ThisiscontentfromElsevier'sDrugInformation
Measles Virus; Mumps Virus; Rubella Virus; Varicella Virus Vaccine, Live
Learn more about Elsevier’s Drug Information today! Get the reliable drug data and decision support you need to enhance patient safety through timely and accessible information.
0.5 mL IM or subcutaneously for 2 doses. For routine immunization, the recommended schedule is administration of the first MMR dose at age 12 to 15 months and the second dose at age 4 to 6 years. The maximum age for MMRV use is 12 years.[31531] [52359] [53026] MMR and varicella can be administered as separate vaccines or as the combined product (MMRV); risk of febrile seizures is higher if MMRV is administered as the first dose to children younger than 48 months.[52359] [53026] For catch-up immunization, the 2 doses should be administered at least 1 to 3 months apart depending on which products are administered. If both doses are going to be administered as the MMRV combination vaccine, then 3 months should elapse between doses. If 1 of the doses is administered as the separate components (MMR and varicella vaccines), at least 1 month should elapse between administration of the MMR and the MMRV combination vaccine. At least 3 months should elapse between administration of the varicella vaccine and MMRV.[31531] [55005] A third MMR or MMRV dose is recommended in patients who were previously vaccinated with 2 doses of a mumps virus-containing vaccine and are identified by public health authorities as being at increased risk for acquiring mumps because of an outbreak.[62828]
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
0.5 mL/dose IM or subcutaneous.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed. However, consult current immunization schedules for recommended vaccines for use in young dialysis patients; the ACIP states that all routine vaccinations are likely effective in patients with chronic renal disease.[43236]
† Off-label indication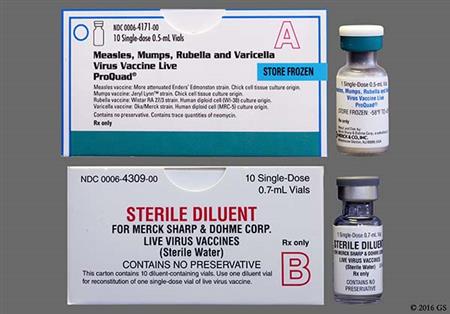
Measles virus; mumps virus; rubella virus; varicella virus (MMRV) vaccine, live is a combination injection consisting of 4 live, attenuated virus vaccinations intended to confer immunity against measles (rubeola), mumps, varicella (chickenpox), and rubella (German measles) viruses. The measles component consists of the Ender's line measles virus obtained from the attenuated Edmonston strain cultured from chick embryos. The mumps component consists of the Jeryl Lynn strain cultured from chick embryos. The rubella component consists of the Wistar Institute RA 27/3 strain of rubella virus propagated in human diploid [WI-38] cells, and the varicella component consists of the Oka/Merck strain of varicella-zoster virus propagated in MRC-5 cells. The antibody responses to each of the antigens in MMRV vaccine were similar compared with the responses after a single dose of the measles virus, mumps virus, rubella virus (MMR) vaccine and varicella virus vaccine given at separate injection sites.[31531] When the MMRV combination vaccine is administered as the first dose to children younger than 48 months, the risk of fever and febrile seizures is higher compared to administration of MMR and varicella vaccines at different injection sites.[55005] MMRV was approved by the FDA in September 2005.
For storage information, see the specific product information within the How Supplied section.
