ThisiscontentfromElsevier'sDrugInformation
Nirmatrelvir; Ritonavir
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
NOTE: The National Institutes of Health (NIH) has issued a statement to provide guidance on treating nonhospitalized patients with mild to moderate coronavirus disease 2019 (COVID-19) who are at high risk of progressing to severe disease. The NIH recommends using 1 of the following therapeutics:
Before prescribing nirmatrelvir; ritonavir, the NIH recommends a careful review of the patient's concomitant medications (including over-the-counter medications and herbal supplements) to evaluate for potential drug interactions. If a significant drug interaction is identified, consider the risks and benefits of treatment. Consider expert consultation, especially for patients receiving highly specialized therapies such as antineoplastics, neuropsychiatric drugs, and certain immunosuppressants.[65314]
NOTE: Health care providers should choose an authorized therapeutic option with activity against the variants circulating in their state, territory, or US jurisdiction. Current variant frequency data are available at: https://covid.cdc.gov/covid-data-tracker/#variant-proportions.
NOTE: Nirmatrelvir; ritonavir is NOT approved or authorized for use in patients requiring hospitalization due to severe COVID-19; however, should a patient require hospitalization after starting treatment, the full 5-day treatment course may be completed per the health care providers' discretion.[67203] [69024] Additionally, the drug may be used in patients who are hospitalized for a diagnosis other than COVID-19, provided they have mild to moderate COVID-19, are at high risk for progression, and are within 5 days of symptom onset.[65314]
NOTE: Nirmatrelvir; ritonavir is NOT for use as pre-exposure or post-exposure prophylaxis to prevent COVID-19.[67203] [69024]
300 mg nirmatrelvir (two 150 mg tablets) and 100 mg ritonavir (one 100 mg tablet) with all 3 tablets taken together PO twice daily for 5 days. Initiate treatment as soon as possible after the positive test for SARS-CoV-2 and within 5 days of symptom onset. Instruct patients to complete the full 5-day treatment course and continue isolation in accordance with public health recommendations; treatment for longer than 5 consecutive days is not approved.[69024] According to the National Institutes of Health (NIH), the optimal management of immunocompromised patients who have prolonged COVID-19 symptoms and evidence of ongoing viral replication despite receiving a course of antiviral therapy is unknown. Some members of the guideline panel suggest using longer or additional courses of nirmatrelvir; ritonavir in these patients; however, there are insufficient data on the efficacy of treatment beyond 5 days or use of a second course.[65314]
300 mg nirmatrelvir (two 150 mg tablets) and 100 mg ritonavir (one 100 mg tablet) with all 3 tablets taken together PO twice daily for 5 days. Initiate treatment as soon as possible after the positive test for SARS-CoV-2 and within 5 days of symptom onset. Instruct patients to complete the full 5-day treatment course and continue isolation in accordance with public health recommendations; treatment for longer than 5 consecutive days is not authorized.[67203]
600 mg nirmatrelvir and 200 mg ritonavir per day PO.
600 mg nirmatrelvir and 200 mg ritonavir per day PO.
weighing 40 kg or more: 600 mg nirmatrelvir and 200 mg ritonavir per day PO per the Emergency Use Authorization.
weighing less than 40 kg: Safety and efficacy have not been established.
12 years and weighing 40 kg or more: 600 mg nirmatrelvir and 200 mg ritonavir per day PO per the Emergency Use Authorization.
12 years and weighing less than 40 kg: Safety and efficacy have not been established.
1 to 11 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
No dosage adjustment is needed for mild to moderate hepatic impairment (Child-Pugh A and B). Not recommended for use in patients with severe hepatic impairment (Child-Pugh C), as pharmacokinetic and safety data are unavailable.[69024]
eGFR 60 mL/minute or more: No dosage adjustment is needed.
eGFR 30 to 59 mL/minute: Give 150 mg nirmatrelvir (one 150 mg tablet) and 100 mg ritonavir (one 100 mg tablet) twice daily for 5 days.
eGFR less than 30 mL/minute: Give a single 300 mg nirmatrelvir (two 150 mg tablets) and 100 mg ritonavir (one 100 mg tablet) dose on Day 1. Then give 150 mg nirmatrelvir (one 150 mg tablet) and 100 mg ritonavir (one 100 mg tablet) once daily on Days 2 through 5.
