ThisiscontentfromElsevier'sDrugInformation
Desogestrel; Ethinyl Estradiol
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
1 tablet (containing 0.15 mg desogestrel and 30 mcg ethinyl estradiol) PO once daily for 21 days, followed by 7 days without drug.[50744]
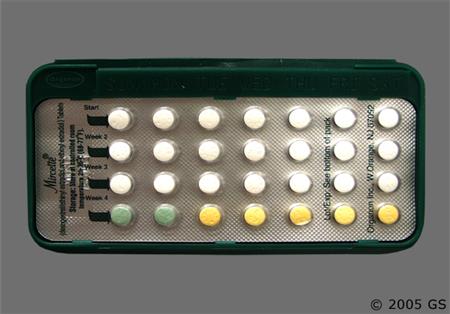
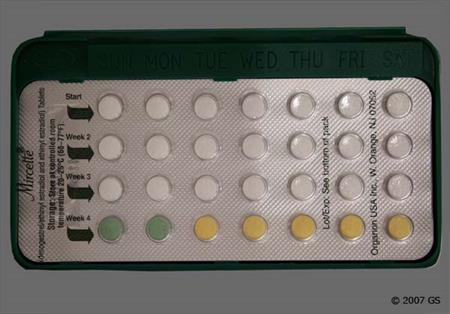
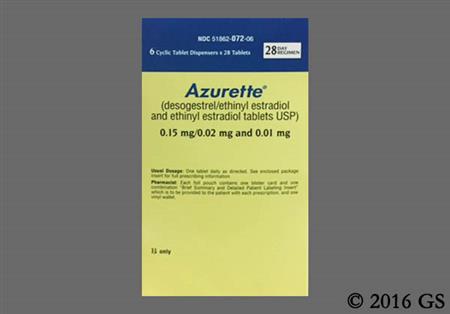
1 tablet PO once daily for 28 days in order indicated in the pack. Phase 1 contains 21 tablets of 0.15 mg desogestrel and 20 mcg ethinyl estradiol, followed by 2 days of inert tablets. Phase 2 contains 5 tablets with 10 mcg ethinyl estradiol only.[43312]
1 tablet PO once daily for 21 days in the order indicated in the pack, followed by 7 days without drug. Phase 1 contains 7 tablets of 0.1 mg desogestrel and 25 mcg ethinyl estradiol. Phase 2 contains 7 tablets of 0.125 mg desogestrel and 25 mcg ethinyl estradiol. Phase 3 contains 7 tablets of 0.15 mg desogestrel and 25 mcg ethinyl estradiol.[62071]
1 tablet PO once daily, in order directed on pack, following dosage as per routine contraception. Then, repeat cycles as directed for product chosen. Expected time to acne improvement with CHCs is usually within 3 to 6 months, and CHCs may be used with other acne therapies early in treatment to accelerate response. Prolonged treatment may be needed for acne control.[58791] [69506] [70323]
0.1 to 0.15 mg desogestrel; 0.02 to 0.03 mg ethinyl estradiol PO once daily for 21 days, followed by 7 days of inert, inactive tablets or 2 days of inert, inactive tablets and then 5 days of 0.01 mg ethinyl estradiol as for routine contraception.[38069] [50744] [58791] [58792] [58793] [62071] [70439] [71064]
0.1 to 0.15 mg desogestrel; 0.02 to 0.03 mg ethinyl estradiol PO once daily for 21 days, followed by 7 days of inert, inactive tablets or 2 days of inert, inactive tablets and then 5 days of 0.01 mg ethinyl estradiol as for routine contraception.[38069] [50744] [58791] [58792] [58793] [62071] [70439] [71064]
NOTE: For individuals who have no known contraindications to combined oral contraceptives, desire contraception, have achieved menarche, and have been evaluated for causes of the condition
Follow dose as for routine contraception. Alternatively, the active tablets can be given continuously in selected patients. Combined hormonal contraceptives can reduce endometriosis-associated dyspareunia, dysmenorrhea, and non-menstrual pelvic pain.[69730]
1 tablet/day PO as directed in pack.
Not indicated.
1 tablet/day PO as directed in pack.
Use before menarche is not indicated.
Safety and efficacy have not been established.
