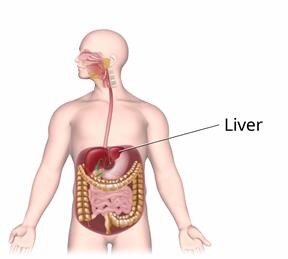
Liver Failure
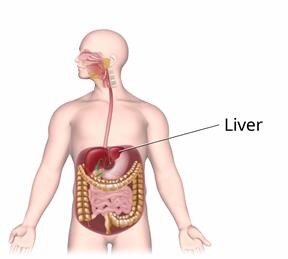
The liver is a large organ in the upper right-hand side of the abdomen. It is involved in many important functions, including storing energy, producing fluids that the body needs, and removing harmful substances from the bloodstream.
Liver failure is a condition in which the liver loses its ability to function due to injury or disease. Liver failure can develop quickly, over days or weeks (acute liver failure). It can also develop gradually, over months or years (chronic liver failure).
What are the causes?
Common causes of chronic liver failure include:
Viral hepatitis.
Liver disease.
Alcohol abuse.
Common causes of acute liver failure include:
What are the signs or symptoms?
Most people do not have symptoms in the early stages of liver failure. If early symptoms do develop, they may include:
As the condition worsens, symptoms of this condition may include:
Yellowing of the skin and the whites of the eyes (jaundice).
Bruising and bleeding easily.
Itchy skin.
Fluid buildup in the abdomen (ascites).
Personality and mood changes.
Confusion and sleepiness.
How is this diagnosed?
This condition is diagnosed based on your symptoms, your medical history, and a physical exam. You may have tests, including:
How is this treated?
Treatment for this condition depends on the cause and the severity of symptoms.
Treatment for chronic liver failure may include:
Medicines to help reduce symptoms.
Lifestyle changes, such as limiting salt and animal proteins in your diet. Foods that contain animal proteins include red meat, fish, and dairy products.
Acute or advanced (
end-stage) liver failure may require hospitalization. Treatment may include:
Giving antibiotic medicine.
Giving IV fluids and minerals (electrolytes).
Flushing out toxic substances from the body using medicine or a cleansing procedure (enema).
Adding certain clotting factors to the bloodstream to prevent bleeding (receiving a transfusion).
Using an artificial kidney to filter your blood (hemodialysis) if you have renal failure.
Adding breathing support with a breathing tube.
Having a liver transplant. This is a surgery to replace your liver with another person's liver (donor liver). This may be the best option if your liver has completely stopped working.
Follow these instructions at home:
Eating and drinking
Follow instructions from your health care provider about what you may eat and drink. These may include:
Limiting the amount of animal protein that you eat.
Increasing the amount of plant-based protein that you eat. Foods that contain plant-based protein include whole grains, nuts, and vegetables.
Taking vitamins or supplements.
Limiting the amount of salt that you eat.
Lifestyle

Do not drink alcohol.
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
Exercise regularly as told by your health care provider.
General instructions
Take over-the-counter and prescription medicines only as told by your health care provider.
Follow instructions from your health care provider about maintaining your vaccinations, especially vaccinations against hepatitis A and B.
Keep all follow-up visits. This is important.
-
National Institute of Diabetes and Digestive and Kidney Diseases:
niddk.nih.gov
-
Contact a health care provider if:
-
You have symptoms that get worse.
-
You lose a lot of weight without trying.
-
You have a fever or chills.
-
You cannot take care of yourself or be taken care of at home.
-
You become confused or very sleepy.
-
You are not urinating.
-
You have difficulty breathing.
-
You have bright red blood in your vomit, or your vomit looks like coffee grounds.
These symptoms may be an emergency. Get help right away. Call 911.
Summary
-
Liver failure is a condition in which the liver loses its ability to function due to injury or disease.
-
Treatment for this condition depends on the cause and the severity of symptoms.
-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
Contact a health care provider if you have symptoms that get worse.
-
Keep all follow-up visits. This is important.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.