70019] [72723]
Ecchymosis (9% to 40%), purpura (40%), bleeding/hemorrhage (29%), petechiae (21%), and thrombocytopenia (15%) have been reported during clinical trials of IVIG for the treatment of immune thrombocytopenic purpura (ITP). Other hematologic adverse effects reported with IVIG use include anemia (6% to 11%), decreased hematocrit (5%), decreased hemoglobin, leukopenia (7%), neutropenia, pancytopenia, autoimmune pure red cell aplasia exacerbation, hemoglobinuria, hematuria, chromaturia, and lymphadenopathy (7%).[30276] [41552] [41553] [42654] [42655] [42659] [42955] [46250] [51240] [57655] [70019]
Antibodies present in IVIG may act as hemolysins and induce immunoglobulin adherence to red blood cells, causing a positive direct antiglobulin test (DAT, Coombs' test), and rarely, hemolysis. Acute hemolysis consistent with intravascular hemolysis, severe hemolysis-related renal dysfunction/failure, and disseminated intravascular coagulation (DIC) have been reported with IVIG therapy. Hemolysis was reported in 7% of immune globulin-treated individuals with chronic inflammatory demyelinating polyneuropathy (CIDP) during a clinical trial. In addition, delayed hemolytic anemia can develop after IVIG therapy due to enhanced red blood cell sequestration; cases have generally been reversible. Hemolytic events not associated with a positive DAT have also been observed in clinical trials. Risk factors related to the development of hemolysis include high doses (2,000 mg/kg or more) as a single infusion or divided over several days, and non-O blood type. An underlying inflammatory state reflected by elevated C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may also contribute to the risk of hemolysis, however the role is uncertain. Monitor individuals receiving immune globulin for hemolysis and hemolytic anemia. In high risk individuals, consider appropriate lab testing, including hemoglobin and hematocrit prior to therapy and for 36 to 96 hours after infusion, and again 7 to 10 days after infusion, depending on the manufacturer's recommendations. If signs and symptoms of hemolysis are present after the infusion, perform confirmatory lab testing. If a transfusion is indicated, perform adequate cross-matching to avoid exacerbating ongoing hemolysis.[30276] [41552] [41553] [42654] [42655] [42659] [42955] [46250] [51240] [57655] [70019] [72723]
Anaphylactoid reactions, including angioedema, facial edema, and anaphylactic shock, have been reported with IVIG use. Individuals who are IgA deficient and have known antibodies to IgA may be at greater risk for developing severe hypersensitivity reactions. Epinephrine should be immediately available during IVIG infusions. If a hypersensitivity reaction occurs, immediately discontinue the infusion.[30276] [46250] [42654] [42655] [42659] [42661] [42955] [51240] [57655] [70019] [72723]
An injection site reaction (5% to 15%), characterized by erythema, pain, irritation/burning, pruritus, edema, and swelling, has occurred with immune globulin. Phlebitis, including thrombophlebitis, has also been reported. Local reactions tend to be more common after hand vein infusions with higher concentrations of immune globulin solution (i.e., 10% vs. 5%); incidence may be reduced by administering immune globulin via the antecubital vein. Local reactions may also be common with subcutaneous infusion, particularly during the first week of infusion. Local reactions were reported in nearly 60% of subcutaneous infusions, and 75% of adult and adolescent patients during clinical trials; incidence rates were similar in pediatric trials (60% of infusions, 100% of patients). The incidence of local reactions may decrease with time in patients receiving chronic infusions. If local reactions occur, application of a warm compress to the infusion site may alleviate symptoms.[30276] [41552] [41553] [42654] [42655] [42659] [42661] [42955] [46250] [51240] [57655] [70019]
Dermatologic adverse reactions, such as urticaria or hives, pruritis, and rash, have been reported in approximately 5% to 12% of patients receiving IVIG infusion; slowing or stopping the infusion, as well as premedication with acetaminophen and antihistamines may help alleviate these symptoms. Stevens-Johnson syndrome, epidermolysis, bullous dermatitis/bullous rash, allergic dermatitis (6%), contact thermal burn or abrasion (7%), eczema or atopic dermatitis, dry skin or xerosis (5% to 9%), maculopapular rash, alopecia, skin exfoliation, and erythema multiforme have also been associated with the use of IVIG.[30276] [41552] [41553] [42654] [42655] [42658] [42659] [42661] [42955] [46250] [51240] [57655] [64039] [70019]