Steroid hormones in combined hormonal contraceptives (CHCs) may be poorly metabolized in those with impaired liver function. If jaundice develops during use, discontinue. Contraindicated for use in those with acute or chronic hepatic disease with abnormal liver function and in those with history of cholestatic jaundice of pregnancy or jaundice with prior CHC use.[43312][50744][62071][48201][70437]
No dosage adjustments for combined hormonal contraceptives (CHCs) are needed; however, depending on the cause and degree of the renal impairment/chronic kidney disease (CKD), other contraceptive agents may be preferred over CHCs. If the person with CKD is a candidate for CHC use, monitor for blood pressure increase, changes in proteinuria, and thromboembolism risk during CHC initiation and periodically thereafter.[48201][70659]
† Off-label indication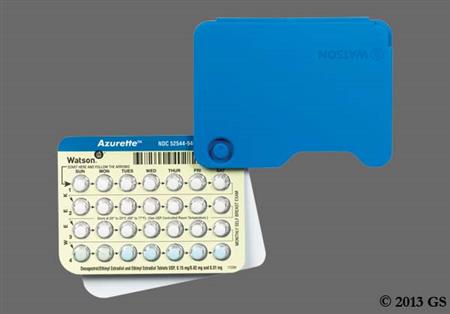















Desogestrel and ethinyl estradiol are used together as an oral combined hormonal contraceptive (CHC). Ethinyl estradiol is a potent, synthetic estrogen. Desogestrel is a third-generation progestin with lowered androgenic effects and relatively no estrogenic action compared to older progestins. Thus, desogestrel may have positive influences on acne, fluid retention, and lipid profiles. CHCs can be used in female patients from menarche to over the age of 40 years up until the time of menopause with proper selection of products, if no contraindications exist. The choice of a routine contraceptive for any given patient is based on the individual's contraceptive needs, underlying medical conditions or risk factors for adverse effects, and individual preferences for use. All combined hormonal contraceptives (CHCs) have risks related to venous and arterial thromboembolism; CHC labels contain a boxed warning regarding the increased risk for thromboembolism in tobacco smokers. The Centers for Disease Control's U.S. Medical Eligibility Criteria describe considerations for risk vs. benefits, including medical conditions or attributes that contraindicate use; these criteria can help practitioners determine product selection for individual patients.[48201][66717] Some desogestrel; ethinyl estradiol products provide a reduced hormone-free interval in the cycle, which may be advantageous for patients experiencing migraines, dysmenorrhea, or other symptoms during the days they do not take active hormones. Desogestrel; ethinyl estradiol products were initially FDA approved in 1992.[43312][50744][62071]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
General information when initiating routine CHCs: [66717]
Initiating CHCs in an individual not previously taking a CHC: There are options to start taking the first cycle of their COC.
Switching from a different CHC or other contraceptive methods:
Initiating a CHC in the person with amenorrhea:
Initiating CHCs postpartum:
Initiating CHCs following induced or spontaneous abortion:
A common side effect of oral combined hormonal contraceptives (CHCs) is breakthrough bleeding and spotting, especially during the first 3 months of CHC use. Menstrual irregularity is reported infrequently with CHCs. Oligomenorrhea and amenorrhea (defined as at least 1 of 6 cycles with a missed withdrawal bleed) are also reported. Menstrual cramps or dysmenorrhea, changes in menstrual flow, and premenstrual syndrome have also been reported during CHC use. If the patient has not adhered to the prescribed dosing schedule, consider the possibility of pregnancy at the time of the first missed period and take appropriate diagnostic measures. If the patient has adhered to the prescribed regimen and misses 2 consecutive periods, rule out pregnancy. A change to another CHC formulation may resolve irregularities that continue to occur during use.[43312] [50744] [62071]
Breast tenderness or mastalgia, breast enlargement, and breast discharge or secretion have been reported in patients receiving oral combined hormonal contraceptives (CHCs) and are believed to be drug-related. Possible lactation suppression may occur when CHCs are given in the immediate postpartum period.[43312] [50744] [62071]
Combined hormonal contraceptive (CHC) recipients have reported the following adverse vaginal and cervical reactions that are believed to be drug-related: vaginal candidiasis, bacterial vaginitis, and change in cervical ectropion and secretion. Vaginal discharge may be noted if vaginal candidiasis or vaginitis occurs. Urogenital adverse events such as cystitis-like syndrome have also been reported.[43312] [50744] [62071]
Headache is a relatively common adverse reaction reported with use of oral combined hormonal contraceptives (CHCs). Discontinue the CHC if new migraines are recurrent, persistent, or severe or if there is an increased frequency or severity of migraines during CHC use (which may be prodromal of a cerebrovascular event). A migraine with aura can increase the risk for cerebrovascular accidents.[43312] [50744] [62071]
Desogestrel; ethinyl estradiol combined hormonal contraceptives (CHCs) may cause edema (fluid retention) and weight gain. Postmarketing, both increased and decreased weight have been reported, as well as peripheral edema and changes in appetite (increase or decrease). There is an increased risk of hypertension in CHC users. Studies suggest that approximately 41.5 cases of hypertension per 10,000 person-years in the U.S. can be attributed to CHC use. Increased blood pressure is more likely in older people with an extended duration of CHC use. Discontinue the CHC if significant elevation of blood pressure occurs. Blood pressures usually return to normal after discontinuation of therapy, and no difference in the occurrence of hypertension exists among ever- and never-users.[43312] [50744] [62071]
