ThisiscontentfromElsevier'sDrugInformation
Estradiol
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
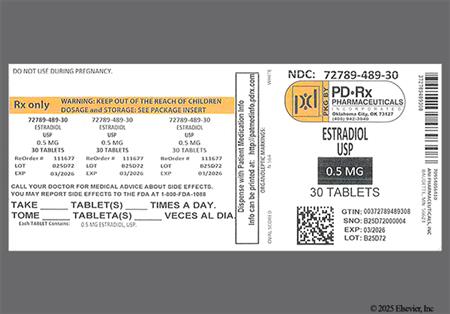
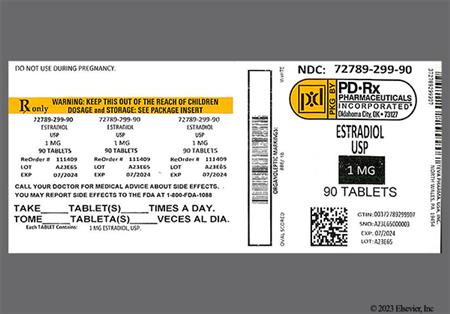
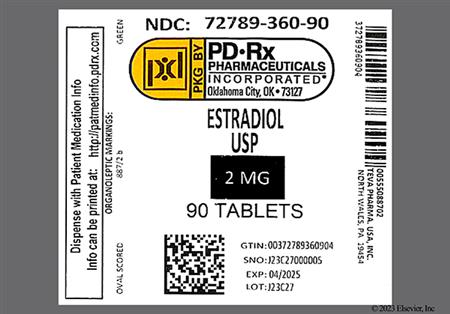
0.5 to 2 mg PO once daily. Usual initial dose: 1 or 2 mg PO once daily. Less than 1 mg/day may suffice for vaginal/vulvar symptoms only; however, in such persons, consider vaginal therapy alone. Use the lowest effective dose. Administration should be cyclic (e.g., 3 weeks on and 1 week off). In persons with an intact uterus, estrogen may be given cyclically or combined with a progestogen for at least 10 to 14 days per month to minimize the risk of endometrial hyperplasia. Continuous, unopposed estrogen administration is acceptable in persons without a uterus. Assess the need for continued use periodically.[67040] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
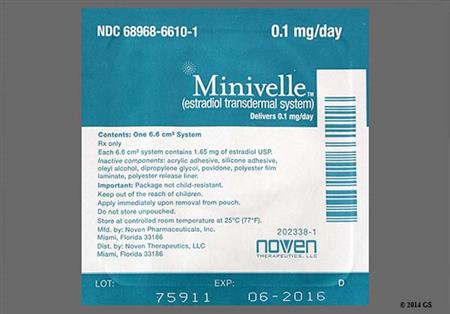
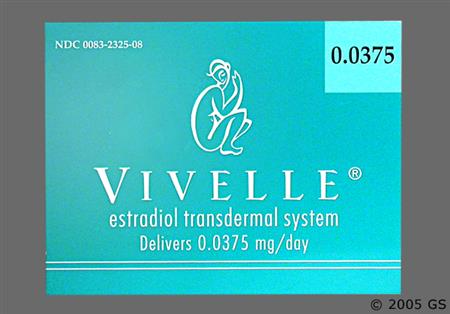
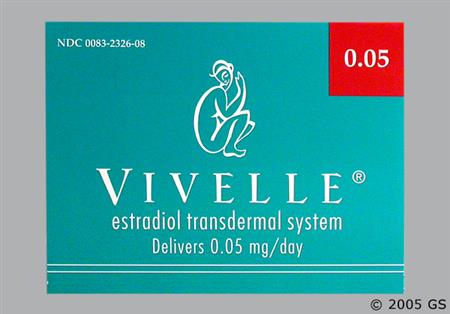
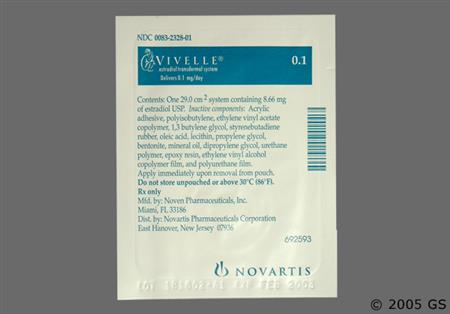
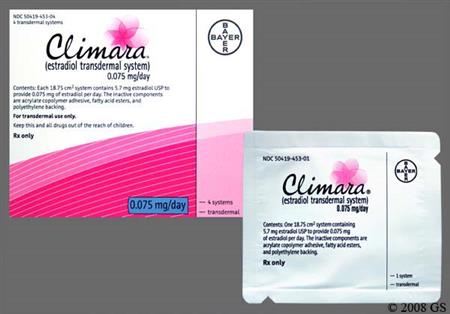
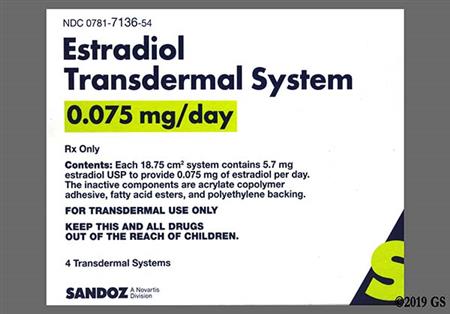
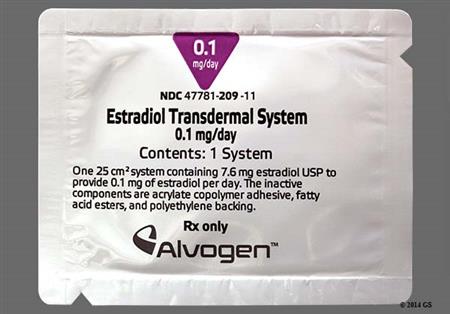
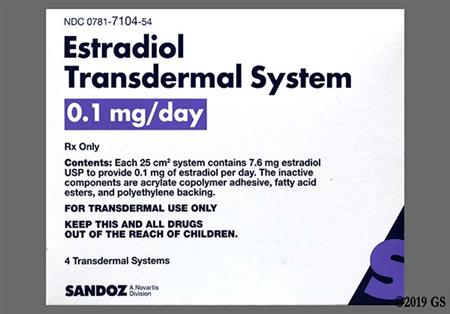
0.0375 or 0.05 mg/day transdermally twice weekly (every 3 to 4 days), initially. Adjust dose based on clinical response. Use the lowest effective dose. Dose range: 0.025 to 0.1 mg/day. A switch between transdermal system types can be done immediately; if on oral therapy, begin a week after oral treatment stopped or when symptoms reappear. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[51117] [58103] [57779] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
0.025 mg/day transdermally once weekly, initially. Adjust dose based on clinical response. Use the lowest effective dose. Max: 0.1 mg/day. A switch between transdermal system types can be done immediately; if on oral therapy, begin 1 week after oral treatment is discontinued or when symptoms reappear. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[52448] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
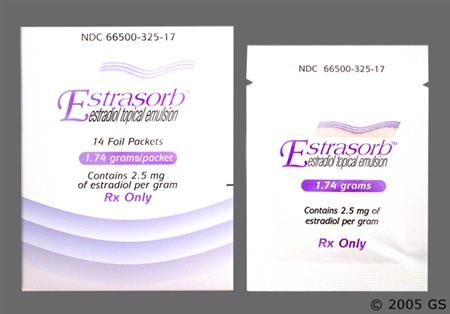
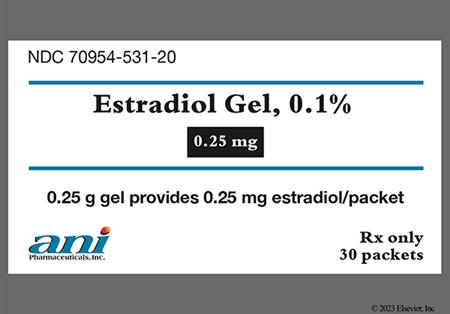
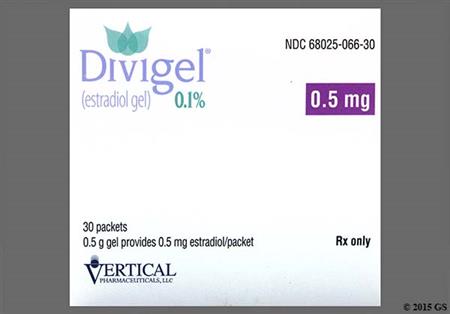
0.25 g (0.25 mg estradiol) transdermally once daily, initially. Adjust dose based on clinical response. Use the lowest effective dose. Max: 1.25 g/day (1.25 mg estradiol/day). Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, consider a progestogen to reduce the risk of endometrial hyperplasia.[62077] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
0.87 g (0.52 mg estradiol) transdermally once daily, initially. Adjust dose based on clinical response. Use the lowest effective dose. Max: 1.7 g/day (1.04 mg estradiol/day). Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[32946] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
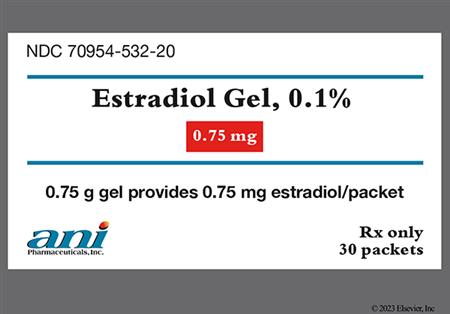
1.25 g (0.75 mg estradiol) transdermally once daily. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[56912] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
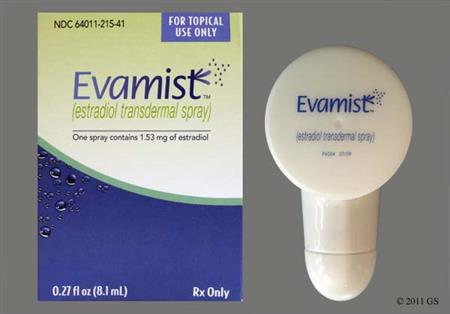
1.53 mg transdermally once daily, initially. Adjust dose based on clinical response. Use the lowest effective dose. Max: 4.59 mg/day. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[46639] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
0.05 mg/day intravaginally every 3 months, initially. Adjust dose based on clinical response. Use the lowest effective dose. Max: 0.1 mg/day. Remove and replace the vaginal ring after 3 months if continued therapy is desired. Assess the need for continued use periodically. The 0.05 mg/day vaginal ring has a central core that contains 12.4 mg of estradiol acetate, which releases at a rate equivalent to 0.05 mg/day for 3 months, and the 0.1 mg/day vaginal ring has a central core that contains 24.8 mg of estradiol acetate, which releases at a rate equivalent to 0.1 mg/day for 3 months. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[51110] Guidelines support the initiation of hormone replacement therapy (HRT) around the time of menopause if no contraindications to use exist and use is acceptable to the individual, as hormone therapy is the most effective treatment for vasomotor and genitourinary symptoms and has been shown to prevent bone loss and fracture.[50638] Early initiation of HRT and continuation of use until the median age of menopause (52 years) is recommended in persons with premature natural or surgically induced menopause. HRT for vasomotor symptoms and/or increased risk for bone loss around the time of menopause may be considered in those younger than 60 years or who are fewer than 10 years from menopause onset.[50638] [52408] For persons who initiate HRT more than 10 or 20 years from menopause onset or are 60 years or older, the benefit-risk ratio is less favorable due to known risks for HRT (e.g., stroke, myocardial infarction, venous thromboembolism, dementia, urinary incontinence), and guidelines generally recommend against use. Decisions regarding whether to continue systemic HRT in persons older than 60 years should be made on an individual basis for quality of life, persistent vasomotor symptoms, or prevention of bone loss and fracture, with consideration given to alternative treatments for prevention of bone loss and other health issues.[50638] [52408]
10 to 20 mg IM every 4 weeks.[61114]
1 to 5 mg IM every 3 to 4 weeks as necessary.[61115]
0.5 to 1 g (50 to 100 mcg estradiol) intravaginally once daily for 2 weeks, then 0.5 g to 1 g (50 to 100 mcg estradiol) intravaginally 1 to 3 times weekly.[50638] [70101] The FDA-approved dosage is 2 to 4 g (200 to 400 mcg estradiol) intravaginally once daily for 1 to 2 weeks, then gradually reduce dose to one-half of the initial dose over 1 to 2 weeks. Usual maintenance dose: 1 g (estradiol 100 mcg) intravaginally 1 to 3 times weekly.[47276] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101]
7.5 mcg/day intravaginally every 3 months. Remove and replace the vaginal system after 3 months if continued therapy is desired. Assess the need for continued use periodically. The estradiol vaginal system contains 2 mg of estradiol to deliver 7.5 mcg/day over 90 days. The estradiol vaginal system is not effective at treating vasomotor symptoms. When used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[49752] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101]
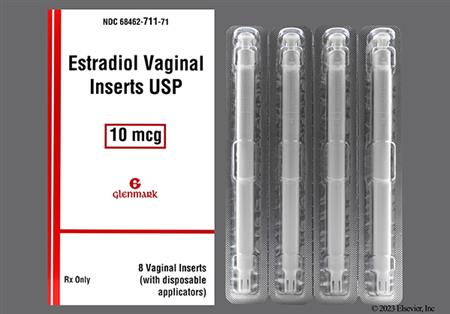
