ThisiscontentfromElsevier'sDrugInformation
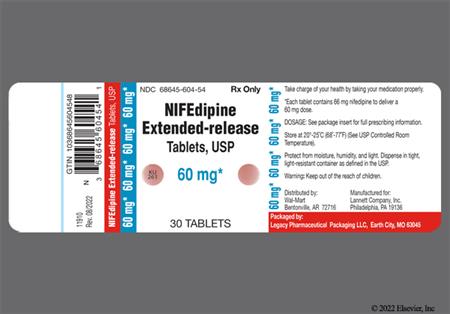
Nifedipine
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
10 mg PO 3 times daily, initially. Increase the dose every 7 to 14 days until desired clinical response is achieved. May increase dose to 20 mg PO 3 times daily, then 30 mg PO 3 times daily over 3 days if needed or may increase dose by 10 mg/dose every 4 to 6 hours for hospitalized patients. Usual dose: 10 to 20 mg PO 3 times daily. Usual Max: 30 mg/dose and 120 mg/day. Max: 180 mg/day.[29068]
30 or 60 mg PO once daily, initially. Increase the dose every 7 to 14 days until desired clinical response is achieved. Usual Max: 90 mg/day. Max: 120 mg/day.[42064]
30 or 60 mg PO once daily, initially. May increase dose over 7 to 14 days if further control is needed. Usual dose: 30 to 90 mg/day. Max: 120 mg/day.[31749] [42064] [72603]
0.2 to 0.5 mg/kg/day PO in 1 to 2 divided doses. May increase dose if further control is needed. Max: 3 mg/kg/day.[32337] [32338] [62353] A maximum of 120 mg/day PO has been recommended by pediatric hypertension guidelines; however, some experts recommend that doses up to 180 mg/day may be necessary in some clinical situations.[32338] [62353]
0.2 to 0.5 mg/kg/dose (Max: 10 mg/dose) PO every 4 to 6 hours as needed.[32338] To avoid a precipitous and unexpected drop in blood pressure, some authors recommend initial doses less than 0.2 mg/kg and avoiding use in patients with CNS injury.[32338] [33329] Mean doses of 0.22 to 0.23 mg/kg (range: 0.04 to 0.69 mg/kg) have been reported in retrospective studies (n = 299 pediatric patients 0.1 to 18.9 years).[33330] [33331] NOTE: Per the FDA and manufacturers, immediate-release nifedipine dosage forms should not be used to treat hypertension and should only be used to treat patients with chronic stable angina or vasospastic angina. The immediate-release nifedipine formulation has been associated with serious side effects when used to treat adult patients with hypertension, hypertensive urgency, hypertensive emergency, or coexisting myocardial infarction. Although the use of immediate-release nifedipine for the treatment acute hypertensive episodes is still relatively common practice in pediatric patients, considerable controversy exists and caution should be used.
Conflicting data exist regarding the use of nifedipine for proteinuria associated with diabetic nephropathy. A significant increase in urinary albumin excretion was reported in 7 normotensive patients with diabetic nephropathy who were treated with slow-release nifedipine 20 mg PO twice daily and followed for 6 weeks.[24070] A significant increase in urinary albumin excretion was also reported in a crossover study of 14 non-insulin dependent diabetic patients during a 20-week trial. The mean study dose was 45 +/- 8 mg of long-acting nifedipine once daily.[24040] Conversely, in another study, 27 diabetics with persistent microalbuminuria received nifedipine 20 to 80 mg PO once daily for 12 months. These data demonstrated a decrease in urinary albumin excretion (UAE) during therapy, however, UAE increased to levels greater than baseline once therapy was discontinued.[24071]
See adult dosage. In general, initiate dosage at the lower end of the adult dosage range. Nifedipine plasma concentrations and half-life are significantly increased in geriatric patients. Adjust dosage based on clinical response.
Doses of 10 to 20 mg PO 3 times daily have been used.[24272] [24273] [32348] [32349]
See adult dosage. In general, initiate dosage at the lower end of the adult dosage range. Nifedipine plasma concentrations and half-life are significantly increased in geriatric patients. Adjust dosage based on clinical response.
