ThisiscontentfromElsevier'sDrugInformation
Morphine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
General Dosing Information
NOTE: Opioid-tolerant adults are considered as those taking, for 1 week or longer, at least 60 mg/day of morphine, 25 mcg/hour transdermal fentanyl, 30 mg/day of oral oxycodone, 8 mg/day of oral hydromorphone, 25 mg/day oral oxymorphone, 60 mg/day oral hydrocodone, or an equianalgesic dose of another opioid.[40951] [61668]
15 to 30 mg PO every 4 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[46350]
15 to 30 mg PO every 4 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[46350] General weight-based dosing for pediatric patients is 0.15 to 0.3 mg/kg/dose PO every 3 to 6 hours as needed.[23625] [43053] [52200] [52207]
0.15 to 0.3 mg/kg/dose (Max: 5 mg/dose) PO every 3 to 6 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[23625] [43053] [52200] [52207]
10 to 20 mg PO every 4 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[43053]
0.15 to 0.3 mg/kg/dose (Max: 10 to 20 mg/dose) every 3 to 6 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[23625] [43053] [52200] [52207]
0.15 to 0.3 mg/kg/dose (Max: 5 mg/dose) PO every 3 to 6 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[23625] [43053] [52200] [52207]
10 to 20 mg PO every 4 hours as needed, initially. Titrate dose as needed to achieve adequate analgesia.[43053]
2 to 10 mg IV every 4 hours as needed.[31296] [52190]
0.05 to 0.2 mg/kg/dose IV every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia. Usual Max: 8 mg/dose; however, dose must be individualized.[23625] [52190]
0.05 to 0.2 mg/kg/dose IV every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia. Usual Max: 4 mg/dose; however, dose must be individualized.[23625] [52190]
0.05 to 0.2 mg/kg/dose IV every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52190]
0.05 to 0.1 mg/kg/dose IV every 3 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52218]
0.05 to 0.1 mg/kg/dose IV every 3 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52218]
10 mg IM or subcutaneously every 4 hours as needed; dose may range from 5 to 20 mg IM or subcutaneously every 4 hours depending on response.[52190]
0.05 to 0.2 mg/kg/dose (Usual Max: 8 mg/dose) IM or subcutaneously every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52190]
0.05 to 0.2 mg/kg/dose (Usual Max: 4 mg/dose) IM or subcutaneously every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52190]
0.05 to 0.2 mg/kg/dose IM or subcutaneously every 2 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52190]
0.03 to 0.1 mg/kg/dose IM or subcutaneously every 3 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52218]
0.03 to 0.1 mg/kg/dose IM or subcutaneously every 3 to 4 hours as needed; begin at the lower end of dosage range and titrate dose as needed to achieve adequate analgesia.[23625] [52218]
Administer a loading dose by slow IV infusion at a rate of 2 mg/minute. Loading doses of 15 to 20 mg may be required for adequate analgesia; higher doses may be needed in opioid-tolerant patients. Initial infusion rates of 2 to 5 mg/hour have been used, with usual rates of 2 to 30 mg/hour used in critically ill patients.[57161] [57196] Higher infusion rates may be required in opioid-tolerant patients. Titrate dose to pain relief.
A bolus of 0.05 to 0.2 mg/kg IV (or 5 to 10 mg IV for patients weighing more than 60 kg) followed by a continuous infusion. Initial infusion rates of 0.01 to 0.03 mg/kg/hour are common, but initial doses up to 0.06 mg/kg/hour may be appropriate for some patients. Alternatively, rates of 0.8 to 3 mg/hour IV may be used for patients over 60 kg. [44860] [52200] [52221] Higher maintenance infusion rates up to 0.2 mg/kg/hour have been used in patients with sickle cell disease.[25111] Titrate to pain relief.
0.01 to 0.03 mg/kg/hour continuous IV infusion. Adjust dose as needed to achieve target pain assessment score.[52218]
Initial infusion rates of 2 to 5 mg/hour subcutaneously may be used, with usual rates of 2 to 30 mg/hour subcutaneously used in critically ill patients.[57161] [57196] Morphine's dose conversion ratio is 1 mg subcutaneous = 1 mg IV. Higher infusion rates may be required in opioid-tolerant patients. Titrate dose to pain relief. Subcutaneous tissue can absorb up to 3 mL/hour.[57164]
An initial infusion rate of 0.03 mg/kg/hour subcutaneously has been recommended; however, an initial dose of 0.01 mg/kg/hour is also reasonable.[52198] The mean infusion rate was 0.0175 mg/kg/hour over the first 24 hours after surgery in 60 patients (aged 7 months to 20 years) and decreased to 0.011 to 0.0133 mg/kg/hour over the next 48 hours.[52199] Higher infusion rates, ranging from 0.025 to 1.79 mg/kg/hour subcutaneously (median: 0.06 mg/kg/hour subcutaneously), were used in 17 patients (aged 22 months to 22 years) with terminal cancer.[52196] Titrate dose to pain relief.
The starting dose should be based on the patient's recent exposure to opioids. Titrate the regimen to patient response. Larger doses may be needed in opioid-tolerant patients. For OPIOID NAIVE patients, start with a demand dose of 1 mg (range: 0.5 to 2.5 mg) IV and lockout interval of 6 minutes (range: 5 to 10 minutes), with a maximal dosing rate of 10 mg/hour. For OPIOID TOLERANT patients, start with a demand dose of 2 to 5 mg IV and lockout interval of 6 minutes (range: 5 to 10 minutes), with a maximal dosing rate of 30 mg/hour.[33306] [57171]
Various regimens have been reported.[52200] [52207] [52223] [52226] [52227]
The following settings have been used in pediatric patients; titrate regimen to patient response.
Demand dose: 0.01 to 0.025 mg/kg IV (max: 1 mg/dose)
Lockout interval: 5 to 10 minutes
Doses per hour: 5
Basal rate (optional): 0.004 to 0.015 mg/kg/hour IV initially
4-hour limit (optional): 0.24 to 0.375 mg/kg
Initially, inject 5 mg epidurally in the lumbar region and assess the patient in 1 hour; if pain relief is not adequate at that time, administer incremental doses of 1 to 2 mg, with sufficient time between injections to appropriately assess for efficacy. The manufacturer recommends a maximum of 10 mg per 24 hours. For continuous epidural infusion, initiate at 2 to 4 mg per 24 hours, with additional doses of 1 to 2 mg given if pain relief is not initially achieved. The incidence of early and late respiratory depression is dramatically increased with thoracic administration. Use preservative-free formulations only.[48405]
Various regimens have been reported including single preoperative and postoperative doses of 0.03 to 0.1 mg/kg epidurally, postoperative doses of 0.02 to 0.03 mg/kg/dose epidurally every 8 hours, and postoperative continuous infusions of 0.004 to 0.01 mg/kg/hour.[52228] [52229] [52230] Use preservative-free formulations only.
0.2 to 1 mg in the lumbar area as a single dose or to establish dosage for continuous intrathecal infusion; repeated injections are not recommended. Intrathecal doses more than 20 mg/day increase the development of tolerance and serious toxicity including myoclonic spasms. Intrathecal dosage is usually one-tenth the epidural dosage. Use preservative-free formulations only.[48405]
Single preoperative doses of 0.002 to 0.02 mg/kg intrathecally have been reported.[52228] Use preservative free formulations only.
10 to 20 mg rectally every 4 hours, as needed.[48404]
0.2 mg/kg/dose rectally every 4 hours or 0.3 mg/kg/dose rectally every 6 hours as needed have been recommended.[52200] Do not exceed the usual adult dose of 10 to 20 mg/dose.
15 mg PO every 8 to 12 hours, initially. Titrate dose every 1 to 2 days as needed to achieve adequate analgesia. To discontinue, gradually decrease the dose by 25% to 50% every 2 to 4 days to prevent withdrawal.[40951] [60209] [61668]
30 mg PO every 24 hours, initially. Titrate dose every 1 to 4 days as needed to achieve adequate analgesia. To discontinue, gradually decrease the dose by 25% to 50% every 2 to 4 days to prevent withdrawal.[31637] [35890]
Discontinue all other around-the-clock opioids. To convert from other morphine formulations, calculate the morphine 24-hour oral requirement; in general, the 24-hour oral requirement is 3 times the 24-hour parenteral requirement. Initiate dosing, using the 24-hour oral requirement (round down to the closest available tablet/capsule strength), for: Arymo ER, Morphabond, or MS Contin at one-half of the requirement every 12 hours or one-third every 8 hours; Avinza at the total requirement once every 24 hours; and Kadian at one-half every 12 hours or the total once every 24 hours. When initiating extended-release morphine, anticipate and treat breakthrough pain with adequate doses of immediate-release morphine as needed. When converting from other opioids, established conversion ratios to extended-release formulations have not been defined by clinical trials. Initiate dosing for: Arymo ER, Morphabond, or MS Contin at 15 mg PO every 8 or 12 hours; and Avinza or Kadian at 30 mg PO every 24 hours. Alternatively, initiate with one-half of the calculated morphine 24-hour oral requirement estimate, anticipating breakthrough pain and providing adequate doses of immediate-release morphine as needed. When converting from methadone, potency ratios to convert to other opioids can vary widely, warranting extreme caution during conversion to extended-release morphine to avoid overdosage. With the exception of Avinza, adjust dosage every 1 to 2 days based on total daily morphine requirements (extended-release dose plus breakthrough doses). Adjust Avinza dose every 3 to 4 days. Monitor frequently for respiratory depression, especially 24 to 72 hours after initiation or dose escalation. To discontinue, taper the dose by 25% to 50% every 2 to 4 days.[31637] [35890] [40951] [60209] [61668]
Although FDA-approved product labeling provides adult dosing for both opioid-naive and opioid-tolerant patients, it would be prudent to limit pediatric use to opioid-tolerant patients. Limited data are available, and there is wide variability in dosage needs. Doses of 0.2 to 2.3 mg/kg/dose PO every 12 hours have been used in patients with various types of cancer and sickle cell disease.[52206] [52207] [52215] [52217] Begin at the lower end of the dosage range, and titrate to pain relief. Do not exceed recommended adult doses; the initial adult dosage recommendation is 15 mg PO every 8 to 12 hours, with the longer interval used in opioid-naive patients.[40951] Many experts recommend beginning with an immediate-release product to titrate to an appropriate daily dose and then switch to an extended-release formulation and divide the patient's total daily dose into 2 or 3 equal doses.[52207] Monitor patients frequently for respiratory depression, particularly during the first 24 to 72 hours after initiation or dose escalation.[40951] Extended-release morphine should not be used for as needed analgesia and is only appropriate for a select group of children; only clinicians highly experienced in pediatric pain management should prescribe extended-release formulations.