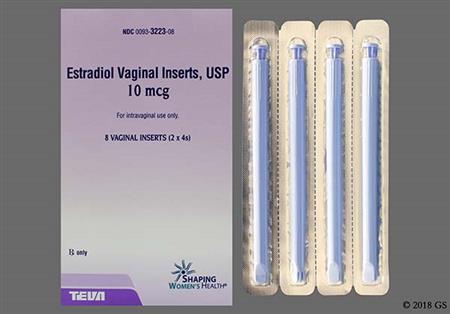
10 mcg intravaginally once daily for 2 weeks, then 10 mcg intravaginally twice weekly (e.g., every Tuesday and Friday). Use the lowest effective dose. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[49751] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101]
4 mcg intravaginally once daily for 2 weeks, then 4 mcg intravaginally twice weekly (e.g., Monday and Thursday). Adjust dose based on clinical response. Use the lowest effective dose. Max: 10 mcg/dose. Assess the need for continued use periodically. Generally, when used in a postmenopausal person with an intact uterus, a progestogen should also be considered to reduce the risk of endometrial hyperplasia.[63254] When isolated genitourinary symptoms caused by menopause are present, guidelines recommend low-dose vaginal estrogens over systemic estrogens as first-line therapy.[50638] [70101]
Dosage range is 0.5 mg to 2 mg PO once daily. Only consider for women at significant risk for osteoporosis and for whom non-estrogen medications are not considered to be appropriate. Use the lowest effective dose. Continuous unopposed estrogen administration is acceptable in those without a uterus. In women with an intact uterus, consider a progestin to reduce the risk of endometrial hyperplasia. Reassess the need and appropriateness of hormone therapy at 3 to 6-month intervals.[67040] In postmenopausal women with low bone mineral density, there is good evidence that standard-dose estrogen therapy reduces the risk for osteoporotic fractures, including hip, spine, and all non-spine fractures; however, estrogens are not generally recommended as a first-line prevention tactic due to the known risks of estrogen treatment (e.g., thromboembolism, cerebrovascular events) relative to other treatments. Women who need osteoporosis prophylaxis who are younger than 60 years or who are within 10 years of menopause onset may be given consideration for estrogen therapy, based on individual assessment of risk vs. benefit. Beyond the age of 60 years, other agents are preferred due to the known risks associated with hormonal therapy. Consider each woman's net balance of individual benefits and harms. If estrogen with or without a progestin is prescribed, use the lowest effective dose for the shortest duration that is consistent with an individual's treatment goals and risks. Estrogen therapy should not be used in patients with known osteoporosis; the risks outweigh the moderate benefit seen in postmenopausal women with established osteoporosis.[52408] [62806] [66837] [67122] [67125]
Initially, 1 patch (0.025 mg/day) applied transdermally applied twice weekly (every 3 to 4 days) as directed in product label. For women at significant risk of osteoporosis after careful consideration of non-estrogen medications. May adjust dose to therapeutic goals. Use the lowest effective dose. Continuous unopposed estrogen administration is acceptable in those without a uterus. For women with an intact uterus, consider a progestin to reduce the risk of endometrial hyperplasia. Alternatively, a cyclic schedule of 3 weeks of estradiol and 1 week off drug may be used. Reassess the need and appropriateness of hormone therapy at 3 to 6-month intervals.[51117] [58103] [57779] In postmenopausal women with low bone mineral density, there is good evidence that standard-dose estrogen therapy reduces the risk for osteoporotic fractures, including hip, spine, and all non-spine fractures; however, estrogens are not generally recommended as a first-line prevention tactic due to the known risks of estrogen treatment (e.g., thromboembolism, cerebrovascular events) relative to other treatments. Women who need osteoporosis prophylaxis who are younger than 60 years or who are within 10 years of menopause onset may be given consideration for estrogen therapy, based on individual assessment of risk vs. benefit. Beyond the age of 60 years, other agents are preferred due to the known risks associated with hormonal therapy. Consider each woman's net balance of individual benefits and harms. If estrogen with or without a progestin is prescribed, use the lowest effective dose for the shortest duration that is consistent with an individual's treatment goals and risks. Estrogen therapy should not be used in patients with known osteoporosis; the risks outweigh the moderate benefit seen in postmenopausal women with established osteoporosis.[52408] [62806] [66837] [67122] [67125]
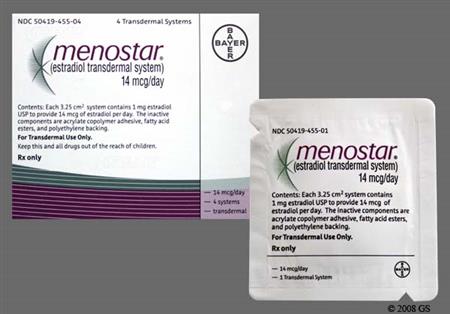
Initially, 1 patch (14 mcg/day or 0.025 mg/day, depending on brand chosen) applied transdermally once weekly (every 7 days) as directed in specific product label. Menostar is only indicated for osteoporosis prophylaxis and only comes in 14 mcg/day strength. For women at significant risk of osteoporosis after careful consideration of non-estrogen medications. May adjust dose to achieve therapeutic goals. Use the lowest effective dose. Continuous unopposed estrogen is acceptable in those without a uterus. Consider a progestin to reduce the risk of endometrial hyperplasia in women with an intact uterus. Reassess the need and appropriateness of hormone therapy periodically.[52451] [52448] In postmenopausal women with low bone mineral density, there is good evidence that standard-dose estrogen therapy reduces the risk for osteoporotic fractures, including hip, spine, and all non-spine fractures; however, estrogens are not generally recommended as a first-line prevention tactic due to the known risks of estrogen treatment (e.g., thromboembolism, cerebrovascular events) relative to other treatments. Women who need osteoporosis prophylaxis who are younger than 60 years or who are within 10 years of menopause onset may be given consideration for estrogen therapy, based on individual assessment of risk vs. benefit. Beyond the age of 60 years, other agents are preferred due to the known risks associated with hormonal therapy. Consider each woman's net balance of individual benefits and harms. If estrogen with or without a progestin is prescribed, use the lowest effective dose for the shortest duration that is consistent with an individual's treatment goals and risks. Estrogen therapy should not be used in patients with known osteoporosis; the risks outweigh the moderate benefit seen in postmenopausal women with established osteoporosis.[52408] [62806] [66837] [67122] [67125]
1 to 2 mg PO once daily, initially. Adjust dose as needed to control symptoms.[67040] Max: 4 mg/day. Continue treatment for reproductive life.[62669] [62670] [71106]
