ThisiscontentfromElsevier'sDrugInformation
Leuprolide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
In several trials, 1 mg subcutaneous once daily has been used. Because the condition is reversible if the drug is discontinued, therapy must be continuous.[24155]
A long-acting, depot formulation administered in a dosage of 3.75 mg IM once every 28 days for 24 weeks was effective. Because the condition is reversible if the drug is discontinued, therapy must be continuous.[24156]
7.5 mg subcutaneously once monthly. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, open-label study, the mean testosterone concentration on day 28 after treatment with once-monthly subcutaneous leuprolide acetate was 21.8 ng/dL; 94.1% of patients had testosterone concentrations below the castrate threshold (50 ng/dL) at day 28 and 100% were below the castrate threshold at day 42. There were no breakthrough occurrences of testosterone concentration greater than 50 ng/dL at any time point after testosterone suppression was achieved.[45097]
22.5 mg subcutaneously every 3 months. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, open-label study, the mean testosterone concentration on day 21 after treatment with every3-month subcutaneous leuprolide acetate was 27.7 ng/dL; 99% of patients had testosterone concentrations below the castrate threshold (50 ng/dL) at day 28 and 100% were below the castrate threshold at day 35. Once testosterone suppression was achieved, one patient (less than 1%) demonstrated breakthrough (testosterone concentration greater than 50 ng/dL) following the initial injection; that patient remained below the castrate threshold following the second injection.[45097]
30 mg subcutaneously every 4 months. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, open-label study, the mean testosterone concentration on day 28 after treatment with once-monthly subcutaneous leuprolide acetate was 17.2 ng/dL; 96% of patients had testosterone concentrations below the castrate threshold (50 ng/dL) at day 28 and 100% were below the castrate threshold at day 42. Three patients (3%) demonstrated breakthrough testosterone concentrations (greater than 50 ng/dL) after the second injection once testosterone suppression was achieved; castrate suppression was reached again up to 18 days after the second injection and was maintained thereafter in all 3 patients.[45097]
45 mg subcutaneously every 6 months. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, open-label study, the mean testosterone concentration on day 28 after treatment with once-monthly subcutaneous leuprolide acetate was 16.7 ng/dL; 99.1% of patients had testosterone concentrations below the castrate threshold (50 ng/dL) at day 28. One patient (less than 1%) demonstrated a breakthrough testosterone concentration (greater than 50 ng/dL) once testosterone suppression was achieved. This patient reached castrate suppression at day 21 and remained suppressed until day 308 (testosterone concentration, 112 ng/dL); at day 336, his testosterone concentration was 210 ng/dL.[45097]
42 mg subcutaneously once every 6 months. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. After the first injection of leuprolide mesylate, serum testosterone concentrations were suppressed to 50 ng/dL or less by week 4 in 98.5% of patients with advanced prostate cancer and a baseline serum testosterone concentration greater than 150 ng/dL in a multinational, single-arm study; serum testosterone was 50 ng/dL or less from week 4 to week 48 in 97% of patients. Serum testosterone concentrations were 20 ng/dL or less on day 28 in 69.3% of patients.[66709] [66714]
7.5 mg IM every 4 weeks. Do not use concurrently a fractional dose, or a combination of doses of this or any depot formulation due to different release characteristics. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, noncomparative trial, patients with previously untreated stage D2 prostate cancer received leuprolide as a once-monthly IM depot injection. Serum testosterone increased by 50% or more above baseline during the first week of treatment in the majority of patients; it was suppressed to castrate levels within 30 days in 94% of patients and within 66 days in all patients. One patient had a breakthrough testosterone concentration (greater than 50 ng/dL) that was associated with a substantial dosing delay.[43800]
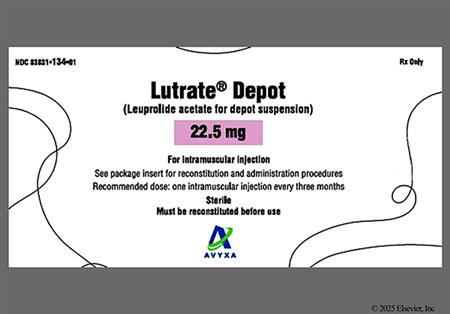
22.5 mg IM every 12 weeks. Do not use concurrently a fractional dose, or a combination of doses of this or any depot formulation due to different release characteristics. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In clinical studies, serum testosterone was suppressed to castrate levels within 30 days in 95% of patients; one patient later experienced a transient minimal elevation of testosterone. During the initial 24 weeks of treatment, 85% of patients did not progress.[43800] [68727]
30 mg IM every 16 weeks. Do not use concurrently a fractional dose, or a combination of doses of this or any depot formulation due to different release characteristics. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, noncomparative trial, patients with previously untreated stage D2 prostate cancer were treated with leuprolide 30 mg IM every 4 months. Serum testosterone increased by 50% or more above baseline during the first week of treatment in the majority of patients; it was suppressed to castrate levels within 30 days in 94% of patients and within 43 days in all patients. Two patients had breakthrough testosterone concentrations (greater than 50 ng/dL) at week 16 and 17, respectively, which returned to castrate level by week 18.[43800]
45 mg IM every 24 weeks. Do not use concurrently a fractional dose, or a combination of doses of this or any depot formulation due to different release characteristics. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a multicenter, noncomparative trial, patients with prostate cancer were treated with leuprolide 45 mg IM every 24 weeks. Serum testosterone was suppressed to castrate levels (less than 50 ng/dL) from week 4 through week 48 in 93.4% of patients; 8 patients had breakthrough testosterone concentrations (greater than 50 ng/dL).[43800]
1 mg subcutaneously once daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. In a controlled study, the survival rate for leuprolide acetate 1 mg subcutaneously once daily was comparable to diethylstilbestrol (DES) 3 mg daily in patients with advanced prostate cancer after 2 years of treatment; the objective response to treatment was also similar for the 2 groups.[66721]
11.25 mg subcutaneous once every 3 months for 2 years has been studied. In a study of 589 patients, leuprolide as compared to 6 cycles of CMF chemotherapy (cyclophosphamide/methotrexate/5-fluorouracil) was shown to be non-inferior for 2-year relapse free survival (63.9% vs. 63.4%, p = 0.83). An exploratory survival analysis favored leuprolide at 5 years (HR 1.5, 95% CI 1.13 to 1.99, p = 0.005).[45417]
3.75 mg IM once monthly or 11.25 mg IM every 3 months for 6 months. May repeat course with norethindrone acetate for recurrence of symptoms; limit total duration of therapy to 12 months.[42683] [51299] [69730]
3.75 mg IM once monthly or 11.25 mg IM every 3 months with or without norethindrone acetate for 6 months. May repeat course with norethindrone acetate for recurrence of symptoms; limit total duration of therapy to 12 months.[42683] [51299] [69730]
NOTE: Leuprolide has been designated an orphan drug by the FDA for this indication.
15 mg IM every 4 weeks. May adjust dose if changes in body weight occur. Max: 15 mg/dose. Monitor hormonal and clinical parameters at month 1 to 2, with dose changes, and further as clinically appropriate to ensure adequate suppression. In the case of inadequate suppression, consider other available GnRH agonists indicated for the treatment of central precocious puberty.[41676]
11.25 mg IM every 4 weeks. Increase the dose to the next available higher dose (e.g., 15 mg) at next monthly injection if inadequate hormonal and clinical suppression with starting dose. May adjust dose if changes in body weight occur. Max: 15 mg/dose. Monitor hormonal and clinical parameters at month 1 to 2, with dose changes, and further as clinically appropriate to ensure adequate suppression.[41676]
7.5 mg IM every 4 weeks. Increase the dose to the next available higher dose (e.g., 11.25 mg) at next monthly injection if inadequate hormonal and clinical suppression with the starting dose. May adjust dose if changes in body weight occur. Max: 15 mg/dose. Monitor hormonal and clinical parameters at month 1 to 2, with dose changes, and further as clinically appropriate to ensure adequate suppression.[41676]
11.25 or 30 mg IM every 12 weeks. Monitor hormonal and clinical parameters at month 2 to 3, month 6, and further as clinically appropriate to ensure adequate suppression. In the case of inadequate suppression, consider other available GnRH agonists indicated for the treatment of central precocious puberty.[41676]
45 mg subcutaneously every 6 months. Monitor hormonal and clinical parameters at month 1 to 2 and further as clinically appropriate to ensure adequate suppression. In the case of inadequate suppression, consider other available GnRH agonists indicated for the treatment of central precocious puberty.[65368]
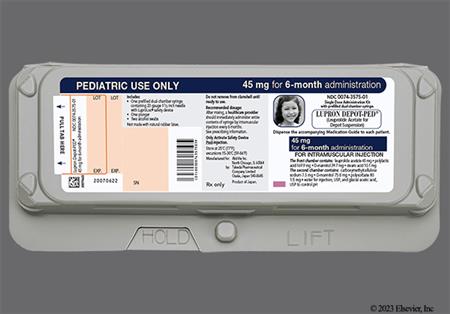
45 mg IM every 6 months. Monitor hormonal and clinical parameters at months 5 to 6 and further as clinically appropriate to ensure adequate suppression. In the case of inadequate suppression, consider other available GnRH agonists indicated for the treatment of central precocious puberty.[41676]
50 mcg/kg/dose subcutaneously once daily. Monitor hormonal and clinical parameters at month 1 to 2, with dose changes, and further as clinically appropriate during therapy to ensure adequate suppression. In the case of inadequate suppression, the dose may be increased by 10 mcg/kg/day.[45475] [70160]
3.75 mg IM once monthly for up to 3 months. Leuprolide is not indicated for combination use with norethindrone acetate add-back therapy. Leuprolide acetate depot 3.75 mg has different release characteristics than leuprolide acetate depot 11.25 mg and is dosed differently. Do not substitute products.[51299]
11.25 mg IM as a single dose, which provides a 3-month treatment course. Leuprolide is not indicated for combination use with norethindrone acetate add-back therapy. Leuprolide acetate depot 11.25 mg has different release characteristics than leuprolide acetate depot 3.75 mg and is dosed differently. Do not substitute products.[43800]
0.5 to 1 mg subcutaneous once daily has been shown to decrease symptoms associated with PMS.[24165] Because of the adverse reaction profile (e.g., osteoporosis, premature coronary artery disease), leuprolide is generally considered a third line agent in the treatment of PMS.
