ThisiscontentfromElsevier'sDrugInformation
Conjugated Estrogens; Medroxyprogesterone
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
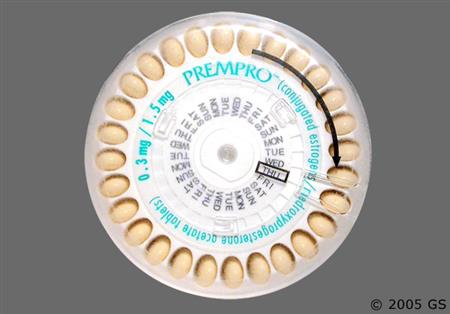
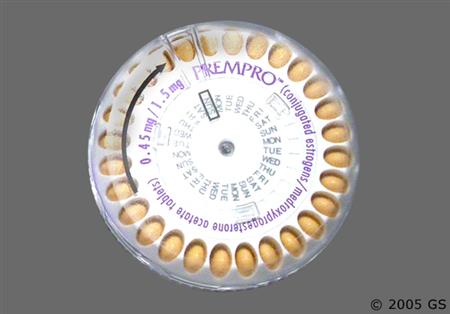
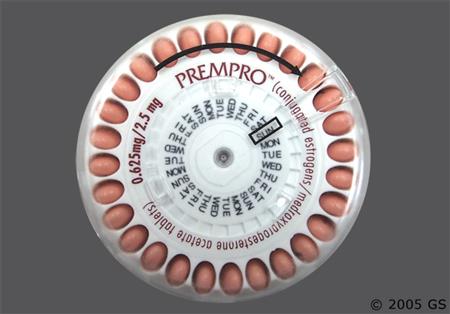
0.3 to 0.45 mg conjugated estrogens/1.5 mg medroxyprogesterone acetate PO once daily or 0.625 mg conjugated estrogens/2.5 to 5 mg medroxyprogesterone acetate PO once daily. Adjust dose based on clinical response. Use the lowest effective dose. Repeat cycle every 28 days. Assess the need for continued use periodically.[49260] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use at until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
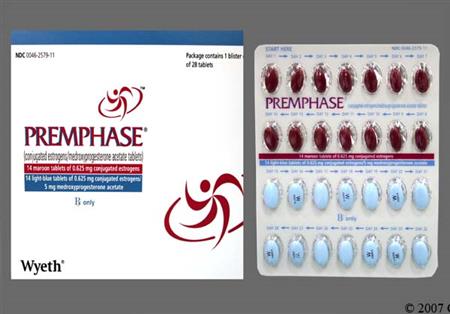
0.625 mg conjugated estrogens PO once daily on days 1 to 14, followed by 0.625 mg conjugated estrogens/5 mg medroxyprogesterone acetate PO once daily on days 15 to 28. Repeat cycle every 28 days. If dosage titration is needed, use another product due to fixed dose availability of this product. Assess the need for continued use periodically.[49260] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use at until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
1 tablet PO once daily. Each blister card contains 28-days of tablets. Cycles are repeated continuously. Dosage titration options include: A) 0.3 mg conjugated estrogen/1.5 mg medroxyprogesterone acetate tablet, B) 0.45 mg conjugated estrogen/1.5 mg medroxyprogesterone acetate tablet, C) 0.625 mg conjugated estrogen/2.5 mg medroxyprogesterone acetate tablet, or D) 0.625 mg conjugated estrogen/5 mg medroxyprogesterone acetate tablet. Use lowest effective dose that achieves clinical and bone density goals. Supplement calcium and vitamin D if dietary intake inadequate. Reassess hormone therapy every 3 to 6 months; carefully consider non-estrogen medication.[49260] In postmenopausal women with low bone mineral density, there is good evidence that standard-dose estrogen therapy reduces the risk for osteoporotic fractures, including hip, spine, and all non-spine fractures; however, estrogens are not generally recommended as a first-line prevention tactic due to the known risks of estrogen treatment (e.g., thromboembolism, cerebrovascular events) relative to other treatments. Women who need osteoporosis prophylaxis who are younger than 60 years or who are within 10 years of menopause onset may be given consideration for estrogen therapy, based on individual assessment of risk vs. benefit. Beyond the age of 60 years, other agents are preferred due to the known risks associated with hormonal therapy. Consider each woman's net balance of individual benefits and harms. If estrogen with or without a progestin is prescribed, use the lowest effective dose for the shortest duration that is consistent with an individual's treatment goals and risks. Estrogen therapy should not be used in patients with known osteoporosis; the risks outweigh the moderate benefit seen in postmenopausal women with established osteoporosis.[52408] [62806] [66837] [67122] [67125]
1 tablet (0.625 mg of conjugated estrogens) PO once daily on days 1 to 14, followed by 1 tablet (0.625 mg conjugated estrogens/5 mg medroxyprogesterone acetate) PO once daily on days 15 to 28. Repeat cycle every 28 days. Supplement calcium and vitamin D if dietary intake inadequate. Reassess hormone therapy every 3 to 6 months; carefully consider non-estrogen medication.[49260] In postmenopausal women with low bone mineral density, there is good evidence that standard-dose estrogen therapy reduces the risk for osteoporotic fractures, including hip, spine, and all non-spine fractures; however, estrogens are not generally recommended as a first-line prevention tactic due to the known risks of estrogen treatment (e.g., thromboembolism, cerebrovascular events) relative to other treatments. Women who need osteoporosis prophylaxis who are younger than 60 years or who are within 10 years of menopause onset may be given consideration for estrogen therapy, based on individual assessment of risk vs. benefit. Beyond the age of 60 years, other agents are preferred due to the known risks associated with hormonal therapy. Consider each woman's net balance of individual benefits and harms. If estrogen with or without a progestin is prescribed, use the lowest effective dose for the shortest duration that is consistent with an individual's treatment goals and risks. Estrogen therapy should not be used in patients with known osteoporosis; the risks outweigh the moderate benefit seen in postmenopausal women with established osteoporosis.[52408] [62806] [66837] [67122] [67125]