NOTE: Clinical practice guidelines recommend the use of a first line tocolytic (i.e., beta agonist, calcium channel blocker, or NSAID) for short-term use (up to 48 hours) to allow for administration of antenatal corticosteroids to enhance fetal lung maturation, magnesium sulfate for fetal neuroprotection, or transport to a tertiary facility, if indicated. There is no evidence that tocolytic therapy alone has any favorable effect on neonatal outcomes. Maintenance therapy with tocolytics is ineffective for preventing preterm birth and improving neonatal outcomes and is not recommended.[57230]
Various regimens have been used. The recommended dose by the American College of Obstetrics and Gynecology (ACOG) is a 30-mg loading dose, followed by 10 to 20 mg every 4 to 6 hours.[33039] NOTE: A route of administration is not provided, although typically PO and/or SL is used for the loading dose and PO is used for subsequent dosing. Typical regimens for the loading dose include 10 mg SL with 20 mg PO, 30 mg PO, or 10 to 20 mg SL or PO every 15 to 20 minutes until contractions stop, up to a maximum of 30 to 40 mg over 1 hour. Although not definitive, typical duration of tocolysis for acute inhibition of premature labor is 24 to 72 hours. When compared to ritodrine or magnesium sulfate, nifedipine has generally demonstrated similar efficacy with similar or fewer maternal side effects. Although maintenance use of tocolytics after acute suppression of contractions has not been shown to prolong pregnancy, doses of 10 to 20 mg PO every 4 to 6 hours have been used. Additionally, some studies have used maintenance dosing with slow-release nifedipine (doses of 60 to 160 mg/day PO).[25430] [25431] [33039] [33596] [33597] Magnesium sulfate therapy should not be given concurrently because of additive effects on maternal cardiac function.
10 to 30 mg PO 30 to 45 minutes before meals.[55823] [66609] Reserve for individuals who refuse or are not candidates for more definitive therapies (pneumatic dilation or surgical myotomy) or who fail to respond to botulinum toxin injections.[66609]
30 mg PO every 12 hours or 20 mg PO every 8 hours until symptoms resolve.[72681] [72682]
30 mg PO every 12 hours until symptoms resolve.[72683]
30 mg PO every 12 hours or 20 mg PO every 8 hours starting the day before ascent and continuing for 4 to 7 days after reaching the target altitude or until descent is initiated.[72681] [72682]
20 mg PO twice daily for 6 to 8 weeks.[67105] [67107] [68162] Guidelines suggest topical calcium channel blockers as first-line therapy. Given the higher incidence of adverse effects with oral calcium channel blockers, topical administration is preferred.[67105] [68165]
Apply an almond-sized amount intra-anally every 8 to 12 hours for 2 to 8 weeks.[67107] [67108] [67110] [68162] Guidelines suggest topical calcium channel blockers as first-line therapy.[67105] [68165]
30 mg PO once daily, initially. Increase the dose to 60 to 120 mg PO twice daily as tolerated.[65921] [68170]
0.3 to 0.6 mg/kg/dose PO once daily, initially. Increase dose as tolerated. Usual dose: 2 to 3 mg/kg/day. Max: 180 mg/day.[60727]
10 mg PO 3 times daily for 2 to 7 days, then 20 mg PO 3 times daily for up 8 to 12 weeks.[68505] [68506] [68541]
10 to 20 mg PO every 15 to 30 minutes, then 10 to 20 mg PO every 2 to 6 hours until blood pressure control is attained. Max: 180 mg/day.[63903] [66595] [69901] [69902] [69903]
10 to 20 mg PO every 15 to 30 minutes, then 10 to 20 mg PO every 2 to 6 hours until blood pressure control is attained. Max: 180 mg/day.[63903] [66595] [69901] [69902] [69903]
10 mg PO once daily, initially. Increase the dose by 10 mg/day every 2 weeks based on tolerability. Usual dose: 10 to 20 mg PO 2 to 3 times daily. Max: 90 mg/day.[70033] [70038] [70040] [70041] Short-acting calcium channel blockers are more likely to produce vasodilatory adverse effects and duration of action lasts only a few hours; therefore, long-acting calcium channel blockers may be preferred.[70033]
30 mg PO once daily, initially. Increase the dose to 60 mg PO once daily after 1 week based on tolerability. Max: 120 mg/day.[70033] [70038] [70039] [70040] [70041]
30 to 60 mg PO once daily, initially. May increase the dose over 7 to 14 days if further control is needed. Usual dose: 30 to 120 mg/day.[31749] [42064] [63903] [72603]
30 to 60 mg PO once daily, initially. May increase the dose over 7 to 14 days if further control is needed. Usual dose: 30 to 120 mg/day.[31749] [42064] [63903]
90 mg/day PO for Procardia XL or 180 mg/day PO for immediate-release capsules for angina; 90 mg/day PO for most extended-release tabs and 120 mg/day PO for Procardia XL for hypertension.
90 mg/day PO for Procardia XL or 180 mg/day PO for immediate-release capsules for angina; 90 mg/day PO for most extended-release tabs and 120 mg/day PO for Procardia XL for hypertension.
Safety and efficacy have not been established; however, up to 3 mg/kg/day PO (not to exceed 180 mg/day) for extended-release tablets has been used off-label for hypertension; 0.5 mg/kg/dose (not to exceed 10 mg/dose) has been used off-label for hypertensive urgency/emergency.
Safety and efficacy have not been established; however, up to 3 mg/kg/day PO (not to exceed 180 mg/day) for extended-release tablets has been used off-label for hypertension; 0.5 mg/kg/dose (not to exceed 10 mg/dose) has been used off-label for hypertensive urgency/emergency.