Hemodialysis
Give a single 300 mg nirmatrelvir (two 150 mg tablets) and 100 mg ritonavir (one 100 mg tablet) dose on Day 1. Then give 150 mg nirmatrelvir (one 150 mg tablet) and 100 mg ritonavir (one 100 mg tablet) once daily on Days 2 through 5. On dialysis days, administer the dose after dialysis.[69024]
† Off-label indication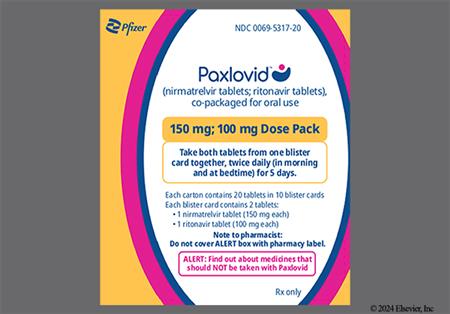

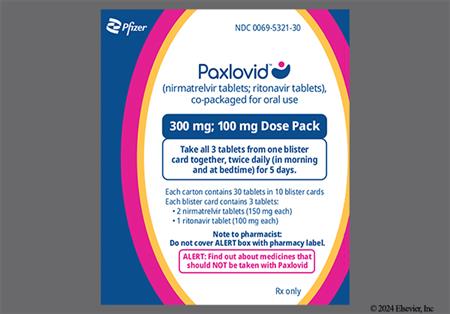
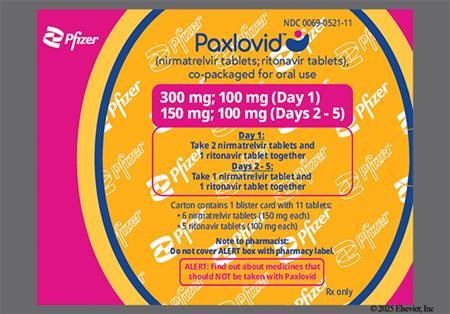
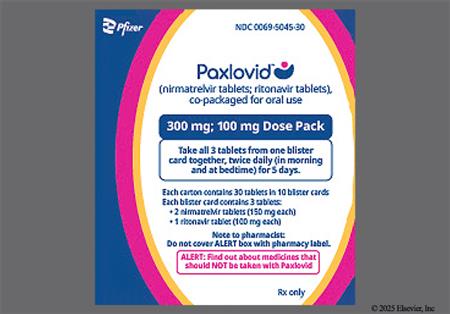
Nirmatrelvir; ritonavir is an oral antiviral medication approved by the FDA for the treatment of adults with mild to moderate coronavirus disease 2019 (COVID-19) who are at high risk for progression to severe COVID-19, including hospitalization or death. Nirmatrelvir; ritonavir is not FDA-approved for use in pediatric patients; however, it has been authorized for emergency use to treat pediatric patients (12 to 17 years of age weighing at least 40 kg) with mild to moderate COVID-19 who are at high risk for progression to severe COVID-19, including hospitalization or death. Initiate treatment as soon as possible after diagnosis of COVID-19, and within 5 days of symptom onset. Should a patient require hospitalization for severe COVID-19 after starting treatment, the full 5-day treatment course may be completed per the health care providers' discretion. The drug is NOT approved or authorized for use as a pre-exposure or post-exposure prophylaxis to prevent COVID-19. Nirmatrelvir; ritonavir has antiviral activity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), with nirmatrelvir working as a SARS-CoV-2 main protease (Mpro: also referred to as 3CLpro or nsp5 protease) inhibitor and ritonavir acting as a pharmacokinetic enhancer or booster. Nirmatrelvir MUST be given concurrently with ritonavir in order to achieve sufficient plasma concentrations; therefore, the medications are co-packaged and supplied in Dose Packs. There are three different Dose Packs available for use depending on the patient's renal function. Nirmatrelvir; ritonavir was FDA approved in 2023.[67203][69024]
The National Institutes of Health (NIH) COVID-19 treatment guidelines recommend nirmatrelvir; ritonavir as a treatment option for nonhospitalized patients with mild to moderate COVID-19 who are at high risk of progressing to severe disease; however, due to the potential for significant drug interactions with concomitant medications, this regimen may not be a safe choice for all patients. Although the drug is not approved or authorized for use in patients hospitalized due to severe COVID-19, it may be used in patients who are hospitalized for a diagnosis other than COVID-19, provided they have mild to moderate COVID-19, are at high risk for progression, and are within 5 days of symptom onset.[65314]
For storage information, see the specific product information within the How Supplied section.