Hyperproteinemia, increased serum viscosity, hyponatremia, and fluid overload may occur in individuals receiving IVIG therapy. The hyponatremia is likely to be a pseudohyponatremia as demonstrated by a decreased calculated serum osmolality or elevated osmolar gap. Distinguishing between true hyponatremia and pseudohyponatremia is important since treatment aimed at decreasing serum free water in individuals with pseudohyponatremia may lead to volume depletion, further increased serum viscosity, and a disposition to thromboembolic events.[30276] [42654] [42655] [42659] [42955] [46250] [51240] [57655] [70019] [72723]
Musculoskeletal pain (5% to 25%), arthralgia (9% or less), back pain (4% to 17%), neck pain (6%), extremity pain (5%), fibromyalgia, myalgia (5% to 6%), muscle cramps or spasms (7%), muscle strain, and muscular weakness or myasthenia have been reported with immune globulin use. Accidental injury (13%) has also been reported. Musculoskeletal adverse events such as arthralgia, myalgia, back pain/backache, muscle cramps, and flu-like symptoms may be associated with IVIG infusion reaction; slowing or stopping the infusion, as well as premedication with acetaminophen and antihistamines may help alleviate these symptoms. Synovitis/tenosynovitis, joint swelling/effusion (6% to 11%), bursitis, chondromalacia patellae, epicondylitis, joint sprain, and trigger finger have been reported during clinical trials of IVIG.[30276] [41552] [41553] [42654] [42655] [42658] [42659] [42661] [42955] [46250] [51240] [57655] [64039] [70019]
Otalgia (earache/pain 18%) has been reported in patients receiving IVIG. Ocular adverse events reported with IVIG include conjunctivitis (9% to 13%), ocular discharge (7%), ocular irritation (7%), ocular pain, and visual impairment/disturbance.[30276] [41552] [41553] [42654] [42655] [42659] [42661] [42955] [46250] [51240] [57655]
Elevated hepatic enzymes and hepatic dysfunction have been reported with the use of IVIG. Elevations in AST (7% to 13%), ALT (7% to 18%), alkaline phosphatase (13%), and lactate dehydrogenase (5%) have occurred. Elevations in AST and ALT are generally mild (less than 3 times the upper limit of normal), transient, and not associated with symptoms of liver disease. Hyperbilirubinemia (5%) and increases in unconjugated bilirubin (9% to 11%), conjugated bilirubin (9%), and total bilirubin (7%) were all noted during clinical trials. Jaundice, hepatic dysfunction, and non-infectious hepatitis have been reported postmarketing.[30276] [41552] [41553] [42654] [42658] [42659] [42955] [46250] [51240] [57655] [64039] [70019]
Infusion-related reactions may occur during immune globulin administration. Symptoms include flushing (6%), chest tightness, headache, chills (5% to 33%), rigors (7% to 37%), fever or increased body temperature (33% or less), diaphoresis, hyperhidrosis (6%), hot flush/hot flashes, dyspnea, wheezing (14%), bronchospasm, dizziness (6%), asthenia (5% to 15%), fatigue (18% or less), malaise (5%), gastrointestinal complaints (nausea, vomiting, upper abdominal pain and/or cramping, loss of appetite), hypotension (2% to 25%), diastolic hypotension (21% in pediatric patients), muscle symptoms (e.g., cramps, backache, arthralgia, myalgia), general flu-like symptoms, anxiety, palpitations, bradycardia (16%), sinus tachycardia (2% to 25%), dizziness, edema, and transient skin reactions. Hypertension occurred in 4% to 14% of patients during clinical trials. Four patients experienced reversible increases in systolic blood pressure to 180 mmHg or more during or within 1 to 4 hours after infusion. Of the 3 patients who had a history of hypertension, a patient with history of untreated hypertension also experienced a reversible increase in diastolic blood pressure from 84 mmHg to 135 mm Hg at 1 hour after the end of the infusion. All cases of hypertension resolved within 1 to 6 hours with observation or changes to oral antihypertensive therapy. Other general adverse events include accidental injury (13% to 16%), angina pectoris, chest discomfort (7% to 9%), extremity pain (11%), and falls (7%). Hyperhidrosis and hot flush/hot flashes have been noted in postmarketing reports. Compared to adult patients, fever was reported more