Combined hormonal contraceptives (CHCs) such as desogestrel; ethinyl estradiol are associated with an increased risk of thromboembolic and thrombotic disease. The risk for the development of VTE, such as deep venous thrombosis and/or pulmonary embolism is approximately 3 to 6 times greater in CHC users than in nonusers. In several studies, the risk was reported to be substantially higher in smokers compared with nonsmokers, and especially if the smoker was over 35 years of age. The relative risk of venous thromboembolism (VTE) in people who have predisposing conditions is twice that of those without such medical conditions. The risk of VTE due to CHC use gradually disappears after the CHC is discontinued. VTE risk is highest in the first year of use and when a CHC is started or re-started after a break in use of 4 weeks or more. Estrogens decrease levels of antithrombin-III and increase the production of blood clotting factors VII, VIII, IX and X; risks increase with ethinyl estradiol doses of more than 50 mcg/day. Serious thromboembolic events, such as heart attack or cerebrovascular accidents, are reported rarely in users of CHCs who do not smoke.[48201] Thrombosis/thromboembolism (coronary artery, pulmonary, cerebral, deep vein, mesenteric), thrombophlebitis and myocardial infarction have also been reported with postmarketing CHC use.[43312] [50744] [62071]
An increase in both the relative and attributable risks of cerebrovascular events (thrombotic and hemorrhagic strokes with intracranial bleeding) has been shown in users of CHCs such as desogestrel; ethinyl estradiol. The risk is greater among people over 40 years of age, smokers, and in individuals with hypertension, dyslipidemia, diabetes, or obesity. In smokers, the risk for stroke increases with age, particularly in those 35 years of age and older, and with the number of cigarettes smoked.[48201] [43312] [50744] [62071]
During postmarketing use of desogestrel; ethinyl estradiol and other combined hormonal contraceptives (CHCs), the following ocular adverse effects have been reported: corneal thinning (keratoconus), and a change in corneal curvature (steepening). Contact lens intolerance may occur in some patients. Rarely, retinal thrombosis may occur, but may cause vision loss. Stop the CHC regimen if there is unexplained loss of vision or visual impairment, proptosis, diplopia, papilledema, or retinal vascular lesions and evaluate for retinal vein thrombosis immediately. While optic neuritis and cataracts have been reported in some CHC users, the association with CHC use has been neither confirmed nor refuted.[43312] [50744] [62071]
Desogestrel; ethinyl estradiol and other combined hormonal contraceptives (CHCs) have been reported to cause hypersensitivity and dermatologic adverse events. Acne vulgaris is infrequently reported; alopecia, rash (allergic), pruritus, hirsutism, erythema multiforme, erythema nodosum, and hemorrhagic eruption have also been reported. Anaphylactoid reactions, urticaria, angioedema, and severe reactions with respiratory (dyspnea) and circulatory symptoms have also been reported. Melasma, a brown patchy skin discoloration, may occur and persist after the CHC is discontinued.[43312] [50744] [62071] Photosensitivity has also been reported rarely with CHC use.[57603]
Nausea (mild and infrequent), vomiting, abdominal pain or cramps, bloating, and pancreatitis have been reported during use of combined hormonal contraceptives (CHCs), including desogestrel; ethinyl estradiol. Gallbladder disease (e.g., cholestasis, cholelithiasis, cholecystitis), hepatic adenoma, colitis, and hemangioma of the liver have been reported during postmarketing experience.[43312] [50744] [62071] Studies suggest a small increased relative risk of developing gallbladder disease among combined hormonal contraceptive (CHC) users.[48201] [62071] Withhold or permanently discontinue the CHC if there are persistent or significant elevated hepatic enzymes or if jaundice occurs. Rare but serious GI system events which may occur with CHC use include cholestatic jaundice, peliosis hepatis, Budd-Chiari syndrome, or hepatic vein obstruction. Peliosis hepatis, a very rare consequence of taking estrogens and CHCs, is characterized by the presence of blood-filled spaces.[51257] In rare cases, CHCs can cause benign but dangerous liver tumors. Indirect calculations have estimated the attributable risk of hepatoma to be in the range of 3.3 cases per 100,000 users, a risk that increases after 4 or more years of use. These benign liver tumors can rupture and cause fatal internal bleeding.[43312] [50744] [62071]
Psychiatric system disorders reported with desogestrel; ethinyl estradiol or other combined hormonal contraceptive (CHC) regimens include mood swings or emotional lability (infrequent per other CHC studies), depression, anxiety or nervousness, and changes in libido (libido increase or libido decrease). Discontinue the CHC regimen if depression occurs to a significant degree.[43312] [50744] [62071]
Dizziness has been reported as a nervous system adverse effect with desogestrel; ethinyl estradiol and other combined hormonal contraceptive (CHC) regimens.[43312] [50744] [62071]
Combined hormonal contraceptives (CHCs) can alter certain laboratory tests. Estrogens may increase the serum concentrations of thyroxine-binding globulin, sex hormone-binding globulin, and cortisol-binding globulin. Endocrine, metabolic or nutritional system effects that have been reported with desogestrel; ethinyl estradiol CHCs include reduced tolerance to carbohydrates resulting in impaired glucose tolerance or hyperglycemia. Those with hypertriglyceridemia, or a family history thereof, may have an increase in serum triglyceride concentrations when using CHCs which may increase the risk of pancreatitis. A decrease in serum folate levels has also been reported.[43312] [50744] [62071]
Porphyria has been reported with use of oral combined hormonal contraceptives (CHCs) such as desogestrel; ethinyl estradiol.[43312] [50744] [62071] Aggravations of varicose veins, exacerbation of systemic lupus erythematosus (SLE), and exacerbation of chorea have been reported and may be drug-related.[62071]
Renal effects reported with combined hormonal contraceptives (CHCs) have included impaired renal function and hemolytic uremic syndrome; however, the association of CHCs to these effects has been neither confirmed nor refuted.[43312] [50744] [62071]
Some people taking combined hormonal contraceptives notice tenderness, swelling, or minor bleeding of their gums, which may lead to gingivitis. Proper attention to oral care and regular dental visits are recommended during desogestrel; ethinyl estradiol use.