Initially, 0.5 mg PO twice daily with slow, weekly titrations improved quality of life and reduced dyspnea in a small study of 44 patients with COPD.[70790] [70791] In another study of 20 opioid-naive patients with COPD, a single dose of 0.1 mg/kg/dose PO (Max: 10 mg/dose) demonstrated benefit in reducing breathlessness and exercise endurance.[70793] Guidelines support consideration of opioids as one of the palliative modalities to relieve breathlessness in advanced COPD.[69470] [70786] [70801] [70802]
10 to 30 mg/day PO has been reported in some studies to improve COPD assessment test scores without respiratory adverse effects.[70787] [70792] However, one randomized, placebo-controlled study reported that daily low-dose, extended-release morphine (8 or 16 mg/day) did not significantly reduce the intensity of worst breathlessness after 1 week of treatment versus placebo.[70788] Guidelines support consideration of opioids as one of the palliative modalities to relieve breathlessness in advanced COPD.[69470] [70786] [70801] [70802]
2 to 10 mg IV every 3 to 4 hours as needed has been used for opioid naive adults.[70802]
6 mg PO 4 times daily. When using deodorized opium tincture 10 mg/mL, 6 mg = 0.6 mL.[56971] Use caution in geriatric patients due to the potential for adverse CNS effects; and consider alternative drugs for treatment.[56971] [56991]
Deodorized opium tincture 10 mg/mL solution is not recommended for use in pediatric patients.[56971]
2 to 4 mg PO 1 to 4 times daily. NOTE: Dosage is expressed in mg/kg dosing units of morphine. When using opium tincture 2 mg/5 mL concentration (Paregoric, USP), 2 to 4 mg = 5 to 10 mL.[56972] Use caution in geriatric patients due to the potential for adverse CNS effects; consider alternative drugs for treatment.[56972] [56991]
0.1 to 0.2 mg/kg/dose PO 1 to 4 times daily (Maximum: 4 mg/dose). NOTE: Dosage is expressed in mg/kg dosing units of morphine. When using opium tincture 2 mg/5 mL concentration (Paregoric, USP), 0.1 to 0.2 mg/kg = 0.25 to 0.5 mL/kg.[56972]
Although no published studies exist on the effectiveness of nonspecific antimotility agents in treating AIDS-associated diarrhea, opioid agonists may be effective.[57033] Morphine doses of 10 to 30 mg/day PO have been recommended.[24292]
NOTE: Morphine should be administered as an inducing agent only by those trained in anesthesia.
2 mg IV.[32456] Premedication with a benzodiazepine may potentiate the response to morphine; a reduced morphine dose may be needed.
0.1 to 0.2 mg/kg IV has been recommended. Onset of action is typically 2 to 5 minutes.[44771]
0.05 to 0.2 mg/kg IV has been recommended. Use the lower end of the range for opioid-naive neonates. Onset is typically 5 minutes.[44771] [44872] Use a preservative-free formulation.
30 mg PO twice daily initially using extended-release tablets (e.g., MS Contin). Use an initial dosage of 15 mg PO twice daily in those who are not opioid tolerant, and consider this lower dose in geriatric patients or those weighing less than 60 kg.[40951] For Kadian, Avinza, and equivalent generic dose forms that may be given once daily, the highest starting dose for patients who are not opioid tolerant is 30 mg PO every 24 hours. Kadian is administered at a frequency of either once daily or twice daily; Avinza is administered at a frequency of once daily.[35890] Titrate as tolerated to a maximum dosage of 120 mg/day PO.[58583] [58281] In one clinical trial, the maximum dosage in patients less than 60 years of age or weighing less than 60 kg was 60 mg/day PO.[58583] Guidelines classify morphine as probably effective for the treatment of painful diabetic neuropathy.[58281]
0.03 to 0.16 mg/kg/dose PO every 3 to 4 hours, initially. Increase the dose by 0.01 to 0.04 mg/kg/dose every 4 to 8 hours based on clinical response and tolerability. Max: 0.2 mg/kg/dose. When the dose is stable for at least 24 hours, start to taper dose by 10% to 20% every 12 to 48 hours. Discontinue treatment once 10% or 20% of initial maximum dose is reached or dose is 0.01 mg/kg/dose or less, and monitor neonate for at least 24 hours.[51390] [52132] [52689] [62704] [63310] [72302] [72303] [72305]
0.03 to 0.05 mg/kg/dose PO every 3 to 4 hours as needed for withdrawal symptoms. Consider scheduled dosing if 3 or more doses are required within 24 to 48 hours.[72302] [72303] [72304] [72305]
0.5 to 1 mg/kg/hour continuous IV infusion.[64489] [64492]
0.02 to 0.05 mg/kg/hour continuous IV infusion.[64509]
15 mg/day PO once daily, initially. Titrate based on efficacy and adverse effects. Usual dose: 15 to 45 mg/day. Longer-acting and controlled-release drugs are preferred, especially at night.[64831]
0.05 to 0.1 mg/kg/dose IV or IM; may repeat dose as needed until desired response is achieved.[32485] [44772]
4 to 8 mg IV once, then 1 to 8 mg IV every 5 to 30 minutes as needed. Morphine can alleviate pain and work of breathing, decrease anxiety, produce venodilation, and reduce heart rate and systolic blood pressure.[55688] [58787]
3 to 20 mg PO 4 times daily. Start at a low dose and increase the dose every 2 to 5 days if inadequate response and depending on tolerability.[69771] [69772]
Immediate-release formulations, extended-release tablets, extended-release capsules (Kadian ONLY), injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release capsules (Avinza ONLY): 1600 mg/day PO due to the high concentrations of fumaric acid in the formulation.
DepoDur liposome injection: 15 mg/dose epidurally.
Deodorized opium tincture (10 mg/mL concentration ONLY): 6 mg/dose PO and 24 mg/day PO total.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): 4 mg/dose PO and 16 mg/day PO total.
Immediate-release formulations, extended-release tablets, extended-release capsules (Kadian ONLY), injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release capsules (Avinza ONLY): 1600 mg/day PO due to the high concentrations of fumaric acid in the formulation.
DepoDur liposome injection: 15 mg/dose epidurally.
Deodorized opium tincture (10 mg/mL concentration ONLY): 6 mg/dose PO and 24 mg/day PO total.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): 4 mg/dose PO and 16 mg/day PO total.
Immediate-release formulations, extended-release tablets (MS Contin ONLY), injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release capsules, extended-release tablets (Arymo ER or Morphabond), DepoDur liposome injection: Safety and efficacy have not been established.
Deodorized opium tincture (10 mg/mL concentration ONLY): Safety and efficacy have not been established.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): 0.2 mg/kg/dose PO (Max: 4 mg/dose) and 0.8 mg/kg/day PO (Max: 16 mg/day).
Immediate-release formulations, extended-release tablets (MS Contin ONLY), injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release capsules, extended-release tablets (Arymo ER or Morphabond), DepoDur liposome injection: Safety and efficacy have not been established.
Deodorized opium tincture (10 mg/mL concentration ONLY): Safety and efficacy have not been established.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): 0.2 mg/kg/dose PO (Max: 4 mg/dose) and 0.8 mg/kg/day PO (Max: 16 mg/day).
Immediate-release formulations, injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release formulations, DepoDur liposome injection: Safety and efficacy have not been established.
Deodorized opium tincture (10 mg/mL concentration ONLY): Safety and efficacy have not been established.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): Safety and efficacy have not been established.
Immediate-release formulations, injectable solution (NOT DepoDur): With appropriate dosage titration, there is no maximum dose.
Extended-release formulations, DepoDur liposome injection: Safety and efficacy have not been established.
Deodorized opium tincture (10 mg/mL concentration ONLY): Safety and efficacy have not been established.
Camphorated opium tincture (0.4 mg/mL concentration ONLY): Safety and efficacy have not been established.
With the exception of morphine sulfate extended-release liposome injection, which is only used as a single epidural dose, morphine dosage should be modified depending on clinical response and degree of hepatic impairment. Begin treatment with a lower than usual initial dosage, and titrate slowly while monitoring for sedation, respiratory depression, and hypotension.
The 6-glucuronide and 3-glucuronide metabolites are renally eliminated. With the exception of morphine sulfate extended-release liposome injection, which is only used as a single epidural dose, morphine dosage should be modified to prevent accumulation of the metabolite and excessive side effects. Begin treatment with a lower than usual initial dosage, and titrate slowly while monitoring for sedation, respiratory depression, and hypotension.
† Off-label indication













































Morphine is the principal alkaloid obtained from the unripened seed capsules of the opium poppy, Papaver somniferum. It was first isolated in 1803 and is the prototype of the opiate agonists. Today, the poppy is still the source of the drug because synthesis of morphine is difficult. Morphine is a strong analgesic that has been used for the relief of moderate to severe acute and chronic pain, for preoperative sedation, and as a supplement to anesthesia; the drug has also been used for analgesia during labor. Morphine is the drug of choice for pain associated with myocardial infarction and cancer. Many different formulations of morphine are available including both extended-release and immediate-release injectable and oral dosage forms, rectal suppositories, and bulk powder for compounding. Morphine was initially marketed before 1962, which is when Congress passed the amended Federal Food, Drug, and Cosmetic Act requiring that the FDA establish both safety and efficacy for all subsequently approved drugs. Many products were approved under current regulations; however, some manufacturers of morphine have not submitted their products for formal evaluation by the FDA. On March 31st 2009, the FDA issued a Warning Letter to specific manufacturers to halt the production and distribution of the unapproved products. Based on this action, all single ingredient morphine products marketed after July 1, 2009 must be FDA approved. Two formulations of opium tincture, deodorized opium tincture and camphorated opium tincture, contain anhydrous morphine and may be useful for the treatment of non-infectious diarrhea. Opium tinctures have not been found to be safe and effective by the FDA, and they are considered unapproved drugs.[56971][56972][57034] Serious medication errors have resulted from confusion between the products, as the deodorized tincture is 25-times more concentrated than the camphorated tincture.[56973]
For storage information, see the specific product information within the How Supplied section.
