Blood Clot in the Lung (Pulmonary Embolism): What to Know
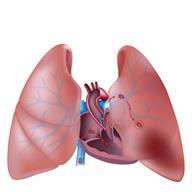
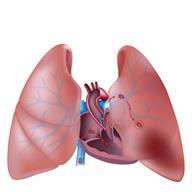
A pulmonary embolism (PE) is when you get a sudden blockage or less blood flow in one or both of your lungs. This typically happens when a blood clot moves into the arteries of your lung. A blood clot is blood that has turned into a gel or solid.
Most blockages come from deep vein thrombosis (DVT). This is when a blood clot forms in the vein of a leg or arm and moves to your lungs.
PE is dangerous. It must be treated right away.
What are the causes?
In most cases, PE is caused by a blood clot that forms in a vein and moves to your lungs.
In rare cases, it may be caused by:
What increases the risk?
You may be more likely to get PE if:
- You get really hurt, such as from:
- You have a big surgery, such as:
- You have certain conditions, such as:
You have a soft tube called a central venous catheter.
You're being treated for cancer.
You take medicines that have estrogen in them.
You smoke.
You spend a lot of time sitting, such as if you travel over 6 hours.
You may also be more likely to get PE if you're:
What are the signs or symptoms?
Symptoms may start all of a sudden. They may include:
Feeling short of breath while moving or resting.
Coughing, coughing up blood, or coughing up bloody mucus.
- Pain that gets worse with deep breaths in your:
Chest.
Back.
Shoulder blade.
A heartbeat that's fast or not normal.
Feeling light-headed or dizzy.
Fainting.
Feeling worried or nervous.
Pain and swelling in a leg. This is a symptom of DVT. DVT can lead to PE.
How is this diagnosed?
PE may be diagnosed based on your medical history, an exam, and tests. Tests may include:
Blood tests.
An electrocardiogram (ECG). This checks how well your heart is working.
A CT pulmonary angiogram. This checks blood flow in and around your lungs.
A ventilation-perfusion scan. This measures air flow and blood flow to your lungs.
An ultrasound to check for a DVT.
How is this treated?
Treatment may depend on what caused the PE, how likely you are to have bleeding, and other conditions you have. Treatment may be done to:
Treatment may include:
- Medicines to:
- Procedures, such as:
An embolectomy. This uses a tube to remove a clot.
Catheter-directed thrombolysis. This uses medicine to get rid of a clot.
Surgical embolectomy. This is a surgery to get rid of the clot. It's used in rare cases.
You may need more than one treatment. Work with your provider to choose the best treatment program for you.
Follow these instructions at home:
Medicines
General instructions
-
Stay at a healthy weight. Ask your provider what weight is healthy for you.
-
Do not smoke, vape, or use nicotine or tobacco.
-
Do not sit or lie down for a long time without moving.
-
Tell your provider if you plan to travel. Make sure you can still take your medicine while you travel.
-
Ask what things are safe for you to do at home. Ask when you can go back to work or school.
-
Keep all follow-up visits. Your provider will closely watch how you're doing.
To learn more, go to these websites:
Contact a health care provider if:
- You have:
New or more pain, swelling, warmth, or redness in an arm or leg.
Worse chest pain.
A heartbeat that's fast or not normal.
A very bad headache.
Changes to your eyesight.
A very bad fall or accident, or you hit your head.
Blood in your pee or poop.
A cut that won't stop bleeding.
-
You feel short of breath, and it gets worse when you're moving or resting.
-
You throw up or cough up blood.
-
You feel light-headed or dizzy, and the feeling doesn't go away.
-
You can't move your arms or legs.
-
You're confused or have memory loss.
These symptoms may be an emergency. Call 911 right away.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.