ThisiscontentfromElsevier'sDrugInformation
Drospirenone
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
1 tablet (4 mg drospirenone) PO once daily for 24 days, followed by 4 days of non-hormonal, inactive tablets PO once daily in the order directed on the pack. Cycle repeats every 28 days. Patients should begin taking this product on day 1 of the menstrual cycle (first day of menstruation). When switching from another contraceptive, patients should start taking this oral contraceptive on the same day that a new pack of the previous oral contraceptive would have been started, or on the day when the next transdermal patch application, vaginal ring insertion, or injection would have been scheduled. Patients switching from an IUD or implant to this oral contraceptive should start on the day of removal.[64244]
4 mg/day PO.
Safety and efficacy have not been established.
4 mg/day PO.
Not indicated in prepubescent females.
Not indicated.
Use is contraindicated.[64244]
CrCl less than 80 mL/minute: Use is contraindicated.[64244]
† Off-label indication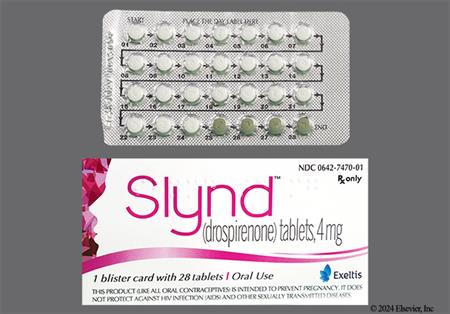
Drospirenone is a progestin-only oral contraceptive and a fourth generation progestin that is an analog of spironolactone with antimineralocorticoid and antiandrogenic properties. Hormonal progestin-only contraceptives can be used in people from menarche to over the age of 40 years up until the time of menopause with proper selection of products. The choice of a routine hormonal contraceptive for any given patient is based on the individual's contraceptive needs, underlying medical conditions or risk factors for adverse effects, and individual preferences for use. The Centers for Disease Control's U.S. Medical Eligibility Criteria describe considerations for risk vs. benefits, including medical conditions or attributes that contraindicate use; these criteria can help prescribing practitioners in product selection for individual patients.[48201][66717] Drospirenone may increase potassium concentrations; do not use drospirenone in people with significant risks for hyperkalemia, such as those with kidney, liver, or adrenal insufficiency. Individuals taking drugs that could increase serum potassium should consult their health care team before taking drospirenone-containing oral contraceptives. Drospirenone-only contraception was FDA-approved in May 2019.[64244]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Administration instructions for patients:
Instructions for missed doses:
Advice in Case of Gastrointestinal Disturbances:
If vomiting or diarrhea occurs within 3 to 4 hours after tablet taking, the new tablet (scheduled for the next day) should be taken as soon as possible. The new tablet should be taken within 12 hours of the usual time of tablet-taking if possible. If more than 2 tablets are missed, the advice concerning 2 missed tablets, including using backup non-hormonal contraception, is applicable.[64244]
Breast tenderness or mastalgia (1.2%), breast pain (2.2%), breast enlargement, and breast discharge or secretion have been reported in patients receiving oral contraceptives such as drospirenone and are believed to be drug-related.[64244] Galactorrhea and lactation suppression may also occur.
