ThisiscontentfromElsevier'sDrugInformation
Pembrolizumab
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
NOTE: Use of a PD-1 or PDL1 blocking antibody such as pembrolizumab with a thalidomide analogue plus dexamethasone is not recommended in patients with multiple myeloma unless it is being evaluated in a controlled clinical trial.[57889] Two clinical trials (KEYNOTE-183 and KEYNOTE-185) were halted due to an increased risk of death in patients who received pembrolizumab and dexamethasone in combination with an immunomodulatory agent (lenalidomide or pomalidomide) for the treatment of multiple myeloma (off-label use).[62286]
NOTE: The FDA has designated pembrolizumab as an orphan drug for the treatment of stage IIB-IV melanoma.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] The primary endpoint of median progression-free survival (PFS), evaluated by independent central review, was significantly improved with pembrolizumab 2 mg/kg IV (n = 180) every 3 weeks (2.9 months) and pembrolizumab 10 mg/kg IV (n = 181) every 3 weeks (2.9 months) compared with investigator-choice chemotherapy (ICC) (n = 179; 2.7 months) in patients with unresectable stage III or IV melanoma who had disease progression following ipilimumab and had received prior treatment with a BRAF- and/or MEK-inhibitor (if BRAF V600 mutant-positive) in a second interim analysis of a multinational, randomized, phase 2 trial (the KEYNOTE-002 trial). ICC consisted of carboplatin/paclitaxel (n = 42) or single-agent carboplatin (n = 13), paclitaxel (n = 28), dacarbazine (n = 45), or temozolomide (n = 43). Ipilimumab-refractory melanoma was defined as progression within 24 weeks after at least 2 doses of ipilimumab. At a median follow-up time of 10 months, the 6-month PFS rates were 34% and 38% in the pembrolizumab 2 mg/kg and 10 mg/kg arms, respectively, compared with 16% in the ICC arm; additionally, the 9-month PFS rates were 24% and 29% compared with 8%, respectively. Treatment crossover to pembrolizumab occurred in 48% of patients who received ICC. Overall survival (OS) data are not yet mature.[59863]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease recurrence or for up to 12 months in patients without disease recurrence. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] The investigator-assessed median relapse-free survival (RFS; HR 0.62) and distant metastases-free survival (DMFS; HR 0.59) times were not reached in either arm after a median follow-up time of 39.4 months in patients with previously untreated, stage IIB or IIC melanoma after complete resection who received up to 1 year of adjuvant pembrolizumab or placebo in interim analyses of a randomized, placebo-controlled, phase 3 trial (KEYNOTE-716). The DMFS at 36 months was 84.4% with adjuvant pembrolizumab compared with 74.7% with placebo; the 36-month RFS rate was 76.2% versus 63.4%, respectively.[67512] [69434] In the 5-year analysis of another randomized, double-blind, phase 3 trial (EORTC 1325/KEYNOTE 054), up to 1 year of adjuvant therapy with pembrolizumab significantly improved the 5-year rate of RFS (55.4% vs. 38.3%) and DMFS (60.6% vs. 44.5%) compared with placebo in patients with resected high-risk stage III cutaneous melanoma. Of note, 70% of patients in the placebo arm with locoregional recurrence crossed over to an anti-PD-1/PD-L1-based treatment and 23% of patients in the pembrolizumab arm were rechallenged with pembrolizumab.[67178] [69435]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease recurrence or for up to 12 months in patients without disease recurrence. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] The investigator-assessed median relapse-free survival (RFS; HR 0.62) and distant metastases-free survival (DMFS; HR 0.59) times were not reached in either arm after a median follow-up time of 39.4 months in patients with previously untreated, stage IIB or IIC melanoma after complete resection who received up to 1 year of adjuvant pembrolizumab or placebo in interim analyses of a randomized, placebo-controlled, phase 3 trial (KEYNOTE-716). The DMFS at 36 months was 84.4% with adjuvant pembrolizumab compared with 74.7% with placebo; the 36-month RFS rate was 76.2% versus 63.4%, respectively. Pediatric patients aged 12 years and older were eligible for study enrollment; 2 pediatric patients were randomized (1 patient in the pembrolizumab arm and 1 patient in the placebo arm) in this trial.[67512] [69434] Efficacy for pediatric patients with stage III melanoma has been extrapolated from clinical trial data in adults with melanoma.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks for 12 weeks as neoadjuvant treatment or until disease progression that precludes definitive surgery or unacceptable toxicity, in combination with cisplatin (75 mg/m2 IV on day 1) and pemetrexed (500 mg/m2 IV on day 1) every 3 weeks for up to 4 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Within 4 to 12 weeks after surgery, resume adjuvant pembrolizumab 200 mg IV every 3 weeks OR 400 mg IV every 6 weeks as monotherapy for 39 weeks or until disease recurrence or unacceptable toxicity. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, double-blind clinical trial (KEYNOTE-671), perioperative treatment with pembrolizumab plus neoadjuvant platinum-based chemotherapy significantly improved the median overall survival (not reached vs. 52.4 months) and median event-free survival (not reached vs. 17 months) compared with perioperative placebo plus platinum-based chemotherapy in patients with previously untreated and resectable stage II, IIIA, or IIIB (N2) NSCLC. Platinum-based chemotherapy included cisplatin plus gemcitabine for patients with squamous histology and cisplatin plus pemetrexed for patients with nonsquamous histology.[69675] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks for 12 weeks as neoadjuvant treatment or until disease progression that precludes definitive surgery or unacceptable toxicity, in combination with cisplatin (75 mg/m2 IV on day 1) and gemcitabine (1,000 mg/m2 IV on days 1 and 8) every 3 weeks for up to 4 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Within 4 to 12 weeks after surgery, resume adjuvant pembrolizumab 200 mg IV every 3 weeks OR 400 mg IV every 6 weeks as monotherapy for 39 weeks or until disease recurrence or unacceptable toxicity. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, double-blind clinical trial (KEYNOTE-671), perioperative treatment with pembrolizumab plus neoadjuvant platinum-based chemotherapy significantly improved the median overall survival (not reached vs. 52.4 months) and median event-free survival (not reached vs. 17 months) compared with perioperative placebo plus platinum-based chemotherapy in patients with previously untreated and resectable stage II, IIIA, or IIIB (N2) NSCLC. Platinum-based chemotherapy included cisplatin plus gemcitabine for patients with squamous histology and cisplatin plus pemetrexed for patients with nonsquamous histology.[69675] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease recurrence, unacceptable toxicity, or for up to 12 months in patients without disease recurrence. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, triple-blind, phase 3 clinical trial (KEYNOTE-091), adjuvant treatment with pembrolizumab after resection and 4 cycles of platinum-based chemotherapy significantly improved disease-free survival (DFS) compared with placebo in the subgroup of patients with stage 1B, II, or IIIA NSCLC which comprised 86% of the study population (58.7 months vs. 34.9 months); in the 14% of patients who did not receive adjuvant chemotherapy, the impact of adjuvant pembrolizumab on DFS was not statistically significant. Overall survival results were not mature.[57889] [68574]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, open-label clinical trial (KEYNOTE-042; n = 1,274), treatment of PD-L1 positive (1% or more), EGFR and ALK-negative, stage III NSCLC in patients who were not candidates for surgical resection or definitive chemoradiation or metastatic NSCLC with pembrolizumab significantly improved median overall survival compared with investigator's choice of platinum-based chemotherapy (16.7 vs. 12.1 months); survival was higher in patients with TPS of 50% or more (20 months). Progression-free survival (PFS) was not significantly improved in patients with TPS of 1% or more (5.4 months vs. 6.5 months) or 50% or more (7.1 vs. 6.4 months). In patients with TPS 1% or more, the objective response rate was 27% in each arm; however, more prolonged responses were seen in patients who received pembrolizumab. A response of 12 months or longer was seen in 47% of responding patients treated with pembrolizumab compared with 16% of those who received chemotherapy; a response duration of 18 months or more was seen in 26% versus 6% of patients, respectively. Another clinical trial with a similar design to KEYNOTE-042 but only enrolling patients with TPS of 50% or more (KEYNOTE-024) was stopped early by an independent data and safety monitoring committee after demonstrating superiority of pembrolizumab compared with platinum-based chemotherapy with regard to PFS (10.3 vs. 6 months), despite a large percentage of patients (66%) in the chemotherapy arm crossing over to receive second-line therapy with pembrolizumab.[61268] [57889] After 5 years of follow-up, treatment with pembrolizumab significantly improved median overall survival (OS) in KEYNOTE-024 compared with platinum-based chemotherapy (26.3 months vs. 13.4 months); the estimated 5-year OS rate was 31.9% versus 16.3%, respectively.[66632]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with pemetrexed (500 mg/m2 IV) on day 1 plus either carboplatin (AUC 5 IV) or cisplatin (75 mg/m2 IV) on day 1 repeated every 21 days for 4 cycles. Administer pembrolizumab prior to pemetrexed and chemotherapy when given on the same day. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Following completion of platinum-based therapy, pembrolizumab may be continued as maintenance therapy for up to 24 months, either alone or in combination with pemetrexed, until disease progression or unacceptable toxicity. In a multicenter double-blind clinical trial (KEYNOTE-189), patients with previously untreated metastatic, EGFR- and ALK-negative, nonsquamous NSCLC, regardless of PD-L1 status, were randomized to treatment with pemetrexed plus either cisplatin or carboplatin, in combination with either pembrolizumab (n = 410) or placebo (n = 206). After a median follow-up of 31 months, the median overall survival (22 months vs. 10.6 months), progression-free survival (9 months vs. 4.9 months), and overall response rate (48.3% vs. 19.9%) were significantly improved in the pembrolizumab arm. The median duration of response was 12.5 months for patients who received pembrolizumab plus pemetrexed/platinum chemotherapy compared with 7.1 months in those receiving placebo plus pemetrexed/platinum chemotherapy.[57889] [28376] [66703] [67147] [70417]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with carboplatin (AUC 6 IV on day 1) plus either paclitaxel (200 mg/m2 IV on day 1) or nab-paclitaxel (100 mg/m2 on days 1, 8, and 15) repeated every 3 weeks for 4 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, double-blind clinical trial (KEYNOTE-407), treatment with pembrolizumab plus carboplatin and either paclitaxel or nab-paclitaxel (n = 278) significantly improved median overall survival (17.1 months vs. 11.6 months) and progression-free survival (6.4 months vs. 4.8 months) compared with placebo plus carboplatin and paclitaxel/nab-paclitaxel (n = 281) in patients with metastatic squamous NSCLC. The objective response rate was also significantly improved in the pembrolizumab arm (58% vs. 35%), for a median duration of 7.2 months and 4.9 months, respectively.[57889] [66530]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] In a multicenter, randomized, open-label clinical trial, treatment with pembrolizumab (n = 346) improved overall survival (OS) and progression-free survival (PFS) compared with docetaxel (n = 343) in patients with PD-L1-expressing (TPS, 1% or greater), platinum-resistant, metastatic NSCLC. In the subgroup of patients with TPS greater than or equal to 1%, OS in patients treated with pembrolizumab was 10.4 months compared with 8.5 months in those who received docetaxel and the objective response rate (ORR) was 18% versus 9%, respectively; PFS was not significantly different. Results were stronger in patients with TPS greater than or equal to 50%, with median OS of 14.9 months in the pembrolizumab arm versus 8.2 months in the docetaxel arm, and ORR 30% compared with 8%, respectively; the improvement in PFS was small but statistically significant in this subgroup (5.2 months vs. 4.1 months).[61369] [57889]
NOTE: The FDA has designated pembrolizumab as an orphan drug for the treatment of Merkel cell carcinoma.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] The overall response rate (ORR) was 58% (complete response (CR) rate, 30%) in 50 patients with advanced Merkel cell carcinoma who received pembrolizumab in a multicenter, phase 2 (KEYNOTE-017) trial. At a median follow-up of 31.8 (range, 0.4 to 56.9) months, the median progression-free survival time was 16.8 months and the median duration of response and overall survival time were not reached.[69693] In another multicenter, phase 2 (KEYNOTE-913) trial, the ORR was 49% (CR rate, 16%) in 55 patients with advanced Merkel cell carcinoma who received pembrolizumab. In these 2 trials, eligible patients (median age, 71 years; range, 46 to 91 years) were not amenable to definitive surgery or radiation therapy and had not previously received systemic therapy; 14% of patients had stage IIIB disease and 86% of patients had stage IV disease.[57889]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Efficacy for pediatric patients has been extrapolated from results from clinical trials in adult Merkel cell carcinoma patients.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with carboplatin (AUC 5 IV on day 1) and fluorouracil (1,000 mg/m2 per day continuous IV infusion on days 1 to 4) repeated every 3 weeks for 6 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue pembrolizumab for severe or life-threatening infusion-related reactions. Treatment with pembrolizumab plus fluorouracil and either carboplatin or cisplatin significantly improved median overall survival (13 months vs. 10.7 months) compared with cetuximab plus fluorouracil and carboplatin/cisplatin in patients with previously untreated metastatic or unresectable, recurrent squamous cell head and neck cancer in a randomized, open-label trial (KEYNOTE-048); hazard ratios were similar in the intent-to-treat population (0.72), in patients with PD-L1 CPS of 1 or more (0.65), and in patients with CPS of 20 or more (0.6). Progression-free survival (PFS) was not significantly different between arms (4.9 months vs. 5.1 months). The objective response rate was 36% in each arm for a median duration of 6.7 months in the pembrolizumab arm and 4.3 months in the cetuximab arm; there were more complete responses in patients who received pembrolizumab (6% vs. 3%), respectively.[57889] [64769]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with cisplatin (100 mg/m2 IV on day 1) and fluorouracil (1,000 mg/m2 per day continuous IV infusion on days 1 to 4) repeated every 3 weeks for 6 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue pembrolizumab for severe or life-threatening infusion-related reactions. Treatment with pembrolizumab plus fluorouracil and either carboplatin or cisplatin significantly improved median overall survival (13 months vs. 10.7 months) compared with cetuximab plus fluorouracil and carboplatin/cisplatin in patients with previously untreated metastatic or unresectable, recurrent squamous cell head and neck cancer in a randomized, open-label trial (KEYNOTE-048); hazard ratios were similar in the intent-to-treat population (0.72), in patients with PD-L1 CPS of 1 or more (0.65), and in patients with CPS of 20 or more (0.6). Progression-free survival (PFS) was not significantly different between arms (4.9 months vs. 5.1 months). The objective response rate was 36% in each arm for a median duration of 6.7 months in the pembrolizumab arm and 4.3 months in the cetuximab arm; there were more complete responses in patients who received pembrolizumab (6% vs. 3%), respectively.[57889] [64769]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Treatment with pembrolizumab monotherapy significantly improved median overall survival (12.3 months vs. 10.3 months) in patients with metastatic or unresectable, recurrent squamous cell head and neck cancer and CPS of 1 or more compared with cetuximab plus fluorouracil and carboplatin/cisplatin in a randomized, open-label clinical trial (KEYNOTE-048); in patients with CPS of 20 or more, median overall survival was 14.9 months versus 10.7 months, respectively. At the time of the interim and final analyses, there was no significant difference in OS for the overall population. Median progression-free survival (PFS) was not significantly different between treatment arms (3.2 months vs. 5 months). The objective response rate was 19% in patients who received pembrolizumab compared with 35% in the cetuximab arm, for a median duration of 20.9 months versus 4.5 months, respectively; complete responses occurred in 5% and 3% of patients, respectively.[57889] [64769]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. After a median follow-up of 8.9 months, treatment with pembrolizumab resulted in an objective response rate (ORR) of 16% (95% CI, 11% to 22%), with a complete response rate of 5% in a multicenter, non-randomized, open-label clinical trial of patients with platinum-resistant, recurrent or metastatic head and neck squamous cell carcinoma (n = 174). The median duration of response was not reached, but ranged from 2.4 months to more than 27.7 months; 23 of 28 responses lasted 6 months or longer. The ORR and duration of response were similar regardless of dosage regimen (10 mg/kg every 2 weeks or 200 mg every 3 weeks) or HPV status.[57889]