The issue of hormonal influences on the development of cancers (new primary malignancy) has been widely researched for many decades. Most studies have been performed with oral combined hormonal contraceptives (CHCs), and the risks related to CHCs, regardless of route of administration, are thought to be similar. In general, the data suggest an increased risk of cervical cancer among CHC users, with a decreased risk for endometrial and ovarian cancers.[43312] [50744] [62071] Epidemiology studies have not found a consistent association between use of CHCs and breast cancer risk. Studies do not show an association between ever (current or past) use of CHCs and risk of breast cancer. However, some studies report a small increase in the risk of breast cancer among current or recent users (less than 6 months since last use) and current users with longer duration of COC use.[62904] Several large, well-designed observational studies have provided data regarding the risk of breast cancer with CHC use.[27233] [24750] [27234] Breast cancers diagnosed in current or previous CHC users tend to be less advanced clinically than in never-users. The risk of breast cancer is only slightly increased in current and recent CHC users (i.e., within 10 years); however, 10 years after CHC cessation, the risk of breast cancer appears to be similar to that in those patients that have never used CHCs.[62647] From one large study published in 2017, the risk of breast cancer was higher among women who currently or recently used contemporary CHCs than among women who had never used CHCs, and this risk increased with longer durations of use; however, absolute increases in risk were small. The absolute risk of breast cancer associated with any CHC use was 13 per 100,000 women-years, which corresponds to 1 extra case of breast cancer for every 7,690 CHC users in 1 year.[62904] Moreover, the same study data suggest that any increased risk of breast cancer usually disappears rapidly after an interruption in the use of CHCs.[62904] There continues to be controversy regarding the risk of CHC use in women with a family history of breast cancer (e.g., BRCA mutations). However, evidence does not suggest that the increased risk for breast cancer among women with either a family history of breast cancer or breast cancer susceptibility genes is modified by the use of CHCs.[48201] Patients should be instructed to perform monthly self-breast examination and report any breast changes, lumps, or discharge to their health care professional. If breast cancer is suspected, CHCs should be discontinued.[43312] [50744] [62071] Some studies suggest that CHC use has been associated with an increase in the risk of cervical cancer or intraepithelial neoplasia; however, such findings may be due to differences in sexual behavior, presence of the human papillomavirus (HPV) and other factors. HPV is thought to be the cause of more than 90% of all cervical cancers, although hormonal factors may influence risk. The relative risk of invasive cervical cancer is 1.37 after 4 years of use; relative risk increased to 1.6 after 8 years of CHC use. Because a potential for cervical dysplasia may exist, regularly evaluate patients taking CHCs via cervical cytology screening as recommended per standards of care.[62647] A meta-analysis of 10 studies indicated significant trends for a reduced risk for endometrial and ovarian cancer with increased duration of CHC use. Risk of endometrial or ovarian cancers may be reduced by up to 60% with 4 or more years of use.[25198] Data suggest CHCs do not protect against hereditary forms of ovarian cancer (e.g., women who carry BRCA1 or BRCA2 gene alterations).[25199] Studies have shown an increased risk of developing hepatocellular carcinoma in long-term (more than 8 years) CHC users. However, these cancers are rare in the U.S., and the attributable risk (the excess incidence) of liver cancers in CHC users approaches less than 1 per million users.[62647][43312] [50744] [62071]
Use of desogestrel; ethinyl estradiol, as with other contraceptive steroids, may result in clinical changes that influence the results of certain laboratory tests, such as coagulation factors, lipids, glucose tolerance, and binding proteins. Specific laboratory test interference has not been reported.[43312] [50744] [62071]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Combined hormonal contraceptives (CHCs), such as desogestrel; ethinyl estradiol, do not protect against human immunodeficiency virus (HIV) infection or other sexually transmitted disease. Patients infected with HIV or with known acquired immunodeficiency syndrome (AIDS) should be aware that the use of a CHC will not prevent the transmission of HIV or other sexually transmitted diseases to their partner(s).[43312][50744][62071]
Combined hormonal contraceptives (CHCs) are contraindicated in people with a current or past history of cerebrovascular disease (including stroke), coronary artery disease, or thromboembolism [including coronary thrombosis, myocardial infarction (MI), thrombophlebitis, thromboembolic disease, or valvular heart disease with complications]. CHCs have been associated with thromboembolic disease such as deep venous thrombosis (DVT) and pulmonary embolism (PE). CHCs are also generally contraindicated in thrombogenic valvular or heart rhythm diseases (e.g., atrial fibrillation or subacute bacterial infective endocarditis with valvular disease atrial fibrillation), or known inherited or acquired hyper-coagulopathic thrombophilia (e.g., protein S deficiency, protein C deficiency, Factor V Leiden, prothrombin G20210A mutation, antithrombin deficiency, antiphospholipid antibodies). People with a history of retinal thrombosis should not receive CHCs due to the potential risk of vision loss should retinal thrombosis occur due to the CHC. Because tobacco smoking increases the risk of serious cardiovascular events and thromboembolism, CHC recipients are strongly advised not to smoke. Risk is especially high for heavy smokers (15 or more