ThisiscontentfromElsevier'sDrugInformation
Medroxyprogesterone
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
5 to 10 mg PO once daily for 5 to 10 days, starting anytime during the cycle; but usually started during the latter half of the cycle (days 16 to 21). If the endometrium has been primed with estrogens, administer 10 mg PO once daily for 10 days starting on the 16th day of the cycle. Progestin withdrawal bleeding usually occurs 3 to 7 days after discontinuation of therapy.[59800]
5 to 10 mg PO once daily for 5 to 10 days during the latter half of the cycle (e.g., days 16 to 21). If the endometrium has been primed with estrogens, use 10 mg/day for 10 day. Progestin withdrawal bleeding usually occurs 3 to 7 days after discontinuation of therapy.[59800]
5 to 10 mg PO once daily for 5 to 10 days during the latter half of the cycle (e.g., days 16 to 21). If the endometrium has been primed with estrogens, use 10 mg/day for 10 day. Progestin withdrawal bleeding usually occurs 3 to 7 days after discontinuation of therapy.[59800]
20 mg PO 3 times daily for 7 days, then 20 mg PO once daily for 21 days.[66801] [69683] [69687]
10 to 20 mg PO every 6 to 12 hours for 7 days, then 10 to 20 mg PO once daily for 21 days.[69683] [69685] [69687]
150 mg IM every 13 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[42126]
150 mg IM every 13 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[42126]
104 mg subcutaneously every 12 to 14 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[57649]
104 mg subcutaneously every 12 to 14 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[57649]
104 mg subcutaneously every 12 to 14 weeks for up to 2 years. Use for longer than 2 years is not recommended (unless other birth control methods or medical therapies for endometriosis-associated pain are considered inadequate) due to the impact of long-term treatment on bone mineral density.[57649] [69730]
104 mg subcutaneously every 12 to 14 weeks for up to 2 years. Use for longer than 2 years is not recommended (unless other birth control methods or medical therapies for endometriosis-associated pain are considered inadequate) due to the impact of long-term treatment on bone mineral density.[57649] [69730]
150 mg IM every 6 to 12 weeks.[69730] [71258] [71259]
150 mg IM every 6 to 12 weeks.[69730] [71258] [71259]
10 to 50 mg/day PO.[69730] [70432] [71258] [71259]
Dosage not established. 20 mg PO 3 times per day is a commonly reported dosage. The results of treatment have been contradictory; some studies have reported improvements in oxygenation and ventilation, others have not. Randomized controlled trials are needed to define efficacy and safety, since medroxyprogesterone can increase the risk for thromboembolism in at-risk patients.[61351]
5 mg PO once daily for 12 to 14 sequential days of every month, beginning on day 1 or 16 of the cycle, initially. May increase the dose to 10 mg PO once daily for 12 to 14 sequential days of every month.[59800]
5 mg PO once daily for 10 to 12 sequential days of every 28-day cycle. Progesterone dose should be proportionate to estrogen dose; higher doses of progesterone may be needed as estrogen dose increases. Max: 10 mg PO once daily for 12 days/month. Continue treatment for reproductive life.[71106]
5 mg PO once daily for 10 to 12 sequential days of every 28-day cycle. Progesterone dose should be proportionate to estrogen dose; higher doses of progesterone may be needed as estrogen dose increases. Max: 10 mg PO once daily for 12 days/month. To allow for normal breast and uterine development, delay adding progestin for 1 to 3 years after starting unopposed estrogen or when breakthrough bleeding occurs. Continue treatment for reproductive life.[71106]
2.5 mg PO once daily. Progesterone dose should be proportionate to estrogen dose; higher doses of progesterone may be needed as estrogen dose increases. Max: 5 mg/day. Continue treatment for reproductive life.[71106]
2.5 mg PO once daily. Progesterone dose should be proportionate to estrogen dose; higher doses of progesterone may be needed as estrogen dose increases. Max: 5 mg/day. To allow for normal breast and uterine development, delay adding progestin for 1 to 3 years after starting unopposed estrogen or when breakthrough bleeding occurs. Continue treatment for reproductive life.[71106]
Various doses have been reported; a common dose is 10 mg or 20 mg PO once daily. Several clinical trials have demonstrated the effectiveness of medroxyprogesterone in significantly reducing the number of daily hot flashes in postmenopausal women. The North American Menopause Society (NAMS) Guidelines recommend the short-term use of progestin monotherapy in women who do not want to use or who have contraindications to the use of estrogens and do not have contraindications to progestin therapy and find the potential risks of progestin therapy acceptable. No long term studies have addressed the safety of progestin-only treatment on menopause symptoms.[50638]