frequently in pediatric patients during clinical trials of IVIG for idiopathic thrombocytopenic purpura (ITP) and primary immunodeficiency. Patients who have never received immune globulin, have been switched from a certain immune globulin product to another, or have had an interruption in immune globulin therapy more than 8 weeks may be at a higher risk for the development of an inflammatory reaction, especially with rapid infusion rates. Symptoms typically begin 30 to 60 minutes after initiation of the infusion and appear to be related to the infusion rate rather than the dose. Slowing or stopping the infusion usually allows these symptoms to resolve. Pretreatment with oral antihistamines and analgesics may help to alleviate these symptoms.[30276] [39573] [41552] [41553] [46250] [42654] [42655] [42658] [42659] [42661] [42955] [51240] [57655] [70019] [72723]
Life-threatening hypoglycemia can occur with the use of Octagam 5% and 10%. Some glucose monitoring systems interpret the maltose in Octagam as glucose. Inaccurate glucose readings can result in inappropriate administration of insulin. Furthermore, falsely elevated glucose readings could mask true cases of hypoglycemia. Monitor glucose in diabetic patients with a glucose-specific method only. Ensure blood glucose testing systems, including test strips, are appropriate to use with maltose-containing products.[30276] [57655]
Immune globulin administration may result in laboratory test interference. After infusion of immunoglobulins, the transitory rise of the various passively transferred antibodies in the blood may yield false positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to erythrocyte antigens (e.g., A, B, D) may cause a positive direct or indirect antiglobulin (Coombs') test. Additionally, false-positive results may occur in assays that detect beta-D-glucans for the diagnosis of fungal infections; this interference may persist for several weeks after immune globulin infusion.[42655] [64039] [70019] [72723] Perform blood glucose measurements using glucose-specific methods when a patient is receiving a parenteral product containing maltose, such as Octagam IVIG. Blood glucose testing systems that use glucose dehydrogenase pyrroloquinolinequinone (GDH-PQQ) or glucose-dye-oxidoreductase methods may falsely interpret the maltose contained in Octagam IVIG as glucose. These falsely elevated glucose readings (false hyperglycemia) have led to inappropriate administration of insulin, resulting in life-threatening hypoglycemia, and may also mask true hypoglycemia. Consult the product information for the blood glucose testing system and test strips to confirm compatibility with maltose-containing parenteral products. If any uncertainty exists, contact the manufacturer of the testing system.[30276] [57655]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Some products contain maltose and are contraindicated in patients with an acute corn hypersensitivity.[30276]
Carefully consider the relative risks and benefits before prescribing the high-dose regimen (e.g., 1 g/kg/day or more) in patients with volume overload. Administration of IVIG can significantly contribute to the daily fluid balance.[42659]
Some immune globulin formulations (e.g., Privigen) are contraindicated in individuals with hyperprolinemia due to the presence of the stabilizer L-proline.[42659] Gammaplex is contraindicated in patients with hereditary fructose intolerance (HFI), as it contains sorbitol as an excipient; it should also not be used in neonates and infants for whom fructose or sucrose tolerance has not been established.[42661] Other IVIG products, such as Flebogamma, also contain sorbitol and should be avoided in patients with HFI.[41552] [41553]
Immune globulin is contraindicated in individuals with IgA deficiency with antibodies against IgA and a history of hypersensitivity. Immune globulin is also contraindicated for use in individuals who have a history of significant adverse event(s) associated with previous use of immune globulin. Severe hypersensitivity reactions may occur in any individual, even if previous treatment with immune globulin was tolerated.[42655] [64039] [70019] [72723]