cigarettes per day) over 35 years of age; therefore, CHCs are considered contraindicated for tobacco smokers more than 35 years of age. Due to association of estrogen dosage with thromboembolic risk, CHCs containing 50-mcg/day ethinyl estradiol should not be used unless medically indicated. In addition, certain progestins may increase thromboembolic risk. The overall risk of venous thromboembolism in oral CHC users has been estimated to be 3 to 9 per 10,000 woman-years. Preliminary data from a large, prospective cohort safety study suggests that the risk is greatest during the first 6 months after initially starting CHC therapy or restarting (following a break from therapy 4 weeks or more) with the same or different combination product. The risk of arterial thromboses, such as stroke or MI, is especially increased in those with other risk factors, such as pre-existing high blood pressure, renal disease, elevated lipids or cholesterol, diabetes with vascular disease, or if morbidly overweight. After a CHC is discontinued, the risk of thromboembolic disease due to CHCs gradually disappears. CHCs are also associated with increases in blood pressure (BP), and CHCs are considered contraindicated in those with uncontrolled hypertension (e.g., persistent blood pressure values of 160 mmHg systolic or 100 mmHg diastolic or greater) or hypertension with vascular disease. For all CHC users, including those with well-controlled hypertension, monitor BP at routine visits and stop the CHC if BP rises significantly. An increase in BP is more likely in older CHC users with extended duration of use. The effect of CHCs on BP may vary according to the progestin in the CHC. CHCs may also cause fluid retention, and individuals predisposed to complications from edema, such as those with chronic kidney disease (CKD) or cardiac disease should be closely monitored.[43312] [50744] [62071] [30858] [48201]
Major surgery can increase the risk for thromboembolism from combined hormonal contraceptives (CHCs). CHCs are contraindicated when there is major surgery with prolonged immobility. If feasible, discontinue the CHC at least 4 weeks before and for 2 weeks after major surgery or other planned procedure known to have an elevated risk of thromboembolism, and during and following any prolonged immobility.[43312] [50744] [62071]
Because of the increased potential for embolic risk, combined hormonal contraceptives (CHCs) are contraindicated in people who currently have diabetes mellitus and are more than 35 years of age, diabetes mellitus with hypertension or with vascular disease or end-organ damage, or diabetes mellitus of greater than 20 years duration. People with diabetes mellitus should be observed for changes in glucose tolerance when initiating or discontinuing CHCs, since estrogens may exacerbate diabetes. Altered glucose tolerance secondary to decreased insulin sensitivity has been reported.[43312] [50744] [62071]
People who are being treated for dyslipidemia should be followed closely if they elect to use combined hormonal contraceptives (CHCs). Some progestogens may elevate LDL levels and may render the control of hyperlipidemia more difficult. Those with hypertriglyceridemia, or a family history thereof, may be at an increased risk of pancreatitis when using CHCs.[43312] [50744] [62071]
Combined hormonal contraceptive (CHC) products are contraindicated in people with migraine with aura or other headache that is accompanied by focal neurological symptoms. CHCs are also contraindicated in people more than 35 years of age with migraine headaches of any type. The onset or exacerbation of migraine or development of headache with a new pattern which is recurrent, persistent, or severe requires discontinuation of CHCs and evaluation of the cause. A migraine with focal neurologic visual changes should be medically evaluated, as such changes may indicate cerebrovascular events.[43312] [50744] [62071] [30858]
Estrogens, such as those in combined hormonal contraceptives (CHCs), can increase the curvature of the cornea. CHC recipients who wear contact lenses who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.[43312] [50744] [62071] [30858]
Exogenous estrogens may induce or exacerbate symptoms of angioedema in individuals with hereditary angioedema.[43312] [50744] [62071]
Combined hormonal contraceptives (CHCs) are contraindicated for use in people with acute or chronic hepatic disease with abnormal liver function, such as hepatic failure, acute hepatitis or decompensated hepatic cirrhosis. Other liver conditions for which estrogen-containing birth control is inappropriate include Budd-Chiari syndrome, a liver transplant that is not working well, or benign or cancerous hepatic tumors. In general, CHCs are also contraindicated in those with a history of intrahepatic cholestasis of pregnancy or a history of significant adverse event(s) associated with previous use of a hormonal contraceptive. Discontinue the CHC if jaundice or cholestasis develops during use. Acute or chronic disturbances of liver function may necessitate CHC discontinuation until markers of liver function return to normal and CHC causation has been excluded. Patients with hepatitis C infection who are being treated with ombitasvir/paritaprevir/ritonavir, with or without dasabuvir, are also contraindicated to receive CHCs due to a risk for elevated hepatic enzymes and hepatotoxicity. Discontinue CHCs prior to starting hepatitis C therapy with these antiviral regimens; a CHC can be restarted approximately 2 weeks following completion of these hepatitis C combination drug regimens. Estrogen therapy may cause an exacerbation of porphyria and should be used with caution in people with this condition.[43312] [50744] [62071] [48201] [70437]