0.625 mg/day PO of conjugated estrogens with 5 mg/day PO of medroxyprogesterone.
0.625 mg/day PO of conjugated estrogens with 5 mg/day PO of medroxyprogesterone.
Not indicated.
Not indicated.
Not indicated.
Contraindicated in the presence of liver dysfunction or hepatic disease of any type.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication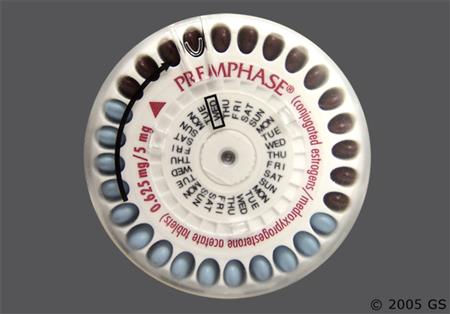

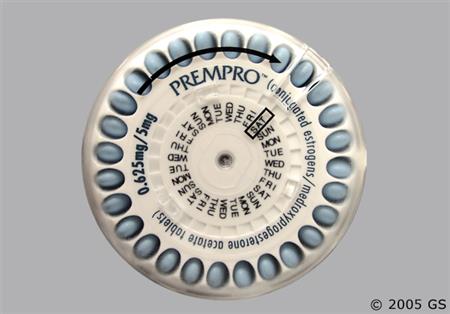


Conjugated estrogens and medroxyprogesterone are used together in an oral preparation to treat vasomotor and genitourinary symptoms associated with menopause, and for the prevention of osteoporosis. Conjugated estrogens are a mixture of the water soluble sodium salts of sulfate esters from estrone, equilin, and 17 alpha-dihydroequilin; other related steroids are also present. The mixture is traditionally derived from pregnant equine urine. The exact composition of the mixture is uncertain; and precisely how each of these various estrogens contribute to the drug's overall effectiveness is not known. Conjugated estrogens may also be synthesized from estrone and equilin, but the composition of the mixtures may not be equivalent to the naturally occurring sources. However, there is no evidence that 'natural' estrogens are more or less efficacious or safe than synthetic estrogens.[50638] Medroxyprogesterone is a synthetic progestin that is 15 times more potent than progesterone; the addition of medroxyprogesterone reduces the risk for endometrial hyperplasia. Oral combination conjugated estrogens-medroxyprogesterone products can enhance patient compliance with hormone replacement therapy (HRT) in women with an intact uterus. These products were first FDA-approved in November 1995.[27332]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
A variety of endocrine and urogenital effects can occur during conjugated estrogens; medroxyprogesterone therapy. Changes in sexuality include libido increase or libido decrease. Positive changes in libido may occur as a result of improvements in vulvar and vaginal atrophy. Vaginal discharge (leukorrhea), vaginal irritation, vaginal candidiasis, vaginitis, cervicitis, or changes in cervical erosion (e.g., cervical ectropion) may appear. Changes in vaginal bleeding pattern and breakthrough bleeding and spotting are commonly reported with estrogens and/or progestins. Amenorrhea is desirable in many postmenopausal women and not considered to be an adverse effect of estrogen therapy, and occurred in roughly 25% or more of women using conjugated estrogens; medroxyprogesterone at 1 year of use. Metrorrhagia, dysmenorrhea and pelvic pain occur infrequently. In clinical trials, adverse events occurring in 5% or more of patients who received conjugated estrogens; medroxyprogesterone included changes in vaginal bleeding pattern, cervical disorder (not specified, 4%), dysmenorrhea (3% to 13%), leukorrhea (4% to 5%), vaginal candidiasis (4% to 8%) and vaginitis (4% to 7%). In postmenopausal women, changes in uterine bleeding patterns will usually taper and stabilize within 3 to 6 months of beginning cyclic or continuous HRT combinations. Unusual vaginal bleeding, menorrhagia, or spotting that persists beyond 6 months in any woman on estrogen therapy should be evaluated by a healthcare professional. Estrogens may also cause enlargement of uterine leiomyomatas (fibroids) if present. A cystitis-like syndrome has also been reported. For women who have a uterus, adequate diagnostic measures such as endometrial sampling, when indicated, should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding. Women who take estrogens should follow advice regarding annual pelvic examinations and periodic Papanicolaou smears.[49260]