0.25 mg PO once daily, initially. Increase the dose gradually over 2 to 4 years to mimic the normal process of puberty. Max: 4 mg/day. Continue treatment for reproductive life.[62669] [62670] [71106]
37.5 to 50 mcg/24 hours transdermally twice weekly, initially. Adjust dose as needed to control symptoms.[51117] [57779] Max: 200 mcg/24 hours transdermally twice weekly. Continue treatment for reproductive life.[62669] [62670] [71106]
6.25 mcg/24 hours transdermally twice weekly, initially. Increase the dose gradually over 2 to 4 years to mimic the normal process of puberty. Max: 200 mcg/24 hours transdermally twice weekly. Continue treatment for reproductive life.[62669] [62670] [71106]
25 mcg/24 hours transdermally once weekly, initially. Adjust dose as needed to control symptoms.[52448] Max: 200 mcg/24 hours transdermally once weekly. Continue treatment for reproductive life.[62669] [62670] [71106]
6.25 to 7 mcg/24 hours transdermally once weekly, initially. Increase the dose gradually over 2 to 4 years to mimic the normal process of puberty. Max: 200 mcg/24 hours transdermally once weekly. Continue treatment for reproductive life.[62669] [62670] [71106]
1.5 to 2 mg IM once monthly.[61115] Continue treatment for reproductive life.[62669] [62670]
0.2 to 0.4 mg IM once monthly, initially. Increase dose gradually over 2 to 4 years to mimic the normal process of puberty. Max: 2.5 mg/dose. Continue treatment for reproductive life.[62669] [62670] [71106]
10 to 20 mg IM once monthly.[61114] Continue treatment for reproductive life.[62669] [62670]
1 to 2 mg PO 3 times daily.[67040] The effectiveness of therapy can be judged by specific prostate antigen (PSA) determinations as well as by symptomatic improvement of the patient.
30 mg IM administered every 1 to 2 weeks.[61114] Efficacy is evaluated according to patient clinical response and serial prostate specific antigen (PSA) levels. A response to estrogen treatment, if it will occur, will usually be noted within 3 months. Continued until a significant advancement of the disease occurs.
10 mg PO 3 times per day for at least 3 months.[67040]
1 to 8 mg/day PO. Usual dose: 2mg to 6mg/day. Divide dose into twice daily dosing if dose is greater than 2mg/day. Titrate dose every 6 months if needed. Dose increases should be based on individual response and monitored hormone levels.[63648] [70630] [70631] [70632] [70633]
5 mcg/kg/day PO for 6 months, may increase to 10 mcg/kg/day PO for 6 months, then 15 mcg/kg/day PO for 6 months, then 20 mcg/kg/day PO. In postpubertal adolescents, the dose may be increased more rapidly at 1 mg/day PO for 6 months, then 2 mg/day PO, then titrate as desired every 6 months. Dose increases should be based on individual response and monitored hormone levels.[63648] [70631]
25 to 400 mcg/24 hours transdermally. Usual dose: 50 to 200 mcg/24 hours. Frequency of transdermal patch change is product specific. Dose increases should be based on individual response and monitored hormone levels.[63648] [70631] [70633]
6.25 to 12.5 mcg/24 hours using patches twice weekly, initially (cut 25 mcg patch to desired strength). Titrate dose every 6 months by 12.5 mcg/24 hours to gradually increase to adult dose. Usual adult dose: 50 to 200 mcg/24 hours. Dose increases should be based on individual response and monitored hormone levels.[63648] [70631] [70632]
5 to 30 mg IM or subcutaneously every 2 weeks. Dose may be divided into weekly injections for cyclical symptoms. Dose increases should be based on individual response and monitored hormone levels.[63648] [70631] [70633]
5 to 20 mg IM every 2 weeks. May increase up to 30 to 40 mg IM every 2 weeks. Dose increases should be based on individual response and monitored hormone levels.[70632]
1 to 10 mg IM or subcutaneous every week. Dose increases should be based on individual response and monitored hormone levels.[63648] [70631] [70633]
2 to 10 mg IM or subcutaneous every week. Dose increases should be based on individual response and monitored hormone levels.[70632]
Monitoring in adults using estradiol for feminine-affirming therapy:
Monitoring in adolescents using estradiol for pubertal suppression:
Monitoring in adolescents using estradiol for feminine-affirming therapy that were previously hormone suppressed or in late pubertal individuals not previously suppressed:
Dependent on indication for therapy.
Dependent on indication for therapy.
Dependent on indication for therapy.
Not indicated in prepubescent females.
Estradiol is contraindicated in the presence of jaundice or known hepatic impairment or disease of any type.[67040]
Specific guidelines for dosage adjustments in renal impairment patients are not available; it appears that no dosage adjustments are needed.[67040]
† Off-label indication












































































Estradiol is the principal intracellular human estrogen and is substantially more active than its metabolites, estrone and estriol, at the cellular level. Estradiol can be obtained from natural sources or prepared synthetically. There is no evidence that 'natural' estrogens are more or less efficacious or safe than 'synthetic' estrogens.[50638] Due to almost complete first-pass metabolism, estradiol must be given in a micronized oral dosage form to ensure therapeutic effect. Esterification of estradiol to estradiol cypionate or valerate increases the parenteral duration of action of estradiol to allow for parenteral intramuscular administration. Estradiol is primarily used to prevent osteoporosis and relieve vasomotor and genitourinary symptoms associated with menopause (natural or surgical), for postmenopausal osteoporosis prevention, and is also used to treat female hypogonadism and other abnormalities of female gonadotropin dysfunction. Various estrogen products have been marketed in the U.S. since 1938. Estradiol is available in many dosage forms, including oral tablets, transdermal systems, topical emulsions, topical gels, topical sprays, vaginal creams, vaginal rings, and parenteral depot injections. Vaginal therapies are preferred in postmenopausal women with exclusive genitourinary symptoms, due to lower systemic absorption/exposure with most of these dosage forms.[50638] Many estradiol products have been FDA-approved since the 1990's, in accordance with the FDA's guidance to provide efficacious low-dose estrogen therapies in alternate drug delivery systems.