Use of combined hormonal contraceptives (CHCs) is contraindicated in people with a benign or malignant liver tumor, such as hepatic adenoma or hepatocellular cancer. Benign hepatic adenomas are associated with CHC use, although the incidence of these benign tumors is rare. The attributable risk (the excess incidence) is 3.3 cases/100,000 CHC users. Rupture of hepatic adenomas may cause death through intra-abdominal hemorrhage. Studies have shown an increased risk of developing hepatocellular carcinoma in long-term (more than 8 years) CHC users. However, these cancers are extremely rare in the U.S. and the attributable risk of liver cancers in CHC users is less than 1 per million CHC users. Estrogen therapy may cause an exacerbation of hepatic hemangiomas and should be used with caution in people with this condition.[43312] [50744] [62071]
Given the increased prevalence of hypercoagulable states in people with systemic lupus erythematosus (SLE), consider the thromboembolic risk versus the benefit of combined hormonal contraceptive (CHC) use. Avoid CHCs in SLE patients with a history of venous or arterial thrombosis or the presence of a hypercoagulable state (antiphospholipid antibodies and lupus anticoagulant). If CHCs are initiated in SLE patients without hypercoagulable states, choose a low-dose estrogen contraceptive (e.g., ethinyl estradiol 35 mcg per day or less); consider use of a progestin-only contraceptive. CHCs have also been reported to induce, unmask, or exacerbate SLE; more data are needed.[31435] [48201]
Mood disorders, like depression, may be aggravated in people taking combined hormonal contraceptives (CHCs). Data regarding the association of CHCs with onset of depression or exacerbation of existing depression are limited. If significant depression occurs, the CHC should be discontinued.[43312] [50744] [62071]
Combined hormonal contraceptives (CHCs) are contraindicated in people with a current diagnosis of, or history of, breast cancer, endometrial cancer, or other known or suspected estrogen-dependent tumor, as such tumors may be hormonally-sensitive. CHCs are also contraindicated in people with abnormal uterine bleeding; evaluate such patients before use to determine if a contraindication to CHC use exists. Clinical surveillance of all individuals using CHCs is important; perform breast examinations or mammography, pelvic examination, and other diagnostic or screening tests, such as cervical cytology (pap smears), as clinically indicated or as generally recommended based on age, risk factors, and other individual needs.[43312] [50744] [62071] [48201]
Use combined hormonal contraceptives (CHCs) with caution in people with existing gallbladder disease as CHCs may worsen gallbladder disease. Consider discontinuing CHCs in people with symptomatic gallbladder disease or cholestatic disease. Earlier studies have reported an increased lifetime relative risk of gallbladder surgery in users of CHCs and estrogens. More recent studies, however, have shown that the relative risk of developing gallbladder disease among CHC users may be minimal. The recent findings of minimal risk may be related to the use of CHC formulations containing lower hormonal doses of estrogens and progestogens.[43312] [50744] [62071]
Avoid combined hormonal contraceptives (CHCs) in persons with a history of chloasma gravidarum or increased sensitivity to sun and/or ultraviolet radiation exposure. Chloasma (melasma) may occur with CHC use, especially in people with a history of chloasma gravidarum.[43312] [50744] [62071]
The estrogen component of combined hormonal contraceptives (CHCs) may raise the serum concentrations of thyroid-binding globulin, sex hormone-binding globulin, and cortisol-binding globulin. Doses of thyroid hormone replacement for hypothyroidism may need to be increased, as indicated by clinical and laboratory monitoring for the individual. Cortisol replacement therapy (e.g., corticosteroid therapy) may also need adjusted for some individuals taking CHCs.[43312] [50744] [62071]
Preexisting morbid obesity is one factor that may increase cardiovascular or thromboembolic risks associated with combination hormonal contraceptives (CHCs). Consider the presence of obesity and other underlying risk factors that may increase the risk of cardiovascular disease or thromboembolism, particularly for people more than 35 years of age.[43312] [50744] [62071] Limited literature suggests that the effectiveness of some hormonal contraceptive formulations might decrease with increasing body mass index (BMI). However, the evidence is conflicting; there are also data to suggest that the efficacy of most CHC products (with a few known exceptions) does not seem to be compromised in those who are overweight.[48201] [66895]
Discontinue desogestrel; ethinyl estradiol if pregnancy is detected as there is no reason to continue combined hormonal contraceptives (CHCs) during pregnancy. Epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies and limb-reduction defects) following exposure to CHCs before conception or during early pregnancy. The administration of CHCs to induce withdrawal bleeding should not be used as a test for pregnancy. CHCs should not be used during pregnancy to treat threatened or habitual abortion. For any CHC user who has missed 2 consecutive periods, pregnancy should be ruled out before continuing CHC use. If the CHC user has not adhered to the prescribed schedule, consider the possibility of pregnancy at the first missed period; discontinue the CHC until pregnancy is ruled out.[43312] [50744] [62071] [30858]