Intramuscular Injection
Subcutaneous Injection
Among 4,497 children 12 to 23 months old who received the frozen formulation of ProQuad (Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine, live), most adverse events occurred in a similar or lower percentage of children as compared with 2,038 children who received MMR and the varicella virus vaccine concomitantly at separate injection sites. A rash at the injection site was more common among recipients of ProQuad (2.3% vs. 1.5%). An injection site reaction with symptoms such as pain/soreness/tenderness (22 to 30.4%), erythema (14.4 to 18%), swelling (8.4 to 9.2%), and ecchymosis (1.5%) was the most common adverse event noted in trials. Extravasation has also been reported during postmarketing use of the drug.[31531]
Among children 12 to 23 months old or 4 to 6 years old who received ProQuad brand of Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine (ProQuad) most adverse events occurred in a similar percentage of children as compared with children who received MMR and varicella virus vaccine concomitantly at separate injection sites. Specifically, irritability was noted in 1 to 6.7% of ProQuad recipients and in 1 to 6.7% of MMR and varicella virus vaccine recipients. Diarrhea was noted in 0.8 to 1.3% of ProQuad recipients and in 1.3% of MMR and varicella virus vaccine recipients. Fewer ProQuad recipients ages 12 to 23 months had irritability (2.4%) or diarrhea (0.6%) after the second dose. Rhinorrhea was noted in 0.5 to 1.1% of ProQuad recipients and in 0.5% of MMR and varicella virus vaccine recipients. Cough was noted in 1.3% of ProQuad recipients and in 0.5% of MMR and varicella virus vaccine recipients. Headache was noted in 0.8% of ProQuad recipients and in 1.6% of MMR and varicella virus vaccine recipients. Vomiting was noted in 0.3 to 1.2% of ProQuad recipients and in 0.5% of MMR and varicella virus vaccine recipients. Drowsiness (somnolence) was also noted in 1.2% of ProQuad recipients, and nausea may be observed. During postmarketing use of ProQuad, cases of agitation, apathy, nervousness, and hypersomnia were reported. Due to the voluntary nature of postmarketing reports, neither a frequency nor a definitive causal relationship can be established.[31531]
Cases of transient thrombocytopenia have been reported within 4 to 6 weeks after vaccination with measles, mumps, and rubella vaccine. Thrombocytopenia, aplastic anemia, epistaxis, lymphadenitis, and regional lymphadenopathy have been reported with the postmarketing use of measles virus; mumps virus; rubella virus; varicella virus vaccine.[31531]
Induction of a subclinical infection with attenuated varicella virus particles is expected after measles virus; mumps virus; rubella virus; varicella virus vaccine, live (MMRV) receipt. The vaccine virus in MMRV may establish latency of varicella-zoster virus in immunocompetent patients, with the potential for later development of herpes zoster. Varicella and herpes zoster infections with the vaccine strain have been noted in vaccine recipients during postmarketing experience. Postmarketing experience suggests that transmission of varicella infection, including disseminated disease, may occur rarely between healthy vaccinees who may or may not develop a varicella-like rash and in both healthy and high-risk contacts. Based on effective donor screening and product manufacturing processes, MMRV vaccine carries an extremely remote risk of transmission of viral infection or disease. A theoretical risk for transmission of Creutzfeldt-Jakob disease also is considered to be extremely remote. Among children 12 to 23 months old who received ProQuad brand of MMRV vaccine, upper respiratory tract infection (1.2% to 1.4%) occurred in a similar percentage of children as compared with children who received MMR and varicella virus vaccine concomitantly at separate injection sites (1% to 1.1%). Naso-pharyngitis was noted in 0.3% of ProQuad recipients and 1% of MMR and varicella virus vaccine recipients 4 to 6 years of age. Infections and symptoms of an infection reported during postmarketing use of the drug include atypical measles, bronchitis, candidiasis, epididymitis, herpes simplex, herpes zoster, influenza, orchitis, parotitis, pneumonia, pneumonitis, pulmonary congestion, rhinitis, sinusitis, sneezing, throat irritation, and skin infections such as cellulitis and impetigo. Due to the voluntary nature of postmarketing reports, neither a frequency nor a definitive causal relationship can be established.[31531]
Among young children 12 to 23 months old who received Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine, live (ProQuad), most adverse events (including varicella-like rash, rash (unspecified), viral exanthema) occurred in a similar percentages of children as compared with children who received MMR and Varivax concomitantly at separate injection sites. Specifically, a varicella-like or vesicular rash was noted in 1.2 to 2.1% of ProQuad recipients and in 2.2% of MMR and varicella virus vaccine recipients. A rash (unspecified) was noted in 1.2 to 1.6% of Proquad recipients and in 1.4% of MMR and varicella virus vaccine recipients. Viral exanthema was noted in 1.2% of ProQuad recipients and in 1.1% of MMR and varicella virus vaccine recipients. A measles-like rash occurred in 3 to 5.1% of ProQuad recipients and in 2.1% of MMR and varicella virus vaccine recipients. Fewer ProQuad recipients had rashes after the second dose: 0.9% had a measles-like or a rubella-like rash, 0.1% had a varicella-like rash, and 0.6% had a rash (unspecified). The measles, mumps, and rubella infection is noncommunicable, but varicella could be transmitted from vaccinated patients to susceptible individuals during the first 6 weeks after vaccination. Vaccine recipients who develop a varicella-like rash should avoid contact with varicella-susceptible persons for at least 6 weeks after vaccination.[31531]
