ThisiscontentfromElsevier'sDrugInformation
Montelukast
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
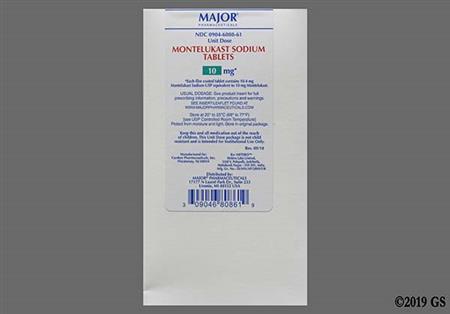
10 mg PO once daily in the evening.[29630]
10 mg PO once daily in the evening.[29630]
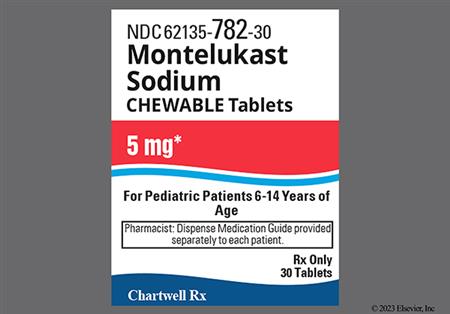
5 mg PO once daily in the evening.[29630]
4 mg PO once daily in the evening.[29630]
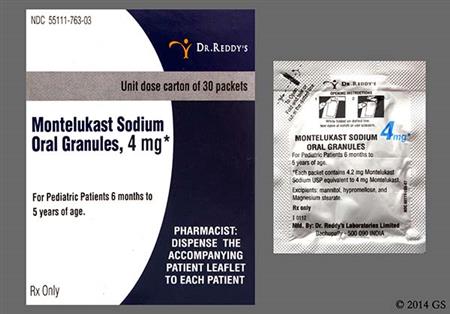
4 mg PO once daily in the evening.[29630]
10 mg PO as a single dose at least 2 hours before exercise. Max: 10 mg/24 hours. Persons receiving daily montelukast for another indication should not take an additional dose to prevent exercise-induced bronchospasm. Rescue medications (e.g., beta-agonists) should be available.[29630]
10 mg PO as a single dose at least 2 hours before exercise. Max: 10 mg/24 hours. Persons receiving daily montelukast for another indication should not take an additional dose to prevent exercise-induced bronchospasm. Rescue medications (e.g., beta-agonists) should be available.[29630]
5 mg PO as a single dose at least 2 hours before exercise. Max: 5 mg/24 hours. Persons receiving daily montelukast for another indication should not take an additional dose to prevent exercise-induced bronchospasm. Rescue medications (e.g., beta-agonists) should be available.[29630]
10 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
10 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
5 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
4 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
4 mg oral granules PO once daily (do not administer tablets).[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
10 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
10 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
5 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
4 mg PO once daily.[29630] LIMITS of USE: Montelukast should not be used for mild symptoms of allergic rhinitis, but should be reserved for patients who are not treated effectively with or cannot tolerate other allergy medication.[29630] [65079]
10 mg PO once daily at bedtime. Use with an established asthma treatment regimen that includes necessary medications such as bronchodilators and inhaled or systemic corticosteroids. The benefit of montelukast in aspirin-intolerant asthmatic patients was assessed in a randomized, double-blind, placebo-controlled trial. Patients were randomized to receive montelukast 10 mg (n = 40) or placebo (n = 40) once daily at bedtime over 4 weeks. Glucocorticosteroids were used in 85% to 90% of patients and theophylline in 40% to 45% of patients at baseline. A 2-week washout period occurred prior to study entry during which no long-acting antihistamines, long-acting beta agonists, or inhaled antimuscarinics were used.At study conclusion, montelukast significantly improved FEV1 and twice daily peak expiratory flow rate (PEFR) rates vs. placebo (p less than 0.001), with mean differences in FEV1 of 10.2%, 28 L/minute (morning PEFR), and 23.1 L/minute (evening PEFR). Less rescue short-acting beta agonist (SABA) was used in treated patients vs. placebo, and the montelukast group had 54% fewer asthma exacerbations. Asthma quality of life improved; patients with nocturnal asthma slept 1.3 nights more per week compared to those treated with placebo. No significant adverse reactions were observed.[55876]