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Estradiol cypionate or Estradiol valerate
Topical gel, Divigel:
Topical gel, Elestrin:
Topical gel, EstroGel:
Topical skin emulsion, Estrasorb:
Topical spray, Evamist:
Vaginal cream (Estrace):
Wash and dry hands before handling. Screw the threaded end of the applicator with plunger onto the opened tube until secure. Squeeze from the bottom of the tube to expel the prescribed amount of cream into the applicator. Patients should be instructed to lie on their back with their knees drawn up, gently insert the applicator deeply into the vagina, and, once inserted, press the plunger downward to its original position. The applicator can be cleansed by removing the plunger from the barrel and washing with mild soap and water. Although not specifically recommended by the manufacturer, it may be prudent to advise patients to administer the vaginal cream just prior to bedtime in order to maximize absorption. Wash hands after use.[47276]
Vaginal system ring inserts (Estring vaginal system, Femring vaginal ring):
Wash and dry hands before handling. The ring system insert may be placed by the patient or a health care provider. The opposite sides of the insert should be pressed together and inserted into the vagina compressed. The ring insert is placed as deeply as possible in the upper third of the vagina and is worn continuously for 90 days. After 90 days, the ring should be removed and a new insert is applied. The insert may be removed by hooking a finger through the ring and pulling it out. The patient should not feel the ring, nor should it interfere with sexual intercourse. In addition, if the ring moves into the lower part of the vagina, the patient can push the ring back into place using a finger. Alternatively, within the 90-day dosage period, if the insert is removed or expelled, rinse it with lukewarm (not hot or boiling) water, and re-insert the ring as needed. Wash hands after use. Remove the old ring insert before inserting a new one.[49752][51110]
Vaginal tablet (Vagifem):
Wash and dry hands before handling. Use a new applicator containing an estradiol vaginal tablet each day, preferably at the same time each day; if the tablet has fallen out of the applicator, but is still contained in the packaging, carefully place it back into the applicator with clean dry hands. If the tablet has inadvertently fallen out of the applicator prior to insertion, the applicator should be thrown out and a new one containing a tablet used. Keep hands clean and dry while handling the tablet. Insert the applicator as far as comfortably possible into the vagina (without force), or until half of the applicator is inside the vagina, whichever is less. Then, gently press the plunger until the plunger is fully depressed. This will eject the tablet inside the vagina where it will dissolve slowly over several hours. After depressing the plunger, gently remove the applicator and dispose of it similarly to a plastic tampon applicator. Wash hands after use.[49751]
Vaginal insert (Imvexxy):
Wash and dry hands before handling the insert. Push the insert through the foil of the blister package. Hold the insert with the larger end between the fingers. The patient should select the best position for vaginal insertion that is most comfortable, either lying down or standing. With the smaller end up, place the insert about 2 inches into the vagina using the finger. Wash hands after use. The patient should write down the days of insertion. Wash hands after use.[63254]
A variety of endocrine and urogenital effects can occur during therapy with estradiol. Changes in sexuality include libido increase or libido decrease. Positive changes in libido may occur as a result of improvements in vulvar and vaginal atrophy in postmenopausal women. Vaginal changes such as discharge or irritation, vaginitis, cervicitis, or changes in cervical erosion (e.g., cervical ectropion) may appear. Vulvovaginal or vaginal candidiasis or other mycotic infections may occur infrequently with systemic or vaginal estrogen therapy. In a clinical trial of postmenopausal women to compare estradiol vaginal tablets to placebo, vulvovaginal mycotic infection occurred in 8% of estradiol-treated subjects vs. 3% with placebo.[49751] Estrogens may also cause enlargement of uterine leiomyomatas (fibroids), if present. A cystitis-like syndrome has also been reported. Changes in vaginal bleeding pattern and abnormal withdrawal bleeding or flow, breakthrough bleeding, spotting, and dysmenorrhea have been noted with estrogens and/or progestins and are commonly reported. In postmenopausal women, changes in uterine bleeding patterns will usually taper and stabilize within 3 to 6 months of beginning cyclic or continuous HRT combinations. Amenorrhea is desirable in many postmenopausal women and not considered to be an adverse effect of estrogen therapy. However, when estrogens are used for the treatment of hypogonadism in premenopausal females, continued amenorrhea may signal a lack of response to estrogen therapy. Unusual vaginal bleeding, menorrhagia, or spotting that persists beyond 6 months in any woman on estrogen therapy should be evaluated by a health care professional. For women who have a uterus, adequate diagnostic measures such as endometrial sampling, when indicated, should be undertaken to rule out malignancy in cases of undiagnosed persistent or recurring abnormal vaginal bleeding. Women who take estrogens should follow current recommendations for periodic pelvic examinations, including Papanicolaou smears, when indicated to detect cervical dysplasia.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Mastalgia (breast pain) is a common adverse effect of estrogens such as estradiol. Breast tenderness, breast enlargement, breast discharge, galactorrhea, and fibrocystic breast changes have been reported with estrogens and/or progestin therapy. Gynecomastia may occur in men on estrogen therapy. Individuals should report breast changes, lumps, or breast discharge to their care team. All women should receive yearly breast examinations by a care team and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on the individual's age, risk factors, and prior mammogram results.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Stomach/abdominal pain or cramps, bloating, nausea, and vomiting are common side effects of estrogens such as estradiol; these effects may attenuate with continued treatment. Diarrhea is infrequent with estradiol use. For example, in a clinical trial comparing estradiol vaginal tablet 10 mcg to placebo, diarrhea occurred in 5% of treated postmenopausal women vs. 0% of those receiving placebo.[49751] Consider benign hepatic adenoma if gastrointestinal symptoms such as abdominal pain/tenderness, abdominal mass, or hypovolemic shock are present, as an adenoma may rupture and cause intraabdominal hemorrhage. Benign hepatic adenomas appear to be associated with the use of oral contraceptives, and enlargement of hepatic hemangiomas has been reported with estrogen and/or progestin therapies. Pancreatitis and colitis have also been reported; high dose estrogens have been associated with ischemic colitis (bowel ischemia) with mesenteric vein thrombus secondary to hypercoagulability, a reported potential mechanism.[57614] In subjects with preexisting hypertriglyceridemia, estrogen therapy may be associated with elevations of plasma triglycerides leading to pancreatitis and other complications. Additionally, GI obstruction of the bowel has been reported in subjects using the estradiol vaginal ring.[51110] Estrogens enhance hepatic lipoprotein uptake and inhibit bile acid synthesis, resulting in increased concentration of cholesterol in the bile, which can lead to cholelithiasis, biliary obstruction, and cholestasis. Cholestatic jaundice and an increased incidence of gallbladder disease have also been reported. A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery (e.g., cholecystitis) in postmenopausal women receiving estrogens has been reported. Estrogens may be poorly metabolized in individuals with impaired liver function. For individuals with a history of cholestatic jaundice associated with past estrogen use or with pregnancy, use estradiol cautiously. If cholestatic jaundice recurs, discontinue the estrogen.[47276] [67040] Rare adverse reactions include hepatitis (and elevated hepatic enzymes). Estrogens may induce peliosis hepatis, a very rare consequence of taking estrogens and combined oral contraceptives that is characterized by the presence of blood-filled spaces.[51257] Persistent or severe abdominal symptoms should be evaluated by their care team.[47276] [51110] [67040]
Deep and superficial venous thrombosis, pulmonary embolism, thrombophlebitis, myocardial infarction, and stroke have been reported with estrogens and/or progestin therapy. The use of estrogens in postmenopausal women, with or without a progestin, carries a risk for thromboembolism, and cardiovascular events such as myocardial infarction (MI) or stroke. Detailed information regarding what is known about thromboembolic and cardiovascular risk in postmenopausal women is available in the boxed warnings and precautions section of the product labeling for the products, as these risks must be considered prior to use of HRT in women, and with consideration to age and other risk factors for these events. Risks vary with the use of estrogen-alone vs. use of estrogen with progestin therapy. Should any of these events occur or be suspected, discontinue the estrogen or estrogen-progestin therapy immediately.[32946] [46639] [47276] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogens such as estradiol can cause sodium and fluid retention, resulting in peripheral edema or mild weight gain. They should be prescribed cautiously to patients in whom the presence of edema would be detrimental. In addition, estrogens can slightly increase blood pressure, occasionally causing hypertension; data indicate in most patients the change is not clinically significant. In a few case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogens such as estradiol. In a large, randomized, placebo-controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. It is recommended to monitor blood pressure periodically in women taking estrogen therapy.[47276] [67040] [32946] [46639] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] In the PEPI trial, postmenopausal women 45 to 65 years of age randomized to any hormone replacement therapy regimen experienced increases in both systolic and diastolic blood pressure of 3% to 5% after the first year of treatment, but the increases were not statistically different from placebo.[24010]
Headache, with no other symptoms, has been noted with use of estrogens such as estradiol, including with vaginal therapy. For example, headache (5% to 7%) was the most common side effect noted with use of an estradiol vaginal insert for dyspareunia. Headache with no other symptoms occurred at an average incidence range of 5% to 21% with various systemic and transdermal estradiol treatments in postmenopausal women. A severe headache or migraine with focal neurologic changes may be a warning sign of a serious adverse event such as a stroke or retinal problems (e.g., thrombosis) in the eye. Discontinue the estrogen pending examination if there is sudden partial or complete loss of vision or new, severe, sudden onset of headache or migraine with focal neurologic changes. If examination reveals a serious event, estrogens should be permanently discontinued.[47276] [67040] [32946] [46639] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] The relationship of headache, specifically migraine headache, and the administration of estrogens is not clearly defined. A number of changes can occur when a woman initiates HRT and include 1) migraines can appear for the first time, 2) a change in frequency, severity and duration of migraine headaches may be seen, or 3) an improvement or decrease in the occurrence of migraine headaches. When initiating estrogen therapy, an individual's headache pattern should be observed and, if migraines worsen, consider discontinuing therapy.