NOTE: If Duramorph or Infumorph gets on the skin, remove any contaminated clothing and rinse the affected area with water.
Immediate-release Tablets
Immediate-release Capsules
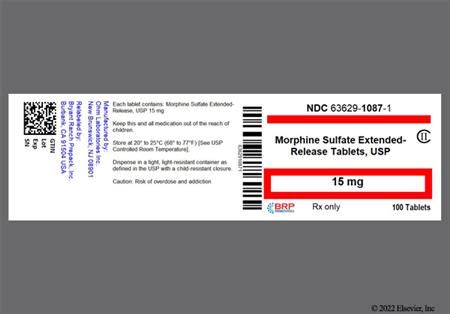
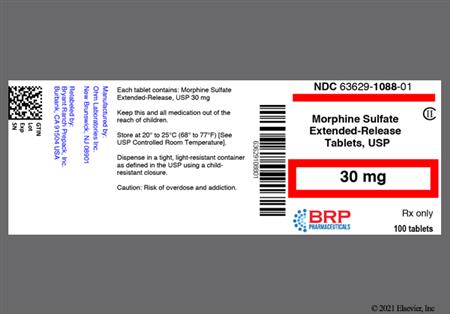
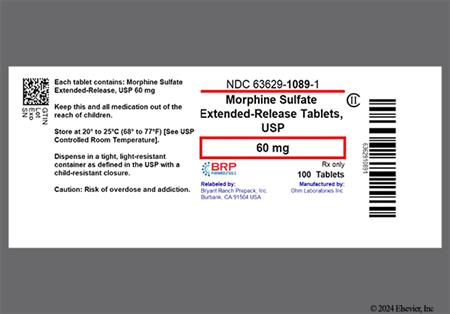
Extended-release Tablets (e.g., Arymo ER, MS Contin, Morphabond)
Extended-release Capsules (e.g., Avinza, Kadian)
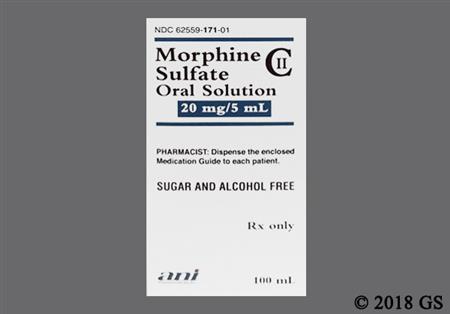
Oral Solution
Opium Tincture (10 mg/mL or 0.4 mg/mL formulations)
Extemporaneous 0.4 mg/mL Morphine Oral Solution Preparation
Intermittent IV Injection
Continuous IV Infusion
Patient-Controlled Analgesia (PCA)
Continuous Subcutaneous Infusion
Intermittent Intrathecal Injection (morphine sulfate solution)
Continuous Intrathecal Infusion (morphine sulfate injection)
Epidural Administration
Intermittent Epidural Injection (morphine sulfate solution)
Continuous Epidural Infusion (morphine sulfate solution)
Pharmacologic tolerance to the analgesic effects of opiate agonists including morphine has been reported in some patients. Tolerance is the need for increasing opioid doses to maintain initial pain relief. Typically, tolerance presents as a decrease in the duration of analgesia and is managed by increasing the opioid dose or frequency. There is no limit to tolerance; thus, some patients may require very large doses of opiate analgesics to control their pain. When increasing doses of analgesia are required causes may be multi-factorial including tolerance, progression of disease, or psychological distress.[43053] [46350]
Although extremely rare, anaphylactoid reactions including cases of anaphylaxis have been reported. Evidence of histamine release such as urticaria, wheals, and local tissue irritation may occur with parenteral morphine administration.[48405] Urticaria (less than 5%) has also been reported with other formulations. Other dermatologic or allergic adverse events that have been reported with morphine include rash (10% or less), decubitus ulcer (less than 3%), xerosis (less than 5%), and edema (less than 5%).[31637] [35890] [40951]
The most significant adverse effects associated with opiate agonist use are respiratory depression (2% to 5%), respiratory arrest, and apnea.[29159] [31296] This results from a decreased sensitivity to carbon dioxide in the brainstem. Respiratory depression is more common in elderly or debilitated patients, after large initial doses in non-opioid tolerant patients or when opioids are given with other agents that cause CNS depression. Respiratory depression is most significant after IV administration.[31296] The sensitivity of the respiratory center returns to normal within 2 to 3 hours. When morphine is appropriately titrated, the risk of respiratory depression is generally small as tolerance rapidly develops to this effect. Bronchospasm has been reported infrequently in patients receiving extended-release morphine tablets; such an event may pose an additive danger in patients with pre-existing elevations in airway resistance.[40951] Other respiratory adverse events include decreased oxygen saturation (more than 10%), hypoxia (5% to 10%), hypercapnia (2% to 5%), dyspnea (2% to 10%), hiccups (less than 5%), hypoventilation (less than 5%), voice alteration (less than 5%), depressed cough reflex (less than 3%), rhinitis (less than 3%), atelectasis (less than 3%), asthma (less than 3%), and non-cardiogenic pulmonary edema (less than 3%).[29159] [31637] [43053] [35890] Symptomatic respiratory depression should be treated cautiously with an opioid antagonist such as naloxone. Patients may also develop respiratory depression through sub-acute overdose of an opiate agonist in which sedation builds up slowly leading to a decreased respiratory rate and then respiratory failure. The risk of this is more common with methadone but may be seen with other long-acting opioid preparations or in patients with renal or hepatic impairment. This can be managed by holding 1 to 2 doses of the opioid and then restarting the opioid at 25% of the previous dose and slowly increasing the dose once the symptoms have resolved. Rarely, patients receiving epidural or intrathecal morphine may develop dose-dependent delayed respiratory depression due to migration of morphine to the medullary respiration center. PaCO2 values in the high 40s to low 50s may be seen in fully awake and alert patients. The incidence of respiratory depression is higher after intrathecal versus epidural administration. The delayed respiratory depression follows the onset of analgesia in higher dermatomes and the onset of gastrointestinal events. Delayed respiratory depression may be seen up to 24 hours after a single epidural dose of morphine. Most cases of respiratory depression during spinal administration of morphine occur in patients receiving concomitant parenteral opioids or sedatives. If naloxone is used to reverse respiratory depression from morphine, repeat doses may be needed.[29159]
Morphine may cause a variety of effects on the GI system, most commonly nausea (7% to 10%), vomiting (less than 3% to more than 10% depending on the patient population and formulation), and constipation (9% or more).[29159] [31637] [35890] Nausea (17%), vomiting (10%), constipation (6%), and flatulence (5%) were among the most common adverse reactions reported on initiation of morphine in pediatric patients.[43053] Nausea and vomiting is most commonly seen at the initiation of therapy or when switching agents. Opioids affect the vestibular system and may cause more nausea/vomiting in ambulatory patients than bedridden patients. Scheduled treatment with an antiemetic during the first 1 to 2 days, then as needed during opiate therapy will usually control these symptoms until tolerance develops. If nausea/vomiting is associated with continuous infusion morphine, receipt of 0.2 mg naloxone intravenously may be helpful.[31296] If patients have nausea associated with movement, an anti-vertigo agent such as meclizine may be appropriate. Metoclopramide may be helpful in treating the symptoms of early satiety or fullness, but chronic use of metoclopramide should be avoided due to risks of adverse events. Constipation due to decrease GI motility and secretions is common during opioid therapy. In some cases patients can develop ileus or GI obstruction. Tolerance rarely develops to this effect; therefore, patients require a bowel regimen consisting of a stool softener and mild stimulant throughout opioid therapy. If the patient does not have a bowel movement for 3 days, an enema or suppository should be administered to prevent impaction. Other GI adverse events reported with morphine include anorexia (10% or less), dysphagia (less than 5%), dyspepsia (5% or less), diarrhea (10% or less), abdominal pain (10% or less), stomach atony disorder (less than 3%), gastroesophageal reflux (less than 3%), delayed gastric emptying (less than 3%), flatulence (5% to 10%), abdominal distention (2% to 5%), gastroenteritis (less than 5%), abnormal liver function tests (less than 5%), rectal disorder (less than 5%), thirst (less than 5%), dysgeusia (less than 5%), weight loss (less than 5%), laryngospasm, and abdominal cramps.[29159] [31637] [35890]
General adverse events reported with morphine use include asthenia (10% or less), accidental injury (10% or less), fever (less than 3% to more than 10%), interference with thermal regulation, pain (less than 3%), chest pain (unspecified) (less than 3%), chills (less than 3%), flu syndrome (10% or less), rigors (2% to 5%), and peripheral edema (10% or less).[29159] [31637] [35890] [48405]
Morphine is a controlled substance with a high potential for abuse and psychological dependence. Abuse and addiction are separate and distinct from physiological dependence and tolerance, which can develop during chronic opioid therapy. Tolerance is characterized by a reduced response to a drug after repeated administration. Physiological dependence develops as a result of repeated drug use. It manifests with a withdrawal syndrome after abrupt discontinuation or significant dose reduction, or administration of an agent with opioid antagonist activity (e.g., naloxone). Withdrawal is characterized by restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms include irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal. Neonatal opioid withdrawal syndrome may be life-threatening and requires management according to protocols developed by neonatology experts. It presents as irritability, hyperactivity and abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, and failure to gain weight.[43053]
Morphine's effect on opioid receptors in the reticular activating system and striatum produces sedation. Patients should be warned that activity requiring mental alertness can be affected since CNS depression, including drowsiness (2% to 19%), confusion (less than 10%), and dizziness (more than 5%) can occur.[29159] [31637] [35890] [40951] Other CNS-related adverse events reported with morphine include headache (4% or more), nervousness (less than 5%), sleep disturbances, dysphoria, euphoria (less than 5%), lightheadedness, alterations of mood (feelings of floating, disorientation, apprehension), anxiety (2% to 6%), restlessness, tremor (less than 5%), malaise (less than 3%), thinking disturbances/abnormal thinking (less than 5%), sedation, abnormal dreams (less than 3%), lethargy (1% to less than 10%), depression (10% or less), loss of concentration (less than 3%), insomnia (10% or less), amnesia (less than 5%), agitation (less than 5%), foot drop (less than 5%), ataxia (less than 5%), hypesthesia/hypoesthesia (less than 5%), slurred speech (less than 3%), apathy (less than 3%), obtunded feeling, non-arousable condition, unresponsiveness, abnormal gait (less than 5%), coma (less than 5%), delirium (less than 5%,) disorientation, weakness, uncoordinated muscle movements, increased intracranial pressure, and vertigo (less than 3%).[29159] [31637] [35890] [40951] [48403] High doses of morphine given intravenously are excitatory due to an increase in circulating catecholamine concentrations. Hallucinations (less than 3%) and seizures (less than 5%) have been reported in patients receiving opioid agonists. Depending upon the individual patient tolerance, hallucinations may be reported in patients undergoing rapid dose escalation.[29159] [31637] [35890] [40951] Dysphoric reactions or toxic psychosis can occur after any dose.[31296] Flushing may also be reported in patients initiating morphine therapy.[29159] [31637] [35890] [40951]
Opioids can cause spasm of the sphincter of Oddi, with morphine producing greater effects than meperidine and meperidine producing greater effects than codeine. Hyperamylasemia, secondary to drug-induced spasm of the sphincter of Oddi, has been associated with various opiate agonists. While serum amylase and lipase concentrations can rise as a result of biliary obstruction or spasm, overt pancreatitis is rare with opiate analgesics. Gastritis and hepatotoxicity are also relatively rare with these agents. Biliary colic (less than 3%), biliary pain (less than 5%), and biliary tract spasm have been reported with the use of morphine.[31637] [35890] [48403]
Morphine and related compounds can cause cardiovascular adverse reactions. These reactions include sinus bradycardia (5% or less), sinus tachycardia (10% or less), atrial fibrillation (less than 3%), pallor (less than 3%), facial flushing (less than 3%), peripheral vasodilation (less than 5%), palpitations (less than 5%), hypertension (5% or less), hypotension (less than 3% to more than 10% depending on the patient population and formulation), orthostatic hypotension, diaphoresis (less than 3%)/sweating (2% to 10%), faintness, presyncope, and syncope (less than 5%). In cases of severe respiratory and/or circulatory depression, shock and cardiac arrest may occur.[29159] [31637] [35890] [40951] [60209] Morphine may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients as a result of peripheral vasodilation. Patients at increased risk for hypotensive effects include those whose ability to maintain blood pressure is already compromised by reduced blood volume or concurrent administration of certain medications (e.g., phenothiazines, general anesthetics).[31637] Monitor patients carefully.