10 mg PO once daily. May be used concomitantly with emollients, antihistamines, or topical corticosteroids. Montelukast efficacy was evaluated in a randomized, double-blind, placebo-controlled crossover trial in 8 adults with mild to moderate atopic dermatitis (AD). Patients in 2 treatment groups were randomized to a regimen of montelukast 10 mg/day for 4 weeks, then placebo daily for 4 weeks after a 2-day washout period, or vice versa. Topical steroids, emollients, and antihistamines were used because of flaring during washout and initial blinded study periods. At study conclusion, a significant decrease in symptom severity was demonstrated by ADASI (atopic dermatitis area and severity index) scores, with scores with montelukast decreasing from approximately 8 to 6, and scores with placebo increasing from approximately 8 to 10 (p = 0.014). Improvements in scaling/dryness, lichenification, induration, erythema, erosions, and excoriation were noted. No patient completely cleared.[55871] In a single-blind study, adult patients with moderate to severe AD were randomized to treatment with montelukast 10 mg/day with placebo tablets 3 times daily or a combination of cetirizine, corticosteroids, and 10 days of clarithromycin. Placebo topical gel or topical emulsions containing urea or ammonium lactate were offered to those treated with montelukast or the combination regimen, respectively. After 6 weeks, the severity of AD, as estimated by the SCORAD (Scoring Atopic Dermatitis) tool, decreased in each treatment group, with mean scores of 25.5 for montelukast (baseline = 46.5) and 23.3 for the combination regimen (baseline = 47.3); the difference between groups was not statistically significant. Patients felt that reduction in pruritus was the most notable symptom improvement (in both treatment groups); montelukast did not improve xerosis. No adverse reactions to treatment were reported.[55872]
10 mg PO once daily in combination with a non-sedating antihistamine is recommended for refractory urticaria if symptoms persist after optimal antihistamine dosing.[55878] [55879] [55880] [72172]
Although specific dosing guidelines are not provided, use of typical age-adjusted doses should be considered (i.e., 4 mg/day for children aged 5 years or younger, 5 mg/day for children 6 to 14 years, and 10 mg/day for adolescents aged 15 years or older).[29630] The addition of a leukotriene receptor antagonist, such as montelukast, to non-sedating antihistamine therapy is recommended if symptoms persist after optimal antihistamine dosing.[55878] [72172]
5 mg PO once daily at bedtime.[55839] [55846]
4 mg PO once daily at bedtime.[55839] [55846]
10 mg/day PO.
10 mg/day PO.
15 years and older: 10 mg/day PO.
13 to 14 years: 5 mg/day PO.
6 to 12 years: 5 mg/day PO.
1 to 5 years: 4 mg/day PO.
6 months and older: 4 mg/day PO.
Less than 6 months: Safety and efficacy have not been established.