Breakthrough bleeding (spotting) (1.7%) and metrorrhagia (2.8%) are sometimes encountered, especially during the first 3 months of oral contraceptive use such as drospirenone. Change in menstrual flow (menstrual irregularity) (1.2%) and amenorrhea have also been reported and are believed to be drug-related. Other adverse effects may include dysmenorrhea (1.9%), menorrhagia, oligomenorrhea, and pelvic pain. Based on subject diaries from 4 clinical trials of drospirenone, 64.4% of females experienced unscheduled bleeding at Cycle 1. This percentage decreased to 40.3% by cycle 13. A total of 91 out of 2593 subjects (0.4%) discontinued drospirenone due to menstrual bleeding disorders including metrorrhagia, menstrual irregular, vaginal hemorrhage, menorrhagia, uterine hemorrhage, and amenorrhea. In the event of breakthrough vaginal bleeding, consider nonhormonal causes and take adequate diagnostic measures to rule out malignancy or pregnancy. If pathology has been excluded, time or a change to another formulation may solve the problem. In the event of amenorrhea, rule out pregnancy. Some women may encounter post-pill amenorrhea or oligomenorrhea, especially when such a condition was pre-existent.[64244]
Weight gain was reported in 1.9% of patients receiving drospirenone.[64244]
Nausea was reported in 1.8% of patients receiving drospirenone.[64244]
Libido decrease was reported in 1.3% of patients receiving drospirenone.[64244]
Headache was reported in 2.7% of patients receiving drospirenone.[64244]
Acne vulgaris was reported in 3.8% of patients receiving drospirenone.[64244]
The antimineralocorticoid actions of 3 mg of drospirenone are comparable to 25 mg of spironolactone and may cause hyperkalemia in predisposed patients. Most females with hyperkalemia in the clinical development studies of drospirenone had mild potassium elevations and/or isolated increases that returned to normal while still on study medication. No concurrent adverse reactions were attributed to hyperkalemia. In the pivotal trial, 2 females (0.2%) with persistent potassium elevations discontinued drospirenone. It is essential to avoid drospirenone in patients with adrenal insufficiency, hepatic disease, or renal disease, who are at higher risk for hyperkalemia from drospirenone.[64244]
Drospirenone is contraindicated in people with renal impairment (i.e., CrCl less than 80 mL/minute), renal failure, or adrenal insufficiency. Drospirenone has antimineralocorticoid activity and may increase serum potassium, and may predispose certain patients to hyperkalemia or impaired adrenal function. People taking daily, long-term treatment for chronic conditions or diseases with medications that may increase serum potassium concentration should have their serum potassium concentration checked before starting drospirenone and during the first treatment cycle. Monitor people taking drospirenone who later develop a medical condition and/or begin medication that has an increased risk for hyperkalemia.[64244]
Drospirenone is contraindicated in patients with hepatic disease, jaundice, or hepatic tumors (benign or hepatocellular cancer). The mean exposure to drospirenone in females with moderate hepatic impairment is approximately 3 times higher than the exposure in females with normal liver function. Increased drospirenone exposure increases risks for hyperkalemia and other side effects. Discontinue drospirenone use if jaundice or acute or chronic disturbances of liver function develop. Do not resume use until markers of liver function return to normal and drospirenone causation has been excluded.[64244]
Epidemiological studies have not indicated an association between progestin-only preparations and an increased risk of arterial or venous thromboembolism. When prescribing drospirenone, consider the increased risk of thromboembolism inherent in the postpartum period and in females with a known history of thromboembolism, including myocardial infarction or stroke. Discontinue drospirenone if arterial or venous thromboembolic events occur.[64244] Tobacco smoking increases the risk of serious cardiovascular disease, myocardial infarction, and stroke. Women who use oral contraceptives should be strongly advised not to smoke. There are no studies definitely linking progestin-only pill (POP) use to an increased risk of heart attack or stroke.[48201] Despite the caution against use in patients with known thrombotic disease, progestin-only contraceptives are generally the hormonal contraceptives of choice in patients with a potential risk for thrombosis when reliable contraception must be ensured and the risks of hormonal therapy are acceptable; advantages of these methods usually outweigh proven or theoretical risks.