Anaphylactoid reactions, anaphylactic shock, angioneurotic edema (angioedema), facial edema, peripheral edema, acute hemorrhagic edema of infancy, pruritus, bronchospasm, wheezing, erythema multiforme, Henoch-Schonlein purpura, panniculitis, photosensitivity (sunburn), purpura, and Stevens-Johnson syndrome have been noted in Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine, live recipients during postmarketing experience or with vaccine components during clinical trials or postmarketing.[31531]
Encephalitis, measles inclusion body encephalitis, encephalopathy, acute disseminated encephalomyelitis (ADEM), aseptic meningitis, and meningitis have been reported during the postmarketing surveillance period for measles virus; mumps virus; rubella virus; varicella virus (MMRV) vaccine. Although not reported with MMRV vaccination, cases of encephalitis or meningitis caused by vaccine strain varicella virus have been reported in immunocompetent individuals months to years after vaccination with varicella virus vaccine. Reported cases were commonly associated with preceding or concurrent herpes zoster rash. Subacute sclerosing panencephalitis (SSPE) has also been reported in the postmarketing surveillance period. Measles inclusion body encephalitis, pneumonitis, and death as a direct consequence of disseminated measles vaccine virus infection have been reported in immunocompromised patients inadvertently vaccinated with measles-containing vaccine.[31531]
In a clinical trial of 6,038 children 12 to 23 months of age, fever (21.5% vs. 68.3%) was more common after measles virus; mumps virus; rubella virus; varicella virus (MMRV) vaccine administration compared to after the concomitant administration of mumps virus; rubella virus; varicella virus (MMR) and varicella vaccine at separate injection sites. A similar incidence of fever was reported after intramuscular (50% to 62.8%) and subcutaneous (47.2% to 68.3%) administration.[31531] The Advisory Committee on Immunization Practices (ACIP) recommends administration of the MMR vaccine and varicella virus vaccine as separate vaccines for the first dose in children 12 to 47 months of age unless the parent or caregiver expresses a preference for the combination MMRV vaccine. When the MMRV combination vaccine is administered as the first dose to children younger than 48 months, the risk of fever and febrile seizures is higher compared to administration of MMR and varicella vaccines at different injection sites.[52359] [55005] In a postmarketing observational study in 31,298 children who received their first dose of vaccine, febrile seizures were noted 5 to 12 days after vaccination in 0.7 per 1,000 recipients of MMRV vaccine. In an age- and gender-matched historical cohort of children who received concurrent MMR and varicella vaccine, the incidence was 0.32 per 1,000 recipients. In the 0 to 30 day time period after vaccination, the incidence of febrile seizures with MMRV vaccine (1.41 per 1,000) was not statistically greater than that observed in children receiving MMR and varicella vaccine concomitantly (1.28 per 1,000).[31531] An increased risk of febrile seizures with MMRV vaccine in the early period after vaccination was also noted in preliminary results from a CDC observational study. A febrile seizure 7 to 10 days after vaccination with MMRV vaccine was noted in 9 per 10,000 vaccinations, whereas the incidence was 4 per 10,000 vaccinations among recipients of concurrent MMR and varicella vaccine.[52359]
Arthritis, arthralgia, musculoskeletal pain, and myalgia have been identified during postmarketing use of the components of ProQuad or ProQuad. Joint symptoms such as arthralgia, arthritis, and myalgia are associated with the rubella component of the measles virus; mumps virus; rubella virus; varicella virus vaccine live. Joint symptoms are usually transient; only rarely have vaccine recipients developed chronic joint symptoms. Among susceptible persons, arthralgia and transient arthritis occur more frequently among adults than among children and more frequently among postpubertal females than among males. In women, incidence rates for arthritis and arthralgia are generally higher (12 to 26%) than those seen in children (0% to 3%), and the reactions tend to be more marked and of longer duration. Symptoms may persist for a matter of months or on rare occasions for years. In adolescent girls, the reactions appear to be intermediate in incidence between those seen in children and in adult women. Even in women older than 35 years, these reactions are generally well tolerated and rarely interfere with normal activities. When acute joint symptoms do occur, they generally begin 1 to 3 weeks after vaccination, persist for 1 day to 3 weeks, and rarely recur. Tell postpubertal females about the frequent occurrence of generally self-limited arthralgia and/or arthritis beginning 2 to 4 weeks after vaccination.
