ThisiscontentfromElsevier'sDrugInformation
Losartan; Hydrochlorothiazide
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
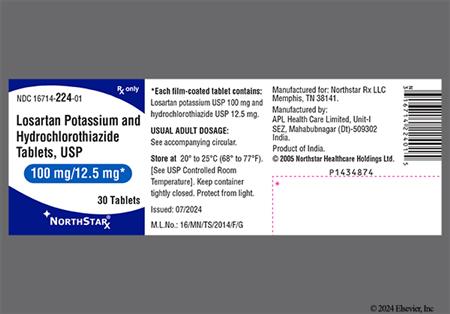
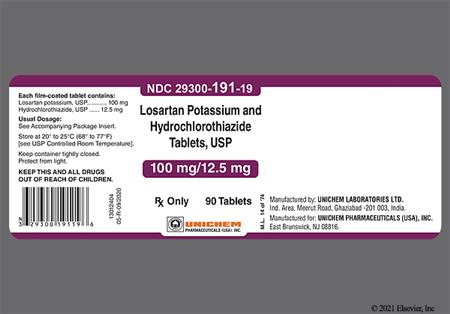
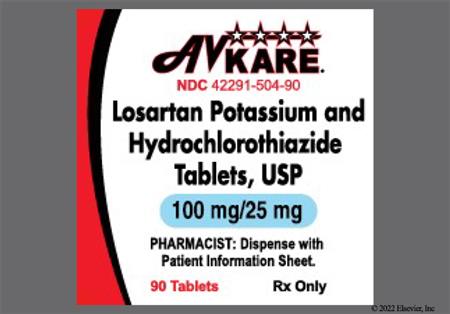
NOTE: Hyzaar is available as losartan 50 mg/hydrochlorothiazide 12.5 mg, losartan 100 mg/hydrochlorothiazide 12.5 mg, losartan 100 mg/hydrochlorothiazide 25 mg dosage strengths, respectively. Individualize dosage by titration of the separate components. If the optimal dose corresponds to the ratio contained in the combination formulation, Hyzaar can be substituted.
Patients whose blood pressure is not adequately controlled with losartan or hydrochlorothiazide (HCTZ) monotherapy may be switched to losartan 50 mg/hydrochlorothiazide 12.5 mg PO once daily. Hyzaar is not intended as first-line therapy, except when the hypertension is severe enough that the value of achieving prompt blood pressure control exceeds the risk of initiating combination therapy. The dosage for Hyzaar is best determined by individual titration with the separate components. Adjust dosage based on clinical response after 3 weeks or more. Dosage may be increased to 2 tablets of losartan 50 mg/hydrochlorothiazide 12.5 mg once daily or 1 tablet of losartan 100 mg/hydrochlorothiazide 25 PO once daily. The maximum dosage is 100 mg/day of losartan combined with 25 mg/day of hydrochlorothiazide. The usual starting dose of losartan monotherapy is 50 mg PO once daily, with 25 mg PO recommended for patients with intravascular volume depletion (e.g., patients treated with diuretics) or a history of hepatic impairment. The addition of a diuretic has a greater effect on lowering blood pressure than increasing the losartan dosage beyond 50 mg/day. The addition of hydrochlorothiazide 12.5 mg to losartan 50 mg once daily results in an additional 50% reduction in DBP and SBP.
See adult dosage. Greater sensitivity in some older individuals is possible. Adjust dosage based on clinical response.
Hyzaar is not intended as first-line therapy, except when the hypertension is severe enough that the value of achieving prompt blood pressure control exceeds the risk of initiating combination therapy. Initiate therapy with losartan 50 mg/hydrochlorothiazide 12.5 mg PO once daily. Adjust dosage based on clinical response after 2 to 4 weeks. Dosage may be increased to 1 tablet of losartan 100 mg/hydrochlorothiazide 25 PO once daily. The maximum dosage is 100 mg/day of losartan combined with 25 mg/day of hydrochlorothiazide.
See adult dosage. Greater sensitivity in some older individuals is possible. Adjust dosage based on clinical response.
NOTE: There is evidence that this benefit does not apply to Black patients.
NOTE: Hyzaar is available as losartan 50 mg/hydrochlorothiazide 12.5 mg, losartan 100 mg/hydrochlorothiazide 12.5 mg, losartan 100 mg/hydrochlorothiazide 25 mg dosage strengths, respectively. Individualize dosage by titration of the separate components. If the optimal dose corresponds to the ratio contained in the combination formulation, Hyzaar can be substituted.