Various doses have been reported. 150 mg IM once every month reduced hot flashes by 90% compared to baseline compared to 25% with placebo.[50638] In another study, a single 400 mg IM injection of medroxyprogesterone was compared to venlafaxine 75 mg/day PO. Hot flash scores were reduced by 79% in the medroxyprogesterone arm compared to 55% in the venlafaxine arm after 6 weeks (p less than 0.0001). In addition, significantly more patients receiving medroxyprogesterone had a decrease in hot flashes by 50% compared to baseline (74% for medroxyprogesterone vs. 46% for venlafaxine, p less than 0.0001). Of note, 61% of the women in this trial had a history of breast cancer.[32281] Lower doses (e.g., 150 mg) administered IM once every 3 months have also been shown to be effective.[50638] The North American Menopause Society (NAMS) Guidelines recommend the short-term use of progestin monotherapy in women who do not want to use or who have contraindications to the use of estrogens and do not have contraindications to progestin therapy and find the potential risks of progestin therapy acceptable. No long term studies have addressed the safety of progestin-only treatment on menopause symptoms.[50638]
In one study of 42 postmenopausal women with mild primary hyperparathyroidism, conjugated estrogens 0.625 mg with medroxyprogesterone 5 mg PO once daily for 2 years improved bone mineral density and biochemical markers of bone turnover compared to placebo.[24685]
Dosage is not established. The evidence for effective dosing is lacking due to the lack of controlled trials and need for individualization of dose to response. Secondary outcomes are often reported in the small trials available, such as reduction in sexual fantasy or other compulsive behavior, rather than reduction in sexual offending. Initial doses are usually given once weekly. Maintenance doses range from 200 to 600 mg IM weekly, biweekly, or monthly and are usually adjusted based on patient sexual response, tolerance, and/or plasma testosterone levels.[61348] In one open-label study, male patients with long-standing histories of deviant sexual behavior (n = 48) received weekly medroxyprogesterone acetate IM (dose individualized) along with therapy for up to 12 months. Forty subjects responded positively, all within 3 weeks, with diminished frequency of sexual fantasies and arousal, decreased desire for deviant sexual behavior, increased control over sexual urges, and improvement in psychosocial functioning.[61350]
Dosage is not established. 150 mg or 400 mg IM as needed (once monthly or for a longer duration between doses) based on patient-reported symptoms has been used. In a retrospective review, 91% of 48 patients that received either 150 mg IM or 400 mg IM reported an improvement in hot flashes, with 46% reporting elimination of hot flashes. Patients received additional injections based on symptoms; in general, patients received a median of 4 injections over a 43 month period. Statistical differences between the 2 dosages were not noted; however, the power for detecting a difference between the 2 groups was small because only 8 patients received the 150 mg dose. Only those patients receiving 400 mg IM reported a complete response.[32284]
5 to 20 mg PO once daily.[18759] [69365] [69392] [69393]
2.5 to 10 mg PO every night at bedtime. Max: 40 mg/day. Typically used in combination with estrogen therapy. Dose increase should be based on patient response and monitored hormone levels.[70632] [70633]
2.5 to 10 mg PO every night at bedtime. Max: 40 mg/day. Typically used in combaintion with estrogen therapy. Dose increase should be based on patient response and monitored hormone levels.[70632] [70633]
150 mg IM every 3 months.[70632]
150 mg IM every 3 months.[70632]
2.5 to 20 mg PO once daily for at least 6 months.[70664] [70665] [70666]
100 to 200 mg PO once daily for at least 6 months. Doses up to 600 mg/day have been used to treat atypical endometrial hyperplasia/endometrial intraepithelial neoplasia.[70664] [70674]
10 to 20 mg PO once daily for 10 to 12 sequential days of every cycle for at least 6 months.[70664]
150 mg IM every 3 months for at least 6 months.[70664] [70665]
150 mg IM every 13 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[42126] [58791] [71619] [71620] [71621]
150 mg IM every 13 weeks. Treatment for longer than 2 years is not recommended unless other options are inadequate, due to the impact of long-term treatment on bone mineral density (BMD).[42126] [58791] [71619] [71620] [71621]
For use in gender-affirming therapy:
Dependent on product used and indication for therapy.