Morphine and other opiate agonists are known to cause pruritus (less than 3% to more than 10% depending on the formulation).[29159] [35890] A high incidence of pruritus is associated with a single dose of either epidurally or intrathecally administered morphine. The pruritus is dose-related and is not confined to the administration site. Occasionally, pruritus is also associated with continuous administration of epidural or intrathecal morphine; the cause is poorly understood.[48405] Pruritus tends to be a less frequent adverse effect of oral morphine products.[24326] If pruritus is associated with continuous administration of morphine, receipt of 0.2 mg naloxone intravenously may lessen the adverse reaction.[31296] Alternatively, use of H1-blockers or changing to a different opioid may lessen the pruritus.
Some patients may experience anticholinergic side effects with morphine therapy. Patients can experience xerostomia (10% or less), blurred vision (less than 3%), or urinary retention (less than 5%) and urinary hesitancy (less than 3%), which can cause oliguria (2% to 5%).[29159] [31637] [35890] Morphine may induce the release of antidiuretic hormone to produce an antidiuretic effect.[60209] After epidural or intrathecal administration of morphine, the incidence of urinary retention is 40% to 100%. Urinary retention may last for 10 to 20 hours after a single epidural or intrathecal dose and for several days after initiation of a continuous infusion. While this may not be a problem for some post-operative patients who have an indwelling urinary catheter, ambulatory and chronic pain patients may have significant problems. Cholinomimetic medication may be advisable. If urinary retention is associated with continuous infusion morphine, receipt of 0.2 mg naloxone intravenously may be helpful.[31296] Other urinary adverse events associated with morphine use include urinary abnormality (less than 3%), bladder spasm (2% to 5%), and dysuria (less than 5%).[29159] [31637] [35890]
Morphine and its congeners can cause miosis at typical therapeutic doses; miosis may even occur in total darkness.[35890] Severe overdose can cause mydriasis once brain anoxia develops. Therapeutic doses can increase accommodation and sensitivity to light reflex and decrease intraocular tension in both normal and glaucomatous eyes. Other ocular adverse events reported with morphine use include amblyopia (less than 3%), conjunctivitis (less than 3%), diplopia (less than 3%), ocular pain (less than 5%), nystagmus (less than 3%), and visual disturbances.[31637] [35890] [48404]
Opioid agonists can exert adverse effects on the endocrine system by inhibiting the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH), and by stimulating secretion of prolactin, growth hormone (GH), insulin, and glucagon. Chronic opioid use may influence the hypothalamic-pituitary-gonadal axis, leading to hormonal changes that may manifest as hypogonadism. A decrease in production of LH and a corresponding decrease in testosterone may result in libido decrease (less than 3%). Women may experience amenorrhea (less than 3%) and infertility, and men may experience abnormal ejaculation (less than 5%) or impotence (erectile dysfunction) (less than 5%). Women may also experience prolonged labor (less than 3%). Hypogonadism (gonadal suppression) and gynecomastia (less than 3%) have also occurred. Other various medical, physical, lifestyle, and psychological stressors may influence gonadal hormone concentrations; these stressors have not been adequately controlled for in clinical studies with opioids. Patients presenting with signs or symptoms of androgen deficiency should undergo laboratory evaluation. Morphine can inhibit the release of thyrotropin, leading to a decrease in thyroid hormone. Morphine and related compounds can stimulate the release of vasopressin (ADH). Hyponatremia (less than 3%) can occur as a result of SIADH.[31637] [35890] [43053] [60660]
Opioids may interfere with the endocrine system by inhibiting the secretion of adrenocorticotropic hormone (ACTH) and cortisol.[35890] Rarely, adrenocortical insufficiency has been reported in association with opioid use. Patients should seek immediate medical attention if they experience symptoms such as nausea, vomiting, loss of appetite, fatigue, weakness, dizziness, or hypotension. If adrenocortical insufficiency is suspected, confirm with diagnostic testing as soon as possible. If diagnosed, the patient should be treated with physiologic replacement doses of corticosteroids, and if appropriate, weaned off of opioid therapy. If the opioid can be discontinued, a follow-up assessment of adrenal function should be performed to determine if corticosteroid treatment can be discontinued. Other opioids may be tried; some cases reported use of a different opioid with no recurrence of adrenocortical insufficiency. It is unclear which, if any, opioids are more likely to cause adrenocortical insufficiency.[60660]
Unusual acceleration of neuraxial morphine requirements can occur in some persons, which may cause concern regarding systemic absorption and the hazards of large doses; these persons may benefit from hospitalization and detoxification. High doses of neuraxial morphine may produce myoclonia events. Myoclonic-like spasm of the lower extremities has been reported in 2 subjects receiving more than 20 mg/day of intrathecal morphine. After detoxification, it might be possible to resume treatment at lower doses, and some persons have been successfully changed from continuous epidural morphine to continuous intrathecal morphine. Repeat detoxification may be indicated at a later date. The upper daily dosage limit during continuing treatment must be individualized.[51758]
Paresthesias (10% or less) have been reported with the use of morphine.[31637] [35890] Non-infectious inflammatory masses, such as granulomas have surrounded catheter tips in patients that received continuous infusions of opioid analgesics by an intrathecal indwelling catheter.[29942] Symptoms that have led to the discovery of an intraspinal mass include loss of analgesic drug effects, spinal cord or cauda equina compression, or a sudden neurologic deficit, such as paresthesias. Serious neurologic impairment, including paralysis, complete paraplegia or paresis has occurred. At least 92 cases of catheter-tip masses have been reported with a mean duration of therapy of 29 months (range, 0.5 to 120). Half of the patients received morphine and another 11 received morphine mixed with other drugs. Of 33 cases that had morphine concentration data available, 28 received a concentration of at least 25 mg/mL. Although the etiology of the masses has not been determined, catheter placement and opioid usage, including drug concentration are possible causes. Placement of the catheter below the conus medullaris may be ideal. The conus medullaris is the lower region of the spinal cord, and the spinal cord usually does not extend beyond the lower margin of the L-2 vertebral body. Thus, injury to the spinal cord from a mass would be prevented by placement of the catheter tip below the conus medullaris. Avoidance of catheter placement in the thoracic region may be desirable, as this region has the narrowest relative space and slow cerebral spinal fluid flow. Some patients with masses that did not fill the spinal canal or cause neurological impairment were treated by stopping or emptying the drug infusion pump or by refilling the pump with preservative-free normal saline. The action either caused mass stabilization or mass regression over several months. In contrast, despite prompt surgical intervention, permanent neurological impairment occurred in some patients with impending paraplegia from a mass that filled the spinal canal.[29942] Patients who receive continual morphine sulfate with or without preservatives by an indwelling intrathecal catheter need to be monitored for new neurologic signs and symptoms.