200 mg IV every 3 weeks for 2 doses prior to surgery (6 weeks), or until unacceptable toxicity or disease progression that precludes surgery occurs first; alternatively, 6 weeks prior to surgery administer 1 dose of pembrolizumab 400 mg IV. After surgery, administer pembrolizumab (200 mg IV every 3 weeks OR 400 mg IV every 6 weeks) in combination with radiotherapy (RT), with or without cisplatin, followed by pembrolizumab monotherapy until disease recurrence or unacceptable toxicity, for up to 1 year. In the KEYNOTE-689 clinical trial, adjuvant pembrolizumab and RT, with or without 3 cycles of cisplatin (100 mg/m2 IV every 3 weeks) began within 6 weeks following surgery and was followed by pembrolizumab 200 mg IV every 3 weeks for up to 12 cycles. Neoadjuvant treatment with pembrolizumab followed by pembrolizumab plus RT (with or without cisplatin) and then pembrolizumab monotherapy significantly improved event-free survival (59.7 months vs. 29.6 months) compared with no neoadjuvant therapy and adjuvant RT (with or without cisplatin) in patients with resectable locally advanced (Stage III-IVA) head and neck squamous cell carcinoma (HNSCC) in a multicenter, randomized, open-label clinical trial (KEYNOTE-689). Patients with high-risk pathological features received cisplatin with adjuvant RT in both treatment arms; this included 35% of patients in the pembrolizumab arm and 52% of patients in the standard of care arm. Overall survival results were not mature at the interim analysis.[57889] [72406]
NOTE: The FDA has designated pembrolizumab as an orphan drug for the treatment of Hodgkin lymphoma.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] The median progression-free survival (PFS) time was significantly improved in patients with relapsed or refractory cHL who received pembrolizumab compared with brentuximab vedotin (13.2 months vs. 8.3 months; hazard ratio (HR) = 0.65; 95% CI, 0.48 to 0.88) in a multicenter, randomized, phase 3 (KEYNOTE-204) trial (n = 304). Patients (median age, 36 years) in this trial received a median of 2 prior therapies and were ineligible for (37%) or had relapsed after (63%) autologous hematopoietic stem-cell transplantation (ASCT).[69216] At a median follow-up of 63.7 months, the objective response rate (ORR) was 71.4% (complete response [CR] rate, 27.6%) in 210 patients with relapsed or refractory cHL who received pembrolizumab in a multicenter, multicohort, phase 2 (KEYNOTE-087) trial. The median duration of response (DOR) was 16.6 months, the median PFS time was 13.7 months, and the median overall survival time was not reached. Patients who achieved a CR and had received at least 6 months of pembrolizumab including 2 cycles beyond CR were allowed to discontinue therapy; these patients could receive a second course of pembrolizumab for up to 1 year if they subsequently experienced progressive disease. In 19 evaluable patients who received a second course of pembrolizumab, the ORR was 73.7% (CR, 36.8%) and the median DOR was 15.2 months. Patients (median age, 35 years; range, 18 to 76 years) in this trial had progressed after the most recent therapy or without a response their most recent ASCT and received a median of 4 (range, 1 to 12) prior systemic therapies; 83.3% had received prior brentuximab vedotin therapy.[69217]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Efficacy for pediatric patients has been extrapolated from results from clinical trials in adult cHL patients.[57889]
200 mg IV repeated every 3 weeks for up to 24 months was evaluated in a phase 2 trial (KEYNOTE-087 trial).[61092] Alternatively, pembrolizumab 400 mg IV every 6 weeks until disease progression or up to 24 months in patients without progression may be used. There does not appear to be any clinically significant differences in efficacy and safety between pembrolizumab dosages of 200 mg IV every 3 weeks or 400 mg IV every 6 weeks based on pharmacokinetic data and model-based simulations. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized clinical trial (KEYNOTE-045), treatment with pembrolizumab significantly improved median overall survival (10.3 vs. 7.4 months) and objective response rates (21% vs. 11%; complete response, 7% vs. 3%; partial response, 14% vs. 8%) for patients with locally advanced or metastatic urothelial carcinoma with disease progression on or after platinum-containing chemotherapy treated with pembrolizumab (n = 270) compared with investigator's choice of chemotherapy (paclitaxel, n = 84; docetaxel, n = 84; vinflunine, n = 87); the median duration of response was not reached in the pembrolizumab arm, compared with 4.3 months in the chemotherapy arm. There was no significant difference in progression-free survival between treatment arms.[61782] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized clinical trial (KEYNOTE-045), treatment with pembrolizumab significantly improved median overall survival (10.3 vs. 7.4 months) and objective response rates (21% vs. 11%; complete response, 7% vs. 3%; partial response, 14% vs. 8%) for patients with locally advanced or metastatic urothelial carcinoma with disease progression on or after platinum-containing chemotherapy treated with pembrolizumab (n = 270) compared with investigator's choice of chemotherapy (paclitaxel, n = 84; docetaxel, n = 84; vinflunine, n = 87); the median duration of response was not reached in the pembrolizumab arm, compared with 4.3 months in the chemotherapy arm. There was no significant difference in progression-free survival between treatment arms. Fifteen percent of patients in this trial had disease progression following platinum-based neoadjuvant or adjuvant chemotherapy.[61782] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, open-label, single-arm clinical trial (n = 370; KEYNOTE-052), treatment with pembrolizumab resulted in an objective response rate of 29% (95% CI, 24% to 34%), with 10% complete responses and 20% partial responses, in patients with locally advanced or metastatic urothelial carcinoma who were not eligible for cisplatin-containing chemotherapy. The median duration of response was 30.1 months, with 67% of responses lasting 12 months and 52% lasting 24 months. The median overall survival was 11.3 months.[66073] [57889] In a multicenter, randomized trial, previously untreated patients with metastatic urothelial carcinoma who were eligible for platinum-containing chemotherapy (KEYNOTE-361) were randomized to treatment with pembrolizumab monotherapy, pembrolizumab with platinum-based chemotherapy to platinum-based chemotherapy alone. This study did not meet its major efficacy measures of improved progression-free survival or overall survival in the pembrolizumab plus chemotherapy arm. In an exploratory analysis, overall survival was similar in patients receiving pembrolizumab monotherapy versus chemotherapy in both the total population (15.6 months vs. 14.3 months) and in patients with CPS of 10% or higher (16.1 months vs. 15.2 months). The monotherapy arm of this trial was closed to accrual for patients with low PD-L1 expression (CPS less than 10%) upon the recommendation of the independent Data Monitoring Committee based on concerning survival data for PD-L1 inhibitor monotherapy in this trial and the IMvigor130 trial.[66963] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression, in combination with enfortumab vedotin (1.25 mg/kg [maximum, 125 mg] IV on days 1 and 8, every 21 days until disease progression or unacceptable toxicity). Administer pembrolizumab after completion of enfortumab vedotin when given on the same day. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, open-label clinical trial (KEYNOTE-A39), treatment with pembrolizumab plus enfortumab vedotin significantly improved overall survival (31.5 months vs. 16.1 months), progression-free survival (12.5 months vs. 6.3 months), and objective response rate (68% vs. 44%; complete response [CR], 29% vs. 12%) compared with platinum-based chemotherapy in patients with locally advanced or metastatic urothelial cancer with no prior systemic treatment for advanced disease. In an open-label, multicohort trial (KEYNOTE-869), treatment with pembrolizumab plus enfortumab vedotin resulted in a confirmed overall response rate of 68% (CR, 12%) in 3 cohorts of patients with previously untreated locally advanced or metastatic urothelial cancer who were ineligible for cisplatin-containing chemotherapy; the median duration of response was 22.1 months in 2 cohorts and was not reached in the third.[64845] [68834] [70064] [57889]
NOTE: Select patients for treatment based on MSI-H/dMMR status in tumor specimens. Because subclonal dMMR mutations and microsatellite instability may arise in high-grade gliomas during temozolomide therapy, it is recommended to test for MSI-H and dMMR in the primary tumor specimens obtained prior to initiation of temozolomide chemotherapy in these patients. It is recommended to confirm local MSI-H or dMMR results with an FDA-approved test if feasible, due to discordance between results. If confirmatory testing is not able to be done, the presence of TMB of 10 mut/Mb or higher may be used to select patients for treatment. Information on FDA-approved tests for patient selection is available at www.fda.gov/CompanionDiagnostics.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In pooled data from 5 multicenter, uncontrolled, open-label, multicohort, single-arm trials (KEYNOTE-016, KEYNOTE-164, KEYNOTE-028, KEYNOTE-012, and KEYNOTE-158), patients with MSI-H or dMMR solid tumors treated with pembrolizumab (10 mg/kg every 2 weeks or 200 mg every 3 weeks; n = 149) had an objective response rate of 39.6% (complete response, 7.4%; partial response, 32.2%) with a median duration of response not reached (range, 1.6+ to 22.7+ months); 78% of patients had a duration of response greater than or equal to 6 months.[57889]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease progression or up to 24 months in patients without progression; the safety and efficacy of pembrolizumab in pediatric patients with MSI-H central nervous system cancers have not been established. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Efficacy for pediatric patients has been extrapolated from results from clinical trials in adult MSI-H patients. In pooled data from 5 multicenter, uncontrolled, open-label, multicohort, single-arm trials (KEYNOTE-016, KEYNOTE-164, KEYNOTE-028, KEYNOTE-012, and KEYNOTE-158), adult patients with MSI-H or dMMR solid tumors treated with pembrolizumab (10 mg/kg every 2 weeks or 200 mg every 3 weeks; n = 149) had an objective response rate of 39.6% (complete response, 7.4%; partial response, 32.2%) with a median duration of response not reached (range, 1.6+ to 22.7+ months); 78% of patients had a duration of response greater than or equal to 6 months.[57889]
NOTE: The FDA has designated pembrolizumab as an orphan drug for the treatment of gastric cancer, including gastroesophageal junction adenocarcinoma
200 mg IV every 3 weeks until disease progression, unacceptable toxicity, or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a randomized, controlled, phase 3 trial (the KEYNOTE-062 trial), first-line treatment of HER2-negative, PD-L1 positive, locally advanced/unresectable or metastatic gastric or GEJ cancer with pembrolizumab monotherapy was noninferior to cisplatin plus fluoropyrimidine chemotherapy for overall survival; the effect on overall survival was greater in patients with PD-L1 CPS of 10 or higher although due to protocol design, this outcome was not statistically analyzed. Patients receiving pembrolizumab monotherapy also experienced fewer treatment-related adverse reactions.[65919]
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks until disease progression, unacceptable toxicity, or for up to 24 months in patients without disease progression. Administer in combination with trastuzumab (8 mg/kg IV on day 1 of cycle 1, followed 3 weeks later by 6 mg/kg IV every 3 weeks in subsequent cycles) followed by fluoropyrimidine- and platinum-containing chemotherapy. In the multicenter, randomized, double-blind clinical trial (KEYNOTE-811), investigator's choice of chemotherapy (ICC) consisted of cisplatin (80 mg/m2 IV on day 1) plus fluorouracil (800 mg/m2/day by continuous IV infusion on days 1 to 5 [total infusional dose, 4,000 mg/m2]) (FP) every 3 weeks for up to 6 cycles OR oxaliplatin (130 mg/m2 IV on day 1) plus capecitabine (1,000 mg/m2 PO twice daily on days 1 to 14, followed by 7 days off) (CAPOX) every 3 weeks for up to 6 to 8 cycles; 85% of patients received CAPOX. Administer pembrolizumab prior to trastuzumab and chemotherapy when given on the same day. Treatment with pembrolizumab plus trastuzumab and ICC significantly improved median overall survival (20.1 months vs. 15.7 months) and median progression-free survival (10.9 months vs. 7.3 months) compared with compared with placebo, trastuzumab, and ICC. The objective response rate was 73% (complete response [CR], 17%) in the pembrolizumab arm for a median duration of 11.3 months compared with 58% (CR, 10%) for a median duration of 9.6 months in the placebo arm.[69837] [57889] [66655] [72048]