Breast changes that may occur with conjugated estrogens; medroxyprogesterone therapy include mastalgia (breast pain) and breast tenderness, which occur in 8% to 12% of women on chronic estrogen HRT; breast pain was reported in 13% to 33% of women taking conjugated estrogens; medroxyprogesterone during clinical trials. Breast enlargement (2% to 5%), breast discharge, galactorrhea, and fibrocystic breast changes have been reported with estrogens and/or progestin therapy. Gynecomastia may occur in men taking estrogen therapy. Patients should report breast changes, lumps, or breast discharge to their health care professionals. All women should receive yearly breast examinations by a healthcare provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results.[49260]
In clinical trials, gastrointestinal (GI) adverse events reported to occur in >= 5% of patients who received conjugated estrogens; medroxyprogesterone included dyspepsia (5—8%), diarrhea (5—7%), flatulence (5—9%), and nausea (7—11%).[49260] Stomach/abdominal pain or cramps, bloating, and nausea sometimes associated with vomiting are common adverse effects of estrogens. Consider benign hepatic adenoma if abdominal pain/tenderness, abdominal mass, or hypovolemic shock is present, as the adenoma may rupture and cause intraabdominal hemorrhage. Benign hepatic adenomas appear to be associated with the use of oral contraceptives, and enlargement of hepatic hemangiomas has been reported with estrogen and/or progestin therapies. Estrogens enhance hepatic lipoprotein uptake and inhibit bile acid synthesis, resulting in increased concentration of cholesterol in the bile which can lead to biliary obstruction, cholestasis, and cholelithiasis. Cholestatic jaundice and an increased incidence of gallbladder disease have also been reported. A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery (e.g., cholecystitis) in postmenopausal women receiving estrogens has been reported.[25473] Estrogens may be poorly metabolized in patients with impaired liver function. For patients with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, use conjugated estrogens; medroxyprogesterone cautiously. If cholestatic jaundice recurs, discontinue the estrogen.[49260] Rare adverse reactions (< 1%) include hepatitis (and elevated hepatic enzymes), enlargement of hepatic hemangiomas, ischemic colitis (bowel ischemia, no incidence reported), or pancreatitis. In patients with preexisting hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis and other complications. Estrogens may induce peliosis hepatis, a very rare consequence of taking estrogens and combined oral contraceptives that is characterized by the presence of blood-filled spaces.[51257] Persistent or severe abdominal symptoms should be evaluated by a medical professional.[49260]
Deep and superficial venous thrombosis, pulmonary embolism, thrombophlebitis, myocardial infarction, and stroke have been reported with estrogens and/or progestin therapy. The use of estrogens in postmenopausal women, with or without a progestin, carries a risk for thromboembolism, and cardiovascular events such as myocardial infarction (MI) or stroke. Detailed information regarding what is known about thromboembolic and cardiovascular risk in postmenopausal women is available in the boxed warnings and precautions section of the product labeling for the products, as these risks must be considered prior to use of HRT in women, and with consideration to age and other risk factors for these events. Risks vary with the use of estrogen-alone vs. use of estrogen with progestin therapy. Should any of these events occur or be suspected, discontinue the estrogen or estrogen-progestin therapy immediately.[49260]
Estrogens can cause sodium and fluid retention, resulting in peripheral edema (4%) or mild weight gain.[49260] Conjugated estrogens; medroxyprogesterone should be prescribed cautiously to patients in whom edema formation would be detrimental. Estrogens and progestins also can slightly increase blood pressure, occasionally causing hypertension. Data indicate in most patients the change is not clinically significant. In a small number of case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. In the PEPI trial, postmenopausal women 45—65 years of age randomized to any hormone replacement therapy regimen experienced increases in both systolic and diastolic blood pressure of 3—5% after the first year of treatment, but the increases were not statistically different from placebo.[24010]