Acute disseminated encephalomyelitis (ADEM), ataxia, Bell’s palsy, Guillain-Barre syndrome, cerebrovascular accident, dizziness, abnormal dreams, ocular palsies, paresthesias, polyneuritis, polyneuropathy, syncope, transverse myelitis, and tremor have been noted without regard to causality postmarketing with measles virus; mumps virus; rubella virus; varicella virus vaccine live (ProQuad) and/or in clinical studies and/or postmarketing with the component vaccines.[31531] Although cases of Guillain-Barre syndrome (GBS) have been reported after administration of MMR vaccination, a causal relationship has not been established. Recent mass vaccination campaigns that involved approximately 8 million doses of measles-rubella vaccine in the UK and more than 70 million doses of measles vaccine in Latin America demonstrated no increased incidence of GBS over baseline rates. Expert committees at the Institute of Medicine (IOM) have reviewed available evidence concerning the causal relationship between MMR vaccination and various adverse events. Although vasculitis, otitis media, conjunctivitis, ocular palsies, Guillain-Barre syndrome, and ataxia have been reported after administration of MMR or its component vaccines and are listed in the manufacturer's package insert, the IOM has determined that no causal relationship has been established between these events and MMR vaccination.[23937] In addition, evidence does not support a causal association of measles-containing vaccine with risk for Crohn's disease or other inflammatory bowel disease. Cases of aseptic meningitis have been reported to VAERS after measles, mumps, and rubella vaccination. Although a causal relationship between the Urabe strain of mumps vaccine and aseptic meningitis has been shown, there is no evidence to link Jeryl Lynn mumps vaccine to aseptic meningitis.
Cases of otalgia, hearing loss, ocular irritation, eyelid edema (blepharedema), retinitis, necrotizing retinitis (in immunocompromised individuals), optic neuritis, and retrobulbar neuritis have been reported during postmarketing use of measles virus; mumps virus; rubella virus; varicella virus vaccine live (ProQuad). Due to the voluntary nature of postmarketing reports, neither a frequency nor a definitive cause relationship can be established.[31531]
Gastrointestinal adverse events reported during postmarketing use of measles virus; mumps virus; rubella virus; varicella virus vaccine live (ProQuad) include abdominal pain, flatulence, hematochezia, and oral ulceration. Due to the voluntary nature of postmarketing reports, neither a frequency nor a definitive causal relationship can be established.[31531]
The measles, mumps, rubella, and varicella (MMRV) vaccine may result in temporary suppression of tuberculin reactivity causing a laboratory test interference with a tuberculin skin test. Therefore, administer a tuberculin skin test either before, simultaneously with, or at least 4 to 6 weeks after MMRV vaccination to avoid false-negative results.[31531] Additionally, syndromic polymerase chain reaction (PCR) panels may incorrectly identify a measles infection if a patient recently received an MMR vaccine. Approximately 5% of individuals experience a rash after the MMR vaccine; approximately 1% of syndromic panels report a positive measles result after MMR vaccination. Individuals identified with a positive result were pediatric patients without known measles risk who, in most cases, received the vaccine less than 3 weeks beforehand. Inclusion of measles virus in syndromic PCR panels can result in incidental detection of measles vaccines. Health care providers should assess clinical features and vaccine history after a positive test.[70504]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine, live is perseverative-free but contains trace neomycin and other components (e.g., gelatin, albumin). It is contraindicated in individuals with immediate-type hypersensitivity to these components. However, contact dermatitis is not a contraindication. Allergist consultation is advised if vaccination is essential in individuals with a history of anaphylactic reactions to neomycin. Most anaphylaxis cases after measles or mumps containing vaccines are due to components (e.g., gelatin, neomycin) other than egg protein.[31531] Despite measles and mumps vaccines being cultured in chick embryos, MMRV can be safely administered to most egg-allergic patients without prior skin testing, as the risk of serious reactions is extremely low. Vaccination is appropriate unless there is a known life-threatening allergy to a specific vaccine component. Providers should review allergy history and be prepared to treat anaphylaxis.[72641]