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks until disease progression, unacceptable toxicity, or for up to 24 months in patients without disease progression. Administer in combination with fluoropyrimidine- and platinum-containing chemotherapy; administer pembrolizumab prior to chemotherapy when given on the same day. In the KEYNOTE-859 trial, chemotherapy consisted of FP (cisplatin [80 mg/m2 IV on day 1] plus fluorouracil [800 mg/m2/day by continuous IV infusion on days 1, 2, 3, 4, and 5; total infusional dose 4,000 mg/m2] every 3 weeks or CAPOX [capecitabine 1,000 mg/m2 PO twice daily on days 1 to 14, followed by 7 days off], plus oxaliplatin [130 mg/m2 IV on day 1] every 3 weeks). Treatment with pembrolizumab plus investigator's choice of chemotherapy (FP or CAPOX) significantly improved overall survival (OS) (13 months vs. 11.4 months), progression-free survival (PFS) (6.9 months vs. 5.6 months), and objective response rate (ORR) (52% vs. 43%; complete response [CR], 10% vs. 6%) compared with placebo plus chemotherapy in patients with HER2-negative, PD-L1 positive (CPS 1 or higher), advanced gastric or GEJ cancer who had not previously received systemic therapy for metastatic disease in a planned interim analysis of a multicenter, randomized, double-blind, phase 3 clinical trial (KEYNOTE-859); 86% of patients received CAPOX. The median OS (15.7 months vs. 11.8 months), PFS (8.1 months vs. 5.6 months), and ORR (61% vs. 43%; CR, 13% vs. 5%) were also significantly improved in the nivolumab arm versus placebo in patients with CPS 10 or higher tumors. In an exploratory analysis, overall survival was not significantly different between groups for patients with CPS less than 1. The duration of response was 8.3 months compared with 5.6 months, respectively, in the CPS 1 or higher population; the duration of response was 10.9 months versus 5.8 months, respectively, in the CPS 10 or higher population.[57889] [69908]
Dosage not available.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] In a nonrandomized, phase 2 (KEYNOTE-170) trial, the primary endpoint of objective response rate (assessed by blinded central review) was 45% (complete response (CR) rate, 13%) following pembrolizumab therapy in 53 patients with PMBCL who had relapsed or refractory disease after at least 2 prior lines of therapy. At a median follow-up time of 48.7 (range, 41.2 to 56.2) months, the investigator-assessed best overall response rate was 41.5% (CR rate, 20.8%) in patients who received pembrolizumab in the KEYNOTE-170 trial. The median progression-free survival (PFS) and overall survival (OS) times were 4.3 months and 22.3 months, respectively. In this study, patients (median age, 33 years; range, 20 to 61 years) had received a median of 3 (range, 2 to 8) prior therapies including rituximab; 26% of patients had previously received an autologous stem-cell transplant and 32% of patients had received prior radiation therapy.[70186] [70187] At a median follow-up time of 29.1 months, the objective response rate was 48% (CR rate, 33%) in a cohort of patients with PMBCL who experienced relapse after or were ineligible for autologous stem-cell transplantation (n = 21) in a phase 1b (KEYNOTE-013) trial. After an additional 26 months of follow-up, the median PFS and OS times were 19 months and 37.1 months, respectively.[70186] [70189]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Efficacy for pediatric patients has been extrapolated from results from clinical trials in adult PMBCL patients.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. The overall response rate was 14.3% in a cohort of 77 patients with recurrent or metastatic PD-L1-expressing cervical cancer who received pembrolizumab in a multi-cohort, nonrandomized trial (KEYNOTE-158). Additionally, a complete response was achieved in 2.6% of patients. At a median follow-up time of 11.7 months, the median duration of response was not reached (range, 4.1 to 18.6+ months); 91% of patients had a response duration lasting 6 months or longer. Patients (median age, 45 years; range, 27 to 75 years) in this study had received 1 (35%) or 2 (65%) lines of prior therapy.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Use in combination with paclitaxel 175 mg/m2 IV on day 1 plus either cisplatin 50 mg/m2 IV on day 1 or 2 OR carboplatin AUC of 5 IV on day 1, with or without bevacizumab 15 mg/kg IV on day 1 every 3 weeks. Administer pembrolizumab prior to chemotherapy when given on the same day. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] At the first interim analysis of a multicenter, randomized, double-blind, phase 3 trial (KEYNOTE-826), treatment with pembrolizumab plus chemotherapy significantly improved the median progression-free survival compared with placebo plus chemotherapy in patients with recurrent, persistent, or metastatic cervical cancer (10.4 months vs. 8.2 months); bevacizumab was added to treatment in 63% of patients in this trial. The objective response rate was 68% in the pembrolizumab arm compared with 50% in the placebo arm, respectively (complete response, 23% vs. 14%); the median duration of response was 18 months versus 10.4 months, respectively. In the final overall survival (OS) analysis, treatment with pembrolizumab plus chemotherapy significantly improved the median OS compared with placebo plus chemotherapy in the intent-to-treat population (26.4 months vs. 16.8 months), the PD-L1 CPS of greater than or equal to 1 population (28.6 months vs. 16.5 months), and in the PD-L1 CPS greater than or equal to 10 population (29.6 months vs. 17.4 months).[67047] [69855]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression, unacceptable toxicity, or for up to 24 months in patients without progression. Administer in combination with cisplatin (40 mg/m2 IV once weekly for 5 cycles) and radiotherapy (external beam radiation therapy [ERBT] followed by brachytherapy [BT]). Administer pembrolizumab prior to chemoradiotherapy when given on the same day. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Treatment with pembrolizumab plus cisplatin and ERBT followed by BT (chemoradiotherapy [CRT]) was compared with placebo plus CRT in a multicenter, randomized, double-blind clinical trial (KEYNOTE-A18) which included patients with cervical cancer who had not previously received any definitive surgery, radiation, or systemic therapy for cervical cancer; of these patients (n = 1,060), 56% had FIGO 2014 stage III to IVA disease and 44% had FIGO 2014 stage 1B2 to IIB node positive disease. In the subset of patients with FIGO 2014 stage III to IVA disease, the addition of pembrolizumab to CRT significantly improved the median progression-free survival PFS by investigator, which was not reached in both arms with a lower level of the 95% confidence interval not reached in the pembrolizumab arm compared with 18.8 months in the placebo arm; the 12-month rate of PFS was 81% versus 70%, respectively. Overall survival at 24 months was also significantly improved in the pembrolizumab arm (87% vs. 81%).[57889] [70191] [72404]
NOTE: The FDA has designated pembrolizumab as an orphan drug for this indication.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Treatment with pembrolizumab significantly improved median overall survival (13.9 months vs. 13 months) compared with placebo in patients with previously-treated Barcelona Clinical Liver Cancer (BCLC) Stage B or C hepatocellular cancer in a multicenter, randomized clinical trial conducted in Asia; 79% of patients had active hepatitis B. The median progression-free survival was 2 months in the pembrolizumab arm compared with 2.3 months in the placebo arm; the objective response rate was 11% versus 1.6%, respectively, with a median duration of 23.9 months in patients who received pembrolizumab and 5.6 months in those who received placebo. Complete responses were achieved by 0.9% of patients in the pembrolizumab arm and 0.8% of those in the placebo arm.[70283] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease recurrence, unacceptable toxicity, or for up to 12 months in patients without disease recurrence. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Adjuvant treatment with pembrolizumab significantly improved disease-free survival (DFS) and overall survival (OS) compared with placebo in patients with renal cell cancer with an intermediate-high or high risk of recurrence after nephrectomy or M1 with no evidence of disease after nephrectomy in a randomized clinical trial (KEYNOTE-564); the 24-month DFS rate was 77% vs. 68% and the 48-month OS rate was 91% vs. 86%, respectively.[57889] [67129]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with axitinib (initial dose, 5 mg PO twice daily). The axitinib dosage may be increased to 7 mg twice daily and then to 10 mg twice daily at intervals of 6 weeks or longer in normotensive patients (BP less than or equal to 150/90) who tolerate the lower dosage for at least 2 consecutive weeks with no greater than grade 2 adverse reactions. Continue axitinib until disease progression or unacceptable toxicity.[63966] [57889] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[48494] Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions; permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] Combination therapy with pembrolizumab and axitinib significantly improved median overall survival (45.7 months vs. 40.1 months) and median progression-free survival (15.7 months vs. 11.1 months) compared with sunitinib in patients with advanced renal cell cancer in the final analysis of an open-label, phase 3 clinical trial (KEYNOTE-426). The objective response rate was 60.4% (complete response [CR], 10%) versus 39.6% (CR, 3.5%), respectively; the median duration of response was 23.6 months in patients receiving combination therapy compared with 15.3 months for patients treated with sunitinib.[67485] [63966] [57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks in combination with lenvatinib (20 mg orally once daily), continue treatment until disease progression or for up to 24 months in patients without progression. After 2 year of combination therapy, lenvatinib may be continued as a single agent until disease progression or unacceptable toxicity. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions; permanently discontinue therapy for severe or life-threatening infusion-related reactions.[57889] [58782] Investigator-assessed median progression-free survival was significantly improved with lenvatinib plus pembrolizumab compared with sunitinib (23.9 months vs. 9.2 months) in patients with previously untreated advanced RCC with a clear-cell component in a 3-arm, randomized (1:1:1), phase 3 trial (CLEAR/KEYNOTE-581); the objective response rate (ORR) was 71% versus 36%, respectively (complete response, 16% vs. 4%).[66893] In an updated overall survival [OS] analysis, the median OS for patients treated with pembrolizumab plus lenvatinib was 53.7 months compared with 54.3 months for those who received sunitinib.[69686] First-line treatment with pembrolizumab plus lenvatinib also resulted in an ORR of 51% (CR, 8%) for a median duration of 19.5 months in a multicenter, single-arm trial of patients with advanced or metastatic non-clear cell RCC (KEYNOTE-B61).[70731]
Dosage not established.
NOTE: The FDA has designated pembrolizumab as an orphan drug for the treatment of esophageal cancer.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Treatment with pembrolizumab significantly improved the median overall survival (OS) (9.3 months vs. 6.7 months) and progression-free survival (3.2 months vs. 2.3 months) compared with investigators' choice of chemotherapy (i.e., paclitaxel, docetaxel, or irinotecan monotherapy) in patients with recurrent, progressive, PD-L1 positive (CPS 10 or higher), locally advanced or metastatic esophageal or GEJ cancer in a randomized clinical trial (KEYNOTE-181); the estimated 12-month survival was 43% versus 20%, respectively; median OS was 8.2 versus 7.1 months, respectively, in patients with squamous cell carcinoma, and was unchanged (7.1 months) in all patients. The objective response rate was 21.5% in the pembrolizumab arm compared with 6.1% in the chemotherapy arm (complete response, 3.7% vs. 0.9%); the median duration of response was 9.3 months versus 7.7 months, respectively.[57889] [66536]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Administer pembrolizumab prior to chemotherapy when given on the same day. In the KEYNTOTE-590 trial, pembrolizumab was administered with FP (cisplatin [80 mg/m2 IV on day 1 every 3 weeks for up to 6 cycles] and fluorouracil (800 mg/m2/day by continuous IV infusion on days 1, 2, 3, 4, and 5; total infusional dose, 4,000 mg every 3 weeks for up to 24 months). In a randomized clinical trial (KEYNOTE-590), treatment with pembrolizumab plus FP significantly improved median overall survival (OS) (12.7 months vs. 9.8 months) and median progression-free survival (PFS) (6.3 months vs. 5.7 months) compared with placebo plus FP in patients with PD-L1 positive (CPS 1 or higher), locally advanced or metastatic esophageal/GEJ tumors who were not candidates for surgical resection or definitive chemoradiation. The median OS (13.5 months vs. 9.4 months) and PFS (7.5 months vs. 5.5 months) were also significantly improved in pembrolizumab-treated patients with PD-L1 CPS of 10 or higher in a prespecified formal exploratory analysis. The objective response rate (ORR) in patients with CPS 1 or higher tumors was 45% in pembrolizumab-treated patients versus 29% in the placebo arm (complete response [CR], 6% vs. 2.8%); in patients with CPS 10 or higher, the ORR was 51% versus 27% (CR, 6% vs. 2.5%), respectively. The median duration of response ranged from 8.6 to 10.4 months in patients who received pembrolizumab plus FP compared with 5.6 to 5.8 months those who received placebo plus FP.[57889] [66945]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or for up to 24 months in patients without disease progression in combination with lenvatinib 20 mg PO once daily until disease progression. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Treatment with pembrolizumab plus lenvatinib significantly improved the median progression-free survival (6.6 months vs. 3.8 months) and overall survival (17.4 months vs. 12 months) compared with doxorubicin or paclitaxel in patients with advanced endometrial cancer who had been previously treated with at least one prior platinum-based chemotherapy regimen in any setting and were not MSI-H or dMMR in a multicenter, randomized, open-label clinical trial (KEYNOTE-775). The objective response rate was also significantly improved in the pembrolizumab/lenvatinib arm (30% vs. 15%; complete response, 5% vs. 3%) for a median duration of 9.2 months versus 5.7 months, respectively.[57889] [58782] [67484]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. In 2 cohorts of a multicenter, open-label, noncomparative, multicohort, phase 2 trial (KEYNOTE-158), the objective response rate was 46% (complete response, 12%) for a median duration that was not reached in patients with unresectable or metastatic MSI-H or dMMR endometrial cancer received at least 1 dose of pembrolizumab; of patients who responded, 68% had a response duration of at least 12 months and 44% had a response duration of at least 24 months.[57889] [67483]
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks until disease progression or for up to 24 months in patients without disease progression in combination with carboplatin AUC 5 IV and paclitaxel 175 mg/m2 IV on day 1 every 3 weeks for 6 cycles. Administer pembrolizumab prior to chemotherapy when given on the same day. Treatment with pembrolizumab plus carboplatin and paclitaxel significantly improved progression-free survival (PFS) in patients with advanced or recurrent endometrial cancer compared with placebo plus carboplatin and paclitaxel in a multicenter, randomized, double-blind clinical trial (KEYNOTE-868) in both the mismatch repair deficient (dMMR) (not reached vs. 6.5 months) and mismatch repair proficient (pMMR) (11.1 months vs. 8.5 months) cohorts.[57889] [70798]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until persistent or recurrent high-risk NMIBC, disease progression, or for up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Treatment of BCG-unresponsive, high-risk NMIBC with pembrolizumab resulted in a complete response rate of 41% for a median duration of 16.2 months in a multicenter, noncomparative trial (n = 96).[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression, unacceptable toxicity, or for up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. Pembrolizumab was administered to 10 cohorts of patients with various previously-treated unresectable or metastatic solid tumors with TMB-H in a prospectively-planned, retrospective analysis of a multicenter, noncomparative trial (KEYNOTE-158). For patients with at least 13 mut/Mb, the objective response rate was 37% (complete response [CR], 3%) for a median duration that was not reached; 58% of patients had a duration of response of at least 12 months, and 50% had a duration of at least 24 months. For patients with at least 10 mut/Mb, the objective response rate was 29% (complete response [CR], 4%) for a median duration that was not reached; 57% of patients had a duration of response of at least 12 months, and 50% had a duration of at least 24 months. The highest response rates were seen in patients with endometrial cancer (n = 15; 47%), neuroendocrine cancer (n = 5; 40%), cervical cancer (n = 16; 31%), and small cell lung cancer (n = 34; 29%); two patients with thyroid cancer were treated and both achieved complete response for a duration of 8.2 months and more than 33.2 months at last follow-up.[57889]