Initially, 50 mg PO losartan once daily. Maximal antihypertensive effects generally occur within 3 to 6 weeks. If needed for blood pressure (BP) reduction, add hydrochlorothiazide (HCTZ) 12.5 mg PO once daily. If additional blood pressure reduction is needed, increase the losartan dose to 100 mg, or losartan 100mg/hydrochlorothiazide 12.5 mg PO once daily may be substituted. The maximum daily dosage is losartan 100 mg and hydrochlorothiazide 25 mg. This FDA-approved indication is based on the findings of the LIFE trial which compared losartan versus atenolol in patients with hypertension and LVH.[26953] In this trial, losartan reduced the risk of stroke (nonfatal and fatal) by 25% compared to atenolol. The overall findings demonstrate that losartan is more effective than atenolol in reducing total mortality and cardiovascular morbidity and mortality, and is associated with less drug-related adverse events.[26953] In a pre-specified subanalysis of the LIFE study in diabetic hypertensives with LVH, similar findings are reported.[26954]
100 mg/day PO losartan and 25 mg/day PO hydrochlorothiazide.
100 mg/day PO losartan and 25 mg/day PO hydrochlorothiazide.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
The fixed combination product, Hyzaar, is not recommended for initial titration in patients with hepatic impairment since the appropriate 25 mg starting dose of losartan cannot be administered. See Losartan monograph for dosing in patients with hepatic impairment. Hydrochlorothiazide should be used with caution in patients with hepatic disease since minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
CrCl more than 30 mL/min: No dosage adjustment is necessary.
CrCl is 30 mL/min or less: Combination therapy with losartan and hydrochlorothiazide is not recommended. Thiazide diuretics are not effective in this setting.
Intermittent hemodialysis
Combination therapy with hydrochlorothiazide is not recommended in patients with CrCl is 30 mL/min or less. Thiazide diuretics are generally not effective in this setting.
† Off-label indication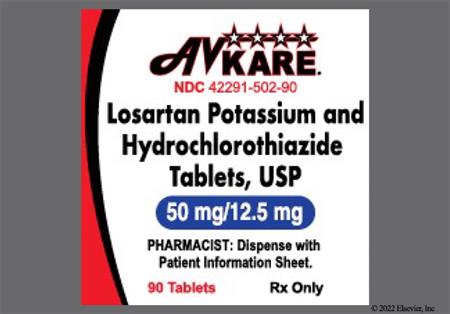
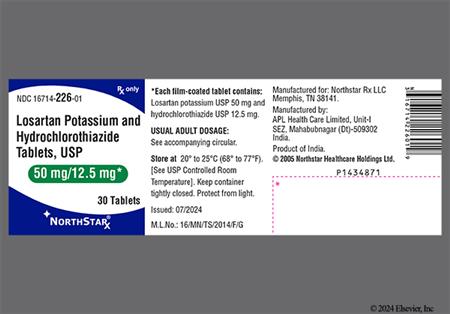

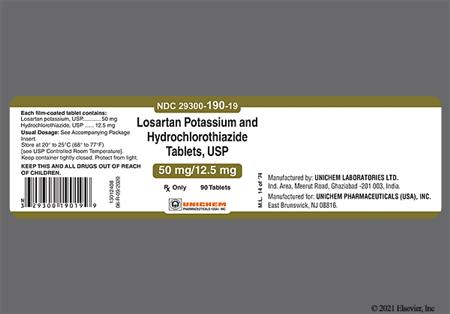
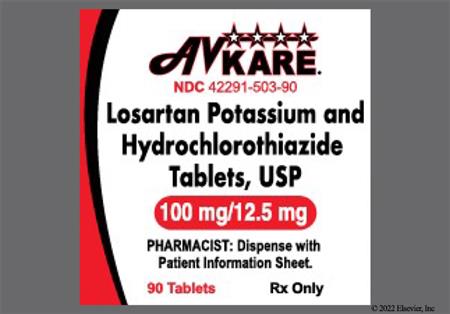






Losartan and hydrochlorothiazide (HCTZ) are used together in a once daily oral preparation to manage hypertension. Hydrochlorothiazide is a thiazide diuretic. Losartan and its metabolite (E-3174) are specific and selective angiotensin II antagonists. Because AT1 receptors are nearly saturated at the starting dose for most angiotensin II antagonists, the antihypertensive dose-response curve of these drugs are nonlinear, with proportionally small decreases in blood pressure attained with increased dosage. Greater antihypertensive efficacy is achieved by adding a small dose of a diuretic to the angiotensin II antagonist. Losartan is associated with dose-related antiproteinuric and uricosuric effects. Losartan tends to reverse the potassium loss and blunts the rise in serum uric acid levels associated with hydrochlorothiazide. Because losartan does not inhibit angiotensin converting enzyme (ACE), it does not result in bradykinin accumulation which is theorized to cause the cough and angioedema associated with ACE inhibitors. However, angioedema has been rarely associated with losartan or other angiotensin II antagonists. Hyzaar (50 mg losartan and 12.5 mg hydrochlorothiazide) was originally approved on April 28, 1995; the subsequent dosage strength (100 mg losartan and 25 mg hydrochlorothiazide) was approved on October 13, 1998.
For storage information, see the specific product information within the How Supplied section.