Dosage reduction and close monitoring of blood pressure is advised in patients with hepatic impairment. Although no specific guidelines are available, the half-life and AUC of nifedipine is markedly increased in cirrhotic patients.
No dosage adjustment is needed.
Intermittent hemodialysis
Nifedipine is minimally removed by hemodialysis or hemoperfusion. Therefore, no supplemental dosage is needed following hemodialysis.
† Off-label indication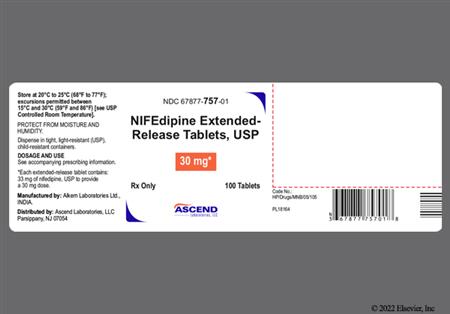





Description: Nifedipine is the prototype of the dihydropyridine class of calcium-channel antagonists. It is structurally and pharmacologically similar to other dihydropyridines including amlodipine, felodipine, isradipine, and nicardipine. In general, the dihydropyridine-type calcium-channel antagonists have more prominent effects on vasodilation and coronary flow relative to diltiazem and verapamil. Unlike both diltiazem and verapamil, however, nifedipine has negligible effects on AV nodal conduction. This difference is attributed to the fact that nifedipine binds to a different site in the calcium channel. Nifedipine is used in the treatment of Prinzmetal's angina, hypertension, and other vascular disorders such as Raynaud's phenomenon†. Nifedipine is available in immediate-release and extended-release dosage forms. The immediate-release nifedipine dosage forms should only be used to treat patients with chronic stable or vasospastic angina angina; the immediate-release formulation is associated with serious side effects when used to treat patients with hypertension, hypertensive urgency, hypertensive emergency, or coexisting myocardial infarction.[24732] Although its actions were described in 1972, nifedipine was not approved by the FDA until 1981.
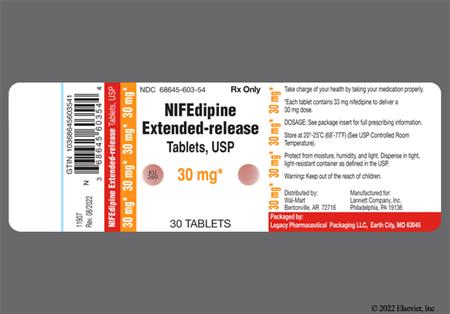
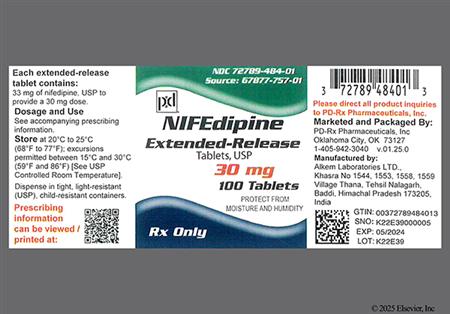
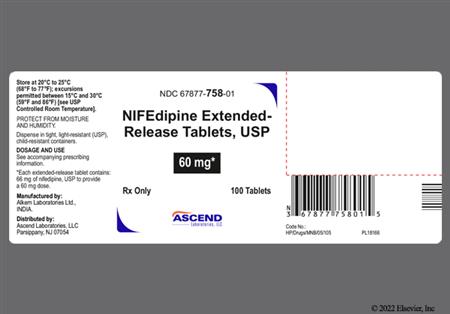
For storage information, see the specific product information within the How Supplied section.