Musculoskeletal adverse events reported with the use of morphine include back pain (10% or less), bone pain (less than 3%), arthralgia (less than 3%), skeletal muscle rigidity (less than 5%), and decreased bone mineral density.[29159] [31637] [35890] [43053]
Hematologic adverse events that have been reported with morphine therapy include anemia (less than 5%), leukopenia (less than 3%), thrombocytopenia (less than 5%), and decreased hematocrit (2% to 5%).[29159] [31637] [35890]
Infection (unspecified) and urinary tract infection were reported in 5% to 10% of patients during morphine therapy; causality to the drug is unknown.[31637]
Serotonin syndrome has been reported in patients taking opioids at recommended doses. Patients taking opioids concomitantly with a serotonergic medication should seek immediate medical attention if they develop symptoms such as agitation, hallucinations, tachycardia, fever, excessive sweating, shivering or shaking, muscle twitching or stiffness, trouble with coordination, nausea, vomiting, or diarrhea. Symptoms generally present within hours to days of taking an opioid with another serotonergic agent, but may also occur later, particularly after a dosage increase. If serotonin syndrome is suspected, either the opioid and/or the other agent should be discontinued.[60660]
Cases of opioid-induced hyperalgesia (OIH) have been reported, both with short-term and longer-term use of opioids. OIH occurs when an opioid paradoxically causes an increase in pain or an increase in sensitivity to pain. Symptoms of OIH include increased levels of pain upon opioid dosage increase, decreased levels of pain upon opioid dosage decrease, or pain from ordinarily non-painful stimuli (allodynia). These symptoms may suggest OIH only if there is no evidence of underlying disease progression, opioid tolerance, opioid withdrawal, or addictive behavior. Data suggests a strong biologic plausibility between opioids and OIH and allodynia. If OIH is suspected, carefully consider appropriately decreasing the dose of the current opioid analgesic or opioid rotation (safely switching to a different opioid).[68838]
Hypoglycemia has been reported during opioid therapy. Most reports occurred in persons with at least 1 predisposing risk factor, such as diabetes.[40951] [46350]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Morphine is contraindicated in persons with known morphine hypersensitivity. Anaphylaxis has been reported in persons receiving morphine.[40951]
Morphine is contraindicated for use in patients with significant respiratory depression in unmonitored settings or in the absence of resuscitative equipment. Patients with significant respiratory depression in unmonitored settings should generally not receive injectable solution products due to the risk of fatal respiratory depression.[31637] [52190] Additionally, avoid coadministration with other CNS depressants when possible, as this significantly increases the risk for profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; if concurrent use is necessary, use the lowest effective doses and minimum treatment durations needed to achieve the desired clinical effect. Monitor patients closely for signs or symptoms of respiratory depression or sedation.[61143] [61668] All formulations of morphine, with the exception of opium tincture oral solutions, are contraindicated in acute or severe bronchial asthma (i.e., status asthmaticus) in unmonitored settings or in the absence of resuscitative equipment. Receipt of moderate doses in these patients may significantly decrease pulmonary ventilation. Although opium tincture solutions are not specifically contraindicated in patients with pre-existing respiratory depression or hypoxia, therapeutic doses may decrease respiratory drive to the point of apnea.[56972] Use of morphine immediate-release tablets and oral solution is contraindicated in patients with hypercarbia, while use of injectable suspension (DepoDur) and solution (Duramorph) is contraindicated in patients with upper airway obstruction. Rapid IV administration may result in chest wall rigidity. Respiratory depression, if left untreated, may cause respiratory arrest and death. Symptoms of respiratory depression include a reduced urge to breathe, a decreased respiratory rate, or deep breaths separated by long pauses (a "sighing" breathing pattern). Carbon dioxide retention from respiratory depression may also worsen opioid sedating effects. Only healthcare professionals who are knowledgeable of the use of opioids for the management of chronic pain should prescribe morphine extended-release capsules and tablets. These extended-release products should be reserved for patients in whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain. Do not use extended-release formulations for as-needed analgesics, for acute pain, or if the pain is mild or not expected to persist for an extended period of time.[55881] Proper dosing and titration are essential; patients should be monitored for respiratory depression, particularly after therapy initiation or after a dose increase. Caution should be exercised when converting from a different opioid to morphine, as initial dose overestimation may lead to fatal overdose. In patients with pulmonary disease such as chronic obstructive pulmonary disease (COPD), cor pulmonale, decreased respiratory reserve, emphysema, hypoxia, hypercapnia, respiratory insufficiency, or preexisting respiratory depression, it is recommended that non-opioid analgesics be considered as alternatives to morphine, as even usual therapeutic doses may decrease respiratory drive and cause apnea in these patient populations. Significant decreases in respiratory drive may lead to adverse intracranial effects from carbon dioxide retention; therefore, it is recommended to avoid the use of morphine extended-release tablets and capsules during a coma or impaired consciousness. Extreme caution should also be used in patients with chronic asthma, kyphoscoliosis (a type of scoliosis), hypoxemia, or paralysis of the phrenic nerve. Patients with advanced age, debilitation, or sleep apnea are at an increased risk for the development of respiratory depression associated with morphine. Use morphine with caution in patients with obesity as this is a risk factor for obstructive sleep-apnea syndrome and/or decreased respiratory reserve. Respiratory depression or other adverse reactions may persist for a significant period of time after discontinuation of or overdosage of long-acting morphine preparations; patients require close monitoring until their respiratory rate has stabilized. Patients who receive the extended-release liposome injection (DepoDur) may need monitoring beyond 48 hours after a dose. An increased risk of respiratory depression may be present if the surgical procedure is canceled after DepoDur administration. If treatment of respiratory depression in an individual physically dependent on opioids is necessary, administer the opioid antagonist with extreme care; titrate the antagonist dose by using smaller than usual doses. A high level of vigilant monitoring is recommended.[29159] [31296] [31637] [43053] [46350] [48404] [56971] [56972] [60209] [61668]
Opioids expose users to the risks of addiction, abuse, and misuse, which can occur at any dosage or duration. Although the risk of addiction in any individual is unknown, it can occur in individuals appropriately prescribed opioids. Addiction can occur at recommended dosages and if the drug is misused or abused. Assess each individual's risk for opioid addiction, abuse, or misuse before prescribing an opioid, and monitor for the development of these behaviors or conditions. Risks are increased in individuals with a personal or family history of substance abuse (including alcoholism) or mental illness (e.g., major depression). The potential for these risks should not prevent the proper management of pain in any given individual. Individuals at increased risk may be prescribed opioids, but use in such individuals necessitates intensive counseling about the risks and proper use of the opioid along with intensive monitoring for signs of addiction, abuse, and misuse. Abuse and addiction are separate and distinct from physical dependence and tolerance; individuals with addiction may not exhibit tolerance and symptoms of physical dependence. Opioids are sought by drug abusers and individuals with addiction disorders and are subject to criminal diversion. Abuse of opioids has the potential for overdose or poisoning and death. Consider these risks when prescribing or dispensing an opioid. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and educating about proper drug storage and disposal. Abuse or misuse of morphine extended-release tablets or capsules by cutting, breaking, chewing, crushing, snorting, or injecting the dissolved product will result in the uncontrolled delivery of morphine and can result in overdose and death. Dosing errors may result from confusion between mg and mL when prescribing, dispensing, and administering morphine oral solution. Ensure that the dose is communicated clearly and dispensed accurately. Instruct individuals on how to measure the dose and to use a calibrated oral dosing device. Improper substitution of Infumorph injectable solution (10 mg/mL or 25 mg/mL) for Duramorph injectable solutions (0.5 mg/mL or 1 mg/mL) may cause serious overdosage. Limit the total daily dose of Avinza to a maximum of 1,600 mg/day; Avinza doses more than 1,600 mg/day contain a quantity of fumaric acid that has not been demonstrated to be safe and may result in serious renal toxicity. Injectable morphine products have been associated with abuse and dependence among health care providers. Special measures to control the products within the hospital or clinic are recommended because of the limited indications, the overdosage risk, and the diversion/abuse risk. Specifically, rigid accounting, rigorous wastage control, and restricted access are recommended. Consumption of morphine extended-release capsules (i.e., Avinza or Kadian) with alcohol may result in increased drug exposure that may cause a fatal overdose; advise against ethanol ingestion and ethanol intoxication, including the ingestion of alcohol contained in prescription or non-prescription medications. Keep opioids out of the reach of children, others for whom the drug was not prescribed, and pets as accidental exposure or improper use may cause respiratory failure and a fatal overdose. Accidental exposure of even a single dose of an opioid, especially by younger individuals, can result in a fatal overdose. Because the risk of overdose increases as opioid dose increases, reserve titration to higher doses of an opioid for individuals in whom lower doses are insufficiently effective and in whom the expected benefits of using a higher dose opioid clearly outweigh the substantial risks. Extended-release opioids are not intended for use in the management of acute pain or on an as-needed basis but rather only for the management of severe and persistent pain that requires an extended treatment period with a daily opioid and for which alternative treatment options are inadequate. Discuss the availability of naloxone with all individuals and consider prescribing it in individuals who are at increased risk of opioid overdose, such as individuals who are also using other CNS depressants, who have a history of opioid use disorder (OUD), who have experienced a previous opioid overdose, or who have household members or other close contacts at risk for accidental exposure or opioid overdose.[31296] [31637] [35890] [40951] [43052] [46350] [48404] [51758] [61668] [65733] [68838]
Morphine is contraindicated in persons with known or suspected GI obstruction, including paralytic ileus. Morphine may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Monitor persons with biliary tract disease, including acute pancreatitis, for worsening symptoms.[46350] Moistened Arymo extended-release tablets may become sticky leading to difficulty in swallowing the tablets. Instruct persons not to pre-soak, lick, or otherwise wet Arymo extended-release tablets prior to placing in the mouth, and to take 1 tablet at a time with enough water to ensure complete swallowing immediately after placing in the mouth. Tablet stickiness and swelling may also predispose persons to intestinal obstruction and exacerbation of diverticulitis. Persons with underlying GI disorders such as esophageal cancer or colon cancer with a small gastrointestinal lumen are at greater risk of developing these complications. Consider use of an alternative analgesic in persons who have dysphagia and persons at risk for underlying GI disorders resulting in a small gastrointestinal lumen.[61668] Deodorized opium tincture (10 mg/mL) and camphorated opium tincture (0.4 mg/mL) are contraindicated for use in diarrhea caused by poisoning until the toxic material is eliminated from the GI tract.[56971] [56972]