Cough was reported in 2.6% of losartan; hydrochlorothiazide-treated patients compared to 2.3% of placebo-treated patients in controlled clinical trials. The incidence of cough appears to be lower with losartan than with an angiotensin converting enzyme inhibitor (ACEI); losartan does not inhibit angiotensin converting enzyme (kinase II), which is thought to be responsible for the ACEI-induced cough. In comparative studies, the incidence of cough in losartan-treated patients with a prior history of ACEI-induced cough was similar to that associated with hydrochlorothiazide or placebo therapy. Cases of cough, including positive re-challenges, have been reported with the use of losartan in postmarketing experience.[32333]
Dizziness was reported in 5.7% of losartan; hydrochlorothiazide-treated patients in clinical trials compared to 2.9% of placebo-treated patients. Asthenia/fatigue and headache were also reported in 1% or more of losartan; hydrochlorothiazide-treated patients, but were as or more common in the placebo group. Nervous system/psychiatric events reported in patients treated with losartan monotherapy without regard to causality include: anxiety, ataxia, confusion, depression, dream abnormality, hypoesthesia, insomnia, libido decrease, memory impairment, migraine, nervousness, panic disorder, paresthesias, peripheral neuropathy, sleep disorder, drowsiness, tremor, and vertigo. Restlessness and weakness have been reported during hydrochlorothiazide monotherapy.[32333]
Impotence (erectile dysfunction) has been reported in patients taking losartan monotherapy and is possible in patients taking losartan; hydrochlorothiazide.[32333]
Adverse reactions reported in losartan; hydrochlorothiazide-treated patients in clinical trials and more frequently than placebo include: edema/swelling (1.3% vs. 1.2%) and palpitations (1.4% vs. 0%). Patients treated with diuretics may become intravascularly volume-depleted (hypovolemia), and symptomatic hypotension may occur after initiation of therapy with losartan; hydrochlorothiazide. Chest pain (unspecified), orthostatic effects (e.g., orthostatic hypotension), syncope, angina pectoris, arrhythmia exacerbation (including atrial fibrillation, sinus bradycardia, sinus tachycardia, ventricular tachycardia and ventricular fibrillation), CVA (stroke), myocardial infarction, and second degree AV block have been reported with losartan.[32333]
Angioedema, including swelling of the larynx and glottis, causing airway obstruction and/or swelling of the face, lips, pharynx, tongue, and/or swelling of the intestine has been reported with postmarketing use of losartan; hydrochlorothiazide. Anaphylactic reactions (anaphylactoid reactions) can present as respiratory distress (including pneumonitis and pulmonary edema).[32333] Theoretically, angiotensin II receptor antagonists (ARBs) should be less likely than angiotensin converting enzyme inhibitors (ACEIs) to precipitate angioedema because ARBs do not cause accumulation of kinins. However, angioedema (swelling of lips and eyelids, facial rash) has been reported in individuals receiving ARBs, including in individuals with a prior history of angioedema during ACE inhibitor therapy. Some of these individuals previously experienced angioedema with other drugs including ACEIs.[32325]
Hypersensitivity reactions may occur during therapy with losartan; hydrochlorothiazide. Vasculitis, including Henoch-Schoenlein purpura, has been reported with losartan. Necrotizing angiitis (vasculitis and cutaneous vasculitis) has been reported with hydrochlorothiazide.[32333]
Clinically significant laboratory abnormalities are rarely reported with losartan. Small decreases in hemoglobin (0.14 grams percent) and hematocrit (0.72 volume percent) occurred frequently during losartan; hydrochlorothiazide therapy; no patient discontinued due to anemia. However, anemia has been reported with losartan monotherapy. Elevated hepatic enzymes and elevated bilirubin concentrations (hyperbilirubinemia) have been reported occasionally during antihypertensive therapy with losartan; hydrochlorothiazide; without requiring discontinuation from therapy. Hepatitis is rarely reported with losartan. Thiazide diuretics have been associated with intrahepatic cholestatic jaundice.[32333]
Rash (unspecified) was reported in 1.4% of losartan; hydrochlorothiazide-treated patients compared to 0% of placebo-treated patients in clinical trials. Superficial peeling of the palms with hemolysis has been reported in one patient receiving losartan monotherapy. Erythroderma (exfoliative dermatitis) has been reported during losartan postmarketing experience. Alopecia, dermatitis, dry skin (xerosis), ecchymosis, erythema, flushing, photosensitivity, pruritus, diaphoresis, and urticaria have also been reported in patients treated with losartan. Adverse dermatologic reactions to hydrochlorothiazide and other thiazide diuretics are uncommon but may occur. These reactions include photosensitivity, urticaria, erythema multiforme including Stevens-Johnson syndrome, and exfoliative dermatitis including toxic epidermal necrolysis (TEN).[32333].