Mental depression, nervousness or anxiety, mood disturbances such as emotional lability and irritability have been reported with estrogens such as estradiol, with or without progestin therapy.[47276] [67040] Complaints of insomnia or fatigue may be associated with the underlying menopausal complaints or may be associated with treatment. Women with a history of depression may need special monitoring. If significant depression occurs, consider discontinuation of hormonal therapy.
A variety of dermatologic or allergic reactions have been reported with use of estrogens, such as estradiol. Melasma, in the form of tan or brown patches, may develop on the forehead, cheeks, temples and upper lip; melasma may persist after the drug is discontinued. In some cases, estrogens may induce or aggravate an existing acne vulgaris. Erythema multiforme, erythema nodosum, hemorrhagic eruption, loss of scalp hair (alopecia), hirsutism, pruritus, maculopapular rash, urticaria, angioedema, and anaphylactoid reactions have been reported with estrogens and/or progestins.[47276] [67040] Estradiol transdermal systems may cause localized bleeding, hematoma (bruising), burning, skin irritation, xerosis, eczema, edema, erythema, inflammation, pain, vesicular rash, or rash. Other dermal reactions reported postmarketing with estradiol transdermal systems include, paresthesias, skin discoloration or pigmentation changes, and swelling.[57779] To help reduce the chance of skin redness or skin irritation, wait at least 1 week before the individual reuses a skin site for transdermal patch application.[51117] Estradiol topical emulsions and sprays have also been associated with pruritus or skin irritation during clinical trials.[30467] [46639] During postmarketing surveillance, estradiol spray (Evamist) has been associated with nipple and areola skin discoloration, usually occurring on the same side as the inner arm where the product was applied; xerosis has also been reported.[46639] Vaginal therapy with estradiol may cause localized itching or irritation; in one clinical trial during use of 10 mcg vaginal tablets, vulvovaginal pruritus occurred in 8% of treated subjects compared to 2% of those receiving placebo.[49751]
Some women taking estrogens, including estradiol, notice tenderness, swelling, or minor bleeding of their gums, which may lead to gingivitis. Proper attention to oral care and regular dental visits are recommended.
Retinal thrombosis has been reported in individuals receiving estrogens such as estradiol. Discontinue the estrogen pending examination if there is sudden visual impairment either partial or complete or a sudden onset of proptosis, diplopia, or migraine/headache symptoms with focal neurologic changes. If examination reveals papilledema, visual loss, or retinal vascular lesions, permanently discontinue estrogen therapy.[32946] [46639] [47276] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] Exogenous estrogen use can cause an increased curvature of the cornea, caused by thinning of the stroma. Individuals with contact lenses may develop intolerance to their lenses and should have their ophthalmologist evaluate any changes.
Reduced carbohydrate tolerance and potentially hyperglycemia has been reported with estrogens and/or progestin therapy. Cautious use of estrogens such as estradiol in individuals with diabetes is advised, as estrogens may cause an exacerbation of diabetes mellitus. Limited clinical studies of estrogen regimens have not noted significant alterations in glucose metabolism in healthy postmenopausal women. In women without diabetes, estrogens appear to have little to no effect on fasting blood glucose.[50831] [32946] [46639] [47276] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Leg muscle cramps, arthralgia, and hypocalcemia have been reported with estrogen and/or progestin therapy. Back pain has been reported within an overall incidence range of 3.3% to 11% with various estradiol formulations, including oral, transdermal, topical and vaginal products.[47276] [67040] [32946] [46639] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254]
Hormone replacement therapy (HRT), both estrogen/progestin combination therapy and estrogen alone therapy, fails to prevent mild impaired cognition (memory loss) and is positively associated with the risk of developing dementia in women 65 years and older; do not use HRT to prevent or treat dementia or preserve cognition (memory).[32946] [46639] [47276] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] When data from the 2 populations in the Women's Health Initiative Memory Study (WHIMS) estrogen-alone and estrogen plus progestin ancillary studies were pooled as planned in the WHIMS protocol, the reported overall relative risk for probable dementia was 1.76 (95% CI 1.19 to 2.60, p = 0.005). Since both ancillary studies were conducted in women 65 to 79 years, it is unknown whether these findings apply to younger postmenopausal women.[27451] [32126] [50638] In the WHIMS estrogen plus progestin ancillary study, a population of 4,532 postmenopausal women 65 to 79 years was randomized to daily estrogen plus progestin or placebo. After an average follow-up of 4 years, 40 women in the estrogen plus progestin group and 21 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for estrogen plus progestin vs. placebo was 2.05 (95% CI, 1.21 to 3.48). The absolute risk of probable dementia for estrogen plus progestin vs. placebo was 45 vs. 22 cases per 10,000 women-years.[27451] In the WHIMS estrogen-alone ancillary study of WHI, a population of 2,947 hysterectomized women 65 to 79 years was randomized to daily estrogen-alone or placebo. After an average follow-up of 5.2 years, 28 women in the estrogen-alone group and 19 women in the placebo group were diagnosed with probable dementia. The relative risk of probable dementia for estrogen-alone vs. placebo was 1.49 (95% CI, 0.83 to 2.66). The absolute risk of probable dementia for estrogen-alone vs. placebo was 37 vs. 25 cases per 10,000 women-years.[32126]
In women with a history of cardiovascular disease, the use of estrogen and progestin combination therapy increases the risk of developing urinary incontinence. Subjects in the Heart and Estrogen/progestin Replacement Study (HERS) study who did not have urinary incontinence prior to the studies initiation were observed to determine if hormone replacement therapy (HRT) was helpful in preventing urinary incontinence. The study found that women who received estrogen/progestin therapy were almost twice as likely as subjects receiving placebo to develop urge incontinence and 3 times as likely to develop stress incontinence after 1 year of treatment. At 4 years, the effect of HRT became even more pronounced, increasing the risk to 3.23 for urge incontinence and to 4.81 for stress incontinence. The applicability of these findings to women who use estrogen alone with estradiol is unclear.[27457]
Estradiol vaginal ring inserts do not dissolve and remain inserted into the vaginal for prolonged periods. Toxic shock syndrome (TSS) has been reported in women using vaginal rings containing estradiol. TSS is a rare but life-threatening complication of bacterial infection; often it results from toxins produced by Staphylococcus aureus bacteria but may also be caused by toxins from group A streptococcus. Examples of signs/symptoms of TSS include fever, nausea, vomiting, diarrhea, muscle pain, dizziness, fainting, or a sunburn-rash on the face and body. Individuals experiencing any of these effects should be instructed to contact their prescriber immediately.[49752] [51110]
Vaginal estradiol products may cause localized vaginal pruritus/itching or rarely, vaginal irritation. In a clinical trial comparing estradiol vaginal tablet inserts 10 mcg to placebo, vulvovaginal pruritus occurred in 8% of treated patients vs. 2% of patients receiving placebo.[49751] Vaginal ring inserts with estradiol do not dissolve, and remain inserted for prolonged treatment durations. Sometimes, these insertions lead to complications with the ring device. A few cases of inadvertent ring insertion into the urinary bladder or adherence to the bladder wall, which may require surgical removal, have been reported for women using vaginal ring inserts. Adherence of the vaginal rings to the vaginal wall, making removal of the ring difficult, has been reported; some cases have required surgical removal. Vaginal or bladder wall ulceration or erosion may occur with use of the vaginal rings. Symptoms of vaginal erosion and vaginal ulceration have included vaginal pain or irritation, erythema, abrasion, and/or spotting. Vaginal pain upon removal or difficulty removing the vaginal ring should be evaluated by a medical professional. If erosion or ulceration occur, consider temporarily discontinuing the vaginal ring until healing is complete.[51110] [49752] During postmarketing surveillance with estradiol vaginal inserts (Imvexxy), vaginal discharge was reported.[63254] Carefully evaluate unusual vaginal discharge, vaginal pain, or persistent unexplained urinary symptoms such as bladder discomfort in patients using vaginal estradiol products.