Thrombosis may occur after treatment with immune globulin products. Risk factors for thromboembolism may include advanced age (geriatric adults), prolonged immobility, hypercoagulable conditions (thrombophilia), history of venous or arterial thrombosis, use of estrogens, indwelling central venous catheter, hyperviscosity, and cardiovascular disease or risk factors. Thrombosis may also occur without known risk factors. In patients at risk for thrombosis, ensure adequate hydration prior to administration, administer immune globulin at the lowest practical dose and infusion rate, and monitor for signs and symptoms of thrombosis. Consider a baseline blood viscosity assessment in patients at risk for hyperviscosity, such as those with cryoglobulinemia, fasting chylomicronemia or hypertriglyceridemia, or monoclonal gammopathy of undetermined significance (paraproteinemia).[42655] [64039] [70019] [72723]
Administer immune globulin at the lowest practical infusion rate in patients at increased risk of renal injury, such as those with renal impairment or renal failure, diabetes mellitus, age greater than 65 years, hypovolemia, sepsis, paraproteinemia, obesity, or those receiving nephrotoxic medications, and ensure adequate hydration prior to administration. Acute renal failure, acute tubular nephrosis, proximal tubular nephropathy, osmotic nephrosis, and death may occur with the use of human immune globulin products. Assess renal function, including blood urea nitrogen (BUN), serum creatinine, and urine output, prior to the initial infusion and periodically during therapy. If renal function deteriorates, consider discontinuing treatment.[42655] [64039] [70019] [72723]
Monitor patients receiving immune globulin for clinical signs and symptoms of hemolysis, particularly those at increased risk, such as individuals with non-O blood types (blood group phenotype A, blood group phenotype B, blood group phenotype AB) or those receiving high doses (2 g/kg or more). Although the contribution of underlying inflammation to hemolysis risk is not fully understood, it may be a contributing factor. Consider appropriate laboratory testing in higher risk patients, including measurement of hemoglobin or hematocrit prior to infusion and within approximately 36 to 96 hours post infusion. If signs and/or symptoms of hemolysis are present after immune globulin infusion, perform appropriate confirmatory laboratory testing. Immune globulin products may contain blood group antibodies that act as hemolysins and induce in vivo coating of red blood cells (RBCs) with immunoglobulin, causing a positive direct antiglobulin test (DAT, Coombs' test). Delayed hemolytic anemia secondary to immune globulin can develop due to enhanced red blood cell sequestration, and acute hemolysis consistent with intravascular hemolysis has been reported.[42655] [64039] [70019] [72723]
Studies with immune globulin IV (IVIG) during pregnancy have not been conducted in humans or animals, and the ability of IVIG to cause fetal harm or affect reproduction capacity is unknown.[42658] [51240] [70019] [72723] Immunoglobulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation.[42658] [70019] In cases of maternal idiopathic thrombocytopenic purpura where IVIG was administered to the mother before delivery, the platelet response and clinical effect were similar in the mother and neonate.[42654] According to the Advisory Committee on Immunization Practices (ACIP), fetal adverse events have not occurred after administration of immune globulin preparations to pregnant women. Administer during pregnancy only if clearly needed.[43236]
Use of immune globulin IV (IVIG) has not been evaluated in women who are breast-feeding and excretion of IVIG into breast milk is unknown.[51240] [70019] [72723] However, endogenous immune globulin is a normal component in breast milk.[60441] Case reports of 2 nursing mothers receiving intravenous immune globulin therapy suggest transfer of IgG and IgM into the colostrum and breast milk.[48199] There is emerging consensus that IVIG may be the preferred treatment for postpartum mothers with multiple sclerosis who are breastfeeding, although 1 retrospective study failed to find a decrease in relapse rate among mothers who received IgG postpartum.[60441] In a retrospective study of patients with relapsing remitting multiple sclerosis, 73% of neonates were breast-fed for periods of 3 to 12 weeks with no adverse effects. Patients received IVIG through 12 weeks postpartum with regimens of 400 mg/kg/day for 5 days after delivery with additional booster doses at 6 and 12 week postpartum (n = 41) or 0.4 mg/kg/day for 5 days during weeks 6 to 8 of gestation with booster doses every 6 weeks until 12 weeks postpartum.[60442]