Optimal daily dosage is individualized by the ART specialist; 'long-protocols' are most common but an alternative leuprolide 'flare protocol' is also used (not discussed here, such dosage regimens for flare protocols are much different than those of long protocols). In the long protocol, leuprolide is typically started on day 22 or 23 of the menstrual cycle prior to the ovarian stimulation cycle; dosages vary with usual range 0.5 to 1 mg per day subcutaneously. Women will menstruate, continuing to use the leuprolide during oocyte stimulation with FSH, which usually begins after estradiol suppression is documented. By day 3 of the menstrual cycle, the dosage of leuprolide is typically decreased by 50%. Leuprolide and FSH are administered until sufficient follicular development is attained. HCG is then administered to induce final follicular maturation for oocyte retrieval. FDA-approved medicines like ganirelix and cetrorelix are now more commonly used for this purpose.[63289]
Case reports suggest standard monthly injections of 1.3 to 7.5 mg IM are effective. An 18-year old male with sickle cell anemia received 5.25 mg IM once monthly for 2 months, followed by 2.625 mg IM monthly for 6 months and then 1.3 mg IM monthly for 8 months; priapism did not recur during treatment and the patient continued to receive 1.3 mg IM monthly chronically.[34288] In another case report, a 32-year old male with idiopathic recurrent priapism received 7.5 mg IM once monthly for 2 months; priapism did not recur as of 4 months after discontinuing the leuprolide.[34289] Both patients achieved castration concentrations of testosterone. The American Urological Association recommends GnRH agonist therapy as a first-line option in the prevention of stuttering priapism; however, do not use leuprolide in patients who have not achieved full sexual maturation and adult stature. Additionally, even though patients experience a decrease in libido, most are able to engage in sexual activity.[34290]
3.75 mg IM every 4 weeks. When used in patients undergoing chemotherapy, leuprolide is usually initiated about 2 weeks prior to chemotherapy.[65690] [65692] [65693] [65694] When proven fertility preservation methods are not feasible, and in the setting of young women with breast cancer, gonadotropin-releasing hormone agonists (GnRHa) may be offered to patients in the hope of reducing the likelihood of chemotherapy-induced ovarian insufficiency.[65695] [65696]
3.75 mg IM every 4 weeks. In one trial, leuprolide injection solution 0.2 mg/day subcutaneously was given daily during the first 2 weeks of treatment so chemotherapy could be started immediately.[65691] When proven fertility preservation methods are not feasible, and in the setting of young women with breast cancer, gonadotropin-releasing hormone agonists (GnRHa) may be offered to patients in the hope of reducing the likelihood of chemotherapy-induced ovarian insufficiency.[65695] [65696]
3.75 mg to 7.5 mg subcutaneously every month. Use doses sufficient to suppress pituitary gonadotropins and gonadal sex steroids.[70632] [71219]
11.25 mg subcutaneously every 3 months.[71219]
22.5 mg subcutaneously every 3 months.[71219]
30 mg subcutaneously every 4 months.[71219]
45 mg subcutaneously every 6 months.[71219]
3.75 mg to 7.5 mg IM every month. Use doses sufficient to suppress pituitary gonadotropins and gonadal sex steroids.[70632] [71219]
11.25 mg IM every 3 months.[71219]
Recommended Monitoring
Endometriosis
Prostate Cancer
Precocious Puberty
For use in pubertal suppression
For use in previously suppressed individuals or in late pubertal individuals not previously suppressed
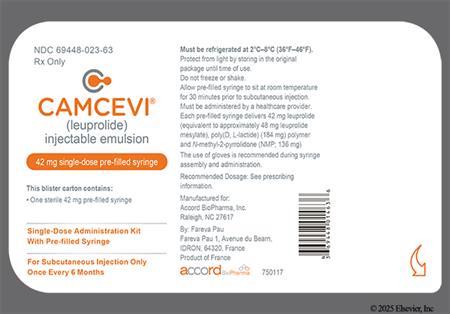
Leuprolide mesylate (Camcevi)
Prostate Cancer: 42 mg subcutaneously every 6 months.
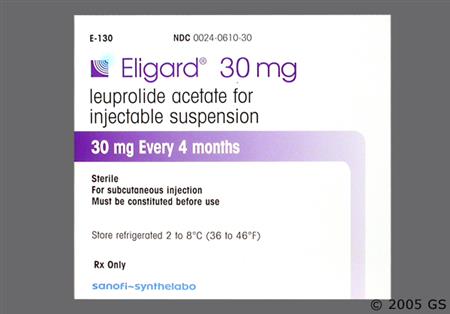
Leuprolide acetate for injectable suspension (Eligard)
Prostate Cancer: 7.5 mg subcutaneously once monthly; OR 22.5 mg subcutaneously every 3 months; OR 30 mg subcutaneously every 4 months; OR 45 mg subcutaneously every 6 months.
Leuprolide acetate for solution (Lupron)
Prostate Cancer: 1 mg subcutaneously once daily.
Leuprolide acetate for depot suspension (Lupron Depot)
Prostate Cancer: 7.5 mg IM once monthly; OR 22.5 mg IM every 3 months; OR 30 mg IM every 4 months; OR 45 mg IM every 6 months.
Endometriosis or Fibroids: 3.75 mg IM once monthly; OR 11.25 mg IM every 3 months.
Leuprolide mesylate (Camcevi)
Prostate Cancer: 42 mg subcutaneously every 6 months.
Leuprolide acetate for injectable suspension (Eligard)
Prostate Cancer: 7.5 mg subcutaneously once monthly; OR 22.5 mg subcutaneously every 3 months; OR 30 mg subcutaneously every 4 months; OR 45 mg subcutaneously every 6 months.
Leuprolide acetate for solution (Lupron)
Prostate Cancer: 1 mg subcutaneously once daily.
Leuprolide acetate for depot suspension (Lupron Depot)
Prostate Cancer: 7.5 mg IM once monthly; OR 22.5 mg IM every 3 months; OR 30 mg IM every 4 months; OR 45 mg IM every 6 months.
Endometriosis or Fibroids: 3.75 mg IM once monthly; OR 11.25 mg IM every 3 months.
Safety and efficacy have not been established.
Leuprolide acetate for injectable suspension (Fensolvi)
45 mg subcutaneously every 6 months.
Leuprolide acetate for depot suspension (Lupron Depot-Ped)
Once monthly regimen:
Weight greater than 37.5 kg: 15 mg IM once monthly.
Weight 26 kg up to 37.5 kg: 11.25 mg IM once monthly.
Weight 25 kg or less: 7.5 mg IM once monthly.
Once every 3 months regimen:
30 mg IM every 3 months
Once every 6 months regimen:
45 mg IM every 6 months
The safety and efficacy of leuprolide acetate has not been established in children younger than 2 years (Fensolvi) or 1 year (Lupron Depot-Ped).