Extemporaneous compounding instructions for Nifedipine 0.5% rectal topical ointment
Sublingual Administration†
Although calcium-channel blockers are effective drugs for treating angina, nifedipine has rarely been associated with increased angina (<= 1%). This reaction may be a result of excessive lowering of blood pressure, coronary steal, or reflex tachycardia. Peripheral edema (4%—30%) has been attributed to nifedipine therapy and appears to be dose-related and related to the mechanism of action, which involves peripheral vasodilation. Peripheral edema occurred in about one in 25 patients (4%) at doses less than 60 mg/day, in about one in eight patients (12.5%) at >= 120 mg/day, and about 30% of patients at doses of 180 mg/day. This reaction reflects the potent vasodilatory effect of this drug because it occurs more frequently with nifedipine than with other calcium-channel blockers. This edema occurs primarily in the lower extremities and usually responds to diuretic therapy. Although not readily distinguishable from the natural history of disease, congestive heart failure (2%) was reported in large uncontrolled experience in patients with vasospastic or resistant angina pectoris (about half had concomitant treatment with beta-blockers). In a subgroup of approximately 250 patients with a diagnosis of congestive heart failure as well as angina, symptoms of congestive heart failure occurred in about 6.7% of patients. With patients whose angina is complicated by congestive heart failure, care should be taken to differentiate peripheral edema from the effects of increasing left ventricular dysfunction. In most patients the hypotensive effect of nifedipine is modest and well tolerated; however, some patients have had excessive and poorly tolerated hypotension (<1%—5%). These responses have usually occurred during initial titration or at the time of dose increase, and may be more likely in patients using concomitant beta-blockers. Other cardiovascular-related adverse events reported during nifedipine therapy include: flushing or heat sensation (< 3%—25%), palpitations (<1%—7%), syncope (0.5%—1%) (mostly with initial dosing and/or an increase in dose), erythromelalgia (0.5%), chest pain (unspecified) (<= 3%), substernal chest pain (< 1%), cardiac arrest (< 1%), phlebitis (< 1%), orthostatic hypotension (< 1%), cutaneous angiectases (< 1%), arrhythmia exacerbation (<= 1%), atrial fibrillation (< 1%), bradycardia (< 1%), sinus tachycardia (<= 1%), atrial or ventricular dysrhythmias (0.7%), extrasystole (i.e., premature ventricular contractions (PVCs))(< 1%), ventricular arrhythmias (< 0.5%), and conduction disturbances (0.5%).[29068] [42064] [31749]
Although not readily distinguishable from the natural history of hypertensive disease, myocardial infarction (4%) was reported in large uncontrolled experience in patients with vasospastic or resistant angina pectoris (about half had concomitant treatment with beta-blockers). In a subgroup of approximately 250 patients with a diagnosis of CHF as well as angina, myocardial infarction occurred in about 6.7% of patients. Patients with angina should be observed for worsening symptoms when nifedipine therapy is begun, particularly if beta-blocker therapy is being withdrawn. Serious adverse effects have been reported with the use of immediate-release nifedipine, primarily due to the unpredictable rate and degree of blood pressure lowering. Profound hypotension, myocardial infarction, and death have been reported when immediate-release nifedipine is used to lower blood pressure acutely, especially when used in elderly patients. Due to the risks associated with the immediate-release nifedipine capsules, this dosage formulation should not be used in patients with chronic hypertension, acute hypertensive crisis, acute myocardial infarction, or in the setting of acute coronary syndrome.[29068] [42064] [31749]
Common CNS-related adverse events reported during nifedipine therapy include: headache (10—23%; due to vasodilation) and dizziness or lightheadedness (4—27%) Other CNS-related adverse events reported during nifedipine therapy include weakness (10—12%), fatigue (4—5.9%), asthenia (< 1%—4%), tremor (<= 8%), paresthesias (<= 3%), vertigo (<= 3%), anxiety (<= 1%), nervousness; mood changes (<= 2%—7%), ataxia (<=1%), libido decrease (<= 1%), depression (<= 1%), hypertonia (<=1%), hypoesthesia (<=1%), migraine (<=1%), paroniria/nightmares (<= 1%), insomnia (< 3%), sleep disturbances (<= 2%), confusion (< 1%), drowsiness (< 3%), shakiness (<= 2%), jitteriness (<= 2%), difficulties in balance (<= 2%), and paranoia (<0.5%).[42064] [29068] [31749]
Respiratory-related adverse reactions reported during nifedipine therapy include: nasal congestion (<=2%—6%), chest congestion (<= 2%), dyspnea (<= 2%—6%), cough (< 1%—6%), wheezing (6%), throat irritation (6%), epistaxis (<= 1%—3%), rhinitis (<= 3%), rales (< 1%), pharyngitis (< 1%), stridor (< 1%), upper respiratory tract infection (<= 1%), respiratory disorder (<= 1%), and sinusitis (<= 1%).[31749] [29068] [42064]