Measles virus; mumps virus; rubella virus; varicella virus (MMRV) live vaccine is contraindicated in pediatric patients with moderate or severe febrile illness with fever greater than 101.3 degrees F and in individuals with active, untreated tuberculosis.[31531]
Recommendations and precautions for individuals with immunosuppression are complex, but the measles virus; mumps virus; rubella virus; varicella virus (MMRV) live vaccine is contraindicated in any person with a primary immunodeficiency state (i.e., severe combined immunodeficiency (SCID), IgA deficiency, hypogammaglobulinemia, agammaglobulinemia, or dysgammaglobulinemia) or an acquired immunodeficiency state.[31531] [52359] Measles inclusion body encephalitis, pneumonitis, and death as a direct consequence of disseminated measles vaccine virus infection have been reported in immunocompromised individuals inadvertently vaccinated with measles-containing vaccine; additionally, disseminated mumps, rubella, and varicella virus infection has occurred in immunosuppressed individuals who were inadvertently given a MMRV vaccine. In addition, although there is no confirmed evidence to indicate the rubella virus can be transmitted to susceptible persons in contact with the vaccinated patient, there is a theoretical risk. Excretion of small amounts of the live, attenuated rubella virus from the nose or throat has occurred in the majority of susceptive individuals 7 to 28 days after vaccination. A family history of congenital or hereditary immunodeficiency is also a contraindication for MMRV vaccine unless the immune competence of the potential vaccine recipient is demonstrated.[31531] [43236] Vaccine recipients should avoid close association with susceptible high-risk individuals for 6 weeks. High-risk individuals include immunocompromised individuals, pregnant women without a documented history of chickenpox or laboratory evidence of prior infection, newborn infants of mothers without documented history of chickenpox or laboratory evidence of prior infection, and all newborn infants born younger than 28 weeks gestation regardless of maternal varicella immunity. In circumstances where contact with high-risk individuals is unavoidable, weigh the potential risk of transmission of vaccine virus against the risk of acquiring and transmitting natural varicella virus.[31531] The vaccine should also not be administered to those with cellular immune deficiency or those individuals on immunosuppressive therapy such as high-dose corticosteroid therapy. Vaccination with MMRV vaccine can result in a more extensive vaccine-associated rash or disseminated disease in these individuals. However, corticosteroid therapy usually is not a contraindication to administering live-virus vaccines when administration is short-term (less than 2 weeks); a low-to-moderate dose (less than 2 mg/kg of body weight or 20 mg/day of prednisone or equivalent for persons who weigh more than 10 kg when administered for less than 2 weeks); long-term, alternate-day treatment with short-acting preparations; maintenance physiologic doses (replacement therapy); or when administered topically (skin, eyes), inhaled, or by local injection. Healthcare providers should wait at least 1 month after discontinuation of high-dose corticosteroid therapy given for more than 2 weeks before administering MMRV vaccine.[43236] The vaccine is also contraindicated in individuals with blood dyscrasias or any neoplastic disease that causes bone marrow suppression or affects the lymphatic system such as leukemia or lymphoma, including individuals currently receiving chemotherapy or radiation therapy.[31531] [43236] [52359] Individuals with leukemia, lymphoma, or other malignancies whose disease is in remission and whose chemotherapy or radiation therapy has been terminated for at least 3 months can receive live-virus vaccines.[43236] Persons living with human immunodeficiency virus (HIV) infection or acquired immunodeficiency syndrome (AIDS) should not receive the MMRV vaccine.[43236] [52359] Pediatric persons living with HIV who have met criteria for vaccination (age specific CD4 percentages 15% or more) should receive the single antigen varicella vaccine along with the MMR vaccine, and not the combination MMRV vaccine.[34366] [43236]
Use caution when administering measles virus; mumps virus; rubella virus; varicella virus vaccine, live to people with an individual or family history of febrile seizures. Pediatric patients ages 12 to 23 months who have not been previously vaccinated, nor have a history of the wild-type infections, have a higher risk of fever and febrile seizures at 5 to 12 days after vaccination with measles virus; mumps virus; rubella virus; varicella virus vaccine, live (dose 1), compared to children who are vaccinated concomitantly with the first dose of measles, mumps, and rubella (MMR) vaccine and varicella-zoster virus vaccine.[31531]