Headache has been noted with use of estrogens such as conjugated estrogens; medroxyprogesterone. A severe headache may be a warning sign of a serious adverse event such as a stroke or retinal problems (e.g., thrombosis) in the eye. Discontinue the estrogen pending examination if there is sudden partial or complete loss of vision or sudden onset of migraine. If examination reveals a serious event, estrogens should be permanently discontinued. The relationship of headache, specifically migraine headache, and the administration of estrogens is not clearly defined. A number of changes can occur when a woman initiates HRT and include 1) migraines can appear for the first time, 2) a change in frequency, severity and duration of migraine headaches may be seen, or 3) an improvement or decrease in the occurrence of migraine headaches. Such adverse events are not frequent. When initiating therapy an individual's headache pattern should be observed and if migraines worsen consider discontinuing therapy. In addition, growth potentiation of benign meningioma has been reported during post marketing surveillance.[49260]
Mental depression, nervousness or anxiety, and mood disturbances such as emotional lability and irritability have been reported with estrogens and/or progestin therapy. Complaints of insomnia or fatigue may be associated with the underlying menopausal complaints or may be associated with treatment. In clinical trials, adverse events reported to occur in patients who received conjugated estrogens; medroxyprogesterone included depression (5—11%), anxiety or nervousness (2—4%), insomnia (6—7%), and dizziness (3—5%).[49260] Women with a history of depression may need special monitoring. If significant depression occurs, estradiol should be discontinued.
Estrogens can cause a variety of dermatological and allergic reactions. In clinical trials, pruritus (4—10%) and rash (unspecified) (4—6%) were noted in conjugated estrogen; medroxyprogesterone recipients. Chloasma or melasma, in the form of tan or brown patches, may develop on the forehead, cheeks, temples, and upper lip. These skin changes may persist after the drug is discontinued. Erythema multiforme, erythema nodosum, hemorrhagic eruption, loss of scalp hair or alopecia, hirsutism, pruritus, urticaria, angioedema, and anaphylactoid reactions have been reported with estrogens and/or progestins.[49260] In some cases estrogens or progestins may induce or aggravate an existing acne vulgaris.
Retinal thrombosis has been reported in patients receiving estrogens such as conjugated estrogens; medroxyprogesterone. Discontinue medication pending examination if there is sudden visual impairment either partial or complete or a sudden onset of proptosis, diplopia, or migraine. If examination reveals papilledema, visual loss, or retinal vascular lesions, permanently discontinue estrogens. Exogenous estrogen use can cause a conical cornea to develop from steepening or increased curvature of the cornea, caused by thinning of the stroma. Patients with contact lenses may develop intolerance to their lenses.[49260]
Conjugated estrogens; medroxyprogesterone can cause impaired carbohydrate metabolism and impaired glucose tolerance, leading to hyperglycemia in some women taking HRT. In the PEPI trial, fasting glucose levels were lower, and mean 2-hour glucose levels were 8% higher, in combined HRT treated women versus placebo in all treatment arms. The effects appeared to be consistent across demographic, clinical, and lifestyle variables.[24010]
Conjugated estrogens; medroxyprogesterone is known to cause teratogenesis during pregnancy and are in FDA category X.[49260] Increased risk of a wide variety of fetal abnormalities, including modified development of sexual organs, cardiovascular anomalies and limb defects, have been reported following the use of estrogens or synthetic progestins alone in pregnant women. In any patient in whom pregnancy is suspected, pregnancy should be ruled out before continuing estrogen-progestin use.