The safety and efficacy of leuprolide mesylate has not been established in children.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication
















Leuprolide is a synthetic nonapeptide analog of naturally occurring gonadotropin-releasing hormone (GnRH); this analog has greater potency than the natural hormone. It is indicated for the treatment of advanced prostate cancer, central precocious puberty (CPP), and for the management of endometriosis and fibroids.[66709][45097][66721][43800][65368][41676][42683][51299][68727] In men with prostate cancer, a transient tumor flare reaction consisting of worsening bone pain, ureteral obstruction, spinal cord compression, or additional signs and symptoms of prostate cancer may develop during the first few weeks of treatment; closely monitor patients and manage symptoms.[66709][45097][66721][43800][68727] An increase in signs and symptoms of puberty (including vaginal bleeding) may occur during the first weeks of therapy for CPP; instruct patients to notify the health care provider if symptoms continue beyond the second month.[65368][41676]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
General Dosing Information
Leuprolide Acetate for Depot Suspension
Preparation (LUPRON Depot and Lupron Depot-Ped)
Preparation (LUTRATE Depot)
IM injection
General Dosing Information
Leuprolide Acetate for Injection (e.g., Lupron)
Preparation
Subcutaneous injection
Leuprolide Acetate for Injectable Suspension (e.g., Eligard)
Preparation
Subcutaneous Injection
Leuprolide Acetate for Injectable Suspension (e.g., Fensolvi)
Preparation
Subcutaneous Injection
Leuprolide Mesylate Injectable Emulsion (e.g., Camcevi)
Preparation
Subcutaneous Injection
Leuprolide may cause adverse effects related to decreased testosterone and estrogen. In males, serum testosterone is reduced to castrate concentrations (less than 50 ng/dL). In premenopausal females, circulating estrogens are reduced to postmenopausal concentrations. After leuprolide initiation, these decreases in hormonal concentrations occur within 2 to 4 weeks. Leuprolide may be used therapeutically to induce a hypo-estrogenic, menopause-like condition in females, which is an induced amenorrhea that usually occurs within 3 months of initiating depot therapy; in some female patients, such a result might be considered a side effect of the drug (74% to 98%). Women treated with leuprolide also reported vaginitis (11% to 28%) and unspecified menstrual disorders (2% to 5%). Chronic leuprolide use can cause male and female infertility; fertility suppression was reversed after drug discontinuation with no evidence that pregnancy rates are affected following discontinuation.[41676] [42683] [51299] Hot flashes occurred in 25% to 98% of men with prostate cancer who received leuprolide; in a small study (n = 74), hot flashes were less common in men who had been orchiectomized (8.3%). Hot flashes also occurred in 73% to 98% of women with endometriosis or fibroids treated with leuprolide; 5% of pediatric patients treated with leuprolide reported hot flushes in 1 trial, 2% reported vasodilation in another, and flushing was reported in postmarketing experience. Gynecomastia occurred in 7.1% or less of men with prostate cancer who received leuprolide; breast enlargement was reported separately in less than 5% of men as well as in postmarketing reports of pediatric patients treated with leuprolide. Less than 2% of pediatric patients reported gynecomastia/breast disorders. Breast soreness or tenderness (mastalgia) occurred in 7% or fewer men, 6% of women with endometriosis, and 4% of children who received leuprolide. Lactation occurred in less than 5% of women in 1 study.[43800] [41676] [42683] [45097] [51299] [65368] [66709] [66721] [68727] Additional adverse reactions in men with prostate cancer related to reduced testosterone include testicular pain (less than 5%), testicular atrophy or decreased testicular size (20.2% or less), impotence (erectile dysfunction) (5.4% or less), hyperhidrosis or sweating (2% or less), clamminess (4.4% or less), night sweats (3.3% or less), penis disorder (less than 5%), reduced penis size (less than 2%), and testis disorder (less than 5%). Prostate pain was reported in postmarketing experience with men receiving leuprolide for the treatment of prostate cancer. Libido decrease (5.4% or less) or loss of libido (less than 2%) was reported in men treated with leuprolide; additionally, 10% to 11% of women receiving treatment for fibroids reported decreased libido.[43800] [45097] [66709] [66721][68727] In pediatric patients, accelerated sexual maturity, dysmenorrhea, feminization, growth inhibition, hirsutism, and unspecified menstrual disorders each occurred in less than 2% of patients; hyperhidrosis was reported in 4% of patients.[41676] [65368]
Administration of leuprolide results in an initial increase in circulating concentrations of luteinizing hormone and follicle stimulating hormone, which leads to a transient increase in concentrations of testosterone (to approximately 50% above baseline) and dihydrotestosterone in males during the first 2 weeks of treatment; testosterone concentrations typically decline to baseline or below by the end of the second week of treatment and to castrate levels within 2 to 4 weeks after starting treatment. Patients with prostate cancer may experience worsening of symptoms or onset of new symptoms (tumor flare). Cases of urinary tract obstruction and spinal cord compression, which may contribute to muscle paralysis with or without fatal complications, have been reported with LHRH agonists such as leuprolide. Monitor patients for symptoms of tumor flare during the first few weeks of treatment; closely monitor patients with urinary tract obstruction or metastatic vertebral lesions for new or worsening symptoms. If spinal cord compression or renal impairment develops, institute standard treatment of these complications. This transient increase in testosterone concentrations is usually manifested by an increase in bone pain (7% or less), but may also include neuropathy, hematuria (6.1% or less), or renal tubular obstruction/bladder outlet obstruction (less than 5%); temporary weakness (3.6% or less) and lower limb paresthesia have been reported in a few cases. Additional possible testosterone-related adverse events reported with leuprolide treatment in men with prostate cancer include increased prostatic acid phosphatase (5% or more), balanitis (less than 5%), epididymitis (less than 5%), prostate disorder (less than 5%), testicular soreness/pain (less than 2%), libido increase, and penile swelling; decreased prostatic acid phosphatase occurred in at least 5% of men in 1 study. Spinal fracture/paralysis was reported in postmarketing experience with leuprolide in prostate cancer patients. Aggravation of a preexisting tumor occurred in less than 2% of pediatric patients who received leuprolide.[41676] [45097] [66709] [43800] [66721] [68727]
Unspecified urinary disorders occurred in 10.2% to 16.5% of men with prostate cancer treated with leuprolide in 2 clinical trials. Specific urinary and related laboratory adverse events occurring in men with prostate cancer in various clinical trials include urinary retention (less than 2%), nocturia (9% or less), increased urinary frequency (2.2% to 12%), urinary urgency (less than 2%), frequency/urgency (6.1% or less), dysuria (less than 5%), micturition urgency which included dysuria (6% or less), urinary incontinence (less than 5%), urination difficulty (less than 2%), urination pain (8% or less), scanty urination (less than 2%), bladder spasm (less than 5%), increased or decreased urine specific gravity (5% or more), dehydration (8.2% or less), post void residual, pyuria, and uric aciduria (5% or more).[45097] [66709] [66721] [43800] [68727] Dysuria was also reported in less than 5% of women receiving leuprolide for the treatment of endometriosis, as a possible effect related to decreased estrogen concentrations; renal calculus (nephrolithiasis) occurred in 0.7% of these women. Urinary incontinence occurred in less than 5% of women treated with leuprolide for fibroids and in less than 2% of pediatric patients receiving leuprolide.[42683] [51299] [41676]
Emotional lability or mood swings, and depression have been reported with leuprolide treatment. There have been very rare reports of suicidal ideation and attempt. Many, but not all, of these patients had a history of depression or other psychiatric illness. Patients should be counseled on the possibility of development or worsening of depression during treatment with leuprolide. Monitor patients for worsening of psychiatric symptoms during treatment with leuprolide. Refer patients with new or worsening depression to a mental health professional, as appropriate.[43800] [41676] [65368] [42683] [51299] Depression and mood swings each occurred in less than 5% of men with prostate cancer treated with leuprolide; suicidal ideation and attempt was reported in postmarketing experience.[45097] [66721] [43800] [66709] [68727]. Depression and/or emotional lability was reported in 11% to 31% of women with endometriosis or fibroids treated with leuprolide, and is thought to be a possible effect of decreased estrogen in these patients; serious cases of depression were reported in 0.7% of patients, and both mood swings and suicidal ideation/attempt were reported in postmarketing experience.[42683] [51299] Psychiatric events, including affect lability, affective disorder, aggression, crying, depressed mood, disruptive mood dysregulation disorder, auditory hallucination, altered mood, mood swings, and trichotillomania were reported in 22% of pediatric patients with central precocious puberty (CPP) receiving leuprolide every 6 months. Altered mood occurred in 5% and depression in less than 2% of pediatric patients with CPP treated with leuprolide, while emotional lability (5%), a general emotional disorder (2%), crying, and tearfulness were also reported in this patient population.[41676] [65368] Additional psychiatric effects that occurred in women and were thought to be a possible effect of deceased estrogen included insomnia (31% or less) and anxiety/nervousness (8% or less).[42683] [51299] Anxiety and nervousness were also reported in less than 5% of men with prostate cancer who received leuprolide, and in less than 2% of children with CPP. Insomnia was reported in 8.5% or fewer men with prostate cancer treated with leuprolide, and was reported in 4% of children.[45097] [66709] [66721] [41676] [65368] [43800] Amnesia (6% or fewer) and delusions (less than 5%) were reported in both men and women treated with leuprolide; unspecified memory disorders (memory impairment) were separately reported in less than 5% of men who received leuprolide.[66721] [43800] [42683] [51299] Abnormal thinking, agitation, auditory hallucinations/tinnitus, confusion, dementia, euphoria, and were each reported in less than 5% of men treated with leuprolide.[66721] [43800] Irritability was reported in 2% of leuprolide-treated children, and unspecified personality disorder in less than 5% of treated women.[65368] [42683] [51299]