2 mg/kg (not to exceed 200 mg) IV repeated every 3 weeks until disease progression, unacceptable toxicity, or for up to 24 months in patients without progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. The use of pembrolizumab in pediatric patients is supported by evidence from adequate and well-controlled studies of pembrolizumab in adults with additional pharmacokinetic and safety data in pediatric patients. Pembrolizumab was administered to 10 cohorts of patients with various previously-treated unresectable or metastatic solid tumors with TMB-H in a prospectively-planned, retrospective analysis of a multicenter, noncomparative trial (KEYNOTE-158). For patients with at least 13 mut/Mb, the objective response rate was 37% (complete response [CR], 3%) for a median duration that was not reached; 58% of patients had a duration of response of at least 12 months, and 50% had a duration of at least 24 months. For patients with at least 10 mut/Mb, the objective response rate was 29% (complete response [CR], 4%) for a median duration that was not reached; 57% of patients had a duration of response of at least 12 months, and 50% had a duration of at least 24 months. The highest response rates were seen in patients with endometrial cancer (n = 15; 47%), neuroendocrine cancer (n = 5; 40%), cervical cancer (n = 16; 31%), and small cell lung cancer (n = 34; 29%); two patients with thyroid cancer were treated and both achieved complete response for a duration of 8.2 months and more than 33.2 months at last follow-up.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions; permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a nonrandomized, phase 2 (KEYNOTE-629) trial, treatment with pembrolizumab resulted in objective response rates of 35% (complete response (CR), 12%) and 52% (CR, 22%) in patients with recurrent or metastatic cSCC or locally advanced cSCC, respectively. In patients with recurrent or metastatic cSCC, the median duration of response was not reached (range, 2.7 months to more than 64.2 months) at a median follow-up time of 23.8 months; the duration of response was at least 12 months in 68% of patients. In patients with locally advanced cSCC, the median duration of response was 47.2 months at a median follow-up time of 48 months; the duration of response was at least 12 months in 75% of patients.[57889]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without disease progression. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions; permanently discontinue therapy for severe or life-threatening infusion-related reactions. At a median follow-up time of 27.6 months (range, 0.2 to 48.3 months), the median progression-free survival time was significantly improved in patients with previously untreated unresectable or metastatic MSI-H or dMMR colorectal cancer who received pembrolizumab compared with standard chemotherapy (16.5 months vs. 8.2 months) in a randomized, phase 3 trial (KEYNOTE-177). The overall survival data were not mature at the time of this analysis. In this trial, patients in the standard chemotherapy arm received therapy every 2 weeks that consisted of either mFOLFOX6 (oxaliplatin 85 mg/m2 IV on day 1; leucovorin 400 mg/m2 (or levoleucovorin 200 mg/m2) IV on day 1; and fluorouracil 400 mg/m2 IV bolus on day 1, then fluorouracil 2,400 mg/m2 IV over 46 to 48 hours) or FOLFIRI (irinotecan 180 mg/m2 IV on day 1; leucovorin 400 mg/m2 (or levoleucovorin 200 mg/m2) IV on day 1; and fluorouracil 400 mg/m2 IV bolus on day 1, then fluorouracil 2,400 mg/m2 IV over 46 to 48 hours). Bevacizumab (5 mg/kg IV on day 1) or cetuximab (400 mg/m2 IV on first infusion, then 250 mg/m2 once weekly) were added to mFOLFOX6 or FOLFIRI in some patients. In pooled data from 4 multicenter, uncontrolled, open-label, multicohort, single-arm trials (KEYNOTE-016, KEYNOTE-164, KEYNOTE-028, and KEYNOTE-158), the objective response rate was 36% in 90 patients with MSI-H or dMMR colorectal cancer who received pembrolizumab (10 mg/kg every 2 weeks or 200 mg every 3 weeks). The median duration of response ranged from 1.6+ to 22.7+ months in these patients. Most (84%) patients with colorectal cancer had received 2 or more prior lines of therapy.[57889]
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks for up to 24 weeks prior to surgery or until disease progression or unacceptable toxicity. In KEYNOTE-522, concomitant neoadjuvant chemotherapy administered with pembrolizumab included 12 weeks of paclitaxel (80 mg/m2 IV once weekly) plus carboplatin (AUC 5 IV every 3 weeks OR AUC 1.5 IV once weekly) followed by 12 weeks of cyclophosphamide (600 mg/m2 IV) plus either doxorubicin (60 mg/m2 IV) OR epirubicin (90 mg/m2 IV) on day 1 every 3 weeks, followed by surgery. Administer pembrolizumab prior to chemotherapy when given on the same day. After surgery, continue pembrolizumab 200 mg IV every 3 weeks OR 400 mg IV every 6 weeks as monotherapy for up to 27 weeks or until disease progression or unacceptable toxicity. Do not administer adjuvant pembrolizumab to patients with disease progression or unacceptable toxicity related to the neoadjuvant phase of treatment. Patients with high-risk, early stage TNBC were randomized to neoadjuvant treatment with pembrolizumab or placebo in combination with chemotherapy in a phase 3 clinical trial (KEYNOTE-522); after definitive surgery, patients received adjuvant pembrolizumab monotherapy or placebo. Treatment with pembrolizumab plus chemotherapy significantly improved the rate of pathologic complete response (pCR) (63% vs. 55.6%) compared with placebo plus chemotherapy. The median event-free survival (EFS) was not reached in either arm, although EFS at 18 months was 91.3% in patients who received pembrolizumab compared with 85.3% in those who received placebo (HR 0.63; 95% CI, 0.43 to 0.93). After a median follow-up of 75.1 months, restricted mean survival time was also significantly improved in the pembrolizumab arm (55.3 months vs. 54.1 months). In a prespecified subgroup analysis, the 5-year survival rate was 94.5% in the pembrolizumab arm for patients who had a pCR compared with 92.2% in the placebo arm; for patients without a pCR, the 5-year survival rate was 69.6% versus 60.7%, respectively.[57889] [66036] [71471]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with nab-paclitaxel (100 mg/m2 on days 1, 8, and 15, every 28 days); the number of cycles of nab-paclitaxel was not specified.[66122] [66123] [57889] Administer pembrolizumab prior to chemotherapy when given on the same day. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, double-blind clinical trial (KEYNOTE-355), patients with locally recurrent unresectable or metastatic TNBC who had not been previously treated with chemotherapy in the metastatic setting were randomized to treatment with either pembrolizumab or placebo in combination with paclitaxel, nab-paclitaxel, or gemcitabine plus carboplatin regardless of tumor PD-L1 expression. The addition of pembrolizumab to chemotherapy significantly improved the median progression-free survival (9.7 months vs. 5.6 months) compared with placebo plus chemotherapy in the subgroup of patients with a CPS of 10 or more in a prespecified interim analysis. At the prespecified final analysis, the median overall survival was also significantly improved in the pembrolizumab arm (23 months versus 16.1 months, respectively). The objective response rate was 53% compared with 40%, respectively (complete response, 17% vs. 13%) for a median duration of 19.3 months in the pembrolizumab arm and 7.3 months in the placebo arm.[57889] [66123]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with paclitaxel (90 mg/m2 on days 1, 8, and 15, every 28 days); the number of cycles of paclitaxel was not specified.[66122] [66123] [57889] Administer pembrolizumab prior to chemotherapy when given on the same day. To prevent hypersensitivity reactions, all patients should be premedicated with dexamethasone 20 mg PO approximately 12 and 6 hours before paclitaxel, diphenhydramine 50 mg IV (or equivalent) 30 to 60 minutes before paclitaxel, and an IV H2-blocker 30 to 60 minutes before paclitaxel.[29200] Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, double-blind clinical trial (KEYNOTE-355), patients with locally recurrent unresectable or metastatic TNBC who had not been previously treated with chemotherapy in the metastatic setting were randomized to treatment with either pembrolizumab or placebo in combination with paclitaxel, nab-paclitaxel, or gemcitabine plus carboplatin regardless of tumor PD-L1 expression. The addition of pembrolizumab to chemotherapy significantly improved the median progression-free survival (9.7 months vs. 5.6 months) compared with placebo plus chemotherapy in the subgroup of patients with a CPS of 10 or more in a prespecified interim analysis. At the prespecified final analysis, the median overall survival was also significantly improved in the pembrolizumab arm (23 months versus 16.1 months, respectively). The objective response rate was 53% compared with 40%, respectively (complete response, 17% vs. 13%) for a median duration of 19.3 months in the pembrolizumab arm and 7.3 months in the placebo arm.[57889] [66123]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression in combination with gemcitabine (1,000 mg/m2 IV on days 1 and 8, every 21 days) and carboplatin (AUC 2 IV on days 1 and 8, every 21 days); the number of cycles of gemcitabine plus carboplatin was not specified.[66122] [66123] [57889] Administer pembrolizumab prior to chemotherapy when given on the same day. Pembrolizumab therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, double-blind clinical trial (KEYNOTE-355), patients with locally recurrent unresectable or metastatic TNBC who had not been previously treated with chemotherapy in the metastatic setting were randomized to treatment with either pembrolizumab or placebo in combination with paclitaxel, nab-paclitaxel, or gemcitabine plus carboplatin regardless of tumor PD-L1 expression. The addition of pembrolizumab to chemotherapy significantly improved the median progression-free survival (9.7 months vs. 5.6 months) compared with placebo plus chemotherapy in the subgroup of patients with a CPS of 10 or more in a prespecified interim analysis. At the prespecified final analysis, the median overall survival was also significantly improved in the pembrolizumab arm (23 months versus 16.1 months, respectively). The objective response rate was 53% compared with 40%, respectively (complete response, 17% vs. 13%) for a median duration of 19.3 months in the pembrolizumab arm and 7.3 months in the placebo arm.[57889] [66123]
NOTE: Pembrolizumab is designated by the FDA as an orphan drug for the treatment of biliary tract carcinoma.
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or up to 24 months in patients without progression. Administer in combination with cisplatin (25 mg/m2 IV) plus gemcitabine (1,000 mg/m2 IV) on days 1 and 8, every 3 weeks; in KEYNOTE-966, treatment with cisplatin was limited to 8 cycles and there was no limit to the number of cycles of gemcitabine. Administer pembrolizumab prior to chemotherapy when given on the same day. Therapy may need to be temporarily withheld or permanently discontinued in patients who develop immune-related reactions. Permanently discontinue therapy for severe or life-threatening infusion-related reactions. In a multicenter, randomized, double-blind phase 3 clinical trial (KEYNOTE-966), treatment with pembrolizumab in combination with cisplatin and gemcitabine significantly improved the median overall survival compared with placebo plus cisplatin and gemcitabine (12.7 months vs. 10.9 months) in patients with locally advanced unresectable or metastatic biliary tract cancer who had not received prior systemic therapy in the advanced disease setting. The median progression-free survival was 6.5 months in the pembrolizumab arm compared with 5.6 months in the placebo arm, and the median objective response rate was 29% in each arm (complete response, 2.1% vs. 1.3%); the median duration of response was 8.3 months vs. 6.8 months, respectively.[57889] [69750]
200 mg IV repeated every 3 weeks OR 400 mg IV repeated every 6 weeks until disease progression or for up to 24 months in patients without progression. Administer in combination with pemetrexed 500 mg/m2 IV on day 1 plus either carboplatin AUC 5 or 6 IV or cisplatin 75 mg/m2 IV on day 1, every 21 days for up to 6 cycles. Administer pembrolizumab prior to pemetrexed and chemotherapy when given on the same day. In a multicenter, randomized, open-label clinical trial (KEYNOTE-483), treatment with pembrolizumab in combination with pemetrexed and platinum-based chemotherapy significantly improved overall survival (OS) (17.3 months vs. 16.1 months) compared with chemotherapy alone in unselected patients with unresectable advanced or metastatic malignant pleural mesothelioma who had received no prior systemic therapy for advanced/metastatic disease; progression-free survival was 7.1 months in each arm. The objective response rate was 52% (1 complete response) in the pembrolizumab arm compared with 29% in the control arm. Seventy-eight percent (78%) of patients had epithelioid histology and 60% had tumors with PD-L1 CPS greater than or equal to 1. In a prespecified exploratory analysis of patients with epithelioid histology, the median OS was 19.8 months in patients who received pembrolizumab plus chemotherapy and 18.2 months for those treated with chemotherapy alone; median OS was 12.3 months versus 8.2 months, respectively, for patients with non-epithelioid histology.[71280] [57889]
Recommended Monitoring
Management of Treatment-Related Toxicity
Immune-Mediated Reactions
NOTE: Corticosteroid therapy consists of prednisone 1 to 2 mg/kg per day or equivalent, followed by a 1-month taper starting when the toxicity resolves to grade 1 or less. Consider starting other systemic immunosuppressants if toxicity is not controlled by corticosteroids. Permanently discontinue pembrolizumab in patients who do not have a complete or partial resolution of toxicity or who cannot reduce their daily prednisone dose to less than 10 mg (or equivalent) within 12 weeks of initiating steroids.[57889]
Colitis
Endocrinopathies(including Type 1 diabetes, Hypophysitis, Hypothyroidism, Hyperthyroidism, and Adrenal Insufficiency)
Exfoliative Skin Reactions
Hematologic Toxicity (classical Hodgkin lymphoma and primary mediastinal large B-cell lymphoma only)
Infusion-Related Reactions
Neurologic Toxicity
Pneumonitis
Other Immune-Mediated Adverse Reactions
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks.
200 mg IV every 3 weeks OR 400 mg IV every 6 weeks.
2 mg/kg (Max: 200 mg) IV every 3 weeks.
2 mg/kg (Max: 200 mg) IV every 3 weeks.
2 mg/kg (Max: 200 mg) IV every 3 weeks.
Treatment-Related Immune-Mediated Hepatitis
Monotherapy, No Tumor Involvement of the Liver
Monotherapy, Tumor Involvement of the Liver
NOTE: For patients with baseline AST/ALT at the ULN or less, follow the recommendations for hepatitis with no tumor involvement of the liver.