Hormone replacement therapy (HRT), both estrogen/progestin combination therapy and estrogen alone therapy, fails to prevent mild impaired cognition (memory loss) and is positively associated with the risk of developing dementia in women 65 years and older; do not use HRT to prevent or treat dementia or preserve cognition (memory).[49260] When data from the 2 populations in the WHIMS estrogen-alone and estrogen plus progestin ancillary studies were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95% CI 1.19 to 2.60, p = 0.005). Since both ancillary studies were conducted in women 65 to 79 years of age, it is unknown whether these findings apply to younger postmenopausal women.[27451] [32126] [50638] In the Women’s Health Initiative Memory Study (WHIMS) estrogen plus progestin ancillary study, a population of 4,532 postmenopausal women 65 to 79 years of age was randomized to daily CE (0.625 mg) plus MPA (2.5 mg) or placebo. After an average follow-up of 4 years, 40 women in the CE plus MPA group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE plus MPA versus placebo was 2.05 (95% CI, 1.21 to 3.48). The absolute risk of probable dementia for CE plus MPA versus placebo was 45 vs. 22 cases per 10,000 women-years.[27451] In the WHIMS estrogen-alone ancillary study of WHI, a population of 2,947 hysterectomized women 65 to 79 years of age was randomized to daily CE (0.625 mg)-alone or placebo. After an average follow-up of 5.2 years, 28 women in the estrogen-alone group and 19 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for CE-alone versus placebo was 1.49 (95% CI, 0.83 to 2.66). The absolute risk of probable dementia for CE-alone versus placebo was 37 versus 25 cases per 10,000 women-years.[32126]
In women with a history of cardiovascular disease, the use of estrogen and progestin combination therapy (e.g., conjugated estrogens; medroxyprogesterone) increases the risk of developing urinary incontinence. Patients in the HERS study who did not have urinary incontinence prior to the studies initiation were observed to determine if hormone replacement therapy was helpful in preventing urinary incontinence. The study found that women who received estrogen/progestin therapy were almost twice as likely as patients receiving placebo to develop urge incontinence and 3 times as likely to develop stress incontinence after 1 year of treatment. At 4 years, the effect of hormone replacement therapy became even more pronounced, increasing the risk to 3.23 for urge incontinence and to 4.81 for stress incontinence. The applicability of these findings to women who use estrogen alone is unclear.[27457]
Adverse events that have been reported with conjugated estrogen; medroxyprogesterone include aggravation of porphyria, arthralgia, leg muscle cramps, hypocalcemia, and exacerbations of asthma and systemic lupus erythematosus.[49260]
Numerous epidemiologic studies have examined the effects of estrogen and estrogen-progestin hormone replacement therapy (HRT) on the development of new primary malignancy (e.g., breast cancer, endometrial cancer, ovarian cancer) in postmenopausal women. Detailed clinical study information regarding what is known about cancer risk in postmenopausal women is available in the boxed warnings and precautions section of the product labeling for the products, as these risks must be considered prior to use of HRT, and with consideration to age and other risk factors for these events.[49260] [60224] [50638] [71260] ENDOMETRIAL HYPERPLASIA and ENDOMETRIAL CANCER: There is an association of unopposed estrogen therapy and endometrial hyperplasia in women with an intact uterus. Adding a progestin to estrogen therapy has been shown to reduce, but not eliminate, the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. The incidence of endometrial hyperplasia due to combined estrogen-progestin HRT (using a cyclic or continuous progestin regimen) is 1% or less. Clinical surveillance of all women using estrogen-alone or estrogen plus progestin therapy is important. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal uterine bleeding. The reported endometrial cancer risk among unopposed estrogen users is about 2 to 12-times greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than 1 year. The greatest risk appears associated with prolonged use, with increased risks of 15-to 24-fold for 5 to 10 years or more, and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. BREAST CANCER: The data available are derived from studies of estrogen-alone or estrogen plus progestin hormonal replacement therapy (HRT). Since the 1970s, numerous epidemiological studies have examined the association of exogenous estrogen and breast cancer (new primary malignancy). The most important randomized clinical study providing information about breast cancer in estrogen-alone users is the Women's Health Initiative (WHI) substudy of daily conjugated estrogens (0.625 mg)-alone. In the WHI estrogen-alone substudy, after an average follow-up of 7.1 years, conjugated estrogen (0.625 mg/day)-alone was not associated with an increased risk of invasive breast cancer (relative risk [RR] 0.80). The use of estrogen-alone has been reported to result