Hydrochlorothiazide has been associated with hyperglycemia and glycosuria without regard to causality. Diabetic patients receiving losartan; hydrochlorothiazide may require dosage adjustment of insulin or oral hypoglycemic agents.[32333]
While serious hematological reactions are rare; aplastic anemia, agranulocytosis, leukopenia, hemolytic anemia, and thrombocytopenia have been reported with hydrochlorothiazide therapy. Thrombocytopenia has also been reported during postmarketing experience with losartan; hydrochlorothiazide.[32333]
Hyperuricemia may occur in patients receiving thiazide diuretics. In predisposed individuals, frank gout or nephrolithiasis may be precipitated. Diuretic-induced acute gouty arthritis and nephrolithiasis are extremely rare in patients with no prior history of gout. Losartan in combination with hydrochlorothiazide attenuates the diuretic-induced hyperuricemia. Although gout has been reported in losartan-treated patients, in a single dose study of losartan, there was a small uricosuric effect leading to a mean decrease in serum uric acid of less than 0.4 mg/dL during chronic oral administration. If some manifestation of gout occurs in a patient who requires diuretic therapy for effective treatment of hypertension, allopurinol or a uricosuric agent can be given to prevent recurrent gouty attacks without diminishing the antihypertensive effect of losartan; hydrochlorothiazide.[32333]
Thiazide diuretics have been shown to increase the urinary excretion of magnesium; this may result in hypomagnesemia. Thiazides may also decrease urinary calcium excretion and may cause intermittent and slight elevations of serum calcium in the absence of known disorders of calcium metabolism. The development of marked hypercalcemia may be evidence of hidden hyperparathyroidism. If hypercalcemia occurs, losartan; hydrochlorothiazide should be discontinued before carrying out tests for parathyroid function.[32333]
Although hypercholesterolemia and/or hypertriglyceridemia have been associated with thiazide diuretic therapy, data from long-term studies suggest that diuretic-induced lipid abnormalities are not clinically significant.[24090] After approximately one year of treatment, total serum cholesterol concentrations will subside to baseline or lower, suggesting that diuretic therapy does not increase coronary heart disease risk. Nevertheless, it would be prudent to monitor serum cholesterol and triglyceride concentrations periodically in hypertensive patients receiving losartan; hydrochlorothiazide.[32333]
Abdominal pain was reported in 1.2% of losartan; hydrochlorothiazide-treated patients vs. 0.6% of placebo-treated patients in clinical trials. Diarrhea and nausea were also reported in 1% or more of losartan; hydrochlorothiazide-treated patients, but were as, or more common in the placebo group. Anorexia, constipation, dental pain, xerostomia, dyspepsia, flatulence, gastritis, and vomiting have been reported with losartan. Sialadenitis, cramping, and gastric irritation have been reported with hydrochlorothiazide.[32333]
Back pain was reported in 2.1% of losartan; hydrochlorothiazide-treated patients in clinical trials compared to 0.6% of placebo-treated patients. Muscle spasm has been reported with hydrochlorothiazide. Arm pain, arthralgia, arthritis, fibromyalgia, hip pain, joint swelling, knee pain, leg pain, muscle cramps, myasthenia (muscle weakness), musculoskeletal pain, myalgia, shoulder pain, and stiffness have been reported with losartan. Rare cases of rhabdomyolysis have been reported during postmarketing experience with angiotensin II receptor antagonists.[32333]
Dysgeusia has been reported in patients taking losartan; hydrochlorothiazide therapy.[32333]
Respiratory-related adverse events that occurred more frequently in losartan; hydrochlorothiazide-treated patients in clinical trials than in placebo-treated patients include: sinusitis (1.2% vs. 0.6%) and upper respiratory infection (6.1% vs. 4.6%). Bronchitis and pharyngitis were reported in 1% or more of losartan; hydrochlorothiazide-treated patients but were as, or more, common in the placebo group. Fever, malaise, dyspnea, epistaxis, nasal congestion, pharyngeal discomfort, respiratory congestion, rhinitis, and sinus disorder have been reported with losartan. Fever and respiratory distress including pneumonitis and pulmonary edema have been reported with hydrochlorothiazide.[32333]
Pancreatitis has been reported rarely in patients receiving thiazide diuretics. Clinical manifestations frequently include pain in the abdomen, abdominal distention, nausea, vomiting, and low-grade fever. Pancreatitis can occur within 2 weeks of initiation of therapy or after several months of therapy. If signs and/or symptoms suggestive of pancreatitis develop in a patient receiving losartan; hydrochlorothiazide, drug therapy should be discontinued.[32333]
Due to the potential for teratogenesis, losartan; hydrochlorothiazide should not be used during pregnancy. Drugs that affect the renin-angiotensin system have been associated with fetal and neonatal abnormalities when administered to women during the second or third trimesters of pregnancy. Adverse fetal and neonatal effects have included hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure, oligohydramnios, and death. Oligohydramnios has been associated with craniofacial deformation and hypoplastic lung development. If oliguria or hypotension occurs in a neonate with a history of in utero exposure to losartan; hydrochlorothiazide, blood pressure and renal perfusion support may be required, as well as exchange transfusion or dialysis to reverse hypotension and/or support decreased renal function.[32333]