Immunoglobulins are antibodies synthesized by B lymphocytes. IVIG is derived from the pooled human plasma of thousands of donors. Most preparations consist of intact immunoglobulin (Ig)G molecules with trace amounts of IgA, IgM, soluble CD4, CD8, human leukocyte antigen (HLA), and cytokines. The pooled, heterogenous IgG present in IVIG provides a plethora of antibodies capable of opsonization and neutralization of many toxins and microbes as well as complement activation. Although the amount of each IgG subclass in the parenteral products is similar to that of human plasma, the titers against specific antigens vary from manufacturer to manufacturer. The Fc fragment of the IgG molecule allows the molecule to interact with and signal through Fc- gamma receptors on B cells and other cells of the phagocytic system. The Fc fragment also interacts with the Fc-binding plasma proteins, which is essential for complement activation and microorganism clearance. The passive immunity imparted by IVIG is capable of attenuating or preventing infectious diseases or deleterious reactions from toxins, mycoplasma, parasites, bacteria, and viruses.[53218]
In immunomodulatory and anti-inflammatory disease states, it is believed the Fc fragment of IgG and the Fc-gamma receptors on target cells (e.g., macrophages, B cells, natural killer cells, plasma cells, eosinophils, neutrophils, platelets) interact to up-regulate or down-regulate inflammatory and immune responses. In autoimmune cytopenias and inflammatory neurologic disorders, blockade of Fc-gamma receptors on macrophages blocks the clearance of opsonized target cells and suppresses antibody-dependent cell-mediated cytotoxicity, respectively. Immunoglobulins may also modulate inflammatory response by preventing complement-mediated tissue damage and regulating the induction of anti-inflammatory cytokines and cytokine antagonists (e.g., interleukin 1-beta, interleukin-1 receptor antagonist, tumor necrosis factor alpha). Immunomodulatory response may be facilitated by the immunoregulatory effects of anti-idiotypic antibodies on B cells and autoantibodies, regulation of helper T cell production, and apoptosis of immune system gene expression.[53218]
In ITP treatment, IVIG produces an immediate rise in platelet count, usually lasting only a few weeks, although platelet stabilization for up to 1 year after administration has been reported.[23982]
Revision Date: 10/06/2025, 05:11:14 PMImmune globulin is administered intravenously; some products (e.g., Gammagard Liquid, Gamunex-C) can also be given as subcutaneous infusion.[42655] Data concerning distribution are scant, but immune globulin appears to distribute equally throughout intravascular and extravascular spaces. It crosses the placenta (in increasing amounts after 30 weeks of gestation) and may be excreted into breast milk. Mean volume of distribution at steady state is 0.05 to 0.08 L/kg. The exact fate of IVIG is not well-defined, but plasma clearance is slow, ranging from 1.3 to 2.5 mL/kg/day; the serum half-life of immune globulin (IgG) is approximately 18 to 25 days. Great interpatient variability exists for the half-life of IgG. Fever, infection, or high IgG concentrations appear to coincide with a shortened half-life whereas immunodeficiency appears to be associated with a longer half-life of IgG (18 to 40 days).[30276][42654][42655][42658][42659][42955][70019][72723]
Peak serum concentrations occur immediately after IV infusion and are dose-related. After infusion, immune globulin follows a biphasic decay curve. The initial phase is characterized by an immediate peak in serum IgG and is followed by rapid decay due to equilibration between the plasma and extravascular fluid compartments; a rapid initial drop in serum IgG is expected. After approximately 6 days, equilibrium is reached and IgG is distributed equally between the intravascular and extravascular space. The second phase is characterized by a slower and constant rate of decay.[30276][42654][42655] In a pharmacokinetic study of 61 adult patients with humoral immunodeficiency receiving intravenous (IV) Gammagard Liquid (median dose: 455 mg/kg/dose every 4 weeks), the mean peak and trough IgG concentration for IV Gammagard Liquid was 2,240 +/- 536 mg/dL and 1,050 +/- 260 mg/dL, respectively. The AUC was 9,958 +/- 2,274 mg x days/dL.[42655]