Nausea/vomiting occurred in 5% to 25% of women with endometriosis or fibroids treated with leuprolide; it was less commonly reported in men with prostate cancer (9% or less). In children with central precocious puberty (CPP), less than 2% of patients experienced nausea and/or vomiting with monthly leuprolide administration compared to 13% with leuprolide administration every 6 months.[45097] [66721] [65368] [41676] [42683] [51299] [68727] Altered bowel function was reported in 14% of women treated with leuprolide.[42683] [51299] Diarrhea was reported in 13% or fewer men with prostate cancer and in 16% of children with CPP receiving leuprolide every 6 months. Constipation was reported by 9% or fewer men and children who received leuprolide.[66721] [45097] [43800] [65368] [41676] [68727] Unspecified GI disturbances were reported in 7% or fewer patients treated with leuprolide. Changes in appetite were reported in 13% or less of treated women, while anorexia occurred in 6% or fewer men and appetite stimulation was reported in less than 5% of men and less than 2% of children; decreased appetite was reported in postmarketing experience in children with CPP who received leuprolide. Weight gain was reported in up to 7% of children and less than 2% of men treated with leuprolide, and was reported in 12% of women; conversely, weight loss occurred in less than 5% of men who received leuprolide.[42683] [51299] [66721] [43800] [65368] [41676] Additional gastrointestinal adverse reactions reported in men and children treated with leuprolide include dyspepsia (less than 2%), dysphagia (less than 5%), and gingivitis (less than 5%).[45097] [66721] [43800] [41676] Xerostomia and thirst occurred in less than 5% of men and women treated with leuprolide.[42683] [51299] [66721] [43800] Adverse reactions only reported in men with prostate cancer who received leuprolide include gum hemorrhage (less than 5%), periodontal abscess (less than 5%), duodenal ulcer (less than 5%), peptic ulcer (less than 5%), abdominal distension (less than 5%), eructation (less than 5%), flatulence (less than 2%), gastroenteritis/colitis (2.5% or less), GI bleeding (less than 5%), occult blood on rectal exam, GI obstruction (less than 5%), rectal fistula/erythema, rectal polyps (less than 5%), and unspecified GI disorders which included dyspepsia and flatulence (0.2% to 16%).[43800] [66721] [45097] Abdominal pain was reported in 8% of men with prostate cancer in 1 study and in up to 18% of children with CPP treated with leuprolide.[65368] [41676] [68727]
A localized injection site reaction including induration, abscess, and skin necrosis has been reported with leuprolide administration.[66721] [43800] [42683] [51299] [41676] [65368] Reactions including pain, erythema, hemorrhage, nodule, paresthesia, pruritus, and warmth at the site occurred in 6% to 37.5% of men with prostate cancer treated with Lupron Depot doses 22.5 mg and higher or Camcevi; the incidence was less than 5% in men receiving the 7.5 mg dose of Lupron Depot and in women with endometriosis or fibroids who also received Lupron Depot (3.75 mg or 11.25 mg doses). A general skin reaction and ecchymosis were each reported in 8.5% or fewer men and women treated with leuprolide; in 1 small study, a general skin was reported in 12.2% of nonorchiectomized men who received leuprolide 30 mg and in 0% of orchiectomized men.[66721] [43800] [66709] [42683] [51299] [68727] Out of 1,338 Eligard injections administered to men with prostate cancer, injection site reactions included mostly brief and mild burning/stinging (16% to 34.6%), pain (2.3% to 4.6%), erythema (0.9% to 2.6%), and bruising (1.7% to 2.5%); pruritus (0.4% to 2.6%), induration (0.4%), and skin ulcer (0.1%) were also reported.[45097] Injection site reactions, including injection site pain, erythema, warmth, bruising, discomfort, and swelling, were reported in 78% of pediatric patients receiving leuprolide every 6 months for central precocious puberty. Mostly mild to moderate injection site reactions including abscess were reported in 9% of pediatric patients receiving leuprolide every month, while injection site pain (19% to 21%) and swelling (2%) were reported in patients receiving leuprolide every 3 months. Sterile abscess, hematoma, induration, and warmth at the injection site were listed as less common injection site reactions. Pruritus (11%) was also reported in this population.[65368] [41676]
Symptoms consistent with anaphylactoid reactions have rarely been reported (0.002%) with leuprolide treatment; anaphylactic reactions to Gonadotropin Releasing Hormone (GnRH) agonists have been reported in the medical literature. General reports of allergic reaction have been reported with leuprolide during clinical trials (estimated incidence less than 2%). Allergic reactions have included rash (less than 2%), urticaria, and photosensitivity reactions.[41676] [42683] [43800] [45097] [51299] [66709] [66721] [65368] Rash, including erythema multiforme, occurred in 3% of pediatric subjects treated with leuprolide monthly and in 7% of subjects receiving leuprolide every 6 months. Rash, urticaria, photosensitivity, erythema multiforme, and bullous dermatitis (bullous rash) were reported during post approval use.[51299]Androgen-like effects of leuprolide in women have included acne (10%) and alopecia (less than 5%). Acneiform rash/seborrhea (3%), alopecia (less than 2%), and hair disorder (less than 2%) were also reported children. Drug-induced body odor and nail disorders were reported in women (less than 5% each) and as less common adverse reactions in children receiving leuprolide.[41676] [42683] [45097] [51299] Skin hypopigmentation (leukoderma) and purpura occurred in less than 2% of children; pallor was reported as a less common adverse reaction. Hyperkeratosis and skin hypertrophy were also reported.[41676] Alopecia/hair disorder (less than 5%), cysts (less than 5%), dermatitis (5%), impaired wound healing (less than 5%), melanosis/melasma (less than 5%), skin hyperpigmentation (less than 5%), skin lesions (less than 5%), xerosis (less than 5%), hyperkeratosis, skin hypertrophy, pallor, blisters on penis, hives, moles, pubic boils, and spiders have been reported in men who received leuprolide for prostate cancer; hair growth was reported in postmarketing experience.[45097] [43800] [41676] [66709] [66721] [65368]
As with other GnRH agonists, there have been reports of ovarian cyst formation (and ovarian enlargement) with the use of leuprolide in females during various types of infertility protocols. When leuprolide is used in combination with gonadotropins, ovarian hyperstimulation syndrome (OHSS) has also occurred.[63289]
Pituitary apoplexy is a syndrome due to a sudden infarction in the pituitary gland. Rare cases of pituitary apoplexy have been reported after the administration of Gonadotropin Releasing Hormone (GnRH) agonists including leuprolide during postmarketing surveillance. In most cases, a pituitary adenoma was diagnosed. A majority of pituitary apoplexy cases occur within 2 weeks of the first dose and some within the first hour. In these cases, pituitary apoplexy has presented as a sudden and severe headache, nausea/vomiting, visual changes including reduction in visual field and ophthalmoplegia, altered mental status, and sometimes cardiovascular collapse. The presence of acute visual loss (e.g., bitemporal hemianopia or hemianopsia) and ocular paresis (reductions in ocular movements from involvement of cranial nerves III, IV, and VI) can assist in the diagnosis. Immediate medical management may be required; management strategies include close observation, corticosteroid administration, maintenance of fluid and electrolyte balance, and possibly surgical decompression of the pituitary fossa.[31507] [31508] [66709] [45097] [66721] [43800] [65368] [41676] [42683] [51299] [68727]