Losartan; hydrochlorothiazide may result in ophthalmic and otic adverse reactions. Hydrochlorothiazide, a sulfonamide, can cause an idiosyncratic reaction, resulting in transient myopia and acute angle-closure glaucoma. Symptoms include acute onset of decreased visual acuity or ocular pain and typically occur within hours to weeks of drug initiation. Untreated acute angle-closure glaucoma can lead to permanent vision loss. Discontinue hydrochlorothiazide as rapidly as possible and consider prompt medical or surgical treatment if the ocular hypertension remains uncontrolled.[42865] Transient blurred vision and xanthopsia have also been reported during hydrochlorothiazide monotherapy. Blurred vision, ocular irritation (i.e., burning/stinging in the eye), conjunctivitis, visual impairment (i.e., decrease in visual acuity), and tinnitus have been reported with losartan.[32333]
Minor increases in blood urea nitrogen or serum creatinine were observed in 0.6% and 0.8%, respectively, of patients treated with losartan; hydrochlorothiazide for hypertension. Treatment with angiotensin converting enzyme inhibitors has been associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure (unspecified) and/or death in patients whose renal function may depend on the activity of the renin-angiotensin-aldosterone system (e.g., patients with severe congestive heart failure). Similar outcomes have been reported with losartan.[32333] In the ELITE study, renal dysfunction (defined as a persistent increase in serum creatinine of 0.3 mg/dl) occurred in 10.5% of elderly heart failure patients treated with losartan and in 10.5% of patients treated with an ACE inhibitor (captopril).[24866] Nocturia, increased urinary frequency, and urinary tract infection have also been reported with losartan. Renal failure, renal dysfunction, and interstitial nephritis have been reported with hydrochlorothiazide.[32333]
Hypokalemia (serum potassium less than 3.5 mEq/L) has been observed in 6.7% patients; whereas hyperkalemia (serum potassium greater than 5.7 mEq/L) has been observed in 0.4% of patients receiving losartan; hydrochlorothiazide. No patients required discontinuation of therapy from the combination product in controlled clinical trials due to changes in serum potassium. Hyponatremia has also been reported with losartan monotherapy. All patients receiving thiazide therapy should be observed for clinical signs of fluid or electrolyte imbalance: hyponatremia, hypochloremic alkalosis, and hypokalemia. Although any chloride deficit is generally mild and usually does not require specific treatment except under extraordinary circumstances (as in liver disease or renal disease), chloride replacement may be required in the treatment of metabolic alkalosis. Dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction, rather than administration of salt except in rare instances when the hyponatremia is life-threatening. In actual salt depletion, appropriate replacement is the therapy of choice.[32333]
Hydrochlorothiazide has been associated with an increased risk of non-melanoma skin cancer. An FDA Sentinel Initiative study found that increased risk was mostly for squamous cell carcinoma and in White patients taking large cumulative doses. The increased risk for the overall population was approximately 1 additional case per 16,000 patients per year. For White patients taking a cumulative dose more than 50,000 mg, the risk increased to approximately 1 additional case per 6,700 patients per year.[32333]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in individuals with a history of hypersensitivity to it or any of its components. According to the manufacturer of hydrochlorothiazide, it is specifically contraindicated in individuals with sulfonamide hypersensitivity. However, while thiazide diuretics, such as hydrochlorothiazide, are sulfonamide derivatives, sulfonamide cross-sensitivity has rarely been documented. Sulfonamide antibiotics contain the N4-aromatic amine (arylamine) and the N1-aromatic heterocyclic ring which are believed to be involved in the development of IgE-hypersensitivity reactions; thiazide diuretics, such as hydrochlorothiazide, do not contain either. A relationship between sulfonamide hypersensitivity and allergic reactions with non-arylamine sulfonamide derivatives has not been definitively established and remains controversial. It has been theorized that individuals with a documented sulfonamide allergy may have a predisposition for the development of allergic drug reactions.[23511][26922][32380][32381][32382][40304][65846][71386][71387]
Individuals with heart failure or post-myocardial infarction treated with angiotensin II receptor blocker (ARB) therapy commonly experience blood pressure reduction. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued once blood pressure has stabilized.[29130]
Instruct individuals taking losartan; hydrochlorothiazide to avoid excessive sunlight (UV) exposure and undergo regular skin cancer screening. Losartan; hydrochlorothiazide has been associated with an increased risk of non-melanoma skin cancer. An FDA Sentinel Initiative study found that increased risk was mostly for squamous cell carcinoma and in White individuals taking large cumulative doses. The increased risk for the overall population was approximately 1 additional case per 16,000 patients per year. For White individuals taking a cumulative dose more than 50,000 mg, the risk increased to approximately 1 additional case per 6,700 patients per year.[32333][72648]