[48201] When multiple risk factors exist for thromboembolic disease (e.g., tobacco smoking, women 35 years and older, diabetes, cerebrovascular disease, hypercoagulopathy, valvular or ischemic heart disease, severe hypertension, etc.), the risk of thromboembolic disease may increase; determine individual risk vs. benefit for use of the progestin-only contraceptive. The increase in the risk of thrombosis from newer progestin-only contraceptives (e.g.,drospirenone) is still substantially less than with combined oral contraceptives containing both estrogen and progestin.[48201] Consider discontinuing drospirenone, if feasible, in case of prolonged immobilization due to major surgery or illness, since these situations increase risk for thromboembolism.[64244]
Drospirenones should be used cautiously in patients with diabetes mellitus. Although the effects appear to be minimal during therapy with progestins, altered glucose tolerance secondary to decreased insulin sensitivity has been reported during hormonal contraceptive therapy.[64244]
Mood disorders, like depression, may be aggravated in women taking exogenous hormones. Women with a history of depression may need special monitoring. Data on the association of progestin-only contraceptive products with onset of depression or exacerbation of depression are limited. If significant depression occurs, drospirenone should be discontinued.[64244]
Drospirenone is contraindicated in patients with known or suspected progestin-sensitive cancers, such as breast cancer. Progestin-only oral contraceptives do not appear to cause breast cancer. However patients who have or have had a cancer that may be sensitive to hormones should not use hormonal contraceptives.[64244] [48201]
Drospirenone is contraindicated in undiagnosed abnormal vaginal bleeding and in patients with known or suspected progestin-sensitive cancers of reproductive organs, such as cervical cancer or uterine cancer. Women who use hormonal contraceptives may have a higher chance of getting cervical cancer. However, the increased risk observed with some hormonal contraceptives may be due to other reasons such as having more sexual partners and exposure to the human papilloma virus (HPV).[64244]
Discontinue drospirenone if pregnancy occurs, because there is no reason to use hormonal contraceptives during pregnancy. Epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies and limb-reduction defects) following maternal use of oral contraceptive progestins before conception or during early pregnancy.[64244]
Be alert to the possibility of ectopic pregnancy in females who become pregnant or complain of lower abdominal pain while on drospirenone. Progestin-only oral contraceptive users have a higher absolute rate of ectopic pregnancy than do users of other hormonal contraceptives, but the risk is still lower than individuals using no method.[64244] [48201]
Progestin-only oral contraceptives are considered compatible with breast-feeding.[48201] Negligible amounts of drospirenone are excreted into breast milk during routine contraceptive use, resulting in infant plasma levels that are approximately 1.5% of those found in maternal plasma, even with exclusive breast-feeding. At therapeutic doses of drospirenone, no effects on breastfed newborns/infants are anticipated. In general, no adverse effects have been found on milk production or on the health, growth, or development of the infant with use of progestin-only oral contraceptives. When prescribing drospirenone, consider the increased risk of thromboembolism inherent in the postpartum period or if the postpartum individual has increased thromboembolic risk.[64244] Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods) and other progestin-only contraceptives (e.g., medroxyprogesterone contraceptive injections, norgestrel oral contraceptive, levonorgestrel IUDs).[48201]
The contraceptive effect of drospirenone is achieved primarily by the suppression of ovulation. Progestins also thicken the cervical mucus to inhibit sperm penetration and make the endometrial lining less suitable for implantation. Drospirenone has no androgenic, estrogenic, glucocorticoid, or antiglucocorticoid activity. As an analog of spironolactone, the drug exhibits both antimineralocorticoid and antiandrogenic activity. Thus this progestin inhibits testosterone production by the ovaries and adrenal glands, as well as some peripheral testosterone synthesis. Drospirenone's endocrine activity may improve luteal symptoms such as negative mood, water retention, and increased appetite. However, the antimineralocorticoid actions of drospirenone are comparable to spironolactone and may increase serum potassium levels in some patients. Progestins in general can alter hepatic carbohydrate metabolism, increase insulin resistance, and have either little to slightly favorable effects on serum lipoproteins. Less androgenic progestins, like drospirenone, have only slight effects on carbohydrate metabolism and are less likely to aggravate acne or blood pressure.[64244][60767][51282]