NOTE: Although not FDA-approved for use in pediatric patients, nirmatrelvir; ritonavir has been authorized for emergency use to treat pediatric patients (12 to 17 years of age weighing at least 40 kg) with mild to moderate coronavirus disease (COVID-19) who are at high risk for progression to severe COVID-19, including hospitalization or death. Under the Emergency Use Authorization (EUA), health care providers are required to communicate to the patient or caregiver information consistent with the "Fact Sheet for Patients, Parents, and Caregivers" prior to the patient receiving treatment; such information includes the following:
NOTE: Under the EUA, nirmatrelvir; ritonavir may be prescribed for an individual patient by:
If any of the following apply, the state-licensed pharmacist should refer an individual patient for clinical evaluation with a physician, advanced practice registered nurse, or physician assistant licensed or authorized under state law to prescribe drugs:
To help identify appropriate candidates for treatment, the FDA has published a "Paxlovid Patient Eligibility Screening Checklist Tool for Prescribers", accessible at www.fda.gov/media/158165/download. This checklist is intended for use as an aid to support clinical decision-making, and is NOT required to prescribe nirmatrelvir; ritonavir under the EUA.[67584]
NOTE: Under the EUA, health care providers are required to report all medication errors and serious adverse events potentially related to nirmatrelvir; ritonavir therapy within 7 calendar days from the health care provider's awareness of the event.[67203]
The safety of nirmatrelvir; ritonavir was evaluated in a placebo-controlled trial of symptomatic adults with laboratory confirmed SARS-CoV-2 infection who were at high risk for progression to severe disease. A total of 1,038 patients received nirmatrelvir; ritonavir and 1,053 received a placebo. Adverse reactions were reported during treatment and through Day 28 after the last dose of treatment. Adverse reactions that occurred in the treatment group at a higher frequency than the placebo group included dysgeusia (5% vs. less than 1%, respectively) and diarrhea (3% vs. 2%).[69024]
Cases of toxic epidermal necrolysis (TEN), Stevens-Johnson Syndrome (SJS), anaphylaxis or anaphylactoid reactions, and other hypersensitivity reactions have been reported with the use of nirmatrelvir; ritonavir under the Emergency Use Authorization (EUA). If signs and symptoms of a clinically significant hypersensitivity reaction or anaphylaxis occur, immediately discontinue use of the drug and initiate appropriate medications and supportive care.[67203] [69024]
Adverse reactions experienced by recipients of nirmatrelvir; ritonavir under the Emergency Use Authorization (EUA) include abdominal pain, nausea, vomiting, headache, hypertension, and malaise. Due to the voluntary nature of these reports, neither a frequency nor a definitive causal relationship can be established.[67203] [69024]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
According to the National Institutes of Health (NIH), the optimal management of patients with immunosuppression who have prolonged COVID-19 symptoms and evidence of ongoing viral replication despite receiving a course of antiviral therapy is unknown. Some members of the guideline panel suggest using longer or additional courses of nirmatrelvir; ritonavir in these patients; however, there are insufficient data on the efficacy of treatment beyond 5 days or use of a second course. If nirmatrelvir; ritonavir is used beyond the FDA approved 5-day treatment course, health care providers are advised that the drug-drug interaction potential of ritonavir may change. When ritonavir is used for 10 days or longer, the induction potential may become clinically relevant.[65314]