Avoid use of losartan; hydrochlorothiazide in individuals with a history of ARB induced angioedema. Exercise caution when using losartan; hydrochlorothiazide in individuals with a history of ACE inhibitor induced angioedema. While angiotensin II receptor blockers (ARBs) have been suggested as potential alternatives because they are less likely than angiotensin-converting enzyme (ACE) inhibitors to precipitate angioedema, anaphylactic reactions and angioedema have been reported in individuals receiving ARBs, including in individuals with a prior history of ACE inhibitor induced angioedema. ARBs do not cause bradykinin accumulation, which may account for the reduction in the risk of angioedema. Individuals with a history of angioedema with an ACE inhibitor may be started on an ARB 6 weeks after discontinuation of the ACE inhibitor. Since Black people are at increased risk of angioedema, ARBs may be preferred over ACE inhibitors in this population.[32325] [32326] [32327] [32328] [32329] [32330] [62854] [66451] [72603]
In individuals with an activated renin-angiotensin system, such as individuals with hypovolemia or hyponatremia receiving high doses of diuretics, symptomatic hypotension may occur with losartan. Correct volume of salt depletion prior to losartan; hydrochlorothiazide administration, or initiate treatment under close medical supervision. The antihypertensive effects of thiazides may be enhanced in individuals predisposed for orthostatic hypotension, including the post-sympathectomy patient; therefore, use losartan; hydrochlorothiazide with caution in these individuals.[32333] [41355]
Losartan; hydrochlorothiazide is contraindicated in individuals with anuria and should be used with caution in individuals with renal disease. Drug-induced hypovolemia can precipitate azotemia or acute kidney injury in individuals with renal disease or impairment. Individuals whose renal function may depend on the activity of the renin-angiotensin system (e.g., individuals with renal artery stenosis, chronic renal disease, severe heart failure, or hypovolemia) may be at risk for developing acute renal failure on ARB therapy. Consider withholding or discontinuing therapy in individuals who develop a clinically significant decrease in renal function while receiving losartan; hydrochlorothiazide. Monitor renal function and potassium periodically in individuals receiving therapy.[32333] The safety and effectiveness of losartan has not been established in pediatric populations with a glomerular filtration rate less than 30 mL/minute/1.73 m2.[28608] [72027] Dialysis is also a risk factor for symptomatic hypotension with ARBs.[27991] Losartan; hydrochlorothiazide is not recommended in patients with moderate-to-severe renal impairment or renal failure (i.e., CrCl less than 30 mL/minute). Guidelines recommend use of loop diuretics and not thiazide diuretics for the treatment of hypertension in individuals with moderate-to-severe chronic kidney disease (GFR less than 30 mL/minute/1.73 m2), as thiazide diuretics are generally considered to be ineffective in this setting.[72603] [72667] [72668]
Initiation of losartan; hydrochlorothiazide is not recommended in individuals with hepatic impairment or hepatic failure because the appropriate starting dose of losartan 25 mg is not available. A lower initial losartan dose is recommended in individuals with mild or moderate hepatic impairment or hepatic failure. Plasma concentrations of losartan and its active metabolite are increased in individuals with mild to moderate hepatic impairment compared to healthy volunteers. Losartan has not been studied in individuals with severe hepatic impairment.[28608] [32333] Hydrochlorothiazide-induced fluid shifts and fluctuations in serum electrolyte concentrations may precipitate hepatic coma in susceptible individuals. Low serum potassium concentrations may develop with rapid diuresis, severe hepatic cirrhosis, or after prolonged therapy. Therefore, use losartan; hydrochlorothiazide with caution in individuals with progressive hepatic disease or hepatic failure.[32333] [40304] [65846]
Due to renin-angiotensin system blockade, individuals treated with angiotensin II receptor blockers and undergoing major surgery and anesthesia may experience hypotension, which is very rarely severe, such that it may require the use of intravenous fluids and vasopressors.[27991]
Correct any serum electrolyte imbalance, such as hypochloremia, hypokalemia, hyperkalemia, hypomagnesemia, hyponatremia and hypercalcemia, prior to starting losartan; hydrochlorothiazide therapy. Angiotensin-converting enzyme (ACE) inhibitors can cause hyperkalemia. Risk factors for the development of hyperkalemia, include renal insufficiency, diabetes, and concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salt substitutes. Hydrochlorothiazide therapy is associated with reductions in sodium, chloride, magnesium, and potassium concentrations. Individuals who are vomiting excessively or receiving parenteral fluids may be at a higher risk for electrolyte imbalances. Due to pharmacological actions of the combination of the ARB and diuretic, the net effect of the use of the combination may be to reduce, elevate, or leave potassium levels unchanged in individual patients. Dilutional hyponatremia may occur in individuals with edema exposed to hot weather. Since hydrochlorothiazide-related hypercalcemia may mask hyperparathyroidism, discontinue losartan; hydrochlorothiazide prior to carrying out tests for parathyroid function. Monitor serum electrolyte concentrations and fluid balance periodically during losartan; hydrochlorothiazide therapy.[28608] [32333] [40304] [65846] [72603]
Losartan; hydrochlorothiazide is contraindicated in individuals with diabetes when coadministered with certain medications, specifically aliskiren.[32333] Carefully monitor blood and/or urine glucose concentrations in individuals with diabetes mellitus who are receiving losartan; hydrochlorothiazide. Hyperglycemia, impaired glucose tolerance, and glycosuria can occur during losartan; hydrochlorothiazide therapy; adjust dose of antidiabetic drugs as necessary.[32333] [40304] [71878]