Treatment with leuprolide can cause decreased bone mineral density (BMD) which can result in osteopenia and a risk for osteoporosis. In women with endometriosis treated with leuprolide, the mean change in BMD of the lumbar spine from baseline at week 24 (n = 41) was -3.2% and at week 52 (n = 29) was -6.3%; in patients who received leuprolide plus norethindrone, the mean change from baseline at week 24 (n = 42) was -0.3% and at week 52 (n = 32) was -1%. Eight months after discontinuation of therapy, the mean change from baseline in patients treated with leuprolide was -3.3% compared with -0.9% for those who received leuprolide/norethindrone; at 12 months, the mean change from baseline was -2.2% versus -0.7%, respectively. In patients receiving leuprolide for the treatment of uterine fibroids, vertebral trabecular BMD showed a mean decrease of 2.7% from baseline at 3 months; a trend toward recovery was observed 6 months after discontinuation of therapy.[51299] [42683] Reduced BMD has also been reported in published literature and postmarketing in pediatric patients with central precocious puberty treated with leuprolide. Published studies have indicated that after discontinuation of leuprolide therapy in children, subsequent bone mass accrual is preserved and peak bone mass in late adolescence does not seem to be affected.[41676] Long periods of medical castration in men can be anticipated to have effects on bone density. Decreased BMD has been reported in men treated with a Gonadotropin Releasing Hormone (GnRH) or a Luteinising Hormone-Releasing Hormone (LHRH) agonist analog. In a clinical trial, 25 men with prostate cancer, 12 of whom had been treated previously with leuprolide acetate for at least 6 months, underwent BMD studies as a result of pain. The leuprolide-treated group had lower bone density scores than the non-treated control group. Pathological bone fractures were reported in less than 5% of men with prostate cancer treated with leuprolide.[45097] [66721] [43800] [66709] [68727]
General complaints of pain (4.2% to 32.7%) and joint disorders (8% to 16.3%) were reported in men with prostate cancer and women with endometriosis or fibroids who were treated with leuprolide in clinical trials; joint disorders were considered to be a possible effect of decreased estrogen status in women.[42683] Arthralgia (1.3% to 11%), extremity pain (10% or less), musculoskeletal pain including back pain and bone pain (11% or less), myalgia (8.2% or less) occurred in men who received leuprolide for prostate cancer in clinical trials. Additional musculoskeletal adverse reactions reported in men treated with leuprolide include ankylosing spondylosis, arthritis, back pain (less than 2%), blurred disc margins, disc hernia (less than 5%), inguinal hernia, joint pain (less than 5%), leg cramps (less than 5%), limb pain (2.7% or less), muscle atrophy (less than 2%), muscle stiffness, muscle tenderness, neck pain (less than 5%), pelvic fibrosis, accidental injury, and knee effusion. Muscle cramps/spasms were reported postmarketing.[66709] [66721] [43800] [51299] [68727] Fibromyalgia and tenosynovitis-like symptoms have been reported postmarketing in both men and women.[66709] [66721] [43800] [42683] [51299] General pain (3%), extremity pain (9%), back pain (7%), ligament sprain (7%), fracture, including ankle and tibia fractures (4%), arthralgia (less than 2%), myalgia (less than 2%), and joint disorders (less than 2%) were reported in pediatric patients with central precocious puberty (CPP). Hyperkinesis, myopathy, antinuclear antibody present, and increased sedimentation rate were also reported in less than 2% of pediatric patients who received leuprolide; synovitis and epiphysiolysis have been reported in postmarketing experience.[65368] [41676]
Hyperglycemia (at least 5% in some studies; less than 5% in others) and an increased risk of developing diabetes mellitus have been reported with the use of Gonadotropin Releasing Hormone (GnRH) agonists in men; diabetes has also been reported in postmarketing experience in pediatric studies with leuprolide. The risk for diabetes in women is unknown due to a lack of data. Periodically monitor blood glucose concentration and/or glycosylated hemoglobin (HbA1c) in those receiving leuprolide therapy. Manage patients according to current clinical practice.[40127] [42683] [66709] [45097] [66721] [43800] [65368] [41676] [68727]
Leukopenia was noted in at least 5% of men with prostate cancer who received leuprolide; leukopenia occurred in more than 10% of men with prostate cancer who received 1 formulation of leuprolide (Lutrate Depot), while decreased white blood cells (WBC) have also been reported in postmarketing experience with all other populations treated with leuprolide products. Increased WBC and eosinophilia have each occurred in at least 5% of men treated with leuprolide. Decreased red blood cells, hematocrit, and hemoglobin were reported in less than 5% of men who received leuprolide; anemia was reported in 5% or less of these patients and in more than 10% of patients treated with Lutrate Depot. In one study, 13.9% of men had a grade 1 or 2 decreased hemoglobin at baseline; during treatment with Lupron Depot, grade 1 (42.4%), grade 2, (2%), and grade 3 or 4 (1.3%) hemoglobin reductions were reported. Thrombocytopenia and decreased platelets were each reported in at least 5% of men; increased platelets were also reported in at least 5% of patients in this population. Additionally, prolonged bleeding time (increased PT and PTT) occurred in at least 5% of men with prostate cancer treated with leuprolide in one clinical trial.[41676] [42683] [43800] [45097] [51299] [65368] [66709] [66721] [68727]
Fever/chills was reported in less than 5% of men with prostate cancer treated with leuprolide and fever in 17% or fewer children with central precocious puberty (CPP) treated with leuprolide. General reports of infection or inflammation were reported in 5.4% or fewer men who received leuprolide and was a reported as a less common adverse reaction in patients with CPP.[66721] [43800] [65368] [41676] Urinary tract infection (UTI) occurred in 7% or fewer men treated with leuprolide; in one small study, 6.6% of men reported UTI/cystitis during treatment but was not felt to be related to treatment in any patient. Serious cases of UTI were reported in 1.9% of women with endometriosis who received leuprolide; pyelonephritis was reported in women with fibroids treated with leuprolide 7.5 mg monthly but not in those who received 3.75 mg monthly.[66721] [43800] [42683] [51299] [68727] Upper respiratory infection (URI) was reported in 17% or fewer men with prostate cancer and children with CPP treated with leuprolide in clinical trials; in one trial, URI occurred in 21.2% of men who received leuprolide but was not felt to be related to therapy in any patient.[66709] [43800] [65368] [68727] In all populations treated with leuprolide including women with endometriosis or fibroids, influenza (less than 5%), rhinitis (less than 5%), and sinusitis (less than 5%) were reported.[66721] [43800] [41676] [42683] [51299] Pharyngitis occurred in less than 5% of men while strep throat was also reported; nasopharyngitis occurred in 22% or fewer pediatric patients.[43800] [41676] [65368] Additional infection-related events reported in men who received leuprolide include abscess (less than 5%), bronchitis (less than 5%), cellulitis (less than 5%), lymphadenopathy (less than 5%), pneumonia (less than 5%; serious cases, at least 2%), pulmonary infiltrates, and shingles/herpes zoster (less than 5%).[66721] [43800]
Respiratory disorders (10.7% or less) reported in men with prostate cancer treated with leuprolide, included: asthma (less than 5%), chest tightness, decreased breath sounds, cough (less than 5%), dysphonia (less than 5%), dyspnea (less than 2%) emphysema (less than 5%), epistaxis (less than 5%), hemoptysis (less than 5%), hiccups (less than 5%), hypoxia (less than 5%), lung disorder (less than 5%), pleuritic chest pain, pleural effusion (less than 5%), pleural rub (less than 5%), pulmonary edema (less than 5%), pulmonary fibrosis (less than 5%), rales/rhonchi, sinus/nasal congestion (5% or less), wheezing (less than 5% and often associated with URI), and increased sputum (less than 5%); interstitial lung disease was reported in postmarketing experience with leuprolide. Cough (13% or less), productive cough (6% or less), bronchospasm (6% or less), and asthma (less than 2%) were also reported in children with central precocious puberty treated with leuprolide, along with epistaxis (less common), and dyspnea (postmarketing). Asthma or wheezing was also reported in leuprolide-treated women with pre-existing histories of asthma or environmental or drug allergies.[42683] [51299] [66721] [43800] [41676] [65368] [68727]
In men, an increased risk of myocardial infarction, sudden cardiac death, and stroke has been reported in association with the use of Gonadotropin Releasing Hormone (GnRH) agonists; the risk appears to be low based on the reported odds ratios. Carefully evaluate cardiovascular risk factors when determining the treatment plan for men with prostate cancer. Monitor patients for signs and symptoms suggestive of the development of cardiovascular disease; if cardiac disease develops, manage patients according to current clinical practice.[66721] [43800] [45097] [66709] [68727] At this time, there are no known comparable studies evaluating the risk of cardiovascular disease in women or children taking GnRH agonists for other indications.[42122] Leuprolide may cause QT prolongation. Ischemia/ECG changes occurred in up to 19% of men with prostate cancer treated with leuprolide.[66721] [68727] Palpitations and sinus tachycardia were each reported in less than 5% of adults (men and women) treated with leuprolide while myocardial infarction occurred in less than 5% of men and in postmarketing experience with women. Stroke and transient ischemic attack (TIA) were reported in men who received leuprolide and in postmarketing experience with women; serious cases of stroke/TIA occurred in at least 2% of men who received Lupron Depot in one study. Phlebitis/thrombosis occurred in 2% or fewer men who received leuprolide. Deep thrombophlebitis/DVT/thromboembolism and pulmonary embolism each occurred in less than 5% of men and in postmarketing experience with women. Ruptured aortic aneurysm, atrial fibrillation (less than 5%), cardiac arrhythmias (less than 5%), carotid bruit, extrasystole, heart failure (less than 5%), and murmur (3% or less) were also reported in leuprolide-treated men.[66721] [43800] [42683] [51299] Hypertension occurred in 15% of men with prostate cancer treated with leuprolide mesylate (Camcevi), in 8.3% or fewer men receiving leuprolide acetate, in less than 2% of children with central precocious puberty (CPP) who received leuprolide acetate, and in postmarketing experience with women with endometriosis or fibroids treated with leuprolide acetate. Hypotension occurred in less than 5% of men and in postmarketing experience with leuprolide in other populations; syncope was reported in less than 5% of adults and in less than 2% of children treated with leuprolide.[66709] [45097] [66721] [43800] [65368] [41676] [42683] [51299] [68727] Angina related to treatment was reported in less than 5% of leuprolide-treated men while chest pain (unspecified) was reported in 4% of children.[66721] [43800] [65368] [41676] Bradycardia occurred in less than 5% of men and less than 2% of children who received leuprolide; varicose veins were reported in less than 5% of men and peripheral vascular disorder in less than 2% of children.[66721] [43800] [41676]