The National Institutes of Health (NIH) and the American College of Obstetricians and Gynecologists (ACOG) recommend that nirmatrelvir; ritonavir be offered to pregnant and recently pregnant patients with symptoms of respiratory illness, especially since pregnancy is a risk factor for severe COVID-19. Obstetricians should be aware of potential drug-drug interactions when prescribing this medication; however, nirmatrelvir; ritonavir may be given with oseltamivir in patients with suspected or confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and influenza coinfection. Do not delay antiviral therapy while awaiting respiratory infection test results. Human data regarding the use of nirmatrelvir during pregnancy are too limited to evaluate for a drug-associated risk of major birth defects, miscarriages, or adverse maternal or fetal outcomes; however, information is available from 2 case series describing outcomes among pregnant patients with COVID-19 who received nirmatrelvir; ritonavir. The first case series included 47 patients with COVID-19 and a median gestational age of 28.4 weeks. These patients started nirmatrelvir; ritonavir after a median duration of 1 day of COVID-19 symptoms. No serious adverse events were reported during the study period in either the pregnant patients or the neonates. The other case series included 7 patients with COVID-19 symptoms for approximately 2 days at the start of treatment and a mean gestational age of 26.4 weeks. Six of the 7 patients completed the 5-day treatment course, and all 6 were fully vaccinated (4 had received a booster dose). The 6 patients reported resolution of their COVID-19 symptoms, and no fetal or neonatal adverse effects were observed during the study period. The 1 patient who discontinued treatment, did so because of dysgeusia. In animal embryo-fetal development studies, reduced fetal body weights (9% decrease) were observed in rabbits after maternal administration of nirmatrelvir doses resulting in systemic exposures 11-times higher than clinical exposures at the authorized human dose. No other adverse developmental outcomes were observed in animal reproduction studies with nirmatrelvir at systemic exposures greater than or equal to 3-times higher than clinical exposures at the authorized human dose. Published observational studies on ritonavir use in pregnant patients have not identified an increased risk for major birth defects [i.e., 2.4% (95% CI: 1.9 to 2.9) after first-trimester exposure vs. 2.7% background birth defect rate]; however, published studies with ritonavir are insufficient to identify a drug-associated risk of miscarriages. When evaluating use of nirmatrelvir; ritonavir in pregnant patients, consider that untreated COVID-19 in pregnancy is associated with adverse maternal and fetal outcomes (i.e., preeclampsia, eclampsia, preterm birth, premature rupture of membranes, venous thromboembolic disease, fetal death).[65314] [67203] [69024] [70419]
Prior to and during treatment with nirmatrelvir; ritonavir, consider that coadministration with certain medications (including over-the-counter medications and herbal supplements) may result in significant drug interactions, causing potentially severe, life-threatening, or fatal events. Review all the patient's medications, and determine if the concomitant medications require a dose adjustment, interruption, or additional monitoring. Nirmatrelvir; ritonavir is contraindicated for use with medications primarily metabolized by CYP3A and for which elevated concentrations are associated with serious or life-threatening reactions. It is also contraindicated for use with strong CYP3A inducers where significantly reduced nirmatrelvir or ritonavir concentrations may be associated with loss of virologic response or possible resistance.[67203] [69024] If a significant drug interaction is identified, consider the risks and benefits of treatment. Consider expert consultation, especially for patients receiving highly specialized therapies such as antineoplastics, neuropsychiatric drugs, and certain immunosuppressants. Potential management strategies to facilitate the use of nirmatrelvir; ritonavir include (depending on the magnitude and significance of the interaction): dose adjustment of the concomitant medication; use of an alternative concomitant medication; increased monitoring for potential adverse reactions; temporarily withholding the concomitant medication. These strategies should be considered during the 5-day treatment and for at least 3 to 5 days after the end of therapy (potentially longer for concomitant medications with long half-lives). In settings where these strategies are not feasible, consider using an alternative COVID-19 therapeutic. Health care providers are advised NOT to adjust the dose of nirmatrelvir; ritonavir to avoid or mitigate drug interactions.[65314]