No dosage adjustment is recommended for mild to moderate hepatic impairment. Montelukast has not been evaluated in patients with severe hepatic impairment or hepatitis; no dosage guidelines are available for these patients.[29630]
No dosage adjustments are recommended; montelukast is not significantly eliminated via the renal route.[29630]
† Off-label indication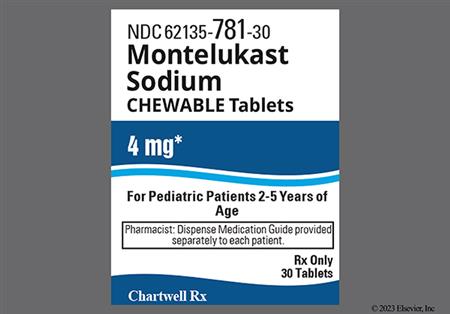




Montelukast is a leukotriene receptor antagonist (LTRA). Unlike zafirlukast, it does not inhibit CYP2C9 or CYP3A4 enzymes and does not interfere with the hepatic clearance of medications metabolized by these enzymes. Montelukast is primarily used for the chronic maintenance treatment of asthma, to prevent exercise-induced bronchoconstriction (EIB), and for the treatment of perennial and seasonal allergic rhinitis.[29630] While generally well tolerated, montelukast has been associated with serious psychiatric effects, including suicidal behaviors, aggression, and depression, reported during postmarketing surveillance.[56750] As a result, the product labeling includes a boxed warning highlighting these potential neuropsychiatric risks.[29630] LTRAs are less effective than inhaled corticosteroids (ICSs) for asthma maintenance therapy and not considered a preferred option for treating persistent asthma. However, LTRAs may be useful for individuals who are unwilling or unable to use ICS, those who experience intolerable ICS side effects, or those with concomitant allergic rhinitis. In adolescents with severe asthma, LTRAs can be used as an add-on therapy, though evidence does not support their added benefit when combined with ICS in children 6 to 11 years of age with more severe asthma. Due to the potential for side effects, montelukast is generally less favored for pediatric asthma treatment.[69016][66299] Montelukast may be considered a first-line add-on therapy to an inhaled short-acting beta-2 agonist (SABA) for preventing EIB symptoms in individuals whose symptoms are not adequately controlled with an inhaled SABA alone.[56291] Among LTRAs, montelukast has the strongest supporting evidence for treating both seasonal and perennial allergic rhinitis.[56376] However, it is not recommended for mild symptoms of allergic rhinitis and should be reserved for patients who do not respond well to, or cannot tolerate, other allergy medication.[29630][65079] Clinical guidelines suggest using montelukast for allergic rhinitis only when alternative therapies are ineffective or not tolerated, due to its lower efficacy compared to other agents and the potential risk of neuropsychiatric side effects. In patients with both allergic rhinitis and asthma, montelukast may be considered if the combined benefits of LTRA monotherapy outweighs the risks, as an alternative for using an inhaled corticosteroid for asthma plus an antihistamine or intranasal corticosteroid for allergic rhinitis.[66102] Montelukast was FDA-approved in February 1998.
For storage information, see the specific product information within the How Supplied section.
Chewable tablets
Film-coated tablets
Oral granules
During initial clinical trials, montelukast was evaluated for safety in over 2600 adolescent (>= 15 years) and adult patients and over 1000 pediatric patients <= 14 years, many of whom received the drug for at least one year. Overall, montelukast was well tolerated. The adverse reaction profile of montelukast is generally similar among pediatric and adult patients. Adverse reactions in adults and adolescents > = 15 years with asthma that were reported more frequently in montelukast-treated patients than in placebo-treated patients included asthenia or fatigue (1.8% vs. 1.2%), fever (1.5% vs. 0.9%), trauma (1% vs. 0.8%), abdominal pain (2.9% vs. 2.5%), dyspepsia (2.1% vs. 1.1%), gastritis (1.5% vs. 0.5%), dental pain (1.7% vs. 1%), dizziness (1.9% vs. 1.4%), headache (18.4% vs. 18.1%), influenza (4.2% vs. 3.9%), nasal congestion (1.6% vs. 1.3%), cough (2.7% vs. 2.4%), pyuria (1% vs. 0.9%), and rash (unspecified) (1.6% vs. 1.2%). Other adverse reactions in adults and adolescents > = 15 years with allergic rhinitis that occurred >= 1% and more frequently than placebo included cough, sinusitis, upper respiratory infection (1.9%), sinus headache, and epistaxis. Adverse reactions reported in one or more pediatric study groups (6 months—14 years) that occurred >= 2% and more frequently than placebo include: abdominal pain, atopic dermatitis, cough, diarrhea, dyspepsia, fever, gastroenteritis, laryngitis, pharyngitis, rhinorrhea, nausea, vomiting, otitis, sinusitis, viral infection, conjunctivitis, dermatitis, rash, ear pain, eczema, pneumonia, urticaria, varicella, acute bronchitis, wheezing, tonsillitis, myopia, rhinitis (infective), skin infection, and tooth infection.[29630]