in an increase in abnormal mammograms requiring further evaluation. The Women's Health Initiative (WHI) estrogen plus progestin study reported increased risks of invasive breast cancer in patients taking combined estrogen-progestin HRT vs. placebo. The potential risk of breast cancer may increase with longer duration of use. All persons should receive yearly breast examinations by a health care provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results. OVARIAN CANCER: Women who used HRT for menopausal symptoms also had an increased risk for ovarian cancer, but data are still uncertain if risk is associated with a specific duration of use. What is known about the risk of ovarian cancer due to hormonal therapy is derived from data available for estrogen-alone and estrogen plus progestin products; studies are not available for estrogen plus selective estrogen receptor modifier combinations. The Women's Health Initiative (WHI) estrogen plus progestin substudy reported a statistically non-significant increased risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for estrogen plus progestin versus placebo was 1.58 (95% CI 0.77 to 3.24). The absolute risk for estrogen plus progestin versus placebo was 4 versus 3 cases per 10,000 women-years. A meta-analysis of 17 prospective and 35 retrospective epidemiology studies found that women who used HRT for menopausal symptoms had an increased risk for ovarian cancer. The primary analysis, using case-control comparisons, included 12,110 cancer cases from the 17 prospective studies. The relative risk associated with current use of hormonal therapy was 1.41 (95% confidence interval [CI] 1.32 to 1.5); there was no difference in the risk estimates by duration of the exposure (less than 5 years [median of 3 years] vs. greater than 5 years [median of 10 years] of use before the cancer diagnosis). The relative risk associated with combined current and recent use (discontinued use within 5 years before cancer diagnosis) was 1.37 (95% CI 1.27 to 1.48), and the elevated risk was significant for both estrogen-alone and estrogen plus progestin products. The exact duration of hormone therapy use associated with an increased risk of ovarian cancer, however, is unknown.[49260] [60224] [50638] [71260]
Estrogen administration may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, discontinue the estrogen and take appropriate measures to reduce the serum calcium concentration.[49260]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Exogenous estrogens may exacerbate symptoms of angioedema in individuals with hereditary angioedema. Consider whether the benefits of estrogen therapy outweigh the risks in such individuals.[49260]
Estrogen-based hormone replacement therapy (HRT) products, such as conjugated estrogens; medroxyprogesterone, are contraindicated in people with undiagnosed abnormal uterine bleeding or a history of or known/suspected breast cancer, endometrial cancer, or other estrogen-dependent tumor, which may be hormonally-sensitive. There is an increased risk of endometrial cancer in a person with a uterus who uses unopposed estrogens. Adding a progestin to estrogen HRT has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding. The use of estrogen-alone or estrogen plus progestin HRT has been reported to result in an increase in abnormal mammograms, requiring further evaluation and observational studies. During the Womens Health Initiative (WHI), estrogen-alone was not associated with an increased risk of invasive breast cancer, but an estrogen plus progestin WHI substudy reported increased risks of invasive breast cancer. Consistent with the WHI clinical trials, observational studies have also reported an increased risk of breast cancer for estrogen plus progestin therapy, and a smaller increased risk for estrogen-alone therapy, after several years of use. All people taking estrogen with or without a progestin as HRT should receive an annual clinical breast examination, perform monthly self-examinations, and have regular mammograms as recommended by their health care professional based on patient age, risk factors, and prior mammogram results.[49260] [71260] While estrogen therapy is rarely used for the palliative treatment of advanced breast cancer, estrogen HRT use may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, use of HRT should be stopped and appropriate measures taken to reduce the serum calcium level.[49260]
Because estrogens influence the growth of endometrial tissues, use estrogen-based hormone replacement therapy (HRT) cautiously in people with endometriosis or uterine leiomyoma (uterine fibroids). A few cases of malignant transformation of residual endometrial growth have been reported in women treated post-hysterectomy with estrogen-alone HRT. For individuals known to have residual endometriosis post-hysterectomy, the addition of a progestin, such as in the use of conjugated estrogens; medroxyprogesterone products, should be considered to reduce the risk of endometrial tissue growth.[49260] [69730] [72653]