Avoid opioid use in persons with CNS depression, impaired consciousness, or coma; opioids may obscure the clinical course in a person with a head trauma injury. Monitor persons who may be susceptible to the intracranial effect of carbon dioxide retention (e.g., those with evidence of increased intracranial pressure, brain tumor, or intracranial mass) for signs of sedation and respiratory depression, particularly when initiating opioid therapy. Opioids may reduce respiratory drive and resultant carbon dioxide retention can further increase intracranial pressure.[46350] Camphorated opium tincture (0.4 mg/mL) is contraindicated in convulsive states, such as those occurring in status epilepticus, tetanus, and strychnine toxicity.[56972] Monitor persons with a history of seizure disorder for worsened seizure control during opioid therapy. Opioids may increase the frequency of seizures in persons with seizure disorders, and may increase the risk of seizures occurring in other clinical settings associated with seizures.[46350] Use opium tincture with caution in persons with cerebral arteriosclerosis.[56971]
Warn persons against performing potentially hazardous activities such as driving or operating machinery unless they are tolerant to the effects of opioids and know how they will react to the medication. Opioids may impair mental or physical abilities required to perform such tasks.[46350]
Opioids may cause severe hypotension, including orthostatic hypotension and syncope in ambulatory persons. There is an increased risk in persons whose ability to maintain blood pressure has already been compromised by hypovolemia or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines, general anesthetics). Monitor these persons for signs of hypotension after initiating or titrating the opioid dosage. Avoid the use of opioids in persons with circulatory shock; it may cause vasodilation that can further reduce cardiac output and blood pressure.[46350]
Opioid use requires an experienced clinician who is knowledgeable about the use of opioids and how to mitigate the associated risks. Duramorph may be given epidurally, intrathecally, or intravenously; it is not for use in continuous microinfusion devices.[31296] Infumorph is only indicated for intrathecal or epidural administration; it is not for single-dose intravenous administration, intramuscular administration, or subcutaneous administration due to the risk of overdose. Infumorph must also not be used for single-dose neuraxial injection because it is too concentrated for accurate delivery of the smaller doses used in this setting.[51758] Administration of morphine via neuraxial routes requires an experienced clinician familiar with administration techniques, proper dosing, and potential patient management problems that may occur with epidural or intrathecal administration. Since single-dose neuraxial administration may result in serious adverse reactions, including acute or delayed respiratory depression; administration requires a specialized care setting where patients can be observed for up to 24 hours following the initial dose, including the initial test dose of Infumorph. The facility must be fully equipped to monitor patients and resuscitate any patient with severe opioid overdosage. Personnel must be familiar with the use of opioid antagonists. Continue to monitor patients receiving Infumorph during the first several days following catheter implantation. Epidural administration has been associated with less potential for immediate or late adverse reactions (e.g., respiratory depression) than intrathecal administration, and is preferable to the intrathecal route whenever possible. For safety concerns, limit Duramorph administration by the intrathecal or epidural routes to the lumbar area; thoracic administration has been shown to greatly increase the incidence of early and late respiratory depression even at doses of 1 to 2 mg. Similarly, limit Infumorph administration by the intrathecal route to the lumbar area. Improper substitution of Infumorph (10 or 25 mg/mL) for Duramorph (0.5 or 1 mg/mL) is likely to result in serious overdosage. Parenteral administration of other opioids in patients receiving epidural or intrathecal morphine may result in overdosage.[31296] [51758] Use caution when morphine is also given intravenously; because of a delay in maximum CNS effects (30 minutes) with intravenous morphine, rapid administration may result in overdose.[31296] Several factors contraindicate the administration of morphine by the epidural or intrathecal routes. These factors include infection at the injection site, concomitant anticoagulant therapy, uncontrolled coagulopathy, or the presence of any other concomitant therapy or medical condition which would render epidural or intrathecal administration of medication especially hazardous.[31296] [51758]
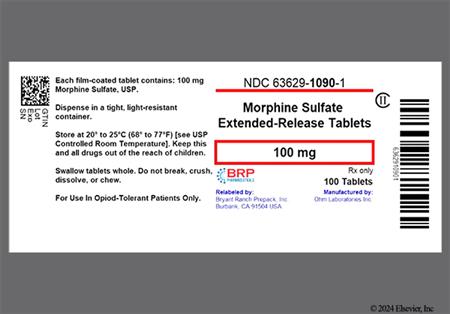
To reduce the risk of life-threatening adverse effects, several formulations of morphine are intended for opioid-tolerant individuals only. Do not use the following in opioid-naive individuals: 90 or 120 mg morphine biphasic-release capsules (Avinza); 100 or 200 mg morphine extended-release capsules (Kadian); 100 or 200 mg morphine extended-release tablets (MS Contin); 100 mg extended-release tablets (Morphabond); or 100 mg/5 mL morphine oral solution. Individuals considered opioid-tolerant are those taking at least 60 mg/day oral morphine, 30 mg/day oral oxycodone, 8 mg/day oral hydromorphone, 25 mg/day oral oxymorphone, 60 mg/day oral hydrocodone, 25 mcg/hour transdermal fentanyl, or an equianalgesic dose of another opioid for 1 week or longer.[31637] [35890] [40951] [43053] [60209]
Morphine and other opioid agonists can cause urinary retention and oliguria, due to increasing the tension of the detrusor muscle. Patients more prone to these effects include those with bladder obstruction, prostatic hypertrophy, urethral stricture, pelvic malignancy, or renal disease. Drug accumulation or prolonged duration of action can occur in patients with renal impairment or hepatic disease. In acute situations, patients require close monitoring to avoid excessive toxicity. Patients with chronic liver or renal disease may require less frequent dosing intervals.[40951] Urinary retention may occur with single epidural or intrathecal morphine administration, or during the first several days of hospitalization for the initiation of continuous intrathecal or epidural morphine therapy. Urinary retention may persist for 10 to 20 hours and occurs more frequently in male patients than females. Monitor patients closely for difficulty in urination and treat as clinically indicated; cases have responded to cholinomimetic treatment and/or judicious use of catheters.[31296] [51758]
Opioid agonists may be used in children with moderate to severe pain. However, certain morphine dosage formulations or administration methods may not be appropriate for children; children also require close monitoring during opioid use. The use of deodorized opium tincture (10 mg/mL) is contraindicated for use in neonates, infants, children, and adolescents; safety and efficacy have not been established.[56971] Neonates and infants younger than 6 months of age have highly variable clearance of opioid agonists. Therefore, infants younger than 6 months of age may be given morphine but must be closely monitored for apnea until 24 hours after their last dose. Guidelines suggest close monitoring of children up to 1 year of age.[23625] The safety and efficacy of epidural or intrathecal use of morphine in children have not been established. The safety and efficacy of extended-release morphine formulations have not been established in pediatric patients younger than 18 years.[31637] [35890] [40951] [60209]
Use morphine with caution in geriatric or debilitated adults as these patients are more susceptible to adverse reactions, especially sedation and respiratory depression, probably as a result of the altered distribution of the drug or decreased elimination. Initial doses may need to be reduced, and doses should be carefully titrated, taking into account analgesic effects, adverse reactions, and concomitant conditions and drugs that may increase CNS depression and depress respiration.[40951] According to the Beers Criteria, opiate agonists are considered potentially inappropriate medications (PIMs) in geriatric adults with a history of falls or fractures and should be avoided in these patient populations, except in the setting of severe acute pain, since opiates can produce ataxia, impaired psychomotor function, syncope, and additional falls. If an opiate must be used, consider reducing the use of other CNS-active medications that increase the risk of falls and fractures and implement strategies to reduce fall risk. In patients receiving palliative care, the balance of benefits and harms of medication management may differ from those of the general population of older adults.[63923]
Published studies with morphine use during pregnancy have not reported a clear association with morphine and major birth defects.[31296] [35890] [46350] [43053] [40951] Results for a population-based prospective cohort, including 448 subjects exposed to morphine at any time during pregnancy and 70 subjects exposed during the first trimester of pregnancy, indicate no increased risk for congenital malformations; however, risk cannot be excluded due to study methodological limitations. Neural tube defects (i.e., exencephaly and cranioschisis) have been noted when morphine was given subcutaneously to hamsters and mice at 5 and 16 times a human daily dose of 60 mg based on body surface area. Lower fetal body weight and increased abortion incidence were observed at 0.4 times the human daily morphine dose in rabbits, growth retardation at 6 times the human daily morphine dose in rats, and axial skeletal fusion and cryptorchidism at 16 times the human daily morphine dose in mice. Morphine doses of 3 to 4 times the human daily dose given during organogenesis and throughout lactation have produced cyanosis, hypothermia, decreased brain weight or body weight, adverse effects on reproductive tissues, and death in rats. Some long-term neurochemical changes in the brains of rat offspring which correlate with altered behavioral responses that persist through adulthood have been observed with morphine exposures comparable to and less than the human daily dose.[61668] Some experts suggest increased risk if morphine is used for prolonged periods during pregnancy or at high doses near term.[46351] Guidelines recommend early universal screening of pregnant individuals for opioid use and opioid use disorder at the first prenatal visit. Obtain a thorough history of substance use and review the Prescription Drug Monitoring Program to determine if individuals have received prior prescriptions for opioids or other high-risk drugs such as benzodiazepines. Discuss the risks and benefits of opioid use during pregnancy, including the risk of becoming physiologically dependent on opioids, the possibility for neonatal withdrawal, and how long-term opioid use may affect care during a future pregnancy.[64838] [64909] Morphine sulfate extended-release tablets or capsules are not recommended for use during and immediately before labor when other analgesic techniques are more appropriate. Opioids can prolong labor and obstetric delivery by temporarily reducing the strength, duration, and frequency of uterine contractions. This effect is not consistent and may be offset by an increased rate of cervical dilatation, which may shorten labor. In addition, neonates exposed to opioids in utero may present with respiratory depression at birth. Because of this, an opioid antagonist (e.g., naloxone) must be available for reversal of opioid-induced respiratory depression in the neonate at delivery.[35890] [40951] In individuals undergoing uncomplicated normal spontaneous vaginal birth, consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks. If opioids are used, use in combination with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate. Use immediate-release opioids instead of extended-release or long-acting opioids; order the lowest effective dosage and prescribe no greater quantity of opioids than needed for the expected duration of such pain severe enough to require opioids.[64909] For individuals using opioids for chronic pain, consider strategies to avoid or minimize the use of opioids, including alternative pain therapies (i.e., nonpharmacologic) and nonopioid pharmacologic treatments. Opioid agonist pharmacotherapy (e.g., methadone or buprenorphine) is preferable to medically supervised withdrawal in pregnant individuals with opioid use disorder.[64838]