Some immune globulin products (e.g., Gammagard Liquid, Gamunex-C) have been administered as subcutaneous infusions. The subcutaneous dose required to provide an exposure non-inferior to the exposure from intravenous (IV) administration was 137% of the IV dose.[42655][54339][51240] Specifically, the mean adjusted subcutaneous dose was 141% (100.5% to 160%) for patients younger than 12 years and 137.3% (125.7 to 150.8%) of the IV dose for patients at least 12 years of age. After subcutaneous administration, the peak IgG concentration occurred 2.9 (1.2 to 3.2) days later, and the mean peak concentration was 1,393 +/- 289 mg/dL. The mean trough concentration was 1,202 +/- 282 mg/dL. As compared with IV administration, the mean peak concentration was lower after subcutaneous administration, and the mean trough concentration was higher.[42655] Therefore, subcutaneous infusion doses are adjusted to 1.37 times the IV dosage on average for these products.[42655][51240]
Neonates
Volume of distribution in neonates has been reported with variance, ranging from 0.04 to 0.25 L/kg. The IVIG half-life is comparable to normal adult parameters with a reported range of 18 to 29 days.[53227][53228][53229] In a study of 15 neonates (gestational age 32 to 41 weeks; birth weight more than 1,500 grams), IVIG infusions of 500 mg/kg resulted in a mean peak IgG concentration of 2,171 mg/dL, 15 minutes after infusion; this dosage resulted in a significant increase in IgG concentrations greater than 8 days after the infusion. IVIG infusions of 1,000 mg/kg resulted in mean peak IgG concentrations of 2,734 mg/dL and resulted in significant increases in IgG concentrations more than 11 days after the infusion. A biphasic decay curve resulted in an initial rapid decay within 24 hours after infusion followed by a slower decay over the next 6 weeks. Plasma clearance was 3 mL/kg/day. Gestational age, birth weight, dose, and pretreatment serum IgG concentrations had minimal effect on pharmacokinetic parameters.[53228]
Children and Adolescents
The pharmacokinetics of intravenous and subcutaneous immune globulin are similar in children, adolescents, and adults.[42658][51240] Both intravenous and subcutaneous infusions of immune globulin appear to be effective in children and with similar trough IgG concentrations achieved as in adults.[42658][54339] No pediatric specific dose requirements are necessary to achieve the desired serum IgG levels. Dosage, as in adults, must be individualized and adjusted over time to achieve the desired trough levels and clinical responses.
Studies with immune globulin IV (IVIG) during pregnancy have not been conducted in humans or animals, and the ability of IVIG to cause fetal harm or affect reproduction capacity is unknown.[42658] [51240] [70019] [72723] Immunoglobulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation.[42658] [70019] In cases of maternal idiopathic thrombocytopenic purpura where IVIG was administered to the mother before delivery, the platelet response and clinical effect were similar in the mother and neonate.[42654] According to the Advisory Committee on Immunization Practices (ACIP), fetal adverse events have not occurred after administration of immune globulin preparations to pregnant women. Administer during pregnancy only if clearly needed.[43236]
Use of immune globulin IV (IVIG) has not been evaluated in women who are breast-feeding and excretion of IVIG into breast milk is unknown.[51240] [70019] [72723] However, endogenous immune globulin is a normal component in breast milk.[60441] Case reports of 2 nursing mothers receiving intravenous immune globulin therapy suggest transfer of IgG and IgM into the colostrum and breast milk.[48199] There is emerging consensus that IVIG may be the preferred treatment for postpartum mothers with multiple sclerosis who are breastfeeding, although 1 retrospective study failed to find a decrease in relapse rate among mothers who received IgG postpartum.[60441] In a retrospective study of patients with relapsing remitting multiple sclerosis, 73% of neonates were breast-fed for periods of 3 to 12 weeks with no adverse effects. Patients received IVIG through 12 weeks postpartum with regimens of 400 mg/kg/day for 5 days after delivery with additional booster doses at 6 and 12 week postpartum (n = 41) or 0.4 mg/kg/day for 5 days during weeks 6 to 8 of gestation with booster doses every 6 weeks until 12 weeks postpartum.[60442]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.