Caution is advised when administering nirmatrelvir; ritonavir to patients with uncontrolled or undiagnosed human immunodeficiency virus (HIV) infection. There is a potential risk that administering nirmatrelvir; ritonavir to these patients may result in the development of resistance to HIV protease inhibitors. If a patient is receiving an antiviral regimen that contains either ritonavir or cobicistat, the treatment regimen should continue as indicated while nirmatrelvir; ritonavir is administered concurrently; no dosage adjustments are required.[67203] [69024]
The National Institutes of Health (NIH) states that nirmatrelvir; ritonavir should be offered to lactating patients who qualify for therapy, and that breast-feeding can continue without interruption.[65314] Both nirmatrelvir and ritonavir are present in human milk, as identified in a clinical study involving 8 healthy lactating patients (at least 12 weeks postpartum) who received three oral doses of 300 mg nirmatrelvir; 100 mg ritonavir every 12 hours (steady state dosing). In this study, the mean daily concentration of nirmatrelvir and ritonavir recovered in breast milk was 0.752 mg and 0.027 mg, respectively, representing 0.13% and 0.014% of the corresponding maternal daily dose. Assuming an average breast milk consumption of 150 mL/kg/day, the estimated daily infant dose was 0.16 mg/kg/day of nirmatrelvir (1.8% maternal dose) and 0.006 mg/kg/day of ritonavir (0.2% maternal dose). There are no data available regarding the effects of the drug on the breast-fed infant or on milk production. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, the potential for viral transmission to SARS-CoV-2-negative infants, and the risk of an untreated or inadequately treated condition. Advise lactating mothers to follow practices according to clinical guidelines to avoid exposing the infant to COVID-19. If a breast-feeding infant experiences an adverse effect related to a maternally administered drug, health care providers are encouraged to report the adverse effect to the FDA.[69024]
Use nirmatrelvir; ritonavir with caution in patients with renal impairment, including those with renal failure. Increased nirmatrelvir exposure may occur in patients with reduced renal function, which may increase the risk of adverse reactions. Dosage adjustments are recommended for patients with moderate (eGFR 30 to 59 mL/minute) or severe (GFR less than 30 mL/minute) renal impairment, including those requiring hemodialysis. Counsel patients regarding renal dosing instructions and monitor for adverse reactions as appropriate.[69024] According to the National Institutes of Health (NIH) COVID-19 treatment guidelines, there is no need to check renal function prior to prescribing nirmatrelvir; ritonavir unless the patient is suspected to have moderate or severe renal impairment (i.e., those with an estimated eGFR less than 60 mL/minute). For these patients, health care providers may consider checking the renal function. If renal dysfunction is identified, recommended dose reductions should be followed.[65314]
Caution is advised when administering nirmatrelvir; ritonavir to patients with pre-existing hepatic disease, as elevated hepatic enzymes, clinical hepatitis, and jaundice have occurred with ritonavir. Avoid use in patients with severe hepatic impairment (Child-Pugh class C) or hepatic failure due to lack of pharmacokinetic and safety data in this population and the potential for increased risk of adverse effects.[67203] [69024]
Nirmatrelvir; ritonavir is an oral antiviral medication with activity against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Ritonavir is an HIV-1 protease inhibitor and a CYP3A inhibitor. Ritonavir does not have antiviral activity against SARS-CoV-2, but instead is used as a pharmacokinetic enhancer to increase plasma concentrations of nirmatrelvir. Nirmatrelvir is a peptidomimetic inhibitor of the SARS-CoV-2 main protease (Mpro), also referred to as 3C-like protease (3CLpro) or nsp5 protease. By binding directly to the SARS-CoV-2 Mpro active site, nirmatrelvir renders the virus incapable of processing polyprotein precursors, thereby preventing viral replication.