Use of morphine oral dosage forms, suppositories, and solution for injection is contraindicated in patients who are receiving or have received MAOI therapy within the past 14 days. Manufacturers of other morphine dosage forms do not recommend the concurrent use of MAOIs or morphine use within 14 days of stopping such treatment. Additive CNS depression, drowsiness, dizziness, or hypotension may occur.[29159] [31296] [31637] [35890] [40951] [43053] [46350] [48404] [56972] [61668]
Counsel people who may become pregnant and people who can cause pregnancy in others about the reproductive risk associated with opioids. Long-term use of opioids may influence the hypothalamic-pituitary-gonadal axis, leading to hormonal changes that may manifest as a libido decrease, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical manifestations of hypogonadism is unknown. It is not known whether the effects on fertility are reversible.[31296] [35890] [40951] [46350] [43053] [60660]
Neonates and infants exposed to this medication in utero may present with respiratory depression and psycho-physiologic effects at birth. Monitor exposed newborns for signs of excess sedation and respiratory depression. If necessary, administer an opioid antagonist (e.g., naloxone) to reverse the effects of opioid-induced respiratory depression. Long-term use of opioids during pregnancy can result in physical dependence in the exposed infant. Monitor newborns for symptoms of withdrawal and manage accordingly. Neonatal opioid withdrawal syndrome may present as irritability, hyperactivity, abnormal sleep pattern, high-pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. It can be life-threatening if not recognized and treated. Onset, duration, and severity of opioid withdrawal may vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination by the infant.[31296] [35890] [40951] [43053] [46350] [55881] [64838]
Avoid use of morphine extended-release products and anhydrous oral solution/opium tincture during breast-feeding. Use other morphine formulations with caution. Morphine passes into breast milk in a dose-dependent manner with a relative infant dose of 9.09% to 35%. The milk to plasma ratio of morphine is between 1.1 to 3.6.[70365] Morphine may cause serious adverse effects in the child, including drowsiness, CNS depression, and death. Use morphine at the lowest effective dose for the shortest amount of time with close monitoring of the breast-fed child.[70364] Monitor children exposed to opioids through breast milk for excess sedation and respiratory depression. Withdrawal symptoms may occur in the breast-fed child when maternal administration of the opioid is stopped or when breast-feeding is discontinued, particularly with chronic use.[31296] [35890] [46350] [43053] [40951] [55881] [64838] Alternative analgesics include acetaminophen and ibuprofen.[70364] In studies of epidural morphine given postcesarean section, morphine passage into colostrum and breast milk is minimal, while higher concentrations are found with intravenous or oral administration.[61697] In a study of 5 lactating patients given epidural, IV, or IM morphine postoperatively, the highest morphine concentrations in milk were 82 mcg/L (measured 30 minutes after two, 4 mg epidural doses) versus 500 mcg/L (measured 45 minutes after 15 mg parenteral dose).[61698] Morphine passage into breast milk was assessed in a study of 5 lactating patients who were given a 7.5 mg loading dose of IV morphine after umbilical cord clamping, then 1 to 1.5 mg every 6 minutes via IV patient-controlled analgesia (PCA), then 5 to 30 mg PO every 2 to 3 hours as needed for pain. Average IV morphine consumption in the first 48 hours was approximately 150 mg. Average morphine consumption across the entire study period (96 hours) was approximately 250 mg (IV and oral). Average milk concentrations among all patients were 50 to 65 mcg/L during the first 48 hours; concentrations decreased to 20 mcg/L at 72 to 96 hours postpartum. Using the maximum reported concentration of 65 mcg/L and assuming 30% oral absorption by the infant, an exclusively breast-fed infant would absorb a maximum of 3 mcg/kg/day equal to 0.3% of the IV maternal weight-adjusted daily dose.[61699] [70364]
Morphine is a potent mu-opiate receptor agonist. Opiate receptors include mu, kappa, and delta, which have been reclassified by an International Union of Pharmacology subcommittee as OP1 (delta), OP2 (kappa), and OP3 (mu). These receptors are coupled with G-protein (guanine-nucleotide-binding protein) receptors and function as modulators, both positive and negative, of synaptic transmission via G-proteins that activate effector proteins. Opioid-G-protein systems include adenylyl cyclase-cyclic adenosine monophosphate (cAMP) and phospholipase3 C (PLC)-inositol 1,4,5 triphosphate (Ins(1,4,5) P3)-Ca2).[25308]
Opiates do not alter the pain threshold of afferent nerve endings to noxious stimuli, nor do they affect the conductance of impulses along peripheral nerves. Analgesia is mediated through changes in the perception of pain at the spinal cord (mu2-, delta-, kappa-receptors) and higher levels in the CNS (mu1- and kappa3 receptors). There is no ceiling effect of analgesia for opiates. The emotional response to pain is also altered. Opioids close N-type voltage-operated calcium channels (kappa-receptor agonist) and open calcium-dependent inwardly rectifying potassium channels (mu and delta receptor agonist) resulting in hyperpolarization and reduced neuronal excitability. Binding of the opiate stimulates the exchange of guanosine triphosphate (GTP) for guanosine diphosphate (GDP) on the G-protein complex. Binding of GTP leads to a release of the G-protein subunit, which acts on the effector system. In this case of opioid-induced analgesia, the effector system is adenylate cyclase and cAMP located at the inner surface of the plasma membrane.[25309] Thus, opioids decrease intracellular cAMP by inhibiting adenylate cyclase that modulates the release of nociceptive neurotransmitters such as substance P, GABA, dopamine, acetylcholine and norepinephrine. Opioids also modulate the endocrine and immune systems. Opioids inhibit the release of vasopressin, somatostatin, insulin, and glucagon.[25310]
The stimulatory effects of opioids are the result of 'disinhibition' as the release of inhibitory neurotransmitters such as GABA and acetylcholine is blocked. The exact mechanism how opioid agonists cause both inhibitory and stimulatory processes is not well understood. Possible mechanisms include differential susceptibility of the opioid receptor to desensitization or activation of more than one G-protein system or subunit (one excitatory and one inhibitory) by an opioid receptor.
Clinically, stimulation of mu-receptors produces analgesia, euphoria, respiratory depression, miosis, decreased gastrointestinal motility, sedation, somnolence, and physical dependence.[40951] Morphine enhances tone in the long segments of longitudinal muscle and inhibits propulsive contraction of both circular and longitudinal muscles to decrease GI motility.[56971] Kappa-receptor stimulation also produces analgesia, miosis, respiratory depression, as well as, dysphoria and some psychomimetic effects (i.e., disorientation and/or depersonalization). Miosis is produced by an excitatory action on the autonomic segment of the nucleus of the oculomotor nerve. Respiratory depression is caused by direct action of opiate agonists on respiratory centers in the brain stem. Opiate agonists increase smooth muscle tone in the antral portion of the stomach, the small intestine (especially the duodenum), the large intestine, and the sphincters. Opiate agonists also decrease secretions from the stomach, pancreas, and biliary tract. The combination of effects of opiate agonists on the GI tract results in constipation and delayed digestion. Urinary smooth muscle tone is also increased by opiate agonists. The tone of the bladder detrusor muscle, ureters, and vesical sphincter is increased, which sometimes causes urinary retention.
Several other clinical effects occur with opiate agonists including cough suppression, hypotension, histamine release, nausea, and vomiting.[40951] The antitussive effects of opiate agonists are mediated through direct action on receptors in the cough center of the medulla. Cough suppression can be achieved at lower doses than those required to produce analgesia. Hypotension is possibly due to an increase in histamine release and/or depression of the vasomotor center in the medulla. Induction of nausea and vomiting possibly occurs from direct stimulation of the vestibular system and/or the chemoreceptor trigger zone. Morphine may inhibit the secretion of ACTH, cortisol, testosterone, and luteinizing hormone. Morphine may stimulate the secretion of prolactin, growth hormone, insulin, and glucagon.[40951]
Revision Date: 10/15/2025, 01:33:00 AMMorphine sulfate is administered orally, parenterally, intrathecally, epidurally, and rectally. There is no predictable relationship between morphine serum concentrations and analgesic response; however, there is a minimum effective analgesia plasma concentration in a given patient. The minimum effective analgesia plasma concentration of morphine varies from patient to patient. Several factors may affect a patient's response to a given opiate agonist including age, prior opiate therapy, medical condition, and emotions. Also, there is no relationship between morphine concentrations and incidence of adverse events, although higher concentrations are associated with more adverse events than lower concentrations.[46350][48403]
Metabolism of morphine occurs primarily through conjugation in the liver. Morphine is also metabolized by P-glycoprotein (P-gp), which is present on the apical side of enterocytes and on the canalicular side of hepatocytes. Lastly, morphine undergoes N-demethylation by cytochrome P450 3A4 enzymes to yield normorphine; however, the pathway contributes less than 4% of the given dose to total urinary excretion of morphine. Morphine is conjugated with glucuronic acid through UDP-glucuronosyltransferases to form 3-glucuronide (50%), 6-glucuronide (5% to 15%), and 3,6-glucuronide and other minor metabolites. Morphine 3-glucuronide has a low affinity for opioid receptors, has no analgesic activity, and may cause hyperalgesia (hyperesthesia), myoclonus, and allodynia. In addition, the 3-glucuronide metabolite may be important in the development of tolerance to morphine. Morphine 3-glucuronide has been shown to stimulate respiration, but the mechanism (either direct stimulation or morphine and morphine 6-glucuronide antagonism) is unclear. Morphine 6-glucuronide has analgesic activity and may significantly contribute to morphine's activity. With chronic dosing of morphine, the systemic exposure of the glucuronide metabolites is greater than that of morphine.[25336] Morphine 6-glucuronide crosses the blood-brain barrier slowly. Thus, prolonged effects may be seen after morphine discontinuation or dialysis to remove morphine 6-glucuronide.
Excretion of morphine is largely in the urine and bile as the morphine 3-glucuronide and 6-glucuronide metabolites. Smaller amounts are excreted as secondary conjugates and approximately 10% is eliminated as unchanged drug. Renal clearance of morphine and morphine- 6-glucuronide exceeds creatinine clearance, which suggests that both are actively secreted by the kidney. Within about 24 hours of the last dose, urinary elimination approximates 90%. Between 7% to 10% is excreted in the feces mainly via the bile. Typical morphine clearance in adults is approximately 15 to 20 mL/minute/kg.[46350] The elimination half-life of morphine is about 1.5 to 2 hours; a half-life after IV administration of 2 to 4 hours has been reported. In some studies with longer durations of plasma sampling, a terminal half-life of approximately 15 hours was reported.[40951] Analgesia can be maintained for 3 to 7 hours after immediate release morphine administration.