Estrogens, with or without progestins, should not be used for the prevention of cardiovascular disease. An increased risk of thromboembolic and serious cardiovascular events [e.g. pulmonary embolism (PE), deep vein thrombosis (DVT), stroke, and myocardial infarction (MI)] are reported with estrogen plus progestin hormone replacement therapy (HRT). Increased risks of stroke and DVT are reported with estrogen-alone HRT. Immediately discontinue the HRT regimen if any of these events occur or are suspected. Due to the potential for serious cardiovascular events, estrogen-containing HRT is contraindicated in people with active thromboembolism (e.g., DVT or PE) or a history of these conditions, or in those with active arterial thromboembolic disease (e.g., stroke and myocardial infarction) or a history of these conditions. HRT regimens are also contraindicated in people with known thrombophilia (e.g., protein C, protein S, or antithrombin deficiency). Individuals with certain risk factors for arterial vascular disease (e.g., cardiovascular disease, hypertension, diabetes, tobacco smoking, hypercholesterolemia, and morbid obesity) and/or venous thromboembolism (VTE) (e.g., personal history or family history of VTE, obesity, or systemic lupus erythematosus) should be monitored and managed appropriately during HRT use.[49260] Monitor blood pressure in all postmenopausal individuals receiving HRT and especially in those with pre-existing hypertension; in a few case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogen HRT therapy. In a large, randomized, placebo controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. Estrogens may cause some degree of fluid retention, and people with conditions that may be aggravated, such as cardiac dysfunction, warrant careful observation when estrogens are prescribed.[49260] [50638]
If feasible, estrogen-based hormone replacement therapy (HRT) should be discontinued at least 4 to 6 weeks before major surgery or a planned procedure associated with an increased risk of thromboembolism, or during periods of prolonged immobility. Resume the HRT regimen only after the patient is fully ambulatory. In addition, people treated with HRT should be advised to move about periodically during travel involving prolonged immobilization, such as during long-duration plane travel.[49260]
Estrogen-based hormone replacement therapy (HRT) is contraindicated in people with hepatic failure, impairment or disease. Estrogens and/or progestins may be poorly metabolized in those with impaired liver function. For people with a history of intrahepatic cholestasis of pregnancy or a history of significant adverse event(s) associated with previous use of an estrogen, such as cholestatic jaundice, use estrogens with caution. If there is a recurrence of cholestatic jaundice, discontinue the HRT regimen. Estrogen HRT may cause an exacerbation of porphyria or hepatic hemangioma (benign liver tumor). Consider whether the benefits of estrogen HRT outweigh the risks in people with such conditions.[49260] Liver disease guidelines recommend that menopausal estrogen-based HRT not be used in people with the following conditions: decompensated liver function, Budd-Chiari syndrome, or hepatocellular adenoma (benign liver tumor).[72725]
Use estrogen-based hormone replacement therapy (HRT) with caution in people with pre-existing gallbladder disease. A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal individuals receiving estrogens has been reported.[49260] [25473]
In people with pre-existing hypertriglyceridemia, estrogen-based hormone replacement therapy (HRT) may be associated with elevations of plasma triglycerides leading to pancreatitis. Discontinue the HRT regimen if pancreatitis occurs.[49260]
Individuals with systemic lupus erythematosus (SLE) may have an increased risk for thromboembolism and should be managed appropriately when estrogen hormone replacement therapy (HRT) is used. Estrogen HRT may cause an exacerbation of SLE and should be used with caution in people with this condition.[49260]
Estrogen-based hormone replacement therapy (HRT) may cause an exacerbation of migraine and should be used cautiously in people with this condition. Discontinue the HRT regimen pending examination if there is a migraine with focal neurologic or visual changes.[49260]
Individuals with diabetes mellitus may have an increased risk for thromboembolism and should be managed appropriately when estrogen-based hormone replacement therapy (HRT) is used. Estrogen HRT may cause an exacerbation of diabetes. Consider whether the benefits of estrogen therapy outweigh the risks in people with this condition.[49260]
Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. People with hypothyroidism dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. Monitor thyroid function in these individuals to ensure maintenance of their free thyroid hormone levels in an acceptable range. People with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T and T serum concentrations in the normal range.[49260]
Estrogen therapy should be used with caution in people with hypoparathyroidism as estrogen-induced hypocalcemia may occur.[49260]
Estrogens may cause exacerbation of asthma or epilepsy (seizure disorder) and should be used with caution in people with these conditions.[49260]