Numerous epidemiologic studies have examined the effects of estrogen hormone replacement therapy (HRT) on the development of new primary malignancy (e.g., breast cancer, endometrial cancer, ovarian cancer) in postmenopausal women. Detailed clinical study information regarding what is known about cancer risk in postmenopausal women is available in the boxed warnings and precautions section of the product labeling for the products, as these risks must be considered prior to use of HRT, and with consideration to age and other risk factors for these events.[50638] [71260] ENDOMETRIAL HYPERPLASIA and ENDOMETRIAL CANCER: There is an association of unopposed estrogen therapy and endometrial hyperplasia in women with an intact uterus. The incidence of endometrial hyperplasia due to estrogen-alone HRT is estimated at 10% or less. Adding a progestin to estrogen therapy has been shown to reduce, but not eliminate, the risk of endometrial hyperplasia, lowering the incidence to about 1% or less. Clinical surveillance of all women using estrogen-alone or estrogen plus progestin therapy is important. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal uterine bleeding. The reported endometrial cancer risk among unopposed estrogen users is about 2- to 12-times greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than 1 year. The greatest risk appears associated with prolonged use, with increased risks of 15-to 24-fold for 5 to 10 years or more, and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. BREAST CANCER: The data available are derived from studies of estrogen-alone or estrogen plus progestin hormonal replacement therapy (HRT). Since the 1970s, numerous epidemiological studies have examined the association of exogenous estrogen and breast cancer (new primary malignancy). The most important randomized clinical study providing information about breast cancer in estrogen-alone users is the Women's Health Initiative (WHI) substudy of daily conjugated estrogens (0.625 mg)-alone. In the WHI estrogen-alone substudy, after an average follow-up of 7.1 years, conjugated estrogen (0.625 mg/day)-alone was not associated with an increased risk of invasive breast cancer (relative risk [RR] 0.80). The use of estrogen-alone has been reported to result in an increase in abnormal mammograms requiring further evaluation. The Women's Health Initiative (WHI) estrogen plus progestin study reported increased risks of invasive breast cancer in patients taking combined estrogen-progestin HRT vs. placebo. The potential risk of breast cancer may increase with longer duration of use. All persons should receive yearly breast examinations by a health care provider and perform monthly breast self-examinations. In addition, mammography examinations should be scheduled based on patient age, risk factors, and prior mammogram results. OVARIAN CANCER: Women who used HRT for menopausal symptoms also had an increased risk for ovarian cancer, but data are still uncertain if risk is associated with a specific duration of use. What is known about the risk of ovarian cancer due to hormonal therapy is derived from data available for estrogen-alone and estrogen plus progestin products; studies are not available for estrogen plus selective estrogen receptor modifier combinations. The Women's Health Initiative (WHI) estrogen plus progestin substudy reported a statistically non-significant increased risk of ovarian cancer. After an average follow-up of 5.6 years, the relative risk for ovarian cancer for estrogen plus progestin versus placebo was 1.58 (95% CI 0.77 to 3.24). The absolute risk for estrogen plus progestin versus placebo was 4 versus 3 cases per 10,000 women-years. A meta-analysis of 17 prospective and 35 retrospective epidemiology studies found that women who used HRT for menopausal symptoms had an increased risk for ovarian cancer. The primary analysis, using case-control comparisons, included 12,110 cancer cases from the 17 prospective studies. The relative risk associated with current use of hormonal therapy was 1.41 (95% confidence interval [CI] 1.32 to 1.5); there was no difference in the risk estimates by duration of the exposure (less than 5 years [median of 3 years] vs. greater than 5 years [median of 10 years] of use before the cancer diagnosis). The relative risk associated with combined current and recent use (discontinued use within 5 years before cancer diagnosis) was 1.37 (95% CI 1.27 to 1.48), and the elevated risk was significant for both estrogen-alone and estrogen plus progestin products. The exact duration of hormone therapy use associated with an increased risk of ovarian cancer, however, is unknown.[32946] [46639] [47276] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] [50638] [71260]
Estrogen administration such as estradiol may lead to severe hypercalcemia in individuals with breast cancer and bone metastases. If hypercalcemia occurs, discontinue estradiol and take appropriate measures to reduce the serum calcium concentration.[47276] [67040]
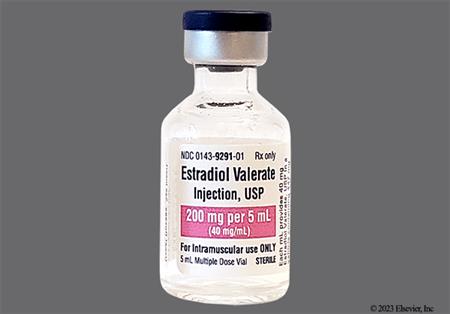
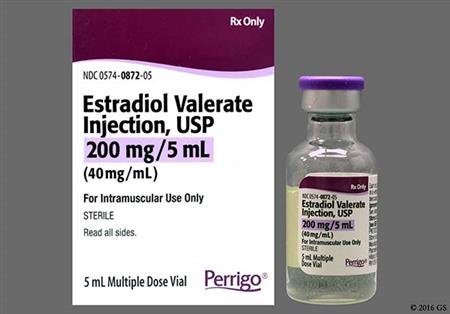
Estradiol cypionate or estradiol valerate injections may cause an injection site reaction, which may include erythema and mild pain and rarely may cause sterile abscess. Never inject these injections intravenously, they are for intramuscular use only. These injections are formulated in oil, and inadvertent intravenous administration may result in pulmonary oil microembolism and serious morbidity.[61114] [61115]
Estradiol is contraindicated for use during known or suspected pregnancy. However, little or no increased risk of birth defects appears to exist in children born to women who have used estrogens and progestins from oral contraceptives inadvertently during early pregnancy. Any estrogen therapy should be discontinued when pregnancy is suspected or confirmed.[47276] [67040] Estrogens are known to cause teratogenesis in animals with continued use during pregnancy. Increased risk of a wide variety of fetal abnormalities, including modified development of sexual organs, cardiovascular anomalies and limb defects, have been reported. For example, diethylstilbestrol (DES) is well known for creating disturbances in the reproductive systems of both male and female offspring in animals and humans during pregnancy.[24356]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Systemic absorption may occur with the use of vaginal estradiol products. Thus, the warnings, precautions, and adverse reactions associated with systemic estrogen treatment should be taken into account.[47276]
Exogenous estrogens may exacerbate symptoms of angioedema in individuals with hereditary angioedema. Consider whether the benefits of estrogen therapy outweigh the risks in such individuals.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogen-based hormone replacement therapy (HRT) products, such as estradiol, are contraindicated in people with undiagnosed abnormal uterine bleeding or a history of or known/suspected breast cancer, endometrial cancer, or other estrogen-dependent tumor, which may be hormonally-sensitive. There is an increased risk of endometrial cancer in a person with a uterus who uses unopposed estrogens. Adding a progestin to estrogen HRT has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding. The use of estrogen-alone or estrogen plus progestin HRT has been reported to result in an increase in abnormal mammograms, requiring further evaluation and observational studies. During the Womens Health Initiative(WHI), estrogen-alone was not associated with an increased risk of invasive breast cancer, but an estrogen plus progestin substudy reported increased risks of invasive breast cancer. Consistent with the WHI clinical trials, observational studies have also reported an increased risk of breast cancer for estrogen plus progestin therapy, and a smaller increased risk for estrogen-alone therapy, after several years of use. All people taking estrogen, whether with or without a progestin, should receive an annual clinical breast examination, perform monthly self-examinations, and have regular mammograms as recommended by their health care professional based on patient age, risk factors, and prior mammogram results. While estrogen therapy is rarely used for the palliative treatment of advanced breast cancer, estrogen HRT use may lead to severe hypercalcemia in patients with breast cancer and bone metastases. If hypercalcemia occurs, use of HRT should be stopped and appropriate measures taken to reduce the serum calcium level.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] [71260]
Because estrogens influence the growth of endometrial tissues, use estradiol products cautiously in people with endometriosis or uterine leiomyoma (uterine fibroids). A few cases of malignant transformation of residual endometrial growth have been reported in women treated post-hysterectomy with estrogen-alone therapy. For individuals known to have residual endometriosis post-hysterectomy, the addition of a progestin should be considered to reduce the risk of endometrial tissue growth.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] [69730] [72653]
Estrogens, with or without progestins, should not be used for the prevention of cardiovascular disease. Increased risks of stroke and DVT are reported with estrogen-alone hormone replacement therapy (HRT). An increased risk of thromboembolic and serious cardiovascular events [e.g. pulmonary embolism (PE), deep vein thrombosis (DVT), stroke, and myocardial infarction (MI)] are reported with estrogen plus progestin hormone replacement therapy (HRT). The use of high-dose estrogens for the palliative treatment of cancer of the prostate or breast has also been shown to increase risks for nonfatal MI, PE, and thrombophlebitis. Immediately discontinue the HRT regimen if any of these events occur or are suspected. Due to the potential for serious cardiovascular events, estrogen-containing HRT is contraindicated in people with active thromboembolism (e.g., DVT or PE) or a history of these conditions, or in those with active arterial thromboembolic disease (e.g., stroke and myocardial infarction) or a history of these conditions. HRT regimens are also contraindicated in people with known thrombophilia (e.g., protein C, protein S, or antithrombin deficiency). Individuals with certain risk factors for arterial vascular disease (e.g., cardiovascular disease, hypertension, diabetes, tobacco smoking, hypercholesterolemia, and morbid obesity) and/or venous thromboembolism (VTE) (e.g., personal history or family history of VTE, obesity, or systemic lupus erythematosus) should be monitored and managed appropriately during HRT use.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] Monitor blood pressure in all postmenopausal individuals receiving HRT and especially in those with pre-existing hypertension; in a few case reports, substantial increases in blood pressure have been attributed to idiosyncratic reactions to estrogen HRT therapy. In a large, randomized, placebo controlled clinical trial, a generalized effect of estrogens on blood pressure was not seen. Estrogens may cause some degree of fluid retention, and people with conditions that may be aggravated, such as cardiac dysfunction, warrant careful observation when estrogens are prescribed.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] [50638]