Pharmacodynamics
In a biochemical assay, nirmatrelvir inhibited the activity of recombinant SARS-CoV-2 Mpro with a half-maximal inhibitory concentration (IC50) value of 19.2 nanomolar (nM). The 50% effective concentration (EC50) and 90% effective concentration (EC90) against SARS-CoV-2 in differentiated normal human bronchial epithelial cells after 3 days of drug exposure were 62 nM and 181 nM, respectively. The antiviral activity of nirmatrelvir against the Omicron subvariants BA.2, BA.2.12.1, BA.4, BA.4.6, BA.5, BF.7, BQ.1, BQ.1.11, XBB.1.5, EG.5, and JN.1 was assessed in the presence of a P-glycoprotein inhibitor. Nirmatrelvir had a median EC50 value of 88 nM (range: 39 to 146 nM) against the Omicron subvariants, reflecting a fold-change of 1.8 or less compared to the USA-WA1/2022 isolate. Additionally, the antiviral activity of nirmatrelvir against the SARS-CoV-2 Alpha, Beta, Gamma, Delta, Lambda, Mu, and Omicron BA.1 variants were assessed. Nirmatrelvir had a median EC50 value of 25 nM (range: 16 to 141 nM). The Beta (B.1.351) variant was the least susceptible tested with an approximate 3.7-fold reduced susceptibility relative to the USA-WA1/2020 isolate. The other variants had EC50 value fold-changes of 1.1 or less.
Resistance
SARS-CoV-2 Mpro residues potentially associated with nirmatrelvir resistance have been identified using a variety of methods.
In the EPIC-HR/SR clinical trials, the following treatment-emergent substitutions in SARS-CoV-2 Mpro were observed in nirmatrelvir; ritonavir-treated subjects: T98I/R/del (n = 4), E166V (n = 3), and W207L/R/del (n = 4). In biochemical assays, the T98I and W207L/R substitutions did not affect nirmatrelvir activity, whereas the E166V substitution reduced nirmatrelvir activity 187- to 7,700-fold. Within the Mpro cleavage sites, the following nirmatrelvir; ritonavir treatment-emergent substitutions were observed: A5328S/V (n = 7) and S6799A/P/Y (n = 4). These cleavage site substitutions were not associated with the concurrence of any specific Mpro substitutions. In a cell culture assay, the A5328S/V and S6799A substitutions did not affect nirmatrelvir activity. None of these substitutions in Mpro gene or cleavage regions occurred in nirmatrelvir; ritonavir-treated subjects who also experienced hospitalization. Thus, the clinical significance is unknown.
Cross-resistance is not expected between nirmatrelvir and remdesivir, molnupiravir, or anti-SARS-CoV-2 monoclonal antibodies.
Post-treatment increases in SARS-CoV-2 RNA shedding levels (i.e., viral RNA rebound) in nasopharyngeal samples have been observed on Day 10 and Day 14 in a subset of nirmatrelvir; ritonavir-treated patients and placebo recipients, irrespective of COVID-19 symptoms. In the EPIC-HR study, 59 nirmatrelvir; ritonavir recipients with available viral sequence data were identified as having post-treatment viral RNA rebound. Of these 59 subjects, treatment-emergent substitutions in Mpro potentially reducing nirmatrelvir activity were detected in 2 subjects (3%), including E166V and T304I. By Day 14, both subjects had viral RNA shedding less than the lower limit of quantification. Post-treatment viral rebound was not associated with the primary clinical outcome of COVID-19 related hospitalization or death from any cause through Day 28 after the single 5-days course of nirmatrelvir; ritonavir. The clinical relevance of post-treatment increases in viral RNA is unknown.[67203][69024]
Revision Date: 10/21/2025, 01:33:00 AMNirmatrelvir; ritonavir is administered orally. Once in systemic circulation, 69% of nirmatrelvir and approximately 99% of ritonavir is bound to human plasma proteins. The mean apparent volume of distribution during the terminal phase for nirmatrelvir and ritonavir are 104.7 L and 112.4 L, respectively. Nirmatrelvir has a blood-to-plasma ratio of 0.6 and the ratio for ritonavir is 0.14. Nirmatrelvir is a CYP3A4 substrate, but the metabolic clearance is minimal when dosed with ritonavir. Ritonavir is primarily metabolized by CYP3A4, with minor contributions from CYP2D6. Nirmatrelvir is primarily eliminated via the kidneys, with a mean half-life of 6.05 hours. Hepatic metabolism is the major route of elimination for ritonavir, which has a mean half-life of 6.15 hours. The percentage of nirmatrelvir drug-related material excreted in the urine and feces is 49.6% and 35.3%, respectively. The percentage of ritonavir drug-related material excreted in the feces and urine is 86.4% and 11.3%, respectively.[67203][69024]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A, CYP2D6 P-glycoprotein (P-gp), Organic anion transporting polypeptide (OATP1B1)