Although the relationship to drug treatment is difficult to assess in this population, various laboratory abnormalities were reported in men with prostate cancer treated with leuprolide, including decreased bicarbonate (5% or more), hyperphosphatemia (5% or more), hyperuricemia (5% or more), increased BUN (Lupron Depot, 5% or more; Lupron, less than 5%), increased creatinine (Lupron Depot, 5% or more; Lupron, less than 5%), and increased calcium (hypercalcemia) (less than 5%). Decreased potassium concentrations (hypokalemia) was also reported in clinical trials and postmarketing experience.[43800] [66721]
During the early phase of therapy, because gonadotropins and sex steroids rise above baseline because of the initial stimulatory effect of the drug, an increase in clinical signs and symptoms of puberty may also be observed in pediatric patients during the first weeks of therapy or after subsequent doses; vaginitis/vaginal bleeding/vaginal discharge occurred in 3% of pediatric patients with central precocious puberty in one study; vaginal bleeding was reported in postmarketing experience with pediatric patients receiving leuprolide.[41676] [65368] In women receiving leuprolide for endometriosis or uterine fibroids, an increase in symptoms may be observed during the initial days of therapy, but these should dissipate with continued therapy. Endocrine adverse effects in women treated with leuprolide have included menstrual irregularity (changes in vaginal bleeding patterns or other menstrual disorders) and lactation (galactorrhea).[42683]
Seizures occurred in less than 5% of men with prostate cancer treated with leuprolide in one clinical trial and have been reported during postmarketing surveillance in patients with a history of epilepsy, cerebrovascular disease, central nervous system anomalies or brain tumor, and patients on concomitant medications that have been associated with seizures. Seizures have also been reported in patients without any risk factors. Manage patients receiving leuprolide who experience convulsions according to current clinical practice.[41676] [43800] [51299] [66709] [42683] [65368] [45097] [66721] [68727]Pseudotumor cerebri (idiopathic intracranial hypertension) has been reported in pediatric patients during postmarketing experience.[41676] [65368] Dizziness (including vertigo) was reported in 2% to 8.3% (grade 3 or 4, 0.7% or less) of men with prostate cancer treated with leuprolide; dizziness was also individually reported in 3.3% to 7% and vertigo in less than 2%.[45097] [66709] [66721] [43800] Dizziness and/or vertigo occurred in 11% to 16% of women treated with leuprolide for endometriosis or fibroids, and was reported as a less common adverse reaction in pediatric patients treated for central precocious puberty.[51299] [42683] [41676] Taste perversion or disorders (dysgeusia) were reported in less than 5% of men and women treated with leuprolide.[66721] [51299] [42683] [45097] Additional CNS-related adverse reactions reported in men with prostate cancer included hyperreflexia (less than 5%), hyporeflexia (less than 5%), loss of smell (parosmia, less than 5%), rigors (less than 2%), and tremor (less than 2%).[66721] [45097] Gait disturbance was a less commonly reported adverse reaction in pediatric patients treated with leuprolide.[41676]
Ocular adverse reactions occurring in less than 5% of men with prostate cancer treated with leuprolide include visual impairment, amblyopia, blurred vision, ptosis, and xerophthalmia; eyelid growth and perivascular cuffing of the eye were also reported in men treated with leuprolide.[43800] [66721] Unspecified ophthalmologic disorders that were possibly an effect of decreased estrogen and conjunctivitis were also reported in less than 5% of women with endometriosis or fibroids treated with leuprolide.[42683] [51299] Decreased vision was a less common adverse reaction reported in pediatric patients with central precocious puberty treated with leuprolide.[41676]
Paresthesias occurred in 8.2% or fewer men with prostate cancer treated with leuprolide in clinical trials; they also occurred in 7% of women with endometriosis who received lower doses of leuprolide in one study.[66721] [43800] [42683] [51299] Neuromuscular disorders (i.e., leg cramps, paresthesia) were reported in less than 9.6% of men with prostate cancer who received leuprolide and in 2% to 7% of women with endometriosis in 2 studies as a possible effect of decreased estrogen.[43800] [42683] [51299] Additional adverse events reported in men with prostate cancer treated with leuprolide include hyperesthesia (less than 5%), motor deficiency (less than 5%), neuropathy (less than 5%), numbness (less than 5%), peripheral neuropathy (less than 5%), weakness (3.6% or less), and "feet burning".[45097] [66721] [43800] [66709] Peripheral neuropathy also occurred in postmarketing experience with women treated with leuprolide.[42683] [51299]
Headache (26% to 65%) was commonly reported in women with endometriosis or fibroids treated with leuprolide in clinical trials, possibly as an effect of decreased estrogen; it was less common in men with prostate cancer treated with leuprolide (10.2% or less) and in children with central precocious puberty (CPP) who received leuprolide treatment.[42683] [51299] [66721] [43800] [65368] [41676] [68727] Asthenia (12.2% or less), fatigue (including asthenia) (15% or less), fatigue/malaise (17.5% or less), fatigue/lethargy (11.9% or less), fatigue as a stand-alone term (less than 5%), and lethargy as a stand-alone term (less than 5%) were also reported in men who received leuprolide across clinical trials.[66721] [43800] [66709] [45097] [68727] Asthenia occurred in 8% to 18% of women treated with leuprolide, and was a less commonly reported adverse reaction in children with CPP; somnolence occurred in less than 2% of children with CPP who received leuprolide and fatigue was reported in postmarketing experience.[65368] [41676] [42683] [51299] Decreased hearing/hearing loss and hearing disorders were reported in postmarketing experience in men treated with leuprolide.[66721]
Elevated hepatic enzymes (2 x baseline and above the upper limit of normal) occurred in 1% to 3% of women with endometriosis or fibroids treated with leuprolide; the increases observed in most (83.3%) of the women with endometriosis occurred beyond 6 months of treatment.[42683] [51299] Increased liver function tests (e.g., ALT, AST, GGTP, LDH) were also reported in at least 5% of men with prostate cancer treated with leuprolide, along with hypoalbuminemia (5% or more) and decreased total protein (5% or more). Hepatomegaly occurred in less than 5% of men treated with leuprolide, while hepatitis and hepatic dysfunction were also reported. Serious drug-induced liver injury (hepatotoxicity) was reported in both men and women treated with leuprolide in postmarketing experience.[66709] [66721] [43800] [42683] [51299] [68727]
Hypercholesterolemia has been reported with leuprolide treatment. In women with normal baseline cholesterol, the mean cholesterol increase was 16 to 17 mg/dL in women with endometriosis (p less than 0.03) and 11 to 29 mg/dL in women with uterine fibroids; after 24 weeks of follow-up, the percent-change from baseline was 9.2% for total cholesterol, 7.4% for HDL, 10.9% for LDL, 5% for the LDL/HDL ratio, and 17.5% for triglycerides; the major impact of adding norethindrone to treatment was a decrease in HDL cholesterol and an increase in the LDL/HDL ratio. Lipid concentrations outside the normal range at week 0 and week 24 of leuprolide treatment in women included total cholesterol (more than 240 mg/dL; 15% and 23%), HDL cholesterol (less than 40 mg/dL; 15% and 10%), LDL cholesterol (more than 160 mg/dL; 0% and 8%), LDL/HDL ratio (more than 4; 0% and 3%); the percentage of women with triglyceride concentrations outside the normal range (hypertriglyceridemia) was unchanged (13%). Changes from baseline tended to be greater at week 52; after treatment, mean serum lipid concentrations in women with follow-up data returned to pretreatment values.[42683] [51299] At least 5% of men with prostate cancer treated with leuprolide experienced hyperlipidemia (total cholesterol, LDL cholesterol, triglycerides) and/or decreased HDL cholesterol. In men treated with Lupron Depot 45 mg every 6 months, 28.5% had grade 1 or 2 increases in cholesterol at baseline; grade 1 or 2 increases (200 to 300 mg/dL) during the study occurred in 55%, grade 2 increases (301 to 400 mg/dL) in 3.3%, and grade 3 increases (greater than 400 mg/dL) in 0.7% of men.[43800] [68727]