Combination Therapy with Axitinib
Treatment-Related Immune-Mediated Nephritis with Renal Dysfunction
Pembrolizumab is a programmed death receptor-1 (PD-1) blocking monoclonal antibody that works by preventing the interaction between PD-1 and the PD-L1 and PD-L2 ligands. It is indicated for the treatment of certain types of breast cancer, cervical cancer, cutaneous squamous cell carcinoma, endometrial cancer, esophageal cancer, gastric cancer, head and neck cancer, hepatocellular cancer, Hodgkin lymphoma, melanoma, Merkel cell carcinoma, mesothelioma, microsatellite instability-high or mismatch repair deficient solid tumors (including colorectal cancer), lung cancer, primary mediastinal large B-cell lymphoma (PMBCL), renal cell carcinoma, tumor mutational burden-high solid tumors, and urothelial carcinoma. Immune-mediated adverse reactions including colitis, pneumonitis, hepatitis, hypophysitis, nephritis, hypothyroidism/hyperthyroidism, and encephalitis have been reported with pembrolizumab use; treatment with high-dose corticosteroids may be necessary for patients who develop immune-mediated toxicity.[57889]
For storage information, see the specific product information within the How Supplied section.
Emetic Risk
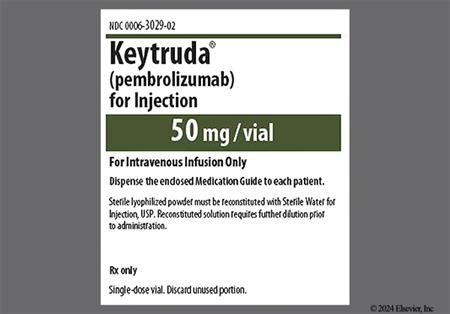
Lyophilized powder single-use vials
Reconstitution
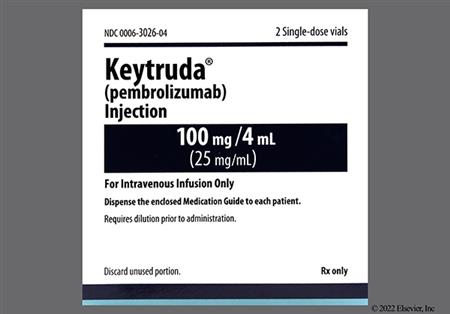
Pembrolizumab single-use solution or reconstituted lyophilized powder
Dilution
Intermittent Intravenous Infusion
Immune-mediated hepatitis occurred in 0.7% (grade 3 or 4, 0.4%) of patients receiving pembrolizumab in clinical trials (n = 2,799); 68% received systemic corticosteroids and 11% of required additional immunosuppressant therapy. Resolution occurred in 79% of patients. An interruption or discontinuation of therapy may be necessary depending on the severity; treatment with systemic corticosteroids or other immunosuppressants may be necessary. All patients who had treatment held for hepatitis resumed treatment after symptom improvement without recurrence. Elevated hepatic enzymes including increased ALT (20% to 33%; grade 3 or 4, 1.8% to 5%) and AST (20% to 38%; grade 3 or 4, 1.8% to 5%) occurred in patients who received pembrolizumab monotherapy in clinical trials for cancers other than hepatocellular cancer (HCC). The incidence of transaminitis increased in monotherapy patients with HCC (40% to 54%; grade 3 or 4, 7% to 20%), and when pembrolizumab was administered with platinum chemotherapy (22% to 50%; grade 3 or 4, 1 to 7%), with fluorouracil or capecitabine and oxaliplatin (40% to 57%; grade 3 or 4, 4.2% to 4.7%), with lenvatinib (52% to 58%; grade 3 or 4, 7% to 9%), with taxanes or gemcitabine/cisplatin (57% to 60%; grade 3 or 4, 9% to 11%), with axitinib (57% to 60%; grade 3 or 4, 13% to 20%), with neoadjuvant platinum therapy followed by neoadjuvant doxorubicin or epirubicin with cyclophosphamide (65% to 70%), and with enfortumab vedotin (59% to 75%; grade 3 or 4, 4.6% to 9%). Increased alkaline phosphatase occurred in 17% to 48% (grade 3 or 4, 0.3% to 7%)of patients regardless of concomitant therapy. Hyperbilirubinemia has also been reported, with an increase in bilirubin from baseline occurring in 11% to 33% of patients without HCC treated with pembrolizumab as monotherapy or in combination with axitinib, capecitabine/oxaliplatin with or without trastuzumab, fluorouracil/oxaliplatin, trastuzumab/fluorouracil/oxaliplatin, or lenvatinib (grade 3 or 4, 1.4% to 5%); increased bilirubin occurred in 47% of patients with HCC who received pembrolizumab monotherapy. Hepatotoxicity occurred in 14% of patients treated with pembrolizumab monotherapy, 25% of those who received combination therapy with lenvatinib, and 39% of those treated in combination with axitinib in 3 clinical trials (grade 3 or 4, 3.7%, 9%, and 20%, respectively), including transaminitis, immune-mediated and autoimmune hepatitis, hepatic failure, increased bilirubin, increased GGT, and drug-induced liver injury. Grade 3 or 4 ascites occurred in 8% of patients with HCC who received single-agent pembrolizumab in 1 clinical trial. Cholangitis (2.8%) and biliary obstruction (2.3%) occurred in patients with advanced biliary tract cancer treated with pembrolizumab in combination with other drugs in clinical trials; sclerosing cholangitis has been reported in postmarketing experience with pembrolizumab. Fatal cases of hepatitis, including autoimmune hepatitis, have been reported.[57889]
Hypoalbuminemia was reported in 16% to 44% of patients who received pembrolizumab as monotherapy (grade 3 or 4, 0.7% to 5%) and in 32% to 60% of those receiving pembrolizumab in combination with chemotherapy or oral targeted therapy in clinical trials (grade 3 or 4, 0.5% to 4.2%).[57889]
Constipation occurred in up to 21% (grade 3 or 4, 1.1% or less) of patients who received single-agent pembrolizumab and in 18% to 42% (grade 3 or 4, 1% or less) of patients who received pembrolizumab in combination with other drugs in clinical trials. Nausea was reported in 11% to 28% (grade 3 or 4, 1.6% or less) of patients who received pembrolizumab monotherapy or in combination with axitinib. The incidence was higher when administered in combination with lenvatinib or cytotoxic chemotherapy (24% to 67%; grade 3 or 4, 7% or less). Vomiting occurred in 19.8% or fewer (grade 3 or 4, 1.4% or less) patients who received single-agent pembrolizumab and in 12% to 37% (grade 3 or 4, 7% or less) of patients who received pembrolizumab plus lenvatinib or cytotoxic chemotherapy. The incidence of vomiting (29%) in pediatric patients (age range, 6 months to 17 years) with various cancers who received pembrolizumab 2 mg/kg IV every 3 weeks was at least 10% higher compared with adults. Abdominal pain was reported in 24% or fewer (grade 3 or 4, 3.1% or less) patients who received pembrolizumab as monotherapy or in combination with chemotherapy including pediatric patients, and in 27% to 34% (grade 3 or 4, 22.6%) of patients who received pembrolizumab plus lenvatinib in clinical trials. The term abdominal pain included pelvic pain, flank pain, tumor pain, bladder pain, hepatic pain, suprapubic pain, and abdominal discomfort in some studies.[57889]
Stomatitis occurred in 3% and mucosal inflammation in 4.3% (grade 3 or 4, 1.3%) of patients with locally advanced or metastatic head and neck cancer treated with pembrolizumab monotherapy in a randomized, open-label trial. The incidence of stomatitis was higher (26% to 43%; grade 3 or 4, 1.6% to 8%) in patients who received pembrolizumab in combination with axitinib, lenvatinib, or platinum-based chemotherapy for various indications. Stomatitis (48%; grade 3 or 4, 14%) was most frequently reported in patients with locally advanced head and neck squamous cell carcinoma (HNSCC) treated with pembrolizumab in combination with radiotherapy with or without cisplatin in an open-label, active-controlled trial. In various trials, the term stomatitis included aphthous ulcer, oral ulceration, cheilitis, oral mucosal erythema or inflammation, glossitis, and tongue ulceration. Oropharyngeal pain was reported in 8% of patients with classical Hodgkin lymphoma who received pembrolizumab monotherapy in a randomized trial. The addition of pembrolizumab to axitinib or platinum-based chemotherapy increased the incidence of grade 3 or 4 stomatitis/mucosal inflammation by 2.2% to 5% compared with control arms.[57889]
Decreased appetite (including early satiety and anorexia) was reported in 15% to 44% (grade 3 or 4, 7% or less) of patients treated with pembrolizumab as monotherapy or in combination with other drugs in clinical trials. Decreased weight/weight loss occurred in 10% to 48% (grade 3 or 4, 14% or less) of pembrolizumab-treated patients.[57889]
Dysphagia occurred in 8% to 12% (grade 3 or 4, 2.3% to 2.9%) of patients with locally advanced or metastatic head and neck cancer receiving pembrolizumab as a single agent or in combination with platinum-based chemotherapy in a randomized, open-label clinical trial; this was similar to the incidence in patients receiving platinum-based chemotherapy without pembrolizumab (10%; grade 3 or 4, 2.1%). Dysphagia (29%; grade 3 or 4, 12%) was most frequent in patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 open-label, active-controlled trial. Dysgeusia was reported in 21% to 35% of urothelial cancer patients who received treatment with pembrolizumab in combination with enfortumab vedotin in another trial.[57889]
Immune-mediated thyroid disorders including hyperthyroidism have been reported with pembrolizumab therapy. Hyperthyroidism occurred in 13% (grade 3 or 4, 0.3% or less) or fewer patients who received pembrolizumab in randomized clinical trials. Begin medical management as clinically indicated. Pembrolizumab therapy may need to be interrupted or discontinued depending on severity; treatment with systemic corticosteroids may also be necessary.[57889]
Immune-mediated thyroid disorders including hypothyroidism and thyroiditis have been reported with pembrolizumab therapy. Thyroiditis may present with or without endocrinopathy; hypothyroidism may follow hyperthyroidism. Hypothyroidism occurred in 8% to 26% (grade 3 or 4, 0.7% or less) of patients treated with pembrolizumab as monotherapy or in combination with cytotoxic chemotherapy; thyroiditis occurred in 0.6% to 2% of patients receiving pembrolizumab monotherapy. Hypothyroidism was reported in 35% (grade 3 or 4, 0.2%) of patients who received pembrolizumab plus axitinib and in 57% to 67% (grade 3 or 4, 0.9% to 1%) of patients who received pembrolizumab plus lenvatinib in clinical trials. Immune-mediated hypoparathyroidism was reported in less than 1% of patients who received pembrolizumab or other PD-1/PD-L1 blocking antibodies. Begin hormone replacement as clinically indicated. Pembrolizumab therapy may need to be interrupted or discontinued depending on severity; treatment with systemic corticosteroids may also be necessary.[57889]
Immune-mediated interstitial nephritis occurred in 0.3% (grade 3 or 4, 0.1%) of patients who received pembrolizumab in clinical trials; 89% were treated with systemic corticosteroids, which resulted in resolution in 56%. After improvement, all patients who had pembrolizumab therapy held for nephritis resumed therapy without recurrence of nephritis. An interruption or discontinuation of therapy may be necessary; treatment with systemic corticosteroids and other systemic immunosuppressants may also be necessary. Increased creatinine occurred in 11% to 39% (grade 3 or 4, 5% or less) of patients treated with pembrolizumab monotherapy, in 21% to 45% (grade 3 or 4, 2% to 7%) of those who received pembrolizumab in combination with cytotoxic chemotherapy, and in 69% to 71% (grade 3 or 4, 3.2% to 3.3%) of patients treated with pembrolizumab plus enfortumab vedotin. In patients with renal cell cancer (RCC), increased creatinine occurred in 43% of those treated with pembrolizumab plus axitinib compared with 40% of those who received sunitinib (grade 3 or 4, 4.3% vs. 2.4%) and in another trial, 61% of patients treated with pembrolizumab plus lenvatinib versus 61% of those who received sunitinib (grade 3 or 4, 5% vs. 2%). Acute kidney injury (AKI) including azotemia, increased creatinine, renal failure, renal impairment, oliguria, decreased glomerular filtration rate, and toxic nephropathy occurred in 13% to 21% (grade 3 or 4, 1.2 to 5%) of patients with RCC treated with pembrolizumab monotherapy or in combination with lenvatinib; it was reported in at least 1% and up to 7% of patients treated with pembrolizumab as monotherapy or in combination with chemotherapy in other clinical trials. Serious cases of urinary retention occurred in 2.5% of patients with advanced urothelial cancer treated with pembrolizumab plus enfortumab vedotin. Fatal cases of acute renal failure were reported in 0.4% of patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 clinical trial.[57889]
Severe or life-threatening infusion-related reactions, including hypersensitivity and anaphylaxis/anaphylactoid reactions occurred in 0.2% of patients who received pembrolizumab across clinical trials (n = 2,799). Monitor patients for signs and symptoms of infusion-related reactions including rigors, chills, wheezing, itching, flushing, rash, hypotension, hypoxemia, and fever. Stop the infusion and permanently discontinue pembrolizumab in patients who develop grade 3 or 4 infusion-related reactions. Hypersensitivity (4.1%) and infusion reactions (9% or less) were reported in patients with classical Hodgkin lymphoma who received pembrolizumab monotherapy in clinical trials. Allergic reactions led to a discontinuation of therapy in 0.4% of patients with unresectable or metastatic melanoma in another clinical trial.[57889]
Proteinuria (including hemoglobinuria and nephrotic syndrome) occurred in 29% (grade 3 or 4, 6%) and 30% (grade 3 or 4, 8%) of patients with endometrial cancer and renal cell cancer, respectively, who received lenvatinib plus pembrolizumab in randomized clinical trials.[57889]
Cough was reported in 11% to 26% (grade 3 or 4, 2% or less) of patients who received pembrolizumab as monotherapy or in combination with cytotoxic chemotherapy, axitinib, or lenvatinib in clinical trials. Dyspnea occurred in 23% or less (grade 3 or 4, 11% or less) of patients who received single-agent pembrolizumab and in 10% to 21% (grade 3 or 4, 1.8% to 3.7%) of patients who received pembrolizumab plus platinum-containing chemotherapy in clinical trials. In some studies, the term cough included upper-airway cough syndrome; the term dyspnea included wheezing. Pleural effusion was reported in 2.2% of patients with non-small cell lung cancer who received single-agent pembrolizumab (n = 636) and in 2% or more of patients with head and neck squamous cell cancer who received single-agent pembrolizumab (n = 192) in clinical trials. One fatality due to pleural effusion was reported in a patient with renal cell carcinoma who received pembrolizumab plus axitinib.[57889]
Immune-mediated pneumonitis occurred in 3.4% (grade 3 or 4, 1.2%; grade 5, 0.1%) of patients who received pembrolizumab in clinical trials (n = 2,799). The incidence of pneumonitis is higher in patients who have received prior thoracic radiation therapy, except in patients with classical Hodgkin lymphoma (cHL). Monitor patients for signs and symptoms of pneumonitis. If confirmed, pembrolizumab therapy may need to be interrupted or discontinued; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary. Of patients who experienced pneumonitis after single-agent pembrolizumab therapy, 67% received systemic corticosteroids, with resolution occurring in 59% of patients. All patients who had pembrolizumab therapy held for pneumonitis resumed therapy after symptoms improvement; of these, 23% had a recurrence of pneumonitis. Pneumonitis/interstitial lung disease (ILD) was reported in 7% to 10% (grade 3 or higher, 1% to 9%) of pembrolizumab-treated patients in individual clinical trials; fatal cases of pneumonitis have been reported.[57889]