Product labels for combined hormonal contraceptives (CHCs) recommend avoidance if possible during breast-feeding until the lactating individual has completely weaned their child. Small amounts of hormonal contraceptive steroids (estrogens and progestins) have been identified in human milk and a few reports of effects on the infant exist, including jaundice and breast enlargement.[43312] [50744] [62071] The U.S. Medical Eligibility Criteria (USMEC) state that CHCs should not be used during the first 4 weeks after delivery because of concerns about the potential effects of estrogen on breast-feeding performance during the establishment of lactation. If a patient is breast-feeding and begins taking a CHC 4 to 6 weeks after delivery, the breastfed infant should be monitored for appetite changes, hormonal side effects, and proper weight gain/growth.[48201] One study found that low-dose CHCs (e.g., 10 mcg per day ethinyl estradiol) may not adversely affect lactation.[48200] However, a systematic review concluded that the available evidence, even from randomized controlled trials, is limited and of low quality; proper trials are needed.[48202] The World Health Organization (WHO) Contraceptive Criteria has recommendations that are more restrictive than USMEC; the WHO criteria state CHCs should not be used in breast-feeding individuals before 42 days after birth and that the disadvantages of CHC use generally outweigh the advantages between 6 weeks and 6 months after birth for individuals who are breast-feeding.[48204] Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods, spermicides) and progestin-only contraceptives (e.g., medroxyprogesterone contraceptive injections, norgestrel oral contraceptive, levonorgestrel IUDs).[48201]
The U.S. Medical Eligibility Criteria state to avoid combined hormonal contraceptives (CHCs) during the first 3 weeks postpartum because of the increased risk for venous thromboembolism in the early postpartum period. Postpartum individuals with additional risk factors for venous thromboembolism (VTE) (e.g., 35 years of age or older, previous VTE, thrombophilia, immobility, transfusion at delivery, peripartum cardiomyopathy, obesity with a BMI of 30 kg/m2 or more, postpartum hemorrhage, post-cesarean delivery, preeclampsia, or tobacco smoking) should generally not use CHCs until at least 6 weeks after delivery. CHCs may be used after 6 weeks postpartum without restriction if no other contraindications to CHCs exist, as postpartum thromboembolism risk returns to baseline.[48201]
The primary action of the combination of an estrogen with a progestin is to suppress the hypothalamic-pituitary system, decreasing the secretion of gonadotropin-releasing hormone (GnRH). Progestins blunt luteinizing hormone (LH) release, and estrogens suppress follicle-stimulating hormone (FSH) from the anterior pituitary. Both estrogen and progestin ultimately inhibit maturation and release of the dominant ovule. In addition, viscosity of the cervical mucus increases with hormonal contraceptive use, which increases the difficulty of sperm entry into the uterus. Alteration in endometrial tissues also occurs, which reduces the likelihood of implantation of the fertilized ovum. The contraceptive effect is reversible.[43312][50744][62071]
Both estrogens and progestins are responsible for a number of other metabolic changes. The summary of these changes is dependent on the net actions of the estrogen and progestin combinations. At the cellular level, estrogens and progestins diffuse into their target cells and interact with a protein receptor. Metabolic responses to estrogens and progestins require an interaction between DNA and the hormone-receptor complex. Target cells include the female reproductive tract, the mammary gland, the hypothalamus, and the pituitary. Estrogens increase the hepatic synthesis of sex hormone binding globulin (SHBG), thyroid-binding globulin (TBG), and other serum proteins. Estrogens generally have a favorable effect on blood lipids, reducing LDL and increasing HDL cholesterol concentrations. Serum triglycerides increase with estrogen administration. Folate metabolism and excretion is increased by estrogens and may lead to slight serum folate deficiency. Estrogens also enhance sodium and fluid retention. Progestins are classified according to their progestational, estrogenic and androgenic properties. Progestins can alter hepatic carbohydrate metabolism, increase insulin resistance, and have either little to slightly favorable effects on serum lipoproteins. Less androgenic progestins, like desogestrel, have only slight effects on carbohydrate metabolism. More androgenic progestins can aggravate acne. Serious adverse events, like thrombosis, are primarily associated with the estrogen component of hormonal contraceptives but may be the result of both estrogen and progestin components. The mechanism for thrombosis may be associated with increased clotting factor production and/or decreases in anti-thrombin III. Minor side effects can be addressed by choosing formulations that take advantage of relative estrogen, progestin, and androgenic potencies.[60767]
Revision Date: 09/26/2025, 01:32:00 AMDesogestrel; ethinyl estradiol is administered orally. Etonogestrel, the active metabolite of desogestrel, was found to be approximately 98% protein bound, primarily to sex hormone-binding globulin (SHBG). Ethinyl estradiol is approximately 98.3% bound, mainly to plasma albumin. Ethinyl estradiol does not bind to SHBG, but induces SHBG synthesis. Desogestrel, in combination with ethinyl estradiol, does not counteract the estrogen-induced increase in SHBG, resulting in lower serum levels of free testosterone. Desogestrel is rapidly and completely metabolized by hydroxylation in the intestinal mucosa and on first pass through the liver to etonogestrel (also known as 3-keto-desogestrel) which is active. In vitro data suggest an important role for hepatic CYP2C9 in the bioactivation of desogestrel. CYP3A4 catalyzes further metabolism of etonogestrel into 6beta-hydroxy etonogestrel and 6beta-13ethyl dihydroxylated metabolites as major metabolites. Other metabolites that are not active (i.e., 3alpha-OH-desogestrel, 3beta-OH-desogestrel, and 3alpha-OH-5alpha-H-desogestrel) also have been identified, and these metabolites are further metabolized to sulfates and glucuronides. Ethinyl estradiol is subject to a significant degree of presystemic conjugation (phase II metabolism). Ethinyl estradiol, escaping gut wall conjugation, undergoes phase I metabolism and hepatic conjugation (phase II metabolism). The major phase I metabolites are 2-OH-ethinyl estradiol and 2-methoxy-ethinyl estradiol. Sulfate and glucuronide conjugates of both ethinyl estradiol and phase I metabolites, which are excreted in bile, can undergo enterohepatic circulation. Etonogestrel and ethinyl estradiol are primarily eliminated in urine, bile and feces. For monophasic tablets, the elimination half-life for 3-keto-desogestrel (etonogestrel) is approximately 38 +/- 20 hours and the ethinyl estradiol elimination half-life is 26 +/- 6.8 hours at steady state.[50744] For the biphasic products on Day 21, the elimination half-life of etonogestrel is 27.8 +/-7.2 hours and the elimination half-life of ethinyl estradiol is 23.9 +/- 25.5 hours for the combined tablet, but the ethinyl estradiol tablet half-life is around 18.9 +/-8.3 hours.[43312] At steady state, on Day 21, the elimination half-lives of the triphasic products are 37.1 +/- 14.8 hours for etonogestrel and 28.2 +/- 10.5 hours for ethinyl estradiol, respectively.[62071]