In rare cases, patients on montelukast therapy presented with systemic eosinophilia, sometimes presenting with clinical features of vasculitis consistent with Churg-Strauss syndrome, a systemic eosinophilic vasculitis which is often treated with systemic corticosteroids. These events usually, but not always, have been associated with the reduction of oral corticosteroid therapy. Symptoms include eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy. Patients may initially complain of generalized, flu-like symptoms such as fever, myalgia, and weight loss. Pulmonary eosinophilia has been reported with post-marketing use. Although a causal relationship with leukotriene receptor antagonism has not been established, caution is advised when oral corticosteroid reduction is being considered in patients receiving montelukast.[29630]
During premarketing clinical trials, the incidence of elevated hepatic enzymes during montelukast treatment was not significantly different from patients taking placebo. ALT increased in 2.1% of montelukast-treated patients and 2% of placebo-treated patients; AST increased in 1.6% and 1.2% of patients, respectively. Increased ALT was also reported in >= 1% of patients in a clinical trial of adults and adolescents >= 15 years with perennial allergic rhinitis. According to the manufacturer, there are reports of eosinophilic infiltration of the liver (hypersensitivity hepatitis), and, in post-marketing experience, cholestatic hepatitis, hepatocellular liver-injury, and mixed-pattern liver-injury. Most of the post-marketing events occurred in patients who had underlying potential for liver disease, such as those with a history of alcohol abuse or other forms of hepatitis.[29630]
In post-marketing experience, the following additional adverse reactions have been reported with montelukast: hypersensitivity reactions, including anaphylaxis (anaphylactoid reactions), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), angioedema, drowsiness, pruritus, erythema nodosum, erythema multiforme, arthralgia, myalgia, muscle cramps, pancreatitis, thrombocytopenia, increased bleeding tendency, bruising (ecchymosis), edema, paresthesias, hypoesthesia, and palpitations.[29630]
Neuropsychiatric events, including changes in mood or behavioral changes, have been reported in adult, adolescent, and pediatric patients taking montelukast. Postmarketing reports include, but are not limited to: agitation, aggressive behavior or hostility, anxiety, depression, disorientation (confusion), attention disturbance, abnormal dreams, dysphemia (stuttering), hallucinations, insomnia, irritability, memory impairment, obsessive-compulsive symptoms (impulse control symptoms), restlessness, somnambulism, suicidal ideation and behavior (including suicide), drowsiness, seizures, tic, and tremor.[29630] Nightmares may be more common in children and typically resolve after drug discontinuation.[56593] In many cases, symptoms resolved after montelukast was discontinued, however, symptoms persisted after discontinuation in some cases. Although neuropsychiatric events were not commonly observed during clinical trials, the clinical details present in some of the postmarketing reports suggest a drug-induced effect, possibly related to the leukotriene pathway. Available data are insufficient to characterize at-risk patients. Advise patients to report changes in behavior and mood; consider alternate therapy if patients develop neuropsychiatric symptoms.[29630] [52011]
Enuresis (night-time urinary incontinence) has been reported in children during post-marketing use of montelukast.[29630]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Montelukast is not effective for the treatment of an acute asthmatic attack, including status asthmaticus or acute bronchospasm. Montelukast is also not recommended to be used as monotherapy for exercise-induced bronchospasm (EIB). Thus, individuals should be advised to have appropriate rescue medication (e.g., inhaled beta-agonist) available. However, montelukast therapy may be continued during the treatment of an acute asthmatic event. Advise individuals not to stop taking or decrease the use of other asthma treatments when starting montelukast unless otherwise directed by their health care prescriber.[29630]
Do not abruptly substitute montelukast for inhaled or oral corticosteroids in asthma therapy. Corticosteroids may be gradually reduced; however, inhaled corticosteroids are the preferred treatment for persistent asthma.[29630][33558]