Revision Date: 08/06/2025, 01:33:00 AMDrospirenone is administered orally, and like other progestins, is widely distributed. Drospirenone is 97% bound to other serum proteins and does not bind to SHBG or CBG. Drospirenone is extensively metabolized to 2 main metabolites, the acid form of drospirenone and the 4,5-dihydrodrospirenone-3-sulfate. These metabolites were shown not to be pharmacologically active. Drospirenone is also subject to oxidative metabolism catalyzed by CYP3A4. Excretion of drospirenone as inactive metabolites occurs via the urine and feces. The terminal elimination half-life is approximately 30 hours. It is the prolonged biologic effects of the hormone that allows for once-daily administration.[64244]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: CYP3A4
Drospirenone is subject to oxidative metabolism catalyzed by CYP3A4. Drugs or herbal products that induce CYP3A4 may decrease the systemic concentrations of drospirenone and potentially diminish the effectiveness of drospirenone or increase the risk of breakthrough bleeding. Drugs that are potent inhibitors of CYP3A4 may moderately increase drospirenone concentrations.[64244]
The pharmacokinetics of oral drospirenone is dose-proportional following single doses ranging from 1 to 10 mg. Following a single ingestion of drospirenone, maximum concentrations (Cmax) of drospirenone in plasma of about 27 ng/mL are attained at 2 to 6 hours. During a treatment cycle, maximum steady-state concentrations of drospirenone in serum of about 41 ng/mL are reached after about 10 days of treatment. Plasma drospirenone Cmax and area under the curve (AUC) accumulate by a factor of about 1.5 to 2 following multiple dose administration. Concomitant ingestion of food has no influence on the extent of absorption of drospirenone.[64244]
Drospirenone is contraindicated in patients with hepatic disease. The mean exposure to drospirenone in females with moderate liver impairment is approximately 3 times higher than the exposure in females with normal liver function. Drospirenone has not been studied in patients with severe hepatic impairment.[64244]
In a pharmacokinetic study, drospirenone kinetics and its effect on serum potassium were evaluated in the presence of renal impairment. All subjects (n = 28) were on a low potassium diet, and 7 subjects were allowed to continue use of potassium-sparing drugs. At day 14 of treatment, similar drospirenone concentrations were observed between subjects with normal renal function (CrCl more than 80 mL/minute) and those with mild renal impairment (CrCl 50 to 80 mL/minute). Drospirenone concentrations were 37% greater among patients with moderate renal impairment (CrCl 30 to 50 mL/minute) compared to those with normal renal function. No clinically significant effect on serum potassium concentration were observed during the study. Hyperkalemia was not observed; however, serum potassium concentrations increased by up to 0.33 mEq/L in 5 of 7 patients allowed to continue use of potassium-sparing drugs.[64244]
Discontinue drospirenone if pregnancy occurs, because there is no reason to use hormonal contraceptives during pregnancy. Epidemiologic studies and meta-analyses have not found an increased risk of genital or nongenital birth defects (including cardiac anomalies and limb-reduction defects) following maternal use of oral contraceptive progestins before conception or during early pregnancy.[64244]
Progestin-only oral contraceptives are considered compatible with breast-feeding.[48201] Negligible amounts of drospirenone are excreted into breast milk during routine contraceptive use, resulting in infant plasma levels that are approximately 1.5% of those found in maternal plasma, even with exclusive breast-feeding. At therapeutic doses of drospirenone, no effects on breastfed newborns/infants are anticipated. In general, no adverse effects have been found on milk production or on the health, growth, or development of the infant with use of progestin-only oral contraceptives. When prescribing drospirenone, consider the increased risk of thromboembolism inherent in the postpartum period or if the postpartum individual has increased thromboembolic risk.[64244] Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods) and other progestin-only contraceptives (e.g., medroxyprogesterone contraceptive injections, norgestrel oral contraceptive, levonorgestrel IUDs).[48201]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.