A goiter occurred in less than 2% of children with central precocious puberty treated with leuprolide in one clinical trial.[41676] Thyroid enlargement, thyroid nodule, and a hard nodule in the throat were each reported in less than 5% of men with prostate cancer treated with leuprolide.[66721]
Edema was generally reported in 14.3% or fewer men with prostate cancer and women with endometriosis or fibroids who received leuprolide, although 1 small study suggested the incidence was higher in orchiectomized men compared to nonorchiectomized (20.8% vs. 8.2%). Swelling of the temporal bone occurred in less than 5% of men, while facial swelling/edema was also reported. Peripheral edema occurred in 12% or fewer men treated with leuprolide and in less than 2% of children.[66709] [45097] [66721] [43800] [65368] [41676] [42683] [51299]
New primary malignancy has been reported in men with prostate cancer treated with leuprolide including bladder cancer (less than 5%), cancer of the skin/ear (less than 5%), and a generalized mass.[41676] [66721] [66709] In one study, a second primary neoplasm was emergent in 7.3% of men who received leuprolide including basal cell carcinoma, bladder transitional cell carcinoma, lung cancer, malignant melanoma, non-Hodgkin's lymphoma, and squamous cell carcinoma; however, none of these cases were felt to be related to treatment.[43800] A cervix disorder/neoplasm occurred in less than 2% of children with central precocious puberty who received leuprolide.[41676]
Severe cutaneous adverse reactions (SCARs) have been reported in people receiving Gonadotropin-Releasing Hormone (GnRH) agonists, including leuprolide. These reactions include exfoliative dermatitis, Stevens-Johnson syndrome / toxic epidermal necrolysis (SJS/TEN), Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP), including cases with visceral involvement and/or requiring skin grafts. Monitor leuprolide recipients for the signs and symptoms of SCARs such as fever, flu-like symptoms, mucosal lesions, progressive skin rash, or lymphadenopathy. Advise people of the signs and symptoms of SCARs. If a SCAR is suspected, interrupt leuprolide until the etiology of the reaction has been determined. Consultation with a dermatologist or health care team member with expertise in the diagnosis and management of SCARs is recommended. If a diagnosis is confirmed, or for other grade 4 skin reactions, permanently discontinue leuprolide.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Since leuprolide suppresses the pituitary-gonadal axis, laboratory test interference may occur with diagnostic tests for pituitary insufficiency or other pituitary-gonadal function conducted during treatment and after cessation of therapy.[45097] [43800] [66721] [68727] Normal function of the pituitary-gonadal system is usually restored within 4 to 12 weeks after treatment is discontinued;[43800] [66721] [68727] in pediatric patients, normal function may be restored within 6 months.[41676]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Leuprolide is contraindicated in individuals with undiagnosed abnormal uterine bleeding.[42683] [51299]
Carefully weigh the risks and benefits of leuprolide therapy in patients at increased risk for osteoporosis, including those with chronic alcohol use (more than 3 units per day), tobacco smoking, strong family history of osteoporosis, or chronic use of drugs that can decrease bone marrow density (BMD) such as anticonvulsants or corticosteroids. The duration of therapy for the treatment of endometriosis and fibroids should not exceed 12 months due to the risk of loss of BMD. The addition of hormone replacement therapy (norethindrone acetate) to leuprolide therapy for endometriosis or uterine fibroids may be effective in reducing bone mineral loss in women. Once norethindrone is added, do not retreat with leuprolide without combination norethindrone; assess BMD prior to retreatment with leuprolide/norethindrone.[51299] [42683]
Use leuprolide with caution in people with baseline QT prolongation or who have conditions that may increase the risk of QT prolongation or torsade de pointes, including bradycardia, congenital long QT syndrome, hypocalcemia, hypokalemia, hypomagnesemia, geriatric adults, females, structural abnormalities that interfere with electrical conduction (e.g., cardiomyopathy, coronary artery disease, ischemic heart disease), or in those who have other additional risk factors for QT prolongation or torsade de pointes. The use of other medications that have been associated with QT prolongation or torsade de pointes may further increase risk.[65180] [67452] [72115] [72116] [72117] [72118] If use is necessary, correct any baseline electrolyte abnormalities and consider periodic monitoring of both electrocardiograms and electrolytes. Additionally, carefully evaluate the risk of coronary artery disease in prostate cancer patients to be treated with leuprolide due to an increased risk of myocardial infarction, sudden cardiac death, and stroke associated with GnRH agonists in men.[43800] [45097] [65368] [66709] [66721] [68727]
Use leuprolide with caution in patients with a history of seizures, brain injury, stroke, or brain tumor. Seizures have occurred in patients treated with leuprolide, both with and without risk factors. Patients should be advised of the risk of developing a seizure and of engaging in any activity where sudden loss of consciousness could cause harm to themselves or others during leuprolide treatment (e.g., driving or operating machinery or performing activities requiring coordination and concentration).[43800] [45097] [65368] [66709] [66721] [68727]
Evaluate the risk of potential new or worsening psychiatric events versus the benefits of treatment with leuprolide in patients with a history of a major psychiatric disorder. During postmarketing experience, emotional lability, such as crying, irritability, impatience, anger, and aggression were reported. Depression, including rare reports of suicidal ideation and attempt, were reported in children treated with GnRH agonists for central precocious puberty. Many, but not all, of these patients had a history of psychiatric illness or other comorbidities with an increased risk of depression. Counsel patients on the possibility of development or worsening of depression during leuprolide receipt, and to report any unusual changes in moods or behavior.[41676] [42683] [51299] [65368] [65368] [68727]
Leuprolide is contraindicated during pregnancy. There are no adequately controlled studies of leuprolide use during human pregnancy. However, leuprolide can cause fetal harm when administered during pregnancy based on its mechanism of action and data from animal studies. In animal reproductive studies, administration of leuprolide to pregnant rabbits during the period of organogenesis caused embryo-fetal toxicity, decreased fetal weights, and a dose-dependent increase in major fetal malformations at doses less than the recommended human dose based on body surface area. A similar study in rats showed increased fetal mortality and decreased fetal weights, but no major fetal abnormalities.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Counsel people who may become pregnant and people who can cause pregnancy in others about the reproductive risk associated with leuprolide. Leuprolide may cause fetal harm. Verify pregnancy status prior to treatment initiation, if clinically indicated. Advise people who may become pregnant to use effective non-hormonal contraception while taking leuprolide. When used at the recommended dose and dosing interval, leuprolide usually inhibits ovulation and stops menstruation; however, contraception is not ensured by taking leuprolide. Based on its mechanism of action, leuprolide can cause male and female infertility.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Use leuprolide with caution during breast-feeding. There are no data on the presence of leuprolide in human milk, its effects on the breast-fed child, or its effects on milk production. Consider the benefits of breast-feeding, the patient's clinical need for treatment, and any potential adverse effects on the breast-fed child from the medication or from the patient's underlying medical condition.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Leuprolide is a synthetic nonapeptide analog of naturally occurring Gonadotropin Releasing Hormone (GnRH) that possesses greater potency than the natural hormone. As a long-acting GnRH agonist, it acts as a potent inhibitor of gonadotropin secretion (luteinizing hormone [LH] and follicle stimulating hormone [FSH]) when given continuously in therapeutic doses. In both animal and human studies, after an initial stimulation of pituitary gonadotropins, chronic administration results in a down-regulation of GnRH receptors, reduction in the release of LH and FSH, and consequent suppression of ovarian and testicular steroidogenesis. Consequently, tissues and functions that depend on gonadal steroids for their maintenance become quiescent. This effect is reversible after discontinuation of therapy.[66709][45097][66721][43800][65368][41676][42683][51299][68727]
In humans, subcutaneous administration of single daily doses of leuprolide initial increases circulating levels of LH and FSH, which transiently increases levels of gonadal steroids (testosterone and dihydrotestosterone in males, and estrone and estradiol in premenopausal females). However, continuous daily administration decreases LH and FSH concentrations. In males, testosterone concentrations are reduced to below castration levels (50 ng/dL or less) within 2 to 4 weeks after initiation of treatment; castration levels of testosterone in men with prostate cancer have been demonstrated for up to 7 years.[66709][45097][66721][43800][68727] Normal function of the pituitary-gonadal system is usually restored within 3 months after treatment is discontinued; diagnostic tests of pituitary gonadotropic and gonadal functions conducted during treatment and for up to 3 months after discontinuation may be affected.[42683][51299]