Dermatologic and allergic adverse reactions reported during administration of nifedipine include: rash (unspecified) (<= 3%), pruritus (< 3%), dermatitis (<= 2%), urticaria (<= 2%), hyperhidrosis (<= 2%), photosensitivity reaction (< 1%), petechiae (< 1%), alopecia (<=1%), and purpura (<=1%). In post-marketing experience, there have been rare reports of exfoliative dermatitis (< 0.5%) caused by nifedipine. There have also been rare reports of exfoliative or bullous skin adverse events (such as erythema multiforme, Stevens-Johnson Syndrome, and toxic epidermal necrolysis). Angioedema (< 1%), allergic reaction (< 1%), cellulitis (< 1%), facial edema (<= 1%), and anaphylactoid reactions have been reported during nifedipine therapy.[29068] [31749] [42064] Nifedipine has also been associated with acute generalized exanthematous pustulosis (AGEP). The nonfollicular, pustular, erythematous rash starts suddenly, is associated with elevated body temperature above 38 degrees C, and is distinct from pustular psoriasis, although biopsy results in each reveal spongiform subcorneal pustules. Drugs are the main cause of AGEP. A period of 2—3 weeks after an inciting drug exposure appears necessary for a first episode of AGEP. Unintentional reexposure may cause a second episode within 2 days. Clinical presentation is diverse with cutaneous lesions beyond erythema and pustules present in half of the cases. For example, bullous lesions, edema, purpura, itching, and mucosal erosions are possible. The mean duration of the pustules is 9.7 days followed by an annular desquamation, as long as the causative drug or factor is discontinued. The physiopathological mechanisms of AGEP have not been determined but the pathological criteria of edema, leukocytoclastic vasculitis, eosinophil exocytosis, and keratinocyte focal necrosis are distinctive. Pustule confluence or very small pustules may lead a clinician to make an incorrect diagnosis of TEN, of drug-induced erythroderma, or of staphylococcal scalded skin syndrome.[27736]
Gynecomastia has been reported in < 1% of patients receiving nifedipine. Breast enlargement or engorgement (< 1%) and breast pain or mastalgia (<= 1%) have also been reported.[29068] [42064] [31749]
Gingival hyperplasia (<=1%) gum disorder (< 1%), and gum hemorrhage (< 1%) have been reported with nifedipine.[29068] [42064] [31749]
Gastrointestinal-related adverse reactions reported during the use of all dosage forms of nifedipine include: nausea (2—11%), pyrosis (heartburn) (11%), diarrhea (< 3%), constipation (<= 3.3%), cramps (<= 2%), xerostomia (< 3%), dysphagia(< 1%), dyspepsia (< 3%), eructation (<= 1%), esophagitis (< 1%), flatulence (< 3%), gastrointestinal disorder (< 1%), GI bleeding (< 1%), vomiting (<= 1%), weight loss (< 1%), dysgeusia (<= 1%), abdominal pain (< 3%), gastrointestinal irritation (< 1%), gastroesophageal reflux (<= 1%), melena (<= 1%), and weight gain (<= 1%).[29068] [42064] [31749] GI obstruction (even in patients with no prior history of gastrointestinal disease, see Contraindications), tablet adherence to the gastrointestinal wall resulting in peptic ulcer, and, rarely, bezoar have been reported in association with extended-release nifedipine formulations. In some cases, hospitalization and surgical intervention have been required.[42064]
Urogenital-related adverse reactions reported during nifedipine therapy include: sexual difficulties (<= 2%), impotence (erectile dysfunction) (< 1%—3%), nocturia (< 0.5%—1%), polyuria (< 3%), increased urinary frequency (<= 3%), pelvic pain (< 1%), dysuria (<= 1%), nephrolithiasis (< 1%), urogenital disorder (< 1%), gout (<= 1%), and hematuria (<= 1%).[29068] [31749] [42064]
Musculoskeletal-related adverse reactions reported during nifedipine therapy include: muscle cramps (<= 2%—8%), inflammation (<= 2%), joint stiffness (<= 2%), arthritis with positive ANA (< 1%), myalgia (< 0.5—1%), pain (< 3%), leg pain (<= 3%), neck pain (< 1%), back pain (<= 1%), leg cramps (<= 3%), arthralgia (< 3%), joint disorder (< 1%), and myasthenia (< 1%).[29068] [42064] [31749]
Clinically significant, but usually transient, elevated hepatic enzymes have been reported rarely during nifedipine therapy. A causal relationship to nifedipine has not been established. These laboratory abnormalities have rarely been associated with clinical symptoms; cholestasis with or without jaundice has been reported. Rare instances of allergic hepatitis have also been reported.[29068] [42064] [31749]
Blurred vision (<= 2%), visual impairment (i.e., abnormal vision (<= 1%) or transient blindness at the peak of plasma level (< 0.5%)), amblyopia (< 1%), conjunctivitis (< 1%), diplopia (< 1%), eye disorder (< 1%), ocular hemorrhage (< 1%), periorbital edema (<= 1%), and abnormal lacrimation (<= 1%) have been reported during nifedipine therapy.[29068] [42064] [31749]
Tinnitus (<= 1%) has been reported during nifedipine therapy.[29068] [42064] [31749]
Hematologic changes have been reported with nifedipine therapy. Eosinophilia and lymphadenopathy have been reported in < 1% of nifedipine-treated patients. Thrombocytopenia, anemia, and leukopenia have been reported in < 0.5% of nifedipine-treated patients. Positive direct Coombs Test with/without hemolytic anemia has been reported but a causal relationship between nifedipine administration and positivity of this laboratory test, including hemolysis, could not be determined.[29068] [42064] [31749]
General effects, such as fever (<= 2%), chills (<= 2%), malaise (<= 1%), and rigors (<= 1%) have been reported during nifedipine therapy.[29068] [42064] [31749]
Nifedipine may produce hyperglycemia and may lead to loss of glucose control.[31749]
Hot flashes have been reported in <= 1% of nifedipine-treated patients, and may be related to vasodilation.[42064]