Affected Cytochrome P450 isoenzymes and drug transporters: CYP3A4, P-glycoprotein (P-gp), UGT1A1, SULT1E1, CYP2C9
Since ethinyl estradiol and desogestrel are partially metabolized by CYP3A4, interactions with drugs that are inhibitors or inducers of CYP3A4 are possible. Drugs or herbal products that induce CYP3A4 may decrease the efficacy of contraception or may increase the risk for breakthrough bleeding. It is recommended to avoid the concomitant use of a strong CYP3A inducer to mitigate the risk of potential contraceptive failure. Moderate and weak inducers may also affect progestin and estrogen exposures depending on the agent. Exposure of ethinyl estradiol is generally increased by up to 50% when coadministered with moderate or strong inhibitors of CYP3A4.[70622] The ability for inducers or inhibitors of CYP2C9 to affect desogestrel pharmacokinetics is possible, but there are no specific studies. Ethinyl estradiol is a substrate of the drug transporter P-gp, but data suggest that clinical drug interactions are not expected with P-gp inhibitors or inducers.[60859][70622] There are not enough data to assess the effects of modulation of UGT1A1 or SULT1E1 on hormone concentrations in these products.[70622] Ethinyl estradiol has been shown to induce lamotrigine glucuronidation.[43312][50744][62071]
Desogestrel is rapidly and almost completely absorbed and converted into etonogestrel, its biologically active metabolite. Following oral administration, the relative bioavailability of desogestrel, as measured by serum levels of etonogestrel (also known as 3-keto-desogestrel), is approximately 84% for the monophasic products and approximately 100% when compared to an oral solution for the biphasic and triphasic contraceptive products. Ethinyl estradiol is rapidly and almost completely absorbed. The relative bioavailability of ethinyl estradiol was 83% for the monophasic and in the range of 93% to 99% for the biphasic and triphasic contraceptive products. The effect of food on bioavailability following oral administration has not been evaluated.[43312][50744][62071]
Steroid hormones may be poorly metabolized in patients with impaired liver function.[43312][50744][62071]
Pharmacokinetic data regarding use of desogestrel; ethinyl estradiol contraceptives in people with renal impairment are not available.[43312][50744][62071]
There are no data regarding the effect of race on the pharmacokinetics of desogestrel; ethinyl estradiol contraceptives.[62071]
Specific pharmacokinetic data regarding the effect of weight are not available for desogestrel; ethinyl estradiol contraceptive products.[43312][50744][62071]
Discontinue desogestrel; ethinyl estradiol if pregnancy is detected as there is no reason to continue combined hormonal contraceptives (CHCs) during pregnancy. Epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies and limb-reduction defects) following exposure to CHCs before conception or during early pregnancy. The administration of CHCs to induce withdrawal bleeding should not be used as a test for pregnancy. CHCs should not be used during pregnancy to treat threatened or habitual abortion. For any CHC user who has missed 2 consecutive periods, pregnancy should be ruled out before continuing CHC use. If the CHC user has not adhered to the prescribed schedule, consider the possibility of pregnancy at the first missed period; discontinue the CHC until pregnancy is ruled out.[43312] [50744] [62071] [30858]
Product labels for combined hormonal contraceptives (CHCs) recommend avoidance if possible during breast-feeding until the lactating individual has completely weaned their child. Small amounts of hormonal contraceptive steroids (estrogens and progestins) have been identified in human milk and a few reports of effects on the infant exist, including jaundice and breast enlargement.[43312] [50744] [62071] The U.S. Medical Eligibility Criteria (USMEC) state that CHCs should not be used during the first 4 weeks after delivery because of concerns about the potential effects of estrogen on breast-feeding performance during the establishment of lactation. If a patient is breast-feeding and begins taking a CHC 4 to 6 weeks after delivery, the breastfed infant should be monitored for appetite changes, hormonal side effects, and proper weight gain/growth.[48201] One study found that low-dose CHCs (e.g., 10 mcg per day ethinyl estradiol) may not adversely affect lactation.[48200] However, a systematic review concluded that the available evidence, even from randomized controlled trials, is limited and of low quality; proper trials are needed.[48202] The World Health Organization (WHO) Contraceptive Criteria has recommendations that are more restrictive than USMEC; the WHO criteria state CHCs should not be used in breast-feeding individuals before 42 days after birth and that the disadvantages of CHC use generally outweigh the advantages between 6 weeks and 6 months after birth for individuals who are breast-feeding.[48204] Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods, spermicides) and progestin-only contraceptives (e.g., medroxyprogesterone contraceptive injections, norgestrel oral contraceptive, levonorgestrel IUDs).[48201]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.