Transient thrombocytopenia has been reported within 4 to 6 weeks after vaccination. Consider the potential risk and benefit of vaccination in individuals with thrombocytopenia or in those who experienced thrombocytopenia after vaccination with a previous dose of a measles, mumps, and rubella-containing vaccine.[31531]
The measles virus; mumps virus; rubella virus; varicella virus vaccine (MMRV) is contraindicated during pregnancy due to the potential for serious maternal and fetal adverse outcomes associated with live virus exposure, as evidenced by data from wild-type infections. Wild-type measles infection during pregnancy has been linked to increased rates of spontaneous abortion, stillbirth, preterm delivery, and congenital defects. Wild-type mumps virus infection in the first trimester may raise the risk of spontaneous abortion; although the mumps vaccine can infect the placenta, it has not been shown to cause congenital malformations or fetal disease. Pregnant individuals infected with wild-type rubella virus face higher risks of miscarriage or stillbirth, and first-trimester infection can cause severe congenital defects leading to Congenital Rubella Syndrome (CRS), which includes eye abnormalities, congenital heart defects, hearing loss, microcephaly, and intellectual disabilities. One vaccine-associated CRS case has been reported postmarketing following inadvertent administration of a measles, mumps, and rubella (MMR)-containing vaccine at 5 weeks gestation. Wild-type varicella infection can cause congenital varicella syndrome. Postmarketing surveillance from 1978 to 2018 of 425 pregnancies with inadvertent MMR vaccination reported 16 major birth defects, 4 fetal deaths, and 50 miscarriages, but no CRS cases. A Vaccine in Pregnancy registry (1971 to 1989) monitoring 1,221 individuals inadvertently vaccinated with rubella virus vaccines around conception found no increase in fetal abnormalities or CRS. Vaccination during pregnancy is not recommended; if vaccination is necessary, it should be administered immediately postpartum.[31531] [55942] [65107]
Counsel people who may become pregnant about the reproductive risk associated with measles virus; mumps virus; rubella virus; varicella virus vaccine, live (MMRV). This vaccine is contraindicated during pregnancy due to the potential for serious fetal adverse outcomes associated with live virus exposure, as evidenced by data from wild-type infections. Advise people who may become pregnant to use effective methods to prevent pregnancy for 3 months after vaccination.[31531] [55942] [65107]
The measles virus; mumps virus; rubella virus; varicella virus vaccine, live (MMRV) is considered compatible with breast-feeding. According to the Advisory Committee on Immunization Practices (ACIP), MMRV, live may be used during lactation. This vaccine does not affect the safety of breast-feeding for the individual or the breast-fed child. The rubella vaccine virus may be excreted in human milk; however, the virus usually does not infect the child. If infection does occur, it is well tolerated because the virus is attenuated. The varicella virus vaccine has not been found in human milk. The ability of either the measles or mumps virus vaccine to be secreted in human milk is unknown. In breast-feeding infants with serological evidence of rubella infection, none exhibited severe disease; however, one exhibited mild clinical illness typical of acquired rubella. There are no data to suggest that passive transfer of antibodies in human milk affects the efficacy of live-virus vaccines. Breast-fed children should be vaccinated according to the recommended schedule.[31531] [43236] [55942]
Mechanism of Action: Active immunization with the vaccine stimulates the immune system to produce disease-specific antibodies by inducing a subclinical infection with attenuated virus particles. The measles, mumps, and rubella infection is noncommunicable, but varicella could be transmitted from vaccinated patients to susceptible individuals during the first 6 weeks after vaccination (see Contraindications). Vaccination with Measles virus; Mumps virus; Rubella virus; Varicella virus vaccine, live produces a detectable IgG antibody humoral immune response in a high proportion of individuals. Vaccine-induced antibodies are capable of virus neutralization by opsonization, complement activation, and induction of cell-mediated immunity. At least 96% of over 1500 children had antibodies to each of the 4 antigens 1 year after vaccination, but the duration of protection from measles, mumps, rubella, and varicella infections after receipt of ProQuad® is unknown.