If feasible, estrogen-based hormone replacement therapy (HRT) should be discontinued at least 4 to 6 weeks before major surgery or a planned procedure associated with an increased risk of thromboembolism, or during periods of prolonged immobility. Resume the HRT regimen only after the patient is fully ambulatory. In addition, people treated with HRT should be advised to move about periodically during travel involving prolonged immobilization, such as during long-duration plane travel.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogen-based hormone replacement therapy (HRT) is contraindicated in people with hepatic failure, impairment or disease. Estrogens and/or progestins may be poorly metabolized in those with impaired liver function. For people with a history of intrahepatic cholestasis of pregnancy or a history of significant adverse event(s) associated with previous use of an estrogen, such as cholestatic jaundice, use estrogens with caution. If there is a recurrence of cholestatic jaundice, discontinue the HRT regimen. Estrogen HRT may cause an exacerbation of porphyria or hepatic hemangioma (benign liver tumor). Consider whether the benefits of estrogen HRT outweigh the risks in people with such conditions.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] Liver disease guidelines recommend that menopausal estrogen-based HRT not be used in people with the following conditions: decompensated liver function, Budd-Chiari syndrome, or hepatocellular adenoma (benign liver tumor).[72725]
Use estrogen-based hormone replacement therapy (HRT) with caution in people with pre-existing gallbladder disease. A 2- to 4-fold increase in the risk of gallbladder disease requiring surgery in postmenopausal individuals receiving estrogens has been reported.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] [71260]
In people with pre-existing hypertriglyceridemia, estrogen-based hormone replacement therapy (HRT) may be associated with elevations of plasma triglycerides leading to pancreatitis. Discontinue the HRT regimen if pancreatitis occurs.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Individuals with systemic lupus erythematosus (SLE) may have an increased risk for thromboembolism and should be managed appropriately when estrogen hormone replacement therapy (HRT) is used. Estrogen HRT may cause an exacerbation of SLE and should be used with caution in people with this condition.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogen-based hormone replacement therapy (HRT) may cause an exacerbation of migraine and should be used cautiously in people with this condition. Discontinue the HRT regimen pending examination if there is a migraine with focal neurologic or visual changes.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Individuals with diabetes mellitus may have an increased risk for thromboembolism and should be managed appropriately when estrogen-based hormone replacement therapy (HRT) is used. Estrogen HRT may cause an exacerbation of diabetes. Consider whether the benefits of estrogen therapy outweigh the risks in people with this condition.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogen administration leads to increased thyroid-binding globulin (TBG) levels. People with hypothyroidism dependent on thyroid hormone replacement therapy who are also receiving estrogens may require increased doses of their thyroid replacement therapy. Monitor thyroid function in these individuals to ensure maintenance of their free thyroid hormone levels in an acceptable range. People with normal thyroid function can compensate for the increased TBG by making more thyroid hormone, thus maintaining free T and T serum concentrations in the normal range.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogen therapy should be used with caution in people with hypoparathyroidism as estrogen-induced hypocalcemia may occur.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estrogens may cause exacerbation of asthma or epilepsy (seizure disorder) and should be used with caution in people with these conditions.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Estradiol is contraindicated for use during pregnancy. There appears to be little or no increased risk of birth defects in children born to individuals who used estrogens and progestins from oral contraceptives inadvertently during early pregnancy. In any patient in whom pregnancy is suspected, pregnancy should be ruled out before continuing estrogen use.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] In selected instances estradiol has been used off-label as an adjuvant to clomiphene treatment of infertility, or in donor oocyte program procedures in assisted reproduction technology (ART) under the direction of ART specialists; however, treatment is discontinued when pregnancy ensues.[63265]
Use estradiol with caution during breast-feeding. Estrogens are present in human milk and can reduce milk production. This reduction can occur at any time but is less likely to occur once breast-feeding is well-established.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [48204] [63254] [67040] Estrogens are not approved for the treatment of postpartum breast engorgement.[67040]
Estrogens may cause fluid retention. Conditions that might be affected by fluid retention, such as renal impairment or renal failure, require careful observation when estrogens are prescribed.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040]
Administration of hormone replacement therapy (HRT) for menopause should generally be avoided in geriatric adults 65 years of age and older, and HRT should not be used to prevent or treat dementia or preserve cognition (memory). Both estrogen-progestin combination hormone replacement therapy (HRT) and estrogen-alone therapy fail to prevent mild cognitive impairment (memory loss) and increase the risk of dementia in females 65 years of age and older.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] Overall risk vs. benefit should be considered along with the goals of use of HRT for the individual patient when considering whether to continue HRT if they are over 65 years of age.[50638] [27451] [32126] [71260] The Beers Criteria consider oral, topical patch, or other systemic forms of estrogens (with or without progestins) as potentially inappropriate medications for use in geriatric adults. Avoid use due to evidence of carcinogenic potential (i.e., breast and endometrium) and the lack of cardiovascular or cognitive protective effects. Avoid oral or transdermal estrogen in geriatric adult women with any type of urinary incontinence due to lack of efficacy for this condition. The use of vaginal estrogens is acceptable for the management of dyspareunia and vaginal/vulvar symptoms.[63923]
The primary source of estrogens in premenopausal women is the ovary, which normally secretes 0.07 to 0.5 mg of estradiol daily, depending on the phase of the menstrual cycle. Once estrogens enter the cells of responsive tissues (e.g., female organs, breasts, hypothalamus, pituitary), they increase the rate of synthesis of DNA, RNA, and some proteins. The secretion of gonadotropin-releasing hormone by the hypothalamus is reduced during estrogen administration, causing reduction in follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary. Exogenous estrogens elicit all of the actions of endogenous estrogens. Estrogens are responsible for the growth and development of female sex organs and the maintenance of sex characteristics including growth of axillary and pubic hair and shaping of body contours and skeleton. At the cellular level, estrogens increase cervical secretions, cause proliferation of the endometrium, and increase uterine tone. Paradoxically, prolonged administration of estrogen can shrink the endometrium. During the preovulatory or nonovulatory phase of the menstrual cycle, withdrawal of estrogen can initiate menstruation; in the ovulatory phase, the decrease in progesterone secretion is the more significant factor causing menstruation. In post-menopausal use, amenorrhea occurs in most women within several months of oral estrogen use.
Estrogens have a weak anabolic effect and also can affect bone calcium deposition and accelerate epiphysial closure. Estrogens appear to prevent osteoporosis associated with the onset of menopause. Estrogens generally have a favorable effect on blood lipids, reducing LDL- and increasing HDL-cholesterol concentrations on average, by 15%. Serum triglycerides increase with estrogen administration. Estrogens increase the rate of synthesis of many proteins, including thyroid binding globulin and several clotting factors. Estrogens reduce levels of antithrombin III, and increase platelet aggregation. Estrogens also enhance sodium and fluid retention.
Unopposed estrogen has been associated with increased risk of endometrial cancer in menopausal women with an intact uterus; concomitant progestin therapy reduces, but does not eliminate, this risk. However, combination hormone replacement therapy (HRT) may add additional health risks for some women, as evidenced by the HERS trials [25473][27270][27271], the Women's Health Initiative study [27272], and other investigations. In particular, the Women's Health Initiative (WHI) study reported an increased risk of myocardial infarction, stroke, dementia, invasive breast cancer, and venous thromboembolism in patients taking combination HRT and an increased risk of stroke, dementia, and venous thromboembolism in patients taking estrogen only HRT; an increased risk of invasive breast cancer was not evident in women taking estrogen only. Because of these findings, patients should be prescribed estrogen HRT or estrogen-progestin HRT for the shortest duration consistent with the treatment goals. Estrogen HRT with or without a progestin is not indicated and should not be used to prevent coronary artery disease or other cardiovascular disease. The risks and benefits of HRT must be determined for a woman individually.