Nirmatrelvir is a substrate for CYP3A4 and the drug transporter P-gp. Nirmatrelvir has the potential to reversibly and time-dependently inhibit CYP3A4, and is also an inhibitor of P-gp and OATP1B1. Nirmatrelvir is also an inducer of CYP2B6, CYP2C8, CYP2C9, and CYP3A4, but there is minimal risk for pharmacokinetic interactions arising from induction of these enzymes at the proposed therapeutic dose. Ritonavir is a substrate for and inhibitor of CYP3A (major) and CYP2D6 (minor). Ritonavir is also a substrate and inhibitor of P-glycoprotein (P-gp).[28380][34557][65314][69024] Additionally, ritonavir appears to induce CYP3A, CYP1A2, CYP2C9, CYP2C19, and CYP2B6.[67203][69024]
The pharmacokinetics of nirmatrelvir; ritonavir were similar in healthy subjects and in patients with mild to moderate COVID-19. After administration of nirmatrelvir, ritonavir (300 mg/100 mg) twice daily to patients with mild to moderate COVID-19, the predicted Day 5 maximum plasma concentration (Cmax), systemic exposure (AUC), and trough concentration (Cmin) of nirmatrelvir were 3.29 mcg/mL, 28.3 mcg x hour/mL, and 1.4 mcg/mL, respectively. Upon administration of a single nirmatrelvir; ritonavir (300 mg/100 mg) dose to healthy subjects, the time to reach peak concentration (Tmax) was 3 hours for nirmatrelvir and approximately 4 hours for ritonavir. Nirmatrelvir AUC increased in a less than dose proportional manner over a single dose range of 250 to 750 mg and multiple dose range of 75 to 500 mg, when administered with ritonavir. Nirmatrelvir steady state was achieved on Day 2 after administration of the recommended dose and the mean accumulation ratio was approximately 2-fold. No clinically significant differences in the pharmacokinetics of nirmatrelvir were observed after administration with a high fat meal (800 to 1,000 calories; 50% fat) in healthy subjects.[67203][69024]
A single 100 mg/100 mg dose of nirmatrelvir; ritonavir in patients with moderate hepatic impairment (Child-Pugh B) resulted in nirmatrelvir exposures that were similar to those observed in subjects with normal hepatic function. The pharmacokinetics of nirmatrelvir; ritonavir have not been evaluated in patients with severe hepatic impairment (Child-Pugh C).[67203][69024]
The pharmacokinetics of nirmatrelvir were compared in healthy subjects and patients with mild, moderate, and severe renal impairment after administration of a single 100 mg/100 mg nirmatrelvir; ritonavir dose. Compared to the healthy controls with no renal impairment, the Cmax and AUC of nirmatrelvir in patients with mild impairment were 30% and 24% higher, in patients with moderate impairment they were 38% and 87% higher, and in patients with severe impairment they were 48% and 204% higher, respectively. In another study, the pharmacokinetics of nirmatrelvir were evaluated in patients with severe renal impairment (eGFR less than 30 mL/minute) who were administered a single 300 mg nirmatrelvir and 100 mg ritonavir dose on Day 1 followed by 150 mg nirmatrelvir and 100 mg ritonavir once daily on Days 2 through 5. Nirmatrelvir exposures (AUC and Cmax) on Day 1 and at steady-state were comparable to those observed in subjects with normal renal function receiving 300 mg nirmatrelvir and 100 mg ritonavir twice daily for 5 days. Among those patients who received intermittent hemodialysis, approximately 6.9% of the nirmatrelvir dose was cleared through dialysis during a 4-hour session. The hemodialysis clearance was 1.83 L/hour.[69024]
The pharmacokinetics of nirmatrelvir; ritonavir in patients younger than 18 years have not been evaluated. Using a population PK model, the authorized dosing regimen is expected to result in comparable steady-state plasma exposure of nirmatrelvir in patients 12 years and older who weigh at least 40 kg to those observed in adults after adjusting for body weight.[67203]
There were no clinically significant differences in the pharmacokinetics of nirmatrelvir based on age (range: 18 to 86 years).[69024]
There were no clinically significant differences in the pharmacokinetics of nirmatrelvir based on gender.[69024]
There were no clinically significant differences in the pharmacokinetics of nirmatrelvir based on ethnicity.[69024]