Revision Date: 10/17/2025, 11:40:49 AMThe measles virus; mumps virus; rubella virus; varicella virus vaccine (MMRV), live vaccine is administered intramuscularly or subcutaneously. The distrubution, metabolism, and excretion of the vaccine have not been well defined.[31531]
The refrigerator-stable formulation of ProQuad (n = 1,006) was compared to the frozen formulation of ProQuad (n = 513) in pediatric patients age 12 to 23 months. Both vaccines were administered subcutaneously. A statistical analysis of non-inferiority in antibody response rates and geometric mean titers (GMTs) to measles, mumps, rubella, and varicella at 6 weeks postvaccination showed the immunogenicity of the refrigerator-stable formulation and the frozen formulation of ProQuad were similar. The estimated antibody response rate to measles in the refrigerator-stable formulation was 99.1% and the frozen formulation was 98.5%. The estimated antibody response rate to mumps in the refrigerator-stable formulation was 97.7% and the frozen formulation was 98.0%. The estimated antibody response rate to rubella in the refrigerator formulation was 99.6% and the frozen formulation was 99.6%. The estimated antibody response rate to varacella in the refrigerator formulation was 90.1% and for the frozen formulation was 88.8%.[31531]
Children 15 to 31 months
After a second dose of measles virus; mumps virus; rubella virus; varicella virus (MMRV) vaccine in children 15 to 31 months, 99% of children had measles antibodies, 99% had mumps antibodies, 98% had rubella antibodies, and 99% had varicella antibodies. Of children who received the measles, mumps, and rubella vaccine and the varicella vaccine at least 1 month before MMRV receipt, 99% had seropositivity for each of the 4 antigens.[31531]
Children 12 to 23 months
Similar antibody responses to each of the antigens are obtained after a single dose of MMRV vaccine as compared with a single dose of the measles, mumps, and rubella vaccine and of varicella virus vaccine. After a single MMRV dose, 97% of initially seronegative children 12 to 23 months had measles antibodies, 95% had mumps antibodies, 98% had rubella antibodies, and 91% had varicella antibodies.[31531]
The measles virus; mumps virus; rubella virus; varicella virus vaccine (MMRV) is contraindicated during pregnancy due to the potential for serious maternal and fetal adverse outcomes associated with live virus exposure, as evidenced by data from wild-type infections. Wild-type measles infection during pregnancy has been linked to increased rates of spontaneous abortion, stillbirth, preterm delivery, and congenital defects. Wild-type mumps virus infection in the first trimester may raise the risk of spontaneous abortion; although the mumps vaccine can infect the placenta, it has not been shown to cause congenital malformations or fetal disease. Pregnant individuals infected with wild-type rubella virus face higher risks of miscarriage or stillbirth, and first-trimester infection can cause severe congenital defects leading to Congenital Rubella Syndrome (CRS), which includes eye abnormalities, congenital heart defects, hearing loss, microcephaly, and intellectual disabilities. One vaccine-associated CRS case has been reported postmarketing following inadvertent administration of a measles, mumps, and rubella (MMR)-containing vaccine at 5 weeks gestation. Wild-type varicella infection can cause congenital varicella syndrome. Postmarketing surveillance from 1978 to 2018 of 425 pregnancies with inadvertent MMR vaccination reported 16 major birth defects, 4 fetal deaths, and 50 miscarriages, but no CRS cases. A Vaccine in Pregnancy registry (1971 to 1989) monitoring 1,221 individuals inadvertently vaccinated with rubella virus vaccines around conception found no increase in fetal abnormalities or CRS. Vaccination during pregnancy is not recommended; if vaccination is necessary, it should be administered immediately postpartum.[31531] [55942] [65107]
The measles virus; mumps virus; rubella virus; varicella virus vaccine, live (MMRV) is considered compatible with breast-feeding. According to the Advisory Committee on Immunization Practices (ACIP), MMRV, live may be used during lactation. This vaccine does not affect the safety of breast-feeding for the individual or the breast-fed child. The rubella vaccine virus may be excreted in human milk; however, the virus usually does not infect the child. If infection does occur, it is well tolerated because the virus is attenuated. The varicella virus vaccine has not been found in human milk. The ability of either the measles or mumps virus vaccine to be secreted in human milk is unknown. In breast-feeding infants with serological evidence of rubella infection, none exhibited severe disease; however, one exhibited mild clinical illness typical of acquired rubella. There are no data to suggest that passive transfer of antibodies in human milk affects the efficacy of live-virus vaccines. Breast-fed children should be vaccinated according to the recommended schedule.[31531] [43236] [55942]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.