Advise individuals with known aspirin sensitivity to continue avoidance of aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) while taking montelukast. Montelukast therapy has not been shown to truncate bronchoconstrictor response to aspirin or NSAIDs in aspirin-sensitive asthmatic individuals.[29630]
Published data from prospective and retrospective cohort studies of montelukast use during human pregnancy have not established a drug-associated risk of major birth defects. Some of these studies did have limitations including small sample size, retrospective design, and inconsistent comparator groups. In animal reproduction studies, no adverse developmental effects were observed with montelukast administration to pregnant rats and rabbits during organogenesis at oral doses approximately 100 and 110 times, respectively, the maximum recommended human daily oral dose (MRHDOD) based on AUCs.[29630] The National Asthma Education and Prevention Program, Asthma and Pregnancy Working Group list leukotriene receptor antagonists as an alternative treatment option in the recommended stepwise management of asthma in pregnancy. The Working Group states that leukotriene receptor antagonists may be considered for use during pregnancy for patients who had a favorable response prior to becoming pregnant.[45934]
Montelukast chewable tablets contain phenylalanine; use with caution in patients with phenylketonuria (PKU). Before prescribing montelukast chewable tablets to a patient with PKU, consider the combined daily amount of phenylalanine from all sources, including montelukast.[29630]
Montelukast may be used during breast-feeding when necessary. Montelukast is present in human milk. However, data available for infants exposed to montelukast either directly (for selected indications) or through breast milk do not suggest a significant risk of adverse effects. Montelukast is approved for use in infants 6 months and older and has been used in newborns in dosages that provide concentrations greater than the amounts in breastmilk. The effects of montelukast on human milk production are unknown. Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for montelukast and any potential adverse effects on the breast-fed infant from montelukast or the underlying maternal condition.[29630] The National Asthma Education and Prevention Program, Asthma and Pregnancy Working Group list leukotriene receptor antagonists, such as montelukast, as an alternative treatment option in the recommended stepwise management of asthma in lactating women.[45934]
Behavioral changes consistent with a psychiatric event or neurologic events, including agitation, aggression, depression, sleep disturbances, and suicidal ideation and behavior (including suicide), have been reported in adult, adolescent, and pediatric patients taking montelukast. Some of these psychiatric and neurologic events appear to be consistent with a drug-related effect. The risk of neuropsychiatric events may not outweigh the benefit of treatment with montelukast in some patients, especially those with mild disease or where alternative therapies are available. Only use montelukast to treat allergic rhinitis in individuals who are not treated effectively with or cannot tolerate other allergy medicines. In many cases, symptoms resolved after montelukast was discontinued, however, symptoms persisted after discontinuation in some cases. Available data are insufficient to characterize at-risk patients. Advise patients and their caregivers to report changes in mood or behavior immediately. Discontinue montelukast immediately if neuropsychiatric symptoms occur and continue to monitor and provide supportive care until symptoms resolve. Re-evaluate the benefits and risks of restarting montelukast treatment.[29630]
Use montelukast with caution in individuals with underlying risk factors for hepatic disease, such as ethanol ingestion or hepatitis. Postmarketing reports indicate cholestatic hepatitis, hepatocellular liver injury, or mixed pattern liver injury occur more frequently in these individuals.[29630]