In men with advanced prostate cancer, estrogens exert their effect by inhibition of the hypothalamic-pituitary axis through negative feedback. This results in decreased secretion of luteinizing hormone (LH). Decreased testosterone production from the Leydig cells in the testes occurs, which may decrease tumor growth and lower prostate specific antigen (PSA) levels. Improvement in bone metastasis may also occur. In the past, high-dose estrogen therapy was also used in selected men and postmenopausal women with inoperable, progressive breast cancer. Since the development of selective estrogen receptor modifiers (SERMs), high-dose estrogen therapy for the palliative treatment of breast cancer is rarely used today.
Revision Date: 10/08/2025, 09:46:30 AMEstradiol products are administered orally, intramuscularly, vaginally, transdermally, and topically. The pharmacokinetics of estradiol differ with the formulation used for delivery and the route of administration. Following systemic absorption, estradiol is rapidly transformed by the liver to estrone and estriol, the major circulating forms in the serum, by 17-beta-hydroxysteroid dehydrogenase. The estrogens are widely distributed and are strongly protein-bound, primarily to albumin and sex hormone-binding globulin (SHBG). Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens are metabolized partially by CYP3A4 in the liver. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens. Estradiol, estrone, and estriol undergo glucuronide and sulfate conjugation to a variety of minor metabolites which are excreted primarily in the urine.[67040]
Generally, a serum estrogen concentration is not a predictor of an individual woman's therapeutic response to estradiol nor her risk for adverse outcomes. Likewise, exposure comparisons across different estrogen products to infer efficacy or safety for the individual woman may not be valid.[52451]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: CYP3A4
In vitro and in vivo studies indicate that estrogens are partially metabolized by CYP3A4. Interactions with drugs that are inhibitors or inducers of CYP3A4 are possible.[67040]
Estradiol is extensively metabolized in the gastrointestinal mucosa during oral absorption and in the liver. Micronization of oral estradiol tablets slows oral absorption and decreases the first-pass metabolizm in the liver and increases the normally poor oral bioavailability of estradiol. Absolute bioavailability of oral micronized estradiol is roughly 5% to 10% of an administered dose. The plasma half-life of orally administered estradiol is approximately 1 to 2 hours at steady state; but other circulating estrogens persist longer.[67040]
Estradiol cypionate and Estradiol valerate: These forms of estradiol are given as a depot injection in oil, which slows absorption after intramuscular (IM) injection. Esterification of estradiol to estradiol cypionate or valerate significantly increases the parenteral duration of action compared to aqueous estradiol formulations. Intramuscular administration of the cypionate esters of estradiol have more prolonged actions (average, 3 to 6 weeks) than the valerate esters (average, 2 to 3 weeks), respectively. However, IM dosage intervals are usually every 4 weeks for both cypionate and valerate esters of estradiol for most indications; dosage and dosage intervals are adjusted to patient response.[61115][61114]
Topical emulsions, gels, or sprays: Topical administration of estradiol avoids first-pass metabolism and allows for continuous delivery of the hormone. The formulas are designed to help deliver systemic estradiol levels through the skin. Estradiol is minimally metabolized in the skin, thus higher therapeutic estradiol serum levels are present, and more closely approximate natural premenopausal concentrations. Different formulations are not interchangeable and differ in amount of estradiol delivered systemically per day and other pharmacokinetic absorption parameters. Estradiol topical emulsion (Estrasorb), for example, utilizes micellar nanoparticle technology. Once in the serum, the distribution, metabolism and excretion of topically administered estradiol occurs through the same pathways as for oral administration.[32946][46639][56912][62077]
Transdermal patches: Transdermal systems are designed to help deliver systemic levels of estradiol through the skin. Transdermal administration of estradiol avoids first-pass metabolism and allows for continuous delivery of the hormone. Estradiol is minimally metabolized in the skin, thus higher therapeutic estradiol serum levels are present, and more closely approximate natural premenopausal concentrations. Transdermal systems differ in the amount of estradiol delivered per day, dosage interval of application, and other absorption pharmacokinetic parameters. Minimal fluctuations in estradiol concentrations are seen with transdermal application. Once in the serum, the distribution, metabolism and excretion of transdermally administered estradiol occurs through the same pathways as for oral administration. Transdermal estradiol has a short elimination half-life (approximately 2 hours); serum estradiol concentrations generally return to postmenopausal levels within 4 to 8 hours of patch removal.[51117][52448][52451][57779][58103]
Vaginal Route
In general, estradiol is well absorbed through the vaginal mucous membranes. The vaginal dosage applied determines systemic hormone exposure; as a result, systemic as well as local tissue effects may occur. However, the systemic effects differ with specific vaginal products and many products are not acceptable for treating systemic or vasomotor symptoms or preventing osteoporosis.
Vaginal Cream: Specific pharmacokinetic data are not available; this dosage form is only acceptable to treat genitourinary symptoms.[47276]
Vaginal Ring Inserts: Drug delivery from vaginal ring dosage forms is rapid; the time to maximum concentrations (Tmax) is usually less than 1 hour following insertion. Serum estradiol concentrations peak, then decrease rapidly such that by 24 to 48 hours following insertion of the dosage form, serum estradiol concentrations are relatively constant through the end of the 3-month dosing interval. Different vaginal ring devices are not interchangeable due to differences in dosage and efficacy in symptom control. For example, Estring dosages are not effective for addressing vasomotor symptoms; low dose systemic delivery of estradiol from Estring (estradiol) results in mean steady-state serum estradiol estimates of 7 to 8.1 pg/mL; with an estradiol delivery rate of roughly 7.5 mcg/24 hours. Following administration of Femring (estradiol acetate) 0.05 mg/day, the average serum estradiol concentration is 40.6 pg/mL; the corresponding apparent in vivo estradiol delivery rate is 0.052 mg/day. Following administration of Femring 0.10 mg/day, the average serum estradiol concentration is 76 pg/mL; the apparent in vivo delivery rate is 0.097 mg/day. Consistent with the avoidance of first-pass metabolism achieved by vaginal estradiol administration, serum estradiol concentrations are slightly higher than estrone concentrations. Once absorbed systemically, the distribution, metabolism and excretion of estradiol delivered via vaginal application occurs via the same pathways as for oral administration.[49752][51110]
Vaginal Tablets (e.g., Yuvefem, Vagifem): In an open-label, multiple-dose, parallel group study conducted in 58 patients, a mean estradiol (E2) average concentration at Day 83 of 5.5 pg/mL was measured after a regimen of 10 mcg vaginally daily for 2 weeks followed by a twice-weekly maintenance regimen for the remaining 10 weeks. When patients received a dose of 25 mcg daily for 2 weeks followed by a twice-weekly maintenance regimen, the average concentration at Day 83 was 11.59 pg/mL.[49751]
Vaginal Insert (e.g., Imvexxy): The vaginal insert does not increase systemic estradiol concentrations significantly. At Day 84 of study, estradiol concentrations following a 2-week daily regimen followed by a twice-weekly maintenance regimen and compared to baseline concentrations were as follows: For the 4 mcg/dose regimen, mean 4.3 vs. 3.9 pg/mL; for the 10 mcg/dose regimen, mean 4.8 vs. 5 pg/mL; and a mean 4.4 vs. 4.5 pg/mL for placebo.[63254]
Estrogens are contraindicated in patients with hepatic impairment.[32946][46639][47276][49751][49752][51110][51117][52448][52451][56912][57779][58103][61114][61115][62077][63254][67040]
Specific pharmacokinetic data for patients with renal impairment are not available for most estradiol products.[32946][46639][47276][49751][49752][51110][51117][52448][52451][56912][57779][58103][61114][61115][62077][63254][67040]
Specific pharmacokinetic studies are not available for most products in adolescents or children, though systemic and transdermal administration is common for selected patients. Recommended initial doses of estrogen therapy in this population are usually one-eighth to one-tenth the doses used for adult replacement, and vary depending on the formulation used.[62669][62670]
Estradiol is contraindicated for use during pregnancy. There appears to be little or no increased risk of birth defects in children born to individuals who used estrogens and progestins from oral contraceptives inadvertently during early pregnancy. In any patient in whom pregnancy is suspected, pregnancy should be ruled out before continuing estrogen use.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [63254] [67040] In selected instances estradiol has been used off-label as an adjuvant to clomiphene treatment of infertility, or in donor oocyte program procedures in assisted reproduction technology (ART) under the direction of ART specialists; however, treatment is discontinued when pregnancy ensues.[63265]
Use estradiol with caution during breast-feeding. Estrogens are present in human milk and can reduce milk production. This reduction can occur at any time but is less likely to occur once breast-feeding is well-established.[32946] [46639] [47276] [49751] [49752] [51110] [51117] [52448] [52451] [56912] [57779] [58103] [61114] [61115] [62077] [48204] [63254] [67040] Estrogens are not approved for the treatment of postpartum breast engorgement.[67040]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.