Affected cytochrome P450 isoenzymes and/or drug transporters: P-gp
Morphine is a substrate for P-gp.[34448]
Morphine is one-third to one-sixth as potent when administered orally compared to intravenous administration due to morphine's significant first-pass metabolism. The oral bioavailability of morphine is approximately 20% to 40%.[40951] Morphine is readily absorbed from the gut and is absorbed even faster after rectal administration. Oral absorption of the immediate release products can be increased by food. Peak analgesia is obtained about 60 minutes after oral administration. Oral sustained-release products have a slower onset of action and at steady state will have a lower maximum serum concentration and higher minimum serum concentration compared to immediate-release oral morphine. After every 24 hour dosing of Kadian, the maximum plasma concentration occurs in about 8 hours. Avinza capsules consist of an immediate release component that rapidly achieves a morphine concentration and an extended release component that maintains the morphine plasma concentrations throughout the 24-hour dosing interval. Steady-state plasma concentrations of morphine are achieved 2 to 3 days after initiation of daily Avinza therapy. Kadian is not bioequivalent to other extended-release morphine preparations. In a crossover study, at steady-state, similar maximum concentrations, time to maximum concentrations, and systemic exposure over time were achieved with Oramorph SR and MS Contin; 30 mg of either product was given every 12 hours for 3 days followed by a 14-day washout period before the other product was given. The mean time to peak concentration after Oramorph SR was 3.75 +/- 1.21 hours and after MS Contin was 3.48 +/- 1.25 hours. The mean peak concentration was 22.61 +/- 5.83 ng/mL for Oramorph SR and 24.28 +/- 5.28 ng/mL for MS Contin, whereas the mean minimum serum concentration was 11.06 +/- 3.64 ng/mL for Oramorph SR and 9.23 +/- 2.94 ng/mL for MS Contin.[33125] When Arymo ER, MS Contin, or Morphabond ER tablets are given as a fixed dosing regimen, steady-state is achieved in about 1 day.[40951] [60209] [61668] Food does not significantly affect the Cmax or overall exposure (AUC) of Arymo ER tablets.[61668] Administration of a single dose of Morphabond ER with a standardized high fat meal resulted in a 33% increase in Cmax and no change in AUC compared to a fasted state.[60209]
Peak analgesia is obtained within 20 minutes after IV injection and the duration of analgesia is approximately 3 to 6 hours.[52190]
Peak analgesia is obtained about 30 to 60 minutes after IM injections and the duration of analgesia is approximately 3 to 6 hours.[52190]
Peak analgesia is obtained about 50 to 90 minutes after subcutaneous injections and the duration of analgesia is approximately 3 to 6 hours.[52190]
Rectal Route
Peak analgesia is achieved about 20 to 60 minutes after rectal administration.[48404] The approximate bioavailability of morphine after rectal administration is 30% (range 6% to 99%) in children. Peak serum concentrations are achieved within 30 minutes when morphine is dissolved in propylene glycol and within 60 to 90 minutes when an aqueous morphine solution is mixed with a dry starch hydrogel.[52231]
Intrathecal Route
Lower doses of morphine (one-tenth of the dose) are required to produce similar analgesia when administered intrathecally versus epidurally because intrathecal administration circumvents the meningeal diffusion barriers. When morphine is injected into the intrathecal space, it slowly diffuses out into the systemic circulation. The slow rate of elimination accounts for the prolonged duration of action when administered by this route. Intrathecal morphine may produce noticeable effects, both pain relief and adverse effects, for up to 24 hours.[31296]
Epidural Route
After epidural administration, morphine is rapidly absorbed systemically with peak plasma concentrations attained in 10 to 15 minutes. Analgesia achieved with epidural morphine is not dependent on systemic morphine concentrations, and the duration of analgesia continues beyond the time during which morphine may be detected in the plasma.[31296]
The half-life of morphine is significantly prolonged and clearance is decreased in patients with cirrhosis or hepatic disease. The morphine-3 glucuronide and 6-glucuronide to morphine plasma AUC ratios are also decreased, indicating diminished metabolic activity.[40951] Adequate studies of morphine pharmacokinetics have not been conducted in patients with severe hepatic impairment.[46350]
In patients with renal dysfunction, morphine AUC is increased and clearance is decreased. The metabolites, morphine-3 glucuronide and morphine-6 glucuronide, may accumulate to much higher plasma concentrations in patients with renal failure.[61668] Adequate studies of morphine pharmacokinetics have not been conducted in patients with severe renal impairment.[46350]
Infants, Children, and Adolescents
Morphine's estimated half-life and clearance are 2 hours and 23.6 mL/kg/minute, respectively. The pharmacokinetics of morphine in pediatric patients appear to approach adult values around 2 to 6 months of age; however, there is large interpatient variability and a range of 2 weeks to 2.5 years of age has been reported. Some young children may exhibit clearance up to twice that of adults.[25335][52231][52233] In a population pharmacokinetic analysis of 66 patients 2 to 17 years, the geometric mean plasma half-life was up to 1.8 hours and the mean terminal elimination plasma half-life was 18.6 hours. The single dose mean Cmax of both the morphine 3-glucuronide and 6-glucuronide metabolite was not greater than in adults.[43053]
Neonates
In premature neonates, the estimated half-life and clearance of morphine are 9 hours and 2.2 mL/kg/minute, respectively; in term neonates, these estimated values are 6.5 hours and 8.1 mL/kg/minute, respectively. Preterm neonates are capable of glucuronidation, but this capability is influenced by gestational and postnatal age and birth weight leading to a lower metabolic capacity and lower elimination rate in preterm and term neonates compared to older pediatric patients.[25335]
A pharmacokinetic analysis of healthy subjects taking extended-release morphine demonstrated that morphine concentrations were similar in males and females.[60209]
Chinese subjects given intravenous morphine had a higher clearance compared to Caucasian subjects (1,852 +/- 116 mL/minute vs. 1,495 +/- 80 mL/minute).[61668]
Published studies with morphine use during pregnancy have not reported a clear association with morphine and major birth defects.[31296] [35890] [46350] [43053] [40951] Results for a population-based prospective cohort, including 448 subjects exposed to morphine at any time during pregnancy and 70 subjects exposed during the first trimester of pregnancy, indicate no increased risk for congenital malformations; however, risk cannot be excluded due to study methodological limitations. Neural tube defects (i.e., exencephaly and cranioschisis) have been noted when morphine was given subcutaneously to hamsters and mice at 5 and 16 times a human daily dose of 60 mg based on body surface area. Lower fetal body weight and increased abortion incidence were observed at 0.4 times the human daily morphine dose in rabbits, growth retardation at 6 times the human daily morphine dose in rats, and axial skeletal fusion and cryptorchidism at 16 times the human daily morphine dose in mice. Morphine doses of 3 to 4 times the human daily dose given during organogenesis and throughout lactation have produced cyanosis, hypothermia, decreased brain weight or body weight, adverse effects on reproductive tissues, and death in rats. Some long-term neurochemical changes in the brains of rat offspring which correlate with altered behavioral responses that persist through adulthood have been observed with morphine exposures comparable to and less than the human daily dose.[61668] Some experts suggest increased risk if morphine is used for prolonged periods during pregnancy or at high doses near term.[46351] Guidelines recommend early universal screening of pregnant individuals for opioid use and opioid use disorder at the first prenatal visit. Obtain a thorough history of substance use and review the Prescription Drug Monitoring Program to determine if individuals have received prior prescriptions for opioids or other high-risk drugs such as benzodiazepines. Discuss the risks and benefits of opioid use during pregnancy, including the risk of becoming physiologically dependent on opioids, the possibility for neonatal withdrawal, and how long-term opioid use may affect care during a future pregnancy.[64838] [64909] Morphine sulfate extended-release tablets or capsules are not recommended for use during and immediately before labor when other analgesic techniques are more appropriate. Opioids can prolong labor and obstetric delivery by temporarily reducing the strength, duration, and frequency of uterine contractions. This effect is not consistent and may be offset by an increased rate of cervical dilatation, which may shorten labor. In addition, neonates exposed to opioids in utero may present with respiratory depression at birth. Because of this, an opioid antagonist (e.g., naloxone) must be available for reversal of opioid-induced respiratory depression in the neonate at delivery.[35890] [40951] In individuals undergoing uncomplicated normal spontaneous vaginal birth, consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks. If opioids are used, use in combination with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate. Use immediate-release opioids instead of extended-release or long-acting opioids; order the lowest effective dosage and prescribe no greater quantity of opioids than needed for the expected duration of such pain severe enough to require opioids.[64909] For individuals using opioids for chronic pain, consider strategies to avoid or minimize the use of opioids, including alternative pain therapies (i.e., nonpharmacologic) and nonopioid pharmacologic treatments. Opioid agonist pharmacotherapy (e.g., methadone or buprenorphine) is preferable to medically supervised withdrawal in pregnant individuals with opioid use disorder.[64838]
Avoid use of morphine extended-release products and anhydrous oral solution/opium tincture during breast-feeding. Use other morphine formulations with caution. Morphine passes into breast milk in a dose-dependent manner with a relative infant dose of 9.09% to 35%. The milk to plasma ratio of morphine is between 1.1 to 3.6.[70365] Morphine may cause serious adverse effects in the child, including drowsiness, CNS depression, and death. Use morphine at the lowest effective dose for the shortest amount of time with close monitoring of the breast-fed child.[70364] Monitor children exposed to opioids through breast milk for excess sedation and respiratory depression. Withdrawal symptoms may occur in the breast-fed child when maternal administration of the opioid is stopped or when breast-feeding is discontinued, particularly with chronic use.[31296] [35890] [46350] [43053] [40951] [55881] [64838] Alternative analgesics include acetaminophen and ibuprofen.[70364] In studies of epidural morphine given postcesarean section, morphine passage into colostrum and breast milk is minimal, while higher concentrations are found with intravenous or oral administration.[61697] In a study of 5 lactating patients given epidural, IV, or IM morphine postoperatively, the highest morphine concentrations in milk were 82 mcg/L (measured 30 minutes after two, 4 mg epidural doses) versus 500 mcg/L (measured 45 minutes after 15 mg parenteral dose).[61698] Morphine passage into breast milk was assessed in a study of 5 lactating patients who were given a 7.5 mg loading dose of IV morphine after umbilical cord clamping, then 1 to 1.5 mg every 6 minutes via IV patient-controlled analgesia (PCA), then 5 to 30 mg PO every 2 to 3 hours as needed for pain. Average IV morphine consumption in the first 48 hours was approximately 150 mg. Average morphine consumption across the entire study period (96 hours) was approximately 250 mg (IV and oral). Average milk concentrations among all patients were 50 to 65 mcg/L during the first 48 hours; concentrations decreased to 20 mcg/L at 72 to 96 hours postpartum. Using the maximum reported concentration of 65 mcg/L and assuming 30% oral absorption by the infant, an exclusively breast-fed infant would absorb a maximum of 3 mcg/kg/day equal to 0.3% of the IV maternal weight-adjusted daily dose.[61699] [70364]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.