Montelukast is a potent and selective antagonist of leukotriene D4 (LTD4) at the cysteinyl leukotriene receptor, CysLT1, found in the human airway.[29630] The cysteinyl leukotrienes (LTC4, LTD4, and LTE4) are important intermediaries of allergic airway disease. They are products of arachidonic acid metabolism and are released from various cells, including mast cells and eosinophils, in response to allergens. The binding of cysteinyl leukotrienes to CysLT receptors has been associated with asthma pathophysiology, including chemoattraction of eosinophils, stimulation of inflammatory mediators, increased endothelial membrane permeability leading to airway edema, smooth muscle contraction, and enhanced secretion of thick, viscous mucus. In addition, the cysteinyl leukotrienes prepare the immune system for future allergic response through dendritic cell maturation and migration.[29630][42834] In allergic rhinitis, the cysteinyl leukotrienes are released from nasal mucosa in response to allergen exposure during early- and late-phase reactions, producing symptoms of sneezing, nasal itching, and late-stage congestion.[29630] Montelukast improves the signs and symptoms of asthma and allergic rhinitis by inhibiting the physiologic actions of LTD4 at the CysLT1 receptor. Clinically, the drug has been shown to inhibit early- and late-phase bronchoconstriction due to antigen challenge by 75% and 57%, respectively.[29630] Montelukast does not have agonist properties at leukotriene receptors and it does not antagonize smooth muscle contractions due to LTC4, acetylcholine, histamine, prostaglandin, or serotonin.[52024]
Revision Date: 09/15/2025, 03:46:59 PMMontelukast is administered orally. Montelukast is more than 99% bound to plasma proteins. The drug has a small volume of distribution; animal studies indicate minimal distribution across the blood-brain barrier. Montelukast undergoes extensive hepatic metabolism; hepatic isozymes CYP2C8, CYP2C9, and CYP3A4 are involved. At clinically relevant concentrations, CYP2C8 appears to play a significant role in the metabolism of montelukast. Plasma concentrations of metabolites of montelukast are undetectable at steady state. Montelukast and its metabolites are excreted almost exclusively via the bile; less than 0.2% of the drug is excreted in urine. Mean elimination half-life of montelukast is 2.7 to 5.5 hours in healthy young adults. The pharmacokinetic profile of montelukast in age-appropriate doses is similar in children 2 years or older, adolescents, and adults.[29630]
Affected cytochrome P450 isoenzymes and drug transporters: CYP2C8, CYP2C9, and CYP3A4
In vitro studies indicate that the hepatic microsomal isoenzyme CYP2C8 plays a major role in montelukast's metabolism, with CYP2C9 and CYP3A4 also contributing to a lesser degree. However, even potent inhibitors of CYP2C8/9 and/or CYP3A4 do not result in appreciable clinical differences in montelukast pharmacokinetics despite increased exposure, and no dosage adjustments are recommended during coadministration of such inhibitors. Strong inducers also have little effect on the clinical effect of the drug, though the manufacturer recommends monitoring to ensure efficacy. While in vitro studies have shown that montelukast is a rather potent inhibitor of CYP2C8, human in vivo data against sensitive CYP2C8 substrates indicate that inhibition of CYP2C8 substrate metabolism does not occur, and thus interactions with CYP2C8 substrates is unlikely. Other hepatic CYP450 isozymes are not inhibited.[29630] [31034] [32856] [34499] A mild induction of CYP1A2 by montelukast may occur, but is likely only to be relevant for a drug like warfarin; such interactions are not established.[28549]
Absorption of montelukast is rapid after oral administration. All oral forms of montelukast may be taken without regard to meals.[29630]
Chewable tablet
The mean oral bioavailability of the 5 mg chewable tablet is 73% in the fasted state. Maximum plasma concentrations are obtained 2 to 2.5 hours after oral administration. For the 4 mg chewable tablet, the mean maximal concentration is obtained 2 hours after administration in children 2 to 5 years of age in the fasted state. Bioavailability is reduced by approximately 10% when administered with food; however, the clinical efficacy of the chewable tablet is not affected by taking the medication with food. The comparative pharmacokinetics of two 5 mg chewable tablets vs. one 10 mg film-coated tablet have not been evaluated.[29630]
Film-coated tablet
The mean oral bioavailability of the 10 mg film-coated tablet is 64% in the fasted state. Maximum plasma concentrations are obtained 3 to 4 hours after oral administration. A standard meal does not affect the Cmax or oral bioavailability.[29630]
Oral granules
The 4 mg oral granules dosage unit is bioequivalent to the 4 mg chewable tablet when administered in the fasted state. Co-administration with applesauce does not have a clinically significant pharmacokinetic effect. Administration of the oral granules with a high fat meal decreases Cmax by 35% and prolongs Tmax from 2.3 hours to 6.4 hours. However, the clinical efficacy of the oral granules is not affected by taking the medication with food.[29630]