Peripheral edema was reported in 11% to 15% (grade 3 or 4, 2% or less) of patients with urothelial cancer, bladder, cancer, or cervical cancer treated with pembrolizumab monotherapy in separate clinical trials. Peripheral edema occurred in 26% of patients who received treatment with pembrolizumab in combination with enfortumab vedotin, and was responsible for an interruption of therapy in 2% of patients with endometrial cancer treated with pembrolizumab plus lenvatinib in a nonrandomized, multicohort study. Generalized edema was responsible for discontinuation of therapy in 1% of patients with ipilimumab-refractory melanoma receiving pembrolizumab monotherapy in a randomized clinical trial (n = 357). Additionally, facial edema occurred in 10% (grade 3 or 4, 2.1) of pembrolizumab-treated patients with head and neck cancer (n = 192).[57889]
Fever was reported in 11% to 28% (grade 3 or 4, 1.3% or less) of adult patients treated with pembrolizumab monotherapy or in combination with chemotherapy at doses ranging from a 200 mg flat dose to 10 mg/kg across various clinical trials in multiple disease states. Fever was among the most common serious adverse reactions reported in patients with endometrial cancer treated with pembrolizumab plus lenvatinib (3%) and in patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin (2.4%) in 2 clinical trials. The incidence of fever (33%) in pediatric patients (age range, 6 months to 17 years) with various cancers who received pembrolizumab 2 mg/kg IV every 3 weeks was at least 10% higher compared with adults.[57889]
Fatigue was reported in 20% to 43% (grade 3 or 4, 6% or less) of patients who received pembrolizumab monotherapy in clinical trials; the incidence was higher in patients who received pembrolizumab plus cytotoxic chemotherapy (26% to 70%; grade 3 or 4, 1% to 12%) or axitinib, lenvatinib, or enfortumab vedotin (51% to 58%; grade 3 or 4, 5% to 11%). The term fatigue included asthenia, malaise, and lethargy in some trials. Asthenia was reported in 11% or fewer (grade 3 or 4, 2% of less) patients who received single-agent pembrolizumab.[57889]
Immune-mediated neurologic toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include meningitis, encephalitis, myelitis and demyelination, myasthenic syndrome/myasthenia gravis (including exacerbation), Guillain-Barre syndrome, nerve paresis, and autoimmune neuropathy; cases may be severe or fatal. Pembrolizumab may need to be interrupted or discontinued depending on the severity of the neurotoxicity; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary. Myositis occurred in 1% of patients receiving pembrolizumab monotherapy in 1 clinical trial and in 0.5% to 3.3% of patients receiving pembrolizumab in combination with enfortumab vedotin 2 other trials; autoimmune myositis with respiratory failure resulted in death in 1 patient who was treated with pembrolizumab monotherapy. Myelitis occurred in 0.5% of patients receiving pembrolizumab monotherapy in 1 clinical trial, and myasthenia gravis occurred in 2.5% of patients treated with pembrolizumab plus enfortumab vedotin. Peripheral neuropathy was reported in 10% or fewer (grade 3 or 4, 0.7%) patients who received pembrolizumab as a single-agent, 14% (grade 3 or 4, 1.1%) of patients treated with pembrolizumab in combination with only platinum-containing chemotherapy, and 31% to 67% (grade 3 or 4, 8% or less) of patients who received pembrolizumab in combination with other cytotoxic chemotherapy. The term peripheral neuropathy included sensory and motor peripheral neuropathy, hypoesthesia, paresthesias, dysesthesia, and polyneuropathy.[57889]
Immune-mediated dermatologic/skin toxicity occurred in 1.4% (grade 3, 1%) of patients who received pembrolizumab in clinical trials (n = 2,799). Monitor patients for suspected severe skin reactions including exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms (DRESS); exclude other causes. Topical emollients and/or topical corticosteroids may be adequate to treat mild-to-moderate non-exfoliative rashes. Pembrolizumab therapy may need to be interrupted or discontinued depending on the severity of rash; treatment with systemic corticosteroids may also be necessary. In clinical trials, 40% of patients who experienced skin toxicity received systemic corticosteroids; skin toxicity resolved in 79% of patients. All patients who had pembrolizumab therapy held for skin toxicity resumed therapy after symptoms improvement; of these, 6% had a recurrence of skin toxicity. Rash was reported in 11% to 52% (grade 3 or 4, 5% or less) of patients who received pembrolizumab as a single-agent or in combination with chemotherapy, axitinib, or lenvatinib in clinical trials; the incidence was higher in patients treated with pembrolizumab in combination with enfortumab vedotin (68% to 71%; grade 3 or 4, 15% to 21%). The term rash included acneiform rash, butterfly rash, erythematous rash/erythema, eczema, asteatotic eczema, follicular rash/folliculitis, maculopapular rash, and pruritic rash, genital rash, pustular rash, atopic dermatitis, contact dermatitis, bullous rash, exfoliative dermatitis/rash, erythema multiforme, seborrheic dermatitis/seborrhea, psoriaform rash/dermatitis, palmar-plantar erythrodysesthesia (hand and foot syndrome), lichenoid keratosis, skin discoloration, perineal rash, eyelid rash, vesicular rash, injection site rash, morbilliform rash, rubelliform rash, vasculitic rash, viral rash, and urticaria in some trials. Vitiligo including skin hypopigmentation occurred in 13% of patients with melanoma who received single-agent pembrolizumab 10 mg/kg IV every 2 or 3 weeks in a randomized trial. Hand and foot syndrome was reported in 23% to 29% (grade 3 or 4, 2.9% to 5%) of patients who received pembrolizumab in combination with axitinib or lenvatinib in separate randomized clinical trials. DRESS resulting in death occurred in 1 patient with melanoma who was treated with pembrolizumab. Xerosis occurred in 17% to 21% (grade 3 or 4, 0.8% or less) of patients who received treatment with pembrolizumab in combination with enfortumab vedotin.[57889]
Pruritus was reported in 11% to 41% (grade 3 or 4, 3.3% or less) of pembrolizumab-treated patients across clinical trials.[57889]
Alopecia occurred in 31% to 61% (grade 3 or 4, 0.8% or less) of patients who received pembrolizumab in combination with cytotoxic chemotherapy.[57889]
Musculoskeletal pain (19% to 41%; grade 3 or 4, 5% or less), arthralgia (18% or less; grade 3 or 4, 1.4% or less), back pain (12% or less; grade 3 or 4, 1.5% or less), myalgia (12% or less; grade 3 or 4, 1% or less), neck pain (6% or less; grade 3 or 4, 0.7% or less), and generalized pain (22% or less; grade 3 or 4, 2% or less) were reported in patients who received pembrolizumab monotherapy in clinical trials. Musculoskeletal pain was also reported in 22% (grade 3 or 4, 1.9%) of patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 clinical trial. Musculoskeletal disorders (53% to 58%; grade 3 or 4, 4% to 5%) and elevated creatine kinase concentrations (19% to 24%; grade 3 or 4, 3.7% to 6%) occurred in patients treated with pembrolizumab plus lenvatinib. The terms musculoskeletal pain and/or musculoskeletal disorders included arthralgia, back pain, myalgia, myositis, bone pain/spinal pain, extremity pain, musculoskeletal chest pain/discomfort, neck pain, arthritis, breast pain, stiffness, and jaw pain. The term generalized pain including breast pain, cancer pain, dysuria, ear pain, gingival pain, groin pain, lymph node pain, oropharyngeal pain, skin pain, radicular pain, stoma site pain, and toothache/dental pain. Arthralgia (29% or less; grade 3 or 4, 1.7% or less) and myalgia (20% or less; grade 3 or 4, 0.5% or less) occurred in patients receiving pembrolizumab in combination with cytotoxic chemotherapy.[57889]
Immune-mediated hematologic hemolytic anemia and aplastic anemia were reported in less than 1% of patients who received pembrolizumab or other PD-1/PD-L1 blocking antibodies in clinical trials. Therapy may need to be interrupted or discontinued, depending on the severity of the reaction; treatment with systemic corticosteroids and other systemic immunosuppressants may also be necessary. Anemia was reported in patients who received pembrolizumab as monotherapy (17% to 54%; grade 3 or 4, 24% or less), and in combination with platinum-containing chemotherapy (65% to 97%; grade 3 or 4, 12% to 35%), enfortumab vedotin (53% to 69%; grade 3 or 4, 7% to 15%), axitinib (29%; grade 3 or 4, 2.1%), and lenvatinib (38% to 49%; grade 3 or 4, 3% to 8%) in clinical trials. The incidence of grade 3 anemia (17%) in pediatric patients with various cancers who received pembrolizumab 2 mg/kg IV every 3 weeks was at least 10% higher compared with adults.[57889]
Lymphopenia was reported in 10% to 54% (grade 3 or 4, 25% or less) of patients who received single-agent pembrolizumab; 57% to 99% (grade 3 or 4, 15% to 96%) of patients who received pembrolizumab plus chemotherapy including enfortumab vedotin; 33% (grade 3 or 4, 11%) of patients who received pembrolizumab plus axitinib; and 51% to 54% (grade 3 or 4, 9% to 18%) of patients who received pembrolizumab plus lenvatinib in clinical trials. Neutropenia occurred in 39% or fewer (grade 3 or 4, 15% or less) patients who received single-agent pembrolizumab; 32% to 88% (grade 3 or 4, 4% to 62%) of patients who received pembrolizumab plus chemotherapy, axitinib, or lenvatinib. Febrile neutropenia was reported in 1% to 15% of pembrolizumab-treated patients. Leukopenia occurred in 47% or fewer patients (grade 3 or 4, 12% or fewer) who received pembrolizumab monotherapy; 34% to 43% (grade 3 or 4, 1% to 3.5%) of patients who received pembrolizumab plus lenvatinib; and in 59% to 93% (grade 3 or 4, 7% to 48%) of patients treated with pembrolizumab in combination with cytotoxic chemotherapy in other clinical trials. The incidence of leukopenia (31%) and neutropenia (28%) in pediatric patients (age range, 6 months to 17 years) with various cancers who received pembrolizumab 2 mg/kg IV every 3 weeks was at least 10% higher compared with adults.[57889]
Thrombocytopenia occurred in 32% or fewer (grade 3 or 4, 9% or less) patients who received single-agent pembrolizumab; 22% to 73% (grade 3 or 4, 1.7% to 19%) of patients who received pembrolizumab plus cytotoxic chemotherapy; 27% (grade 3 or 4, 1.4%) of patients who received pembrolizumab plus axitinib; and 39% to 50% (grade 3 or 4, 2% to 8%) of patients who received pembrolizumab plus lenvatinib in clinical trials. The incidence of thrombocytopenia (22%) in pediatric patients with various cancers who received pembrolizumab 2 mg/kg IV every 3 weeks was at least 10% higher compared with adults.[57889]
Cases of infection, some fatal, have been reported in patients treated with pembrolizumab across clinical trials including urinary tract infections (11% to 35%; grade 3 or 4, 12% or less), pneumonia (8% to 19%; grade 3 or 4, 1% to 11%), upper respiratory infections (11% to 41%; grade 3 or 4, 2.6% or less), nasopharyngitis (10%), influenza-like illness (11%), herpes virus infection (9%), COVID-19 (10% or less) including fatal cases, and sepsis (1% or more); additional infections have included autoimmune encephalitis, cellulitis, Clostridium difficile, cystitis, device-related infections, empyema, erysipelas, herpes virus infection, infected neoplasm, influenza, lower respiratory tract congestion, lung infection, oral candidiasis, osteomyelitis, pelvic infection, pharyngotonsillitis, pharyngitis, rhinorrhea, rhinitis, sinusitis, tooth abscess, uterine abscess, and vulvovaginal candidiasis.[57889]
Hypophosphatemia occurred in 19% to 51% (grade 3 or 4, 4.7% to 15%) of patients who received pembrolizumab as monotherapy or in combination with other drugs in clinical trials. Hyponatremia was reported in 10% to 46% (grade 3 or 4, 3.3% to 18%) of patients treated with monotherapy and in 28% to 60% (grade 3 or 4, 3.9% to 20%) of those who received pembrolizumab in combination with chemotherapy. Decreased bicarbonate/metabolic acidosis (22% or less; grade 3 or 4, 0.4% or less) occurred in ipilimumab-refractory melanoma patients who received single-agent pembrolizumab in 1 randomized trial.[57889]
Hypocalcemia occurred in 20% to 27% (grade 3 or 4, 2.5% or less) of patients treated with pembrolizumab monotherapy and in 22% to 56% (grade 3 or 4, 0.2% to 5%) of those who received pembrolizumab in combination with chemotherapy or oral targeted therapy in clinical trials. Hypercalcemia was reported in 14% to 27% (grade 3 or 4, 0.7% to 4.5%) of patients treated with pembrolizumab as monotherapy or in combination with other agents; fatal cases of hypercalcemia were reported in 0.4% of patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 clinical trial.[57889]
Hyperkalemia was reported in 13% to 28% (grade 3 or 4, 0.8% to 3%) of patients treated with pembrolizumab monotherapy in clinical trials and in 20% to 44% (grade 3 or 4, 1.4% to 9%) of those who received pembrolizumab in combination with chemotherapy or oral targeted therapies. Hypokalemia was primarily reported in combination with other anticancer treatments (20% to 45%; grade 3 or 4, 4.4% to 15%) but was reported in 19% to 20% (grade 3 or 4, 5% to 6%) of patients who received pembrolizumab monotherapy in 2 clinical trials.[57889]
Hypomagnesemia was reported in 15% to 23% of patients treated with pembrolizumab monotherapy (grade 3 or 4, 0.4% or less) and in 25% to 59% of those who received pembrolizumab in combination with cytotoxic chemotherapy or lenvatinib in clinical trials. Hypermagnesemia occurred in 23% (grade 3 or 4, 2%) of patients with renal cell carcinoma who received pembrolizumab plus lenvatinib in 1 randomized trial.[57889]
Immune-mediated cardiovascular toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include myocarditis, pericarditis, and vasculitis; cases may be severe or fatal. Pembrolizumab therapy may need to be to be interrupted or discontinued in patients who develop immune-mediated toxicity, depending on the severity of the reaction; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary. Myocarditis was reported in 1.4% of patients with classical Hodgkin lymphoma who received pembrolizumab in clinical trials. Myocarditis has been reported in postmarketing surveillance of pembrolizumab. Death due to myocarditis occurred in patients with renal cell carcinoma who received pembrolizumab and axitinib (n = 1) or levatinib (n = 1). Pericarditis occurred in 4% of patients with primary mediastinal large B-cell lymphoma who received pembrolizumab in a clinical trial (n = 53).[57889]