Nifedipine may cause infertility. A literature report showed a reversible reduction in the ability of human sperm obtained from a limited number of infertile people taking recommended nifedipine doses to bind to and fertilize an ovum in vitro. There are published reports of reversible infertility in people who can cause pregnancy in others taking nifedipine for hypertension. When given to rats prior to mating at doses approximately 5- and 30-times the maximum recommended human dose, nifedipine caused a reduction in fertility.[31749] [42064] [66517] [66518]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Do not use nifedipine to treat beta-blocker withdrawal; nifedipine does not reduce heart rate and gives no protection against the effects of abrupt beta-blocker withdrawal. Withdraw beta-blockers only after a gradual dose reduction.[29068][31749][42064]
Do not use immediate-release nifedipine for the treatment of essential hypertension.[29068] Guidelines also recommend avoiding use of sublingual, rapidly acting, administration of nifedipine for treatment of hypertensive urgency as the degree of blood pressure lowering cannot be anticipated and may often be too fast and larger than desired.[72366]
Worsening angina and acute myocardial infarction can develop after starting or increasing the dose of nifedipine, particularly in individuals with severe obstructive coronary artery disease.[29068][31749][42064]
Heart failure has been reported rarely after nifedipine initiation, usually in individuals receiving concomitant beta-blocker therapy. Individuals with severe aortic stenosis may be at greater risk for developing heart failure, as the unloading effect of nifedipine would be expected to be of less benefit, owing to the fixed impedance to flow across the aortic valve in these individuals.[29068] [31749] [42064] Do not administer immediate-release nifedipine within the first or second week after acute myocardial infarction. Avoid immediate-release nifedipine in individuals with acute coronary syndrome, where infarction may be imminent. In some clinical trials, subjects with acute myocardial infarction who received immediate-release nifedipine had significantly worse outcomes than those who received placebo.[29068] Some formulations of extended-release nifedipine are contraindicated in cardiogenic shock.[31749]
Careful monitoring and nifedipine dose reduction may be necessary in individuals with hepatic cirrhosis; consider initiating nifedipine therapy with the lowest dose available. Nifedipine clearance is reduced and systemic exposure is increased in individuals with hepatic cirrhosis.[31749]
There have been rare reports of gastrointestinal obstructive symptoms in individuals with known strictures in association with the ingestion of some extended-release nifedipine formulations. Risk factors for a gastrointestinal obstruction identified from postmarketing reports of some extended-release nifedipine formulations include alteration in gastrointestinal anatomy (e.g., severe GI obstruction, colon cancer, bowel resection, bariatric surgery (i.e., gastric bypass, vertical banded gastroplasty), colostomy, diverticulitis, diverticulosis, and inflammatory bowel disease), hypomotility disorders (e.g., constipation, gastroesophageal reflux disease, ileus, obesity, hypothyroidism, and diabetes mellitus) and concomitant medications (e.g., H2-histamine blockers, opioids, nonsteroidal antiinflammatory drugs, laxatives, anticholinergic agents, levothyroxine, and neuromuscular blocking agents).[42064]
Some formulations of extended-release nifedipine contain lactose. Do not use lactose-containing formulations of nifedipine in individuals with hereditary problems of galactosemia, Lapp lactase deficiency, or glucose-galactose malabsorption.[31749]
Use cautious dose selection for nifedipine in geriatric adults, usually starting at the low end of the dosage range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and concomitant disease or other drug therapy. Age appears to have a significant effect on nifedipine pharmacokinetics, unrelated to changes in renal function.[29068] [31749] [42064]
Nifedipine is compatible with breast-feeding. Nifedipine is present in breast milk in small amounts with a relative infant dose of 2.3% to 3.4%. Due to limited infant ingestion, nifedipine is not expected to cause adverse events in a breast-feeding infant, and no infant adverse effects due to nifedipine exposure in breast milk have been reported.[70364] [70365] Guidelines state nifedipine may be continued during breast-feeding.[63903] After study of a single infant-mother pair, the amount of nifedipine transferred into human milk was determined to be an insignificant fraction of the maternal dose; over 24 hours, it appears to amount to less than 5% of a pediatric therapeutic dose. Nifedipine administration did not appear to alter milk composition. The authors concluded that breast-feeding during nifedipine therapy appears to pose little risk to an infant, even a very low birth weight infant.[48512] Nifedipine has been used to treat Raynaud phenomenon of the nipple to decrease the pain associated with breast-feeding.[66515] [66516]