Dependent on product used and indication for therapy.
Dependent on product used and indication for therapy.
Not indicated in prepubescent children.
Elimination of medroxyprogesterone is reduced in patients with alcoholic cirrhosis; the oral dose may need to be lowered in patients with significant hepatic impairment. No guidelines are available for the injectable formulations. In general, progestins such as medroxyprogesterone should be avoided in patients with hepatic dysfunction.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication









Medroxyprogesterone is an oral and parenteral synthetic progestin that is 15 times more potent than progesterone. Injectable medroxyprogesteron (Depo-Provera CI and Depo-Subq Provera) are used as a long-acting contraceptive in people of reproductive potential to prevent pregnancy; repeat injections are given every 3 months for a duration of up to 2 years.[42126][57649] The subcutaneous depot contraceptive injection is additionally approved for the management of endometriosis-associated pain.[57649][69730] Hormonal progestin-only contraceptives can be used in people from menarche to over the age of 40 years up until the time of menopause with proper selection of products. The choice of a routine hormonal contraceptive for any given patient is based on the individual's contraceptive needs, underlying medical conditions or risk factors for adverse effects, and individual preferences for use. The Centers for Disease Control's U.S. Medical Eligibility Criteria describe considerations for risk vs. benefits, including medical conditions or attributes that contraindicate use; these criteria can help prescribing practitioners in product selection for individual patients.[48201][66717] Oral medroxyprogesterone is used for the treatment of several hormonal conditions, including the treatment of secondary amenorrhea, abnormal uterine bleeding due to hormonal imbalance in the absence of organic pathology, and in the prevention of endometrial hyperplasia in nonhysterectomized postmenopausal individuals receiving daily estrogen replacement.[59800] A depot injection of medroxyprogesterone is used for adjunctive therapy and palliative treatment of inoperable, recurrent, and metastatic endometrial or renal carcinoma.[57648] Medroxyprogesterone was first approved by the FDA in 1959.
For storage information, see specific product information within the How Supplied section.
Hazardous Drugs Classification
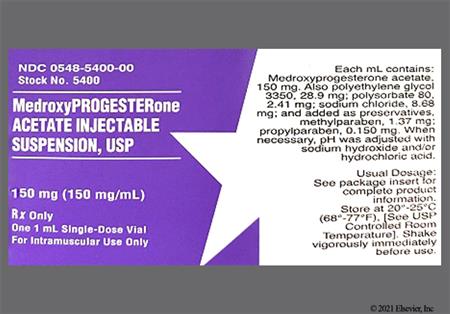
Medroxyprogesterone acetate contraceptive injection suspension 150 mg/mL (e.g., Depo-Provera CI contraceptive injection):
Medroxyprogesterone acetate injection suspension 400 mg/mL:
Medroxyprogesterone acetate contraceptive subcutaneous injection suspension 104 mg/0.65 mL (e.g., Depo-SubQ Provera 104 Contraceptive):
The types of adverse events that are experienced during medroxyprogesterone use are dependent on the indication for use, and the gender of the recipient. Some of the more common events involve the female genitourinary (GU) system. For the use of medroxyprogesterone depot contraceptive injections, menstrual irregularity predominates, with 57.3% of patients reporting irregular menses during the first 12 months and 32.1% after 24 months of use, respectively. Intermenstrual bleeding was reported in roughly 7% of patients during clinical trials for the subcutaneous contraceptive injection, and amenorrhea in approximately 6%. Amenorrhea is even more common with continued contraceptive injection use (55% at 12 months, 68% at 24 months).[42126] [57649] Other GU events reported with contraceptive injection use in 1% to 5% of women include leukorrhea (2.9%), vaginitis (1.2%), abnormal cervical smears, dysmenorrhea, menometrorrhagia, menorrhagia, uterine hemorrhage, and vaginal hemorrhage.