Type 1 diabetes mellitus (which may present with diabetic ketoacidosis) has been reported with pembrolizumab therapy. Monitor patients for hyperglycemia and other signs and symptoms of diabetes. Withhold pembrolizumab therapy for cases of severe hyperglycemia until blood sugar control is achieved; administer insulin as clinically indicated. Type 1 diabetes mellitus occurred in 0.2% of patients who received pembrolizumab in clinical trials. All patients who developed diabetes required long-term insulin therapy. Hyperglycemia occurred in 33% to 59% (grade 3 or 4, 1.3% to 8%) of patients treated with pembrolizumab monotherapy and in 51% to 74% (grade 3 or 4, 4.3% to 14%) of those who received pembrolizumab in combination with other anticancer therapy in clinical trials; diabetic ketoacidosis occurred in 1% of patients with renal cell cancer who received pembrolizumab monotherapy in 1 clinical trial. Hypoglycemia occurred in 13% to 20% (grade 3 or 4, 1.3% or less) of patients treated with pembrolizumab monotherapy in 2 clinical trials and in 44% (grade 3 or 4, 2%) of patients who received pembrolizumab plus lenvatinib in another. Decreases from baseline in glucose were reported in 17% of patients who received pembrolizumab plus trastuzumab and fluoropyrimidine- and platinum-containing chemotherapy in a different clinical trial.[57889]
Headache was reported in 15% or fewer (grade 3 or 4, 2% or less) patients who received single-agent pembrolizumab and in 11% to 30% (grade 3 or 4, 1% or less) of patients receiving pembrolizumab in combination with other anticancer drugs. The term headache included tension headache and migraine. The incidence of headache (25%) in pediatric patients (age range, 6 months to 17 years) with various cancers who received pembrolizumab was at least 10% higher compared with adults. Dizziness occurred in 5% (grade 3 or 4, 0.3%) of patients with HNSCC who received single-agent pembrolizumab and 10% (grade 3 or 4, 0.4%) of HNSCC patients who received pembrolizumab plus platinum-containing chemotherapy. Dizziness was reported in 23% of patients treated with pembrolizumab in combination with enfortumab vedotin.[57889]
Primary or secondary adrenocortical insufficiency and immune-mediated hypophysitis have been reported with pembrolizumab therapy. Initiate symptomatic treatment including hormone replacement therapy for grade 2 or higher adrenal insufficiency and for hypophysitis as clinically indicated. Pembrolizumab therapy may need to be interrupted or discontinued depending on severity; treatment with systemic corticosteroids may also be necessary. Adrenal insufficiency (0.8%; grade 3 or 4, 0.3%) and immune-mediated hypophysitis (0.6%; grade 3 or 4, 0.3%) occurred in patients who received pembrolizumab in clinical trials (n = 2,799). Of patients that developed adrenal insufficiency or hypophysitis, 77% and 94% received systemic corticosteroids, respectively; additionally, the majority of these patients remained on corticosteroids. Hypophysitis can present with acute symptoms associated with mass effect such as photophobia or visual field defects; hypophysitis may lead to hypopituitarism. Adrenal insufficiency was reported in 3% of patients with endometrial cancer treated with pembrolizumab plus lenvatinib in a nonrandomized study (n = 94).[57889]
Antibody formation occurred in 27 patients (2.1%) who received pembrolizumab in clinical studies (n = 1,289). Of these, neutralizing antibodies were confirmed in 6 patients (0.5%).[57889]
Cardiac arrhythmias including atrial fibrillation, sinus tachycardia, and supraventricular tachycardia (SVT) (11%; grade 3 or 4, 4%), pericardial effusion (2%), cardiac tamponade (2%), myocardial infarction (MI) (2%), and pericarditis (4%; grade 3 or 4, 2%) have been reported in patients with primary mediastinal large B-cell lymphoma who received pembrolizumab in a nonrandomized trial. MI (3%) and angina pectoris (1%) occurred in patients with renal cell carcinoma who received pembrolizumab plus lenvatinib in a randomized trial; fatal cardiovascular events included arrhythmia (0.3%) and multiple organ dysfunction syndrome (0.3%). Additionally, pembrolizumab therapy was discontinued due to heart failure in 0.4% of patients with ipilimumab-naive, unresectable or metastatic melanoma treated with pembrolizumab 10 mg/kg every 2 or 3 weeks in a randomized clinical trial. Fatal cases of respiratory/cardiac arrest and myocardial infarction have also occurred with pembrolizumab therapy.[57889]
Hypercholesterolemia (20%; grade 3 or 4, 0.7% to 1.2%) and hypertriglyceridemia (33% to 43%; grade 3 or 4, 2.6% or less) were reported in patients with advanced melanoma or non-small cell lung cancer (NSCLC) who received pembrolizumab at doses of either 2 mg/kg or 10 mg/kg (n = 1,594) in separate clinical trials. The incidence of hypercholesterolemia (53% to 64%; grade 3 or 4, 3.2% to 5%) and hypertriglyceridemia (70% to 80%; grade 3 or 4, 6% to 15%) were increased in patients treated with pembrolizumab plus lenvatinib in randomized trials.[57889]
Fatal and serious adverse events occurred in patients who received an allogeneic hematopoietic stem-cell transplant (HSCT) prior to and after treatment with a PD-1/PD-L1 blocking antibody, such as pembrolizumab. Monitor patients closely for evidence of transplant-related complications such as hyperacute graft-versus-host disease (GVHD), acute GVHD, chronic GVHD, sinusoidal obstruction syndrome (SOS) previously termed veno-occlusive disease (VOD) after reduced intensity conditioning, and steroid-requiring febrile syndrome (without an identified infectious cause); treat adverse events promptly. These complications may occur despite intervening therapy between PD-1 blockade and allogeneic HSCT.GVHD occurred in 1% or more of patients with classical Hodgkin lymphoma (n = 206) who received pembrolizumab in a clinical study; 1 patients died from GVHD after subsequent allogeneic SCT.[57889]
Immune-mediated toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include hemophagocytic lymphohistiocytosis, systemic inflammatory response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi lymphadenitis), sarcoidosis, immune thrombocytopenic purpura, and solid organ transplant rejection and other transplant rejection including corneal graft rejection; cases may be severe or fatal. Pembrolizumab therapy may need to be interrupted or discontinued in patients who develop immune-mediated toxicity, depending on the severity of the reaction; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary.[57889]
Prolonged bleeding time including increased INR and increased activated partial thromboplastin time occurred in 10% to 29% of patients treated with pembrolizumab monotherapy or in combination with other anticancer treatments in several clinical trials. Bleeding/hemorrhage was reported in 19% of patients who received pembrolizumab monotherapy in a single-arm, nonrandomized trial (grade 3 or 4, 5%); serious hemorrhagic events were reported in 0.8% to 4.1% of patients treated with pembrolizumab plus chemotherapy. Bleeding events occurred in 25% to 27% of patients treated with pembrolizumab plus lenvatinib in 2 clinical trials (grade 3 or 4, 2.6% to 5%). The term "bleeding" or "hemorrhage" included blood blister, coital bleeding, contusion, disseminated intravascular coagulation (DIC), ecchymosis, epistaxis, GI bleeding, hematemesis, hematochezia, hematoma, hematuria, hemoptysis, hemothorax, injection site bleeding or bruising, intracranial bleeding, Mallory-Weiss syndrome, melena, metrorrhagia, mouth bleeding, ocular hemorrhage, petechiae, pulmonary hemorrhage, purpura, rectal bleeding, renal or urinary tract bleeding, retroperitoneal hemorrhage, ruptured aneurysm, stoma site hemorrhage, subdural hematoma, thrombotic thrombocytopenic purpura (TTP), tumor bleeding, umbilical hemorrhage, uterine hemorrhage, vaginal bleeding, and wound hemorrhage. Fatal bleeding events including aneurysm rupture, subarachnoid hemorrhage, pulmonary hemorrhage, and GI bleeding have also been reported in patients treated with pembrolizumab. Hematuria occurred in 12% to 19% of patients treated with pembrolizumab monotherapy in 3 clinical trials and was grouped with the term "bleeding" in several others (grade 3 or 4, 1.4% to 3%); serious cases of hematuria were reported in 3.3% of patients with advanced urothelial cancer who received pembrolizumab in combination with enfortumab vedotin in 1 clinical trial.[57889]
Confusion occurred in at least 2% of patients with recurrent or metastatic head and neck cancer who received pembrolizumab in an open-label, single-arm clinical trial (n = 192). Additionally, confusion (4%) was among the commonly reported serious adverse reactions in patients with endometrial cancer treated with pembrolizumab plus lenvatinib in a nonrandomized, multicohort study.[57889]
Dysphonia was reported in 22% to 30% (grade 3 or 4, 0.2% or less) of patients treated with pembrolizumab plus either axitinib or lenvatinib in separate clinical trials.[57889]
Hypertension was reported in 48% (grade 3 or 4, 24%) of patients who received pembrolizumab plus axitinib, 56% to 67% (grade 3 or 4, 29% to 39%) of patients who received pembrolizumab plus lenvatinib, and 24% (grade 3 or 4, 9%) of patients who received pembrolizumab plus chemotherapy with or without bevacizumab in clinical trials. Fatal hypertensive crisis occurred in 1 patient (0.3%) who received pembrolizumab plus lenvatinib. The term hypertension included hypertensive crisis, labile hypertension, hypertensive encephalopathy, and hypertensive retinopathy.[57889]
Insomnia occurred in 7% to 10% (grade 3 or 4, 0.7% or less) of patients with advanced head and neck cancer treated with pembrolizumab as monotherapy or in combination with platinum-based chemotherapy. In another clinical trial, 21% (grade 3 or 4, 0.5%) of patients with high-risk, early stage triple-negative breast cancer experienced insomnia during neoadjuvant treatment with pembrolizumab in combination with carboplatin/paclitaxel followed by doxorubicin/cyclophosphamide. Altered mental state was reported in 2.7% of patients with classical Hodgkin lymphoma who received pembrolizumab monotherapy in a randomized trial.[57889]
Immune-mediated toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include pancreatitis and increases in serum amylase levels/hyperamylasemia and lipase levels; cases may be severe or fatal. Pembrolizumab therapy may need to be interrupted or discontinued in patients who develop immune-mediated toxicity, depending on the severity of the reaction; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary. In pooled results from 2 trials (n = 105), grade 3 or 4 increased lipase level was reported in 17% of patients with advanced Merkel cell carcinoma who received pembrolizumab. Hyperamylasemia (25% to 59%; grade 3 or 4, 6% to 17%) and increased lipase level (36% to 61%; grade 3 or 4, 14% to 34%) occurred in patients who received pembrolizumab plus lenvatinib in a randomized trial. An increase in lipase from baseline was also reported in 59% (grade 3 or 4, 32%) of patients who received treatment with pembrolizumab in combination with enfortumab vedotin. Exocrine pancreatic insufficiency has been reported in postmarketing experience with pembrolizumab.[57889]
Fatal reversible posterior leukoencephalopathy syndrome (RPLS) was reported in a nonrandomized, multicohort study of patients with endometrial cancer treated with pembrolizumab plus lenvatinib.[57889]
Fatal intestinal/GI perforation was reported in patients with endometrial cancer treated with pembrolizumab plus lenvatinib and in patients with cervical cancer who received pembrolizumab plus chemotherapy with or without bevacizumab.[57889]
Muscle weakness was responsible for discontinuation of therapy in 2% of patients with endometrial cancer treated with pembrolizumab plus lenvatinib in a nonrandomized, multicohort study.[57889]
Syncope was responsible for interruption of therapy in 2% of patients with endometrial cancer treated with pembrolizumab plus lenvatinib in a nonrandomized, multicohort study.[57889]
Pulmonary embolism occurred in 2% of patients with high-risk non-muscle invasive bladder cancer in a multicenter, noncomparative trial. Fatal mesenteric thrombosis/thromboembolism was reported in 0.4% of patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 clinical trial. A fatal event involving a cerebrovascular accident and femur fracture with perioperative pulmonary embolus occurred in 1 patient with cervical cancer who received pembrolizumab plus chemotherapy with or without bevacizumab in a randomized trial.[57889]
Tumor flare was reported in 1.4% of patients with classical Hodgkin lymphoma who received pembrolizumab monotherapy (n = 148) in a randomized trial.[57889]
Immune-mediated ocular toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include uveitis, iritis, and other ocular inflammation toxicity; some cases may be associated with retinal detachment. Pembrolizumab therapy may need to be interrupted or discontinued in patients who develop immune-mediated toxicity, depending on the severity of the reaction. Patients may require treatment with systemic corticosteroids to reduce the risk of permanent vision loss. Visual impairment including vision loss/blindness may occur. If uveitis occurs in combination with other immune-mediated adverse reactions, consider a diagnosis of Vogt-Koyanagi-Harada syndrome. Uveitis was reported in 1.4% or less of patients with classical Hodgkin lymphoma who received pembrolizumab in clinical trials. Xerophthalmia (24% to 25%) and blurred vision (6%) were reported in patients treated with pembrolizumab in combination with enfortumab vedotin.[57889]
Immune-mediated arthritis occurred in 1.5% of patients who received pembrolizumab therapy. Other immune-mediated musculoskeletal toxicity that was reported in less than 1% of patients who received pembrolizumab or that occurred with the use of other PD-1/PD-L1 blocking antibodies include myositis/polymyositis, rhabdomyolysis (and associated sequelae, including renal failure) and polymyalgia rheumatica; cases may be severe or fatal. Pembrolizumab therapy may need to be to be interrupted or discontinued in patients who develop immune-mediated toxicity, depending on the severity of the reaction; treatment with systemic corticosteroids and other systemic immunosuppressants may be necessary. Myositis was reported in 0.5% of patients with classical Hodgkin lymphoma who received pembrolizumab in a clinical trial (n = 210). Autoimmune myositis with respiratory failure resulted in death in 1 patient with melanoma who was treated with pembrolizumab. Arthritis was reported in 2% of patients with primary mediastinal B-cell lymphoma who received pembrolizumab in a clinical trial (n = 53).[57889]
An injection site reaction/extravasation occurred in 0.8% to 2% of patients who received treatment with pembrolizumab in combination with enfortumab vedotin.[57889]