Adults with mild to moderate hepatic insufficiency and clinical evidence of cirrhosis had evidence of decreased metabolism of montelukast resulting in 41% higher mean AUC values following a single 10 mg dose. The elimination of montelukast was slightly prolonged compared with that in healthy subjects (mean half-life, 7.4 hours). No dosage adjustment is required in individuals with mild or moderate hepatic impairment. The pharmacokinetics of montelukast in individuals with more severe hepatic impairment or with hepatitis have not been evaluated.[29630]
Since montelukast and its metabolites are not excreted in the urine, the pharmacokinetics of montelukast were not evaluated in individuals with renal insufficiency. No dosage adjustment is recommended in these patients.[29630]
Adolescents 15 years and older
The plasma concentration profile of montelukast is similar in adolescents 15 years or older and young adults after oral administration of the 10 mg film-coated tablet.[29630]
Children 2 years and older and Adolescents younger than 15 years
The mean systemic exposure of the chewable tablets in children and young adolescents is similar to that of adults receiving film-coated tablets.[29630]
Children younger than 2 years
The systemic exposure to montelukast in children less than 2 years is higher than in adults; however, it is less variable compared to infants. Mean AUC (3,574 nanograms x hour/mL) was 33% higher and mean Cmax (562 nanograms/mL) was 60% higher than those observed in adults (mean AUC: 2,689 nanograms x hour/mL; mean Cmax: 353 nanograms/mL). Safety and tolerability of montelukast in pediatric patients 6 to 23 months of age are similar to that of pediatric patients 2 years or older.[29630]
Infants 6 months and older
The systemic exposure to montelukast and variability of montelukast plasma concentrations are higher in infants than in adults. In infants aged 6 to 11 months, the mean AUC (4,296 nanograms x hour/mL [range: 1,200 to 7,153]) was 60% higher and mean Cmax (667 nanograms/mL [range: 201 to 1,058) was 89% higher than those observed in adults (mean AUC: 2,689 nanograms x hour/mL [range: 1,521 to 4,595]; mean Cmax: 353 nanograms/mL [range: 180 to 548]). Safety and tolerability of montelukast in pediatric patients 6 to 23 months of age are similar to that of pediatric patients 2 years or older.[29630]
Montelukast clearance is only slightly decreased in the elderly compared to younger adults.[29630]
Gender does not affect the pharmacokinetics of montelukast.[29630]
Published data from prospective and retrospective cohort studies of montelukast use during human pregnancy have not established a drug-associated risk of major birth defects. Some of these studies did have limitations including small sample size, retrospective design, and inconsistent comparator groups. In animal reproduction studies, no adverse developmental effects were observed with montelukast administration to pregnant rats and rabbits during organogenesis at oral doses approximately 100 and 110 times, respectively, the maximum recommended human daily oral dose (MRHDOD) based on AUCs.[29630] The National Asthma Education and Prevention Program, Asthma and Pregnancy Working Group list leukotriene receptor antagonists as an alternative treatment option in the recommended stepwise management of asthma in pregnancy. The Working Group states that leukotriene receptor antagonists may be considered for use during pregnancy for patients who had a favorable response prior to becoming pregnant.[45934]
Montelukast may be used during breast-feeding when necessary. Montelukast is present in human milk. However, data available for infants exposed to montelukast either directly (for selected indications) or through breast milk do not suggest a significant risk of adverse effects. Montelukast is approved for use in infants 6 months and older and has been used in newborns in dosages that provide concentrations greater than the amounts in breastmilk. The effects of montelukast on human milk production are unknown. Consider the developmental and health benefits of breast-feeding along with the mother's clinical need for montelukast and any potential adverse effects on the breast-fed infant from montelukast or the underlying maternal condition.[29630] The National Asthma Education and Prevention Program, Asthma and Pregnancy Working Group list leukotriene receptor antagonists, such as montelukast, as an alternative treatment option in the recommended stepwise management of asthma in lactating women.[45934]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.