Caution should be used when losartan; hydrochlorothiazide is administered to individuals with a history of gout or hyperuricemia. Thiazide diuretics, such as hydrochlorothiazide, have been reported to reduce the clearance of uric acid and may exacerbate hyperuricemia and precipitate gout. Losartan decreases uric acid and may attenuate hydrochlorothiazide-induced hyperuricemia when coadministered. Guidelines recommend monitoring individuals taking hydrochlorothiazide with a history of acute gout who are not currently taking uric acid lowering therapy.[32333] [40304] [71878] [72603]
Use losartan; hydrochlorothiazide with caution in individuals with a history of systemic lupus erythematosus. Hydrochlorothiazide may exacerbate or activate systemic lupus erythematosus.[32333]
Counsel people who may become pregnant about the reproductive risk and embryo-fetal toxicity associated with medications that affect the renin-angiotensin system (RAS), such as ACE inhibitors and angiotensin II receptor antagonists. Use of RAS inhibitors during the second and third trimesters of pregnancy is associated with reduced fetal renal function and increased risks of fetal and neonatal morbidity and mortality.[32333][63903] [65551] [68837] [68860]
Closely observe neonates and infants exposed to this medication in utero for hypotension, oliguria, and hyperkalemia. If oliguria or hypotension occurs, blood pressure and renal perfusion support may be required, as well as exchange transfusion or dialysis to reverse hypotension and/or support decreased renal function. Rare reports of jaundice, thrombocytopenia, and electrolyte imbalance have also been reported in neonates exposed to thiazide diuretics prenatally.[32333] [41355] [71878]
Use losartan; hydrochlorothiazide with caution in individuals with narrow iridocorneal angles or glaucoma. Sulfonamide or sulfonamide-derivative drug therapies may cause an idiosyncratic reaction resulting in acute closed-angle glaucoma and increased intraocular pressure with or without noticeable acute myopic shift and/or choroidal effusions. Risk factors for developing acute angle-closure glaucoma may include a history of sulfonamide hypersensitivity or penicillin hypersensitivity. If symptoms occur, discontinue losartan; hydrochlorothiazide as soon as possible. Prompt medical or surgical treatments may be necessary if the intraocular pressure remains uncontrolled.[32333] [61206] [72554] [72555]
Use losartan; hydrochlorothiazide with caution in breast-feeding patients. It is not known whether losartan is excreted into human milk.[32333] [70364] [70365] Hydrochlorothiazide is present in human milk in small amounts, with a relative infant dose (RID) of 1.68%. This limited hydrochlorothiazide exposure is not expected to cause adverse effects in the breastfed child. High hydrochlorothiazide dosages (100 mg to 150 mg/day) have been used to suppress lactation; however, lactation suppression has not been reported with doses of 50 mg or less.[70364] [70365] Due to low concentrations in human milk, guidelines consider the ACE inhibitors captopril and enalapril to be compatible with breast-feeding unless high doses are required. Benazepril and quinapril are also excreted in low quantities into human milk and have been suggested as options during breast-feeding.[63903] [65551] [68835] [68836] [68837] [68860]
Greater sensitivity to the usual dosage of losartan; hydrochlorothiazide may occur in some older adults, and care should be taken in initial dose selection for the geriatric adult. Thiazides may worsen dilutional hyponatremia, and an increased risk of falls has been reported for older adult individuals receiving thiazide diuretics.[32527] [32528] [65846] Individuals receiving diuretics should be monitored for clinical signs of acid/base, fluid, or electrolyte imbalances. According to the Beers Criteria, diuretics are considered potentially inappropriate medications (PIMs) in geriatric individuals and should be used with caution due to the potential for causing or exacerbating SIADH or hyponatremia. Sodium levels should be closely monitored when starting or changing dosages of diuretics in older adults.[63923]
Once pregnancy is detected, discontinue losartan; hydrochlorothiazide as soon as possible. Use of medications that affect the renin-angiotensin system (RAS), such as ACE inhibitors and angiotensin II receptor antagonists, are generally not recommended for use during pregnancy. Use of RAS inhibitors during the second and third trimesters of pregnancy is associated with reduced fetal renal function and increased risks of fetal and neonatal morbidity and mortality. Exposure to these agents in pregnancy may result in adverse outcomes including fetal death, hypotension, neonatal skull hypoplasia, craniofacial abnormalities, fetal limb contractures, hypoplastic lung development, anuria, fetal growth restriction, and both reversible and irreversible renal failure. Additionally, cases of oligohydramnios and anhydramnios have been reported. Development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformations.[32333] [63903] [65551] [68837] [68860] Use of RAS inhibitors during the first trimester of pregnancy may increase the risk of fetal harm, such as congenital malformations; however, available data are conflicting.[32294] [46406] [64367] [71327] [71329] Thiazides cross the placenta. Umbilical vein concentrations are similar to those in the pregnant person's plasma. Thiazides accumulate in the amniotic fluid, with concentrations that can be up to 19 times higher than those in the umbilical vein plasma.