Administration of leuprolide inhibits growth of certain hormone-dependent tumors (prostatic tumors in Noble and Dunning male rats and DMBA-induced mammary tumors in female rats) as well as atrophy of the reproductive organs.[66721][43800][68727]
Revision Date: 10/06/2025, 07:43:13 AMLeuprolide is administered subcutaneously or intramuscularly; it is not active when administered orally. In vitro binding to human protein ranged from 43% to 49%. The mean steady-state volume of distribution was 27 liters after an IV bolus in healthy male volunteers. The mean systemic clearance of leuprolide was 7.6 L/hour to 8.34 L/hour after an IV bolus in healthy male volunteers, with a terminal elimination half-life estimated to be about 3 hours based on a 2-compartment model.[66709][45097][66721][43800][65368][41676][42683][51299][68727] Leuprolide is metabolized to smaller inactive peptides including a pentapeptide which is the major metabolite (Metabolite I; M1), tripeptides (Metabolites II and III), and a dipeptide (Metabolite IV) which may then be further catabolized.[66709][66721][65368][41676][68727] Plasma concentrations of M1 were approximately 6% of the peak parent drug concentration; one week after dosing, mean M1 concentrations were approximately 20% of mean leuprolide concentrations. Following IM administration of leuprolide to 3 patients, less than 5% of the dose was recovered in the urine as parent and M1 metabolite.[66721][43800][41676][42683][51299] The excretion of leuprolide has not been evaluated with the extended-release subcutaneous formulations (i.e., Eligard, Fensolvi, and Camcevi).[66709][45097][65368]
Affected cytochrome P450 isoenzymes: None
Leuprolide acetate is primarily degraded by peptidase. Although drug interaction studies have not been conducted, leuprolide is not degraded by CYP450 enzymes thus drug interactions associated with these enzymes are not expected to occur.[66721][42683][51299][41676]
The Cmax of leuprolide ranged from 4.6 ng/mL to 10.2 ng/mL at 4 hours after a single IM injection of leuprolide 3.75 mg in healthy female volunteers; after the initial rise, leuprolide concentrations began to plateau within 2 days after dosing and remained relatively stable for 4 to 5 weeks with plasma concentrations of about 0.3 ng/mL.[51299] After a single IM injection of leuprolide 11.25 mg in female subjects, a mean plasma concentration of 36.3 ng/mL was observed at 4 hours; mean levels declined to near the lower limit of detection by 12 weeks, with the mean leuprolide concentration from 3 to 12 weeks at 0.23 +/- 0.09 ng/mL. There was no statistically significant difference in changes of serum estradiol concentrations from baseline in a pharmacokinetic/pharmacodynamic study of endometriosis patients treated with leuprolide 3.75 mg IM every 4 weeks or 11.25 mg IM every 12 weeks.[42683]
Mean peak plasma concentrations were 20 ng/mL, 48.9 ng/mL, and 59.3 ng/mL at 4 hours after administration in patients after a single IM injection of Lupron Depot 7.5 mg, 22.5 mg, and 30 mg, respectively; mean peak plasma concentrations of 6.7 ng/mL were observed 2 hours after IM administration of leuprolide acetate 45 mg. Plasma concentrations decreased to 0.36 ng/mL 4 weeks after administration of leuprolide 7.5 mg; 0.67 ng/mL 12 weeks after administration of 22.5 mg; 0.3 ng/mL 16 weeks after administration of 30 mg; and 0.07 ng/mL 24 weeks after administration of 45 mg.[43800] After 2 sequential IM injections of Lutrate Depot 22.5 mg with a 3-month interval, the mean plasma concentration of leuprolide obtained at 2 hours after administration was 46.8 ng/mL; the mean concentration then declined until the next administration.[68727] Plasma concentrations of M1 in prostate cancer patients (n = 5) reached maximum concentrations 2 to 6 hours after dosing.[66721] For the 3-month, 4-month, and 6-month formulations, the initial peak followed by a decline to steady-state concentrations was similar to the release pattern seen with the monthly formulation. Intact leuprolide and an inactive major metabolite could not be distinguished by the assay employed in the studies.[43800][42683][51299] Leuprolide appears to be released at a constant rate following the onset of steady-state concentrations during the third week after dosing, providing steady plasma concentrations through the dosing interval.[43800][42683]
The bioavailability of leuprolide after subcutaneous administration is comparable to that by IV injection.[66721] Leuprolide concentrations are variable, exhibiting an initial rapid increase followed by a rapid decline over the first 3 days before reaching steady concentrations for the remainder of the dosing interval. The mean Cmax of leuprolide mesylate (Camcevi)was 94.5 ng/mL to 99 ng/mL, with mean serum concentrations maintained between 0.497 ng/mL to 2.57 ng/mL after the third day; the median Tmax was 2.1 to 3.2 hours. The mean AUC was between 224 ng x day/mL and 268 ng x day/mL.[66709] The mean Cmax of leuprolide acetate (Eligard) after subcutaneous administration to men with prostate cancer was 25.3 ng/mL for those receiving 7.5 mg once monthly; 127 ng/mL for those receiving 22.5 mg every 3 months; 150 ng/mL for those receiving 30 mg every 4 months, and 82 ng/mL for those receiving 45 mg every 6 months. The Tmax ranged from 3.3 to 5 hours in these patients. Following a single dose, serum concentrations at the end of each dosing interval were 0.42 ng/mL for the 7.5 mg dose; 0.34 ng/mL for the 22.5 mg dose; 0.1 ng/mL for the 30 mg dose; and 0.2 ng/mL for the 45 mg dose. After the initial increase following each subcutaneous injection, serum concentrations ranged from 0.1 ng/mL to 2 ng/mL. There was no evidence of significant accumulation during repeated dosing.[45097]
The effect of hepatic impairment on the pharmacokinetics of leuprolide has not been evaluated.[66709][45097][66721][65368][41676][42683][51299]
The effect of renal impairment on the pharmacokinetics of leuprolide has not been evaluated.[66709][45097][66721][65368][41676][42683][51299]
Leuprolide for 1-month administration
Mean trough plasma concentrations in children with central precocious puberty after initial doses of leuprolide 7.5 mg, 11.25 mg, and 15 mg for 1-month administration were 0.77, 1.25, and 1.59 ng/mL, respectively. Concentrations after 3 and 6 doses were similar to those seen after the first dose.[41676]
Leuprolide for 3-month administration
In children with central precocious puberty who received a single intramuscular injection of leuprolide 11.25 mg or 30 mg for 3-month administration, leuprolide concentrations increased with increasing dose; mean peak leuprolide plasma concentrations were 19.1 and 52.5 ng/mL at 1 hour for the 11.25 and 30 mg dose levels, respectively. At 2 weeks post dose, the concentrations declined to 0.08 and 0.25 ng/mL for the 11.25 and 30 mg dose levels, respectively. The mean leuprolide plasma concentration remained constant from month 1 to month 3 for both 11.25 and 30 mg doses. Repeated administration did not lead to leuprolide accumulation.[41676]
Leuprolide for 6-month administration
In children with central precocious puberty who received a single intramuscular injection of leuprolide 45 mg, leuprolide mean peak plasma concentration increased rapidly to 15.7 ng/mL 1 hour post dose and declined to 0.03 ng/mL by week 24. The mean leuprolide plasma concentrations were similar 6 months after the first and second injections indicating no accumulation.[41676] In children with central precocious puberty who received a single subcutaneous injection of leuprolide 45 mg, concentrations peaked 4 hours post dose with a mean peak leuprolide plasma concentration of 212.3 ng/mL. Absorption occurred in 2 phases, a burst phase followed by a plateau phase. The mean plateau serum leuprolide concentration from 4 to 48 weeks was approximately 0.37 ng/mL with a range of 0.18 to 0.63 ng/mL. There was no accumulation of leuprolide after the second dose.[65368]
Age (51 to 88 years) did not have a clinically significant effect on the exposure of leuprolide mesylate.[66709]
Race/ethnicity (White, Black, Asian) did not have a clinically significant effect on the exposure of leuprolide mesylate.[66709] Mean concentrations of leuprolide acetate were also similar regardless of race (White, Black, Hispanic).[45097]
Body weight (54 to 134 kg) did not have a clinically significant effect on the exposure of leuprolide mesylate.[66709]
Leuprolide is contraindicated during pregnancy. There are no adequately controlled studies of leuprolide use during human pregnancy. However, leuprolide can cause fetal harm when administered during pregnancy based on its mechanism of action and data from animal studies. In animal reproductive studies, administration of leuprolide to pregnant rabbits during the period of organogenesis caused embryo-fetal toxicity, decreased fetal weights, and a dose-dependent increase in major fetal malformations at doses less than the recommended human dose based on body surface area. A similar study in rats showed increased fetal mortality and decreased fetal weights, but no major fetal abnormalities.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Use leuprolide with caution during breast-feeding. There are no data on the presence of leuprolide in human milk, its effects on the breast-fed child, or its effects on milk production. Consider the benefits of breast-feeding, the patient's clinical need for treatment, and any potential adverse effects on the breast-fed child from the medication or from the patient's underlying medical condition.[41676] [43800] [45097] [51299] [65368] [66709] [66721]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.