The National Institutes of Health (NIH) and the American College of Obstetricians and Gynecologists (ACOG) recommend that nirmatrelvir; ritonavir be offered to pregnant and recently pregnant patients with symptoms of respiratory illness, especially since pregnancy is a risk factor for severe COVID-19. Obstetricians should be aware of potential drug-drug interactions when prescribing this medication; however, nirmatrelvir; ritonavir may be given with oseltamivir in patients with suspected or confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and influenza coinfection. Do not delay antiviral therapy while awaiting respiratory infection test results. Human data regarding the use of nirmatrelvir during pregnancy are too limited to evaluate for a drug-associated risk of major birth defects, miscarriages, or adverse maternal or fetal outcomes; however, information is available from 2 case series describing outcomes among pregnant patients with COVID-19 who received nirmatrelvir; ritonavir. The first case series included 47 patients with COVID-19 and a median gestational age of 28.4 weeks. These patients started nirmatrelvir; ritonavir after a median duration of 1 day of COVID-19 symptoms. No serious adverse events were reported during the study period in either the pregnant patients or the neonates. The other case series included 7 patients with COVID-19 symptoms for approximately 2 days at the start of treatment and a mean gestational age of 26.4 weeks. Six of the 7 patients completed the 5-day treatment course, and all 6 were fully vaccinated (4 had received a booster dose). The 6 patients reported resolution of their COVID-19 symptoms, and no fetal or neonatal adverse effects were observed during the study period. The 1 patient who discontinued treatment, did so because of dysgeusia. In animal embryo-fetal development studies, reduced fetal body weights (9% decrease) were observed in rabbits after maternal administration of nirmatrelvir doses resulting in systemic exposures 11-times higher than clinical exposures at the authorized human dose. No other adverse developmental outcomes were observed in animal reproduction studies with nirmatrelvir at systemic exposures greater than or equal to 3-times higher than clinical exposures at the authorized human dose. Published observational studies on ritonavir use in pregnant patients have not identified an increased risk for major birth defects [i.e., 2.4% (95% CI: 1.9 to 2.9) after first-trimester exposure vs. 2.7% background birth defect rate]; however, published studies with ritonavir are insufficient to identify a drug-associated risk of miscarriages. When evaluating use of nirmatrelvir; ritonavir in pregnant patients, consider that untreated COVID-19 in pregnancy is associated with adverse maternal and fetal outcomes (i.e., preeclampsia, eclampsia, preterm birth, premature rupture of membranes, venous thromboembolic disease, fetal death).[65314] [67203] [69024] [70419]
The National Institutes of Health (NIH) states that nirmatrelvir; ritonavir should be offered to lactating patients who qualify for therapy, and that breast-feeding can continue without interruption.[65314] Both nirmatrelvir and ritonavir are present in human milk, as identified in a clinical study involving 8 healthy lactating patients (at least 12 weeks postpartum) who received three oral doses of 300 mg nirmatrelvir; 100 mg ritonavir every 12 hours (steady state dosing). In this study, the mean daily concentration of nirmatrelvir and ritonavir recovered in breast milk was 0.752 mg and 0.027 mg, respectively, representing 0.13% and 0.014% of the corresponding maternal daily dose. Assuming an average breast milk consumption of 150 mL/kg/day, the estimated daily infant dose was 0.16 mg/kg/day of nirmatrelvir (1.8% maternal dose) and 0.006 mg/kg/day of ritonavir (0.2% maternal dose). There are no data available regarding the effects of the drug on the breast-fed infant or on milk production. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, the potential for viral transmission to SARS-CoV-2-negative infants, and the risk of an untreated or inadequately treated condition. Advise lactating mothers to follow practices according to clinical guidelines to avoid exposing the infant to COVID-19. If a breast-feeding infant experiences an adverse effect related to a maternally administered drug, health care providers are encouraged to report the adverse effect to the FDA.[69024]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.