Use nifedipine during pregnancy only if the potential benefit justifies the potential risk. There are no adequate and well-controlled studies with nifedipine during pregnancy.[29068] [31749] [42064] Available human data have not shown nifedipine to pose a risk for major teratogenicity and experts consider nifedipine an option for treating hypertension during pregnancy.[65551] For the long-term treatment of pregnant individuals who require drug therapy, extended-release nifedipine is considered a reasonable option, and along with labetalol, is recommended above all other antihypertensive drugs. Immediate-release nifedipine may also be considered an option for urgent blood pressure control, as long as sublingual use is avoided.[63903] [72603] Nifedipine has been shown to produce teratogenic findings in rats and rabbits, including digital anomalies similar to those reported for phenytoin. Digital anomalies have been reported to occur with other members of the dihydropyridine class and are possibly a result of compromised uterine blood flow. Nifedipine use was associated with a variety of embryotoxic, placentotoxic, and fetotoxic effects, including stunted fetuses (rats, mice, rabbits), rib deformities (mice), cleft palate (mice), small placentas and underdeveloped chorionic villi (monkeys), embryonic and fetal deaths (rats, mice, rabbits), and prolonged pregnancy/decreased neonatal survival (rats; not evaluated in other species). On a mg/kg basis, all the doses associated with the teratogenic embryotoxic or fetotoxic effects in animals were higher (5 to 50 times) than the maximum recommended human dose (MRHD) of 120 mg/day. On a mg/m2 basis, some doses were higher and some were lower than the MRHD, but all are within an order of magnitude of it. The doses associated with placentotoxic effects in monkeys were equivalent to or lower than the MRHD on a mg/m2 basis.[29068] [31749] [42064]
Nifedipine may be associated with reproductive risk in people who can cause pregnancy in others. There is a literature report of reversible reduction in the ability of human sperm obtained from a limited number of infertile individuals receiving recommended doses of nifedipine to bind to and fertilize an ovum in vitro. In vivo mutagenicity studies were negative.[29068] [31749] [42064] [66517] [66518]
Mechanism of Action: Like other calcium-channel antagonists, nifedipine inhibits the influx of extracellular calcium through myocardial and vascular membrane pores, which are selective for specific ions. Serum calcium levels remain unchanged. It is believed that nifedipine inhibits this influx by physically plugging the channel. While verapamil and diltiazem exert balanced effects on calcium channels in the SA node, AV node, and vasculature, nifedipine and other members of the dihydropyridine group act predominantly on the vasculature, making these agents more potent peripheral vasodilators. The decrease in intracellular calcium inhibits the contractile processes of smooth muscle cells, causing dilation of the coronary and systemic arteries. This results in increased oxygen delivery to the myocardial tissue, decreased total peripheral resistance, decreased systemic blood pressure, and decreased afterload.
Although these drugs originally were believed to improve oxygen supply, it now appears that their effectiveness as anti-ischemic agents arises from their ability to alter the systemic balance between supply and demand. Reduced afterload and reduced myocardial wall tension lead to reduced myocardial oxygen demand, which now seems to best explain the benefit of nifedipine and other dihydropyridines in the treatment of angina. Thus, nifedipine increases myocardial oxygen supply (secondary to coronary vasodilation) and decreases myocardial oxygen demand (secondary to decreased afterload). Nifedipine appears particularly effective in treating variant angina (i.e., vasospastic angina) due to this ability to increase myocardial oxygen supply by inducing coronary vasodilation. The effectiveness of nifedipine in treating chronic stable angina, on the other hand, is related to the decrease in myocardial oxygen demand secondary to decreased afterload.
Nifedipine has no clinical effect on AV conduction, which may be due to its inhibition of phosphodiesterase. This intracellular mechanism of nifedipine actually enhances calcium inflow and counteracts its own inhibitory effects on calcium influx at the membrane surface. Also, phosphodiesterase inhibition causes additional relaxation of vascular smooth muscle. Thus, nifedipine is more potent than verapamil as a peripheral vasodilator but has negligible effects on AV nodal conduction. Negative inotropic effects rarely are noted clinically, presumably due to a reflex increase in heart rate in response to nifedipine's vasodilatory activity. Nifedipine therapy usually does not affect cardiovascular parameters in patients with normal ventricular function, but patients with decreased left ventricular function can experience an increase in ejection fraction and a decrease in left ventricular filling pressures. In general, calcium-channel blockers exert favorable effects on LVH, and do not worsen insulin resistance or exert detrimental effects on the lipid profile.
Revision Date: 10/15/2025, 01:33:00 AMNifedipine is administered orally and sublingually. It is relatively well distributed, including into breast milk. Nifedipine is protein-bound in a concentration-dependent way, ranging from 92% to 98%. Hepatic metabolism is rapid and complete, causing the formation of 2 inactive metabolites that, along with the parent drug, are excreted primarily in the urine and, to a lesser extent, the feces. Less than 5% is eliminated as unchanged drug. The elimination half-life of nifedipine is approximately 2 to 5 hours.