[35588] Diuretics are generally considered second-line agents for the treatment of hypertension during pregnancy. Theoretically, there is concern about the potential for diuretics to cause intravascular volume depletion, which could cause fetal growth restriction or oligohydramnios. However, this concern has not been supported by the literature. Closely monitor the pregnant person's blood pressure, heart rate, and volume status and adjust their pharmacologic treatment as necessary to avoid hypotension and placental hypoperfusion. Diuretics should be generally avoided in preeclampsia, as plasma volume is reduced.[63903] [68064] [68860] [69901] There have been rare reports of fetal or neonatal jaundice, thrombocytopenia, and electrolyte imbalance associated with thiazide use during pregnancy.[41355] [71878] In rare cases when another antihypertensive agent cannot be used to treat a pregnant patient, serial ultrasound examinations should be performed to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue losartan; hydrochlorothiazide unless it is considered life-saving for the pregnant individual. Oligohydramnios may not appear until after the fetus has sustained irreversible injury.[32333]
The effects of losartan and hydrochlorothiazide on blood pressure are additive. Thiazide diuretics lower the blood pressure by increasing the excretion of sodium; whereas losartan and its principal metabolite lower blood pressure by selectively blocking the AT1 receptor to antagonize the actions of angiotensin II, the primary vasoactive hormone of the renin-angiotensin system. Losartan tends to reverse the hypokalemia caused by the hydrochlorothiazide; this effect is related to the dose of losartan. Due to the dose-related uricosuric effects of losartan, the combination of losartan with hydrochlorothiazide partially attenuates the rise in serum uric acid and the association with hydrochlorothiazide monotherapy.
Losartan; hydrochlorothiazide is administered orally. No pharmacokinetic drug interaction is observed between losartan and hydrochlorothiazide.
Use losartan; hydrochlorothiazide with caution in breast-feeding patients. It is not known whether losartan is excreted into human milk.[32333] [70364] [70365] Hydrochlorothiazide is present in human milk in small amounts, with a relative infant dose (RID) of 1.68%. This limited hydrochlorothiazide exposure is not expected to cause adverse effects in the breastfed child. High hydrochlorothiazide dosages (100 mg to 150 mg/day) have been used to suppress lactation; however, lactation suppression has not been reported with doses of 50 mg or less.[70364] [70365] Due to low concentrations in human milk, guidelines consider the ACE inhibitors captopril and enalapril to be compatible with breast-feeding unless high doses are required. Benazepril and quinapril are also excreted in low quantities into human milk and have been suggested as options during breast-feeding.[63903] [65551] [68835] [68836] [68837] [68860]
Once pregnancy is detected, discontinue losartan; hydrochlorothiazide as soon as possible. Use of medications that affect the renin-angiotensin system (RAS), such as ACE inhibitors and angiotensin II receptor antagonists, are generally not recommended for use during pregnancy. Use of RAS inhibitors during the second and third trimesters of pregnancy is associated with reduced fetal renal function and increased risks of fetal and neonatal morbidity and mortality. Exposure to these agents in pregnancy may result in adverse outcomes including fetal death, hypotension, neonatal skull hypoplasia, craniofacial abnormalities, fetal limb contractures, hypoplastic lung development, anuria, fetal growth restriction, and both reversible and irreversible renal failure. Additionally, cases of oligohydramnios and anhydramnios have been reported. Development of oligohydramnios may be associated with fetal lung hypoplasia and skeletal deformations.[32333] [63903] [65551] [68837] [68860] Use of RAS inhibitors during the first trimester of pregnancy may increase the risk of fetal harm, such as congenital malformations; however, available data are conflicting.[32294] [46406] [64367] [71327] [71329] Thiazides cross the placenta. Umbilical vein concentrations are similar to those in the pregnant person's plasma. Thiazides accumulate in the amniotic fluid, with concentrations that can be up to 19 times higher than those in the umbilical vein plasma.[35588] Diuretics are generally considered second-line agents for the treatment of hypertension during pregnancy. Theoretically, there is concern about the potential for diuretics to cause intravascular volume depletion, which could cause fetal growth restriction or oligohydramnios. However, this concern has not been supported by the literature. Closely monitor the pregnant person's blood pressure, heart rate, and volume status and adjust their pharmacologic treatment as necessary to avoid hypotension and placental hypoperfusion. Diuretics should be generally avoided in preeclampsia, as plasma volume is reduced.[63903] [68064] [68860] [69901] There have been rare reports of fetal or neonatal jaundice, thrombocytopenia, and electrolyte imbalance associated with thiazide use during pregnancy.[41355] [71878] In rare cases when another antihypertensive agent cannot be used to treat a pregnant patient, serial ultrasound examinations should be performed to assess the intra-amniotic environment. If oligohydramnios is observed, discontinue losartan; hydrochlorothiazide unless it is considered life-saving for the pregnant individual. Oligohydramnios may not appear until after the fetus has sustained irreversible injury.[32333]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.