Estrogens may cause fluid retention. Conditions that might be affected by fluid retention, such as renal impairment or renal failure, require careful observation when estrogens are prescribed.[49260]
Administration of hormone replacement therapy (HRT) for menopause should generally be avoided in geriatric adults 65 years of age and older, and HRT should not be used to prevent or treat dementia or preserve cognition (memory). Both estrogen-progestin combination hormone replacement therapy (HRT) and estrogen-alone therapy fail to prevent mild cognitive impairment (memory loss) and increase the risk of dementia in females 65 years of age and older.[49260] Overall risk vs. benefit should be considered along with the goals of use of HRT for the individual patient when considering whether to continue HRT if they are over 65 years of age.[50638] [27451] [32126] [71260] The Beers Criteria consider oral, topical patch, or other systemic forms of estrogens (with or without progestins) as potentially inappropriate medications for use in geriatric adults. Avoid use due to evidence of carcinogenic potential (i.e., breast and endometrium) and the lack of cardiovascular or cognitive protective effects. Avoid oral or transdermal estrogen in geriatric adult women with any type of urinary incontinence due to lack of efficacy for this condition. The use of vaginal estrogens is acceptable for the management of dyspareunia and vaginal/vulvar symptoms.[63923]
There is no FDA-approved indication for the use of conjugated estrogens; medroxyprogesterone products in pregnancy. There are no data with the use of conjugated estrogens; medroxyprogesterone in pregnant women; however, epidemiologic studies and meta-analyses have not found an increased risk of a wide variety of fetal abnormalities, including modified development of sexual organs, cardiovascular anomalies and limb defects following the chronic use of estrogen and progestin before conception or during early pregnancy.[49260]
Use conjugated estrogens; medroxyprogesterone products with caution during breast-feeding. Estrogens and progestins and metabolites are present in human milk. These hormones can reduce milk production in nursing individuals. This reduction can occur at any time but is less likely to occur once nursing is well established. Consider the developmental and health benefits of breast-feeding, the clinical need for treatment, and any potential adverse effects on the breastfed child from the medication or from the underlying maternal medical condition.[49260]
The administration of estrogen and progestin hormones results in different pharmacologic effects in individual females dependent upon the underlying estrogen balance and age of the individual patient. This monograph describes the basic mechanism of action of conjugated estrogens and medroxyprogesterone in the postmenopausal woman.[49260]
Conjugated estrogens; medroxyprogesterone is administered orally. Conjugated estrogens bind primarily to albumin; unconjugated estrogens bind both to albumin and sex-hormone-binding globulin. Conjugated estrogens are metabolized primarily in the liver to glucuronide and sulfate conjugates of estradiol, estrone, and estriol. These products are eliminated in the urine. A portion of the conjugates are excreted into the intestine through the biliary system; hydrolysis in the gut allows for enterohepatic recirculation of the estrogens. In postmenopausal women, a significant portion of the sulage conjugates exist as estrone sulfate, which serves as a reservoir for the formation of the more active estrogens, estradiol and estriol. The apparent terminal half life of conjugated estrone is 4—18.5 hours and the half-life of conjugated equilin is 4—17 hours. Metabolism of medroxyprogesterone is hepatic, and elimination is primarily fecal. Medroxyprogesterone's half-life is roughly 38—48 hours.
Conjugated estrogens and medroxyprogesterone are rapidly absorbed from the GI tract after oral administration; the manufactured tablets are designed to release the estrogens slowly over a period of several hours.
There is no FDA-approved indication for the use of conjugated estrogens; medroxyprogesterone products in pregnancy. There are no data with the use of conjugated estrogens; medroxyprogesterone in pregnant women; however, epidemiologic studies and meta-analyses have not found an increased risk of a wide variety of fetal abnormalities, including modified development of sexual organs, cardiovascular anomalies and limb defects following the chronic use of estrogen and progestin before conception or during early pregnancy.[49260]
Use conjugated estrogens; medroxyprogesterone products with caution during breast-feeding. Estrogens and progestins and metabolites are present in human milk. These hormones can reduce milk production in nursing individuals. This reduction can occur at any time but is less likely to occur once nursing is well established. Consider the developmental and health benefits of breast-feeding, the clinical need for treatment, and any potential adverse effects on the breastfed child from the medication or from the underlying maternal medical condition.[49260]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.