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4
Nifedipine is a CYP3A4 substrate, and its metabolism may be affected by CYP3A4 inhibitors or inducers.[31749]
Nifedipine is rapidly and well absorbed (90%) following an oral dose but undergoes extensive first-pass metabolism, resulting in a bioavailability of 50% to 70%. The bioavailability of the sustained-release tablet ("gastrointestinal therapeutic system [GITS]") relative to the capsule is 86% after chronic administration. The bioavailability of nifedipine does not appear to be affected by food. Co-administration of nifedipine with grapefruit juice increases the AUC and peak plasma concentrations of nifedipine by 2-fold, with no change in half-life. Bioavailability is substantially increased (up to a 100% increase) in the presence of hepatic impairment. Decreases in gastrointestinal transit time can significantly alter the absorption characteristics of the sustained-release formulation in a relatively unpredictable fashion by increasing the time available for the osmotically driven release to occur.
Sublingual administration of nifedipine liquid (expressed from regular-release capsules) to achieve rapid decreases in blood pressure, such as in the case of hypertensive urgency, has generated much controversy and confusion and is not recommended. There is little difference in the bioavailability when nifedipine capsules are swallowed whole or if they are bitten and swallowed, or bitten and held sublingually. Biting through the capsule does, however, result in slightly earlier plasma concentrations (within 10 minutes) than if capsules were swallowed intact.[29068]
Onset of hypotensive effects occurs in 30 minutes to 1 hour after administration of regular-release capsules, with peak effects occurring within 30 minutes to 2 hours. With the sustained-release tablet, serum concentrations do not peak for 6 hours, and hypotensive effects are correspondingly delayed. Duration of pharmacodynamic activity for the immediate-release preparation is approximately 8 hours. The extended-release tablet is designed to release nifedipine continuously in a zero-order process. Once-daily dosing is possible with this dosage form.
Bioavailability is substantially increased (up to a 100% increase) in the presence of hepatic impairment. Protein binding is significantly reduced in patients with hepatic dysfunction. In patients with clinically significant hepatic impairment, the half-life increases to an average of 7 hours with accumulation of plasma nifedipine concentrations.
Protein binding is significantly reduced in patients with hepatic dysfunction. Nifedipine is minimally removed by hemodialysis or hemoperfusion.
Age significantly affects the pharmacokinetics of nifedipine. In healthy subjects, the clearance of nifedipine after intravenous administration was decreased by 33% in the elderly compared to younger subjects. These changes are not due to changes in renal function.[42064]
Nifedipine is compatible with breast-feeding. Nifedipine is present in breast milk in small amounts with a relative infant dose of 2.3% to 3.4%. Due to limited infant ingestion, nifedipine is not expected to cause adverse events in a breast-feeding infant, and no infant adverse effects due to nifedipine exposure in breast milk have been reported.[70364] [70365] Guidelines state nifedipine may be continued during breast-feeding.[63903] After study of a single infant-mother pair, the amount of nifedipine transferred into human milk was determined to be an insignificant fraction of the maternal dose; over 24 hours, it appears to amount to less than 5% of a pediatric therapeutic dose. Nifedipine administration did not appear to alter milk composition. The authors concluded that breast-feeding during nifedipine therapy appears to pose little risk to an infant, even a very low birth weight infant.[48512] Nifedipine has been used to treat Raynaud phenomenon of the nipple to decrease the pain associated with breast-feeding.[66515] [66516]
Use nifedipine during pregnancy only if the potential benefit justifies the potential risk. There are no adequate and well-controlled studies with nifedipine during pregnancy.[29068] [31749] [42064] Available human data have not shown nifedipine to pose a risk for major teratogenicity and experts consider nifedipine an option for treating hypertension during pregnancy.[65551] For the long-term treatment of pregnant individuals who require drug therapy, extended-release nifedipine is considered a reasonable option, and along with labetalol, is recommended above all other antihypertensive drugs. Immediate-release nifedipine may also be considered an option for urgent blood pressure control, as long as sublingual use is avoided.[63903] [72603] Nifedipine has been shown to produce teratogenic findings in rats and rabbits, including digital anomalies similar to those reported for phenytoin. Digital anomalies have been reported to occur with other members of the dihydropyridine class and are possibly a result of compromised uterine blood flow. Nifedipine use was associated with a variety of embryotoxic, placentotoxic, and fetotoxic effects, including stunted fetuses (rats, mice, rabbits), rib deformities (mice), cleft palate (mice), small placentas and underdeveloped chorionic villi (monkeys), embryonic and fetal deaths (rats, mice, rabbits), and prolonged pregnancy/decreased neonatal survival (rats; not evaluated in other species). On a mg/kg basis, all the doses associated with the teratogenic embryotoxic or fetotoxic effects in animals were higher (5 to 50 times) than the maximum recommended human dose (MRHD) of 120 mg/day. On a mg/m2 basis, some doses were higher and some were lower than the MRHD, but all are within an order of magnitude of it. The doses associated with placentotoxic effects in monkeys were equivalent to or lower than the MRHD on a mg/m2 basis.[29068] [31749] [42064]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.