Immune-mediated reactions, which may be severe or fatal, can occur in patients treated with drugs that bind to either the programmed death-receptor 1 (PD-1) or the PD-ligand 1 (PD-L1), thus removing inhibition of the immune response, such as pembrolizumab. These immune-mediated reactions can occur in any organ system or tissue and can also affect more than one body system simultaneously. Although usually occurring during treatment with PD-1/PD-L1 inhibitors, immune-mediated reactions can occur at any time after starting therapy including after discontinuation of therapy. Because early identification and management is critical to safe usage of PD-1/PD-L1 inhibitors, closely monitor patients for signs and symptoms that may be clinical manifestations of underlying immune-mediated reactions. Initiate an appropriate workup to exclude alternative etiologies including infection in cases of suspected immune-mediated reaction. Begin medical management promptly, including specialty consultation as appropriate. An interruption or discontinuation of pembrolizumab therapy may be necessary, depending on the severity of the reaction. In general, if an interruption or discontinuation of therapy is necessary, administer systemic corticosteroids (1 to 2 mg/kg per day of prednisone or equivalent); upon improvement to grade 1 or less, begin a steroid taper over at least 1 month. Consider additional systemic immunosuppression in patients whose symptoms are not controlled with corticosteroid therapy.[57889]
Dry mouth (xerostomia) was reported in 22% (grade 3 or 4, 1.4%) of patients with locally advanced head and neck cancer treated with pembrolizumab in combination with radiotherapy with or without cisplatin in 1 open-label, active controlled trial.[57889]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Use pembrolizumab with caution in patients with a history of autoimmune disease, including inflammatory bowel disease. Immune-mediated reactions, which may be severe or fatal, can occur in patients treated with drugs that bind to either the programmed death-receptor 1 (PD-1) or the PD-ligand 1 (PD-L1), thus removing inhibition of the immune response, such as pembrolizumab. These immune-mediated reactions can occur in any organ system or tissue and can also affect more than one body system simultaneously. Although usually occurring during treatment with PD-1/PD-L1 inhibitors, immune-mediated reactions can occur at any time after starting therapy including after discontinuation of therapy. Because early identification and management is critical to safe usage of PD-1/PD-L1 inhibitors, closely monitor patients for signs and symptoms that may be clinical manifestations of underlying immune-mediated reactions. Initiate an appropriate workup to exclude alternative etiologies including infection in cases of suspected immune-mediated reaction. Begin medical management promptly, including specialty consultation as appropriate. An interruption or discontinuation of pembrolizumab therapy may be necessary, depending on the severity of the reaction. In general, if an interruption or discontinuation of therapy is necessary, administer systemic corticosteroids (1 to 2 mg/kg per day of prednisone or equivalent); upon improvement to grade 1 or less, begin a steroid taper over at least 1 month. Consider additional systemic immunosuppression in patients whose symptoms are not controlled with corticosteroid therapy.[57889] [72085]
Use pembrolizumab with caution in patients who have a history of pre-existing pulmonary disease; immune-mediated pneumonitis/interstitial lung disease has been reported in patients treated with pembrolizumab. The incidence is higher in patients who have received prior thoracic radiation therapy, except in patients with classical Hodgkin lymphoma, where pneumonitis rates were similar regardless of prior thoracic radiation. Monitor patients for signs and symptoms of pneumonitis (e.g., new or worsening cough, chest pain, shortness of breath). If confirmed, pembrolizumab therapy may need to be interrupted or discontinued depending on severity; treatment with systemic corticosteroids may be necessary.[57889] [72085]
Perform a risk/benefit analysis prior to starting treatment with a PD-1/PD-L1 blocking antibody, such as pembrolizumab, in patients who may receive or who have a history of undergoing an allogeneic stem cell transplant (SCT). Fatal and other serious complications including hyperacute, acute, and chronic graft-versus-host-disease, sinusoidal obstruction syndrome (SOS) previously termed veno-occlusive disease (VOD) after reduced intensity conditioning, and a steroid-requiring febrile syndrome (without an identified infectious cause) have been reported in patients who receive an allogeneic SCT before or after being treated with a PD-1/PD-L1 blocking antibody. Monitor patients closely for evidence of transplant-related complications and intervene promptly. Complications may occur despite intervening therapy between PD-1/PD-L1 blockade and allogeneic SCT.[57889]
Use pembrolizumab with caution in patients who have a history of neurological disease such as myasthenia gravis or Guillain-Barre syndrome. Immune-mediated neurotoxicity has been reported with pembrolizumab or other PD-1/PD-L1 inhibitors. Pembrolizumab may need to be interrupted or discontinued depending on the severity of the neurotoxicity; treatment with systemic corticosteroids may also be necessary.[57889]
Use pembrolizumab with caution in patients who have previously had a solid organ transplant or tissue transplant (including corneal transplant). Immune-mediated organ transplant rejection has been reported with PD-1/PD-L1 inhibitor therapy.[57889]
Monitor patients with obesity as well as those who are considered overweight for an increased risk of infusion-related reactions when treated with pembrolizumab. Patients with a high BMI have a greater risk even if they have a low metabolic risk (i.e., fewer than 2 of diabetes, dyslipidemia, hypertension).[72085] [72101] [72102]
Use pembrolizumab with caution in patients with cardiovascular risk factors such as hypertension, heart failure, cardiac disease, and myocardial infarction as they are at increased risk of cardiac immune-related adverse reactions such as myocarditis, vasculitis, and pericarditis.[72105] [72085]
Pembrolizumab can cause fetal harm when used during pregnancy based on its mechanism of action. There are no available data on the use of pembrolizumab during human pregnancy. A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining immune tolerance to the fetus. Animal studies indicate that PD-1/PD-L1 inhibition may increase the risk of immune-mediated rejection of the developing fetus, resulting in fetal death. Human IgG4 antibodies are known to cross the placenta, so pembrolizumab has the potential to be transmitted to the fetus. Fetal exposure to pembrolizumab may increase the risk of developing immune-mediated disorders or altering the normal immune response. Patients should be counseled on the potential fetal risks.[57889] [66947] [66948] [66949]
Counsel people who may become pregnant about the reproductive risk associated with pembrolizumab. Pembrolizumab can cause fetal harm. Verify pregnancy status prior to treatment initiation. Advise people who may become pregnant to use effective contraception while taking pembrolizumab and for 4 months after the last dose.[57889]
Advise patients to avoid breast-feeding while taking pembrolizumab and for 4 months after the last dose due to the potential for serious adverse reactions in the breastfed child. There are no data on the presence of pembrolizumab in human milk, its effects on the breast-fed child, or its effects on milk production. Maternal IgG is known to be present in human milk.[57889] Pembrolizumab is a large protein molecule (molecular weight of 149,000 Daltons). It is unknown if pembrolizumab is present in human milk; the amount of drug in milk is likely to be very low. Pembrolizumab may be partially destroyed in the gastrointestinal tract, resulting in minimal absorption.[66941] The effects of localized gastrointestinal exposure and limited systemic exposure in the breastfed child to pembrolizumab are unknown.[57889]
Pembrolizumab is a humanized monoclonal IgG4 kappa antibody that binds to the programmed death receptor-1 (PD-1) found on T-cells and blocks the interaction of PD-1 with its ligands, PD-L1 and PD-L2, on the tumor cell. Melanoma and some other solid tumors suppress cytotoxic T-cell activity by over-expressing PD-L1 on the cell surface. Blocking the PD-1/PD-L1 pathway inhibits T-cell proliferation and cytokine production. In mice, inhibiting PD-1 activity deceased tumor growth.[57889] Pembrolizumab differs from ipilimumab, another monoclonal antibody that binds to the cytotoxic T-lymphocyte Antigen-4 (CTLA-4) and blocks the interaction of CTLA-4 with its ligands, in that pembrolizumab blocks the PD-1/PD-L1 interaction peripherally at the tumor site whereas ipilimumab blocks the CTLA4/ligand interaction primarily in the lymphoid organs.[57904] Combination treatment of a PD-1 blocking antibody and lenvatinib decreased tumor-associated macrophages, increased activated cytotoxic T cells, and reduced tumor growth in syngeneic mouse tumor models compared to either treatment alone.[57889]
Revision Date: 10/17/2025, 02:32:46 PMPembrolizumab is administered intravenously. In a population pharmacokinetic analysis (n = 2,993), pembrolizumab clearance was approximately 23% lower at steady state (geometric mean, 195 mL/day; coefficient of variation (CV), 40%) than after the first dose (252 mL/day; CV, 37%); this difference is not considered clinically important. The geometric mean steady-state volume of distribution (Vd) was 6 L (CV, 20%), and the mean terminal half-life was 22 days (CV, 32%).[57889]
In a population pharmacokinetic analysis, steady-state pembrolizumab concentrations were reached by 16 weeks following an every 3-week regimen; the systemic accumulation was approximately 2.1-fold. The pembrolizumab Cmax, Cmin, and AUC at steady state increased proportionally in the dose range of 2 to 10 mg/kg IV every 3 weeks.[57889] In a multicenter, randomized, open-label, dose comparative, phase I study (n = 173), patients with ipilimumab-refractory advanced melanoma received pembrolizumab 2 mg/kg IV or 10 mg/kg IV every 3 weeks. The AUC values were 0.643 grams X day/L (coefficient of variation (CV), 28%) and 3.77 grams X day/L (CV, 33%) in the 2 mg/kg and 10 mg/kg arms, respectively. Pembrolizumab exposure was 5.9 times higher in the 10 mg/kg arm.[57890] A pembrolizumab dosage regimen of 400 mg IV every 6 weeks was compared with 200 mg IV every 3 weeks and 2 mg/kg IV every 3 weeks regimens in a model-based analysis using concentration-time profile simulations from 2,993 subjects with solid tumors (i.e., melanoma, non-small cell lung cancer) from 5 clinical trials. At steady state (days 169 to 210), the average pembrolizumab concentration over the dosage interval (AUC) following the 400 mg IV every 6 weeks regimen was similar to the 200 mg IV every 3 weeks (difference from mean value, 0.7%) and higher than the 2 mg/kg IV every 3 weeks regimen (difference in mean value, 35%). Based on a time-dependent pharmacokinetic (PK) model that evaluated PK parameters across indications, the clearance of pembrolizumab is reduced in patients with Hodgkin lymphoma (HL) or primary mediastinal B-cell lymphoma (PMBCL) tumor types; however, the minor increase in pembrolizumab exposure is not considered clinically significant.[65362] Although there does not appear to be any clinically significant differences in efficacy and safety with pembrolizumab dosages of 200 mg every 3 weeks compared with 400 mg every 6 weeks in patients with solid tumors, the exposure-response relationships for efficacy or safety are not fully known at the pembrolizumab 400 mg every 6 weeks dosage in patients with classical HL or PMBCL.[57889]
Mild to moderate hepatic impairment (total bilirubin less than 3 times the upper limit of normal (ULN) and any AST) had no clinically significant impact on pembrolizumab clearance. Pembrolizumab has not been studied sufficiently in patients with severe hepatic impairment (total bilirubin greater than 3 times ULN and any AST).[57889]
Renal impairment (eGFR 15 mL/min/1.73 m2 or higher) had no clinically significant impact on pembrolizumab clearance in a population pharmacokinetic analysis.[57889]
Following weight-based dosing at 2 mg/kg IV every 3 weeks, pembrolizumab concentrations in pediatric patients (age range, 10 months to 17 years) were comparable to pembrolizumab concentrations in adults who received the same dosage.[57889]
Age (range, 15 to 94 years) had no clinically significant impact on pembrolizumab clearance in a population pharmacokinetic analysis.[57889]
Gender had no clinically significant impact on pembrolizumab clearance in a population pharmacokinetic analysis.[57889]
Race had no clinically significant impact on pembrolizumab clearance in a population pharmacokinetic analysis.[57889]
Tumor Burden
Tumor burden had no clinically significant impact on pembrolizumab clearance in a population pharmacokinetic analysis.[57889]
Pembrolizumab can cause fetal harm when used during pregnancy based on its mechanism of action. There are no available data on the use of pembrolizumab during human pregnancy. A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining immune tolerance to the fetus. Animal studies indicate that PD-1/PD-L1 inhibition may increase the risk of immune-mediated rejection of the developing fetus, resulting in fetal death. Human IgG4 antibodies are known to cross the placenta, so pembrolizumab has the potential to be transmitted to the fetus. Fetal exposure to pembrolizumab may increase the risk of developing immune-mediated disorders or altering the normal immune response. Patients should be counseled on the potential fetal risks.[57889] [66947] [66948] [66949]
Advise patients to avoid breast-feeding while taking pembrolizumab and for 4 months after the last dose due to the potential for serious adverse reactions in the breastfed child. There are no data on the presence of pembrolizumab in human milk, its effects on the breast-fed child, or its effects on milk production. Maternal IgG is known to be present in human milk.[57889] Pembrolizumab is a large protein molecule (molecular weight of 149,000 Daltons). It is unknown if pembrolizumab is present in human milk; the amount of drug in milk is likely to be very low. Pembrolizumab may be partially destroyed in the gastrointestinal tract, resulting in minimal absorption.[66941] The effects of localized gastrointestinal exposure and limited systemic exposure in the breastfed child to pembrolizumab are unknown.[57889]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.