[42126] [57649] Postmarketing, the following events have been reported with the medroxyprogesterone contraceptive injections: oligomenorrhea, unexpected pregnancy, uterine hyperplasia, genitourinary infections, and vaginal cysts.[42126] [57649] The following GU effects have been reported in the use of medroxyprogesterone tablets as monotherapy (e.g., without estrogens) in females for hormone replacement therapy (HRT): change in menstrual flow; breakthrough bleeding or spotting; changes in cervical erosion; and changes in cervical secretions.[59800] The incidence of amenorrhea during estrogen-medroxyprogesterone HRT in postmenopausal women is determined by the regimens chosen. Amenorrhea accompanies continuous use of combined HRT in many menopausal women; cyclic administration produces amenorrhea in roughly 5%.[59848] When medroxyprogesterone tablets have been used along with estrogens in women for combined hormone replacement therapy (HRT), abnormal uterine postmenopausal bleeding/spotting/flow; breakthrough bleeding or spotting; dysmenorrhea or pelvic pain; increase in size of uterine leiomyomata; vaginitis, including vaginal candidiasis; changes in amount of cervical secretion; changes in cervical ectropion or cervical dysplasia; endometrial growth, and female-related cancers have been reported. The following adverse reactions have also been observed in females receiving estrogen; progestin combination drugs: premenstrual syndrome, cystitis-like syndrome.[57648] [59800]
The types of adverse events that are experienced during medroxyprogesterone use are dependent on the indication for use, and the gender of the recipient. Changes in the breasts and in sexual function have been reported in both females and males. For the use of medroxyprogesterone depot contraceptive injections in females, breast pain (mastalgia) was reported in 2.8%, and libido decrease in up to 5.5%. Breast lumps, changes in breast size, nipple bleeding, galactorrhea, dyspareunia, and libido increase have been reported in post-market reports with contraceptive depot injection use. Lactation suppression is not common with progestin-only contraception, and depot contraceptive medroxyprogesterone injections are often a hormonal agent of choice in the early weeks postpartum [66564]; however, lactation prevention has been reported postmarketing.[42126] [57649] The following breast changes have been reported in the use of medroxyprogesterone tablets as monotherapy (e.g., without estrogens) in females for hormone replacement therapy (HRT): breast tenderness, mastodynia or mastalgia, or galactorrhea.[59800] When medroxyprogesterone tablets have been used along with estrogens in women in combined HRT regimens, breast tenderness, breast enlargement, pain (mastalgia), nipple breast discharge, galactorrhea; fibrocystic breast changes; and breast cancer have been reported.[59800] Changes in libido (decrease or increase) have been reported with the use of medroxyprogesterone-estrogen HRT regimens and with medroxyprogesterone 400 mg/mL depot injection as well.[57648] In males receiving medroxyprogesterone depot injections for palliative reasons or for paraphilia, impotence (erectile dysfunction) may occur when plasma testosterone levels decreased by 25% (one-quarter) or more of the pretreatment concentration.[57648]
Dermatologic, vascular, and allergic reactions may occur with medroxyprogesterone therapy. Angioedema, anaphylactoid reactions, and anaphylactic shock have been reported with the use of medroxyprogesterone. The following common skin reactions occurred in 1—5% of women receiving medroxyprogesterone depot contraceptive injections: hot flashes or flushes and acne vulgaris; increased acne can be a common reason for contraceptive injection discontinuation. No hair growth or alopecia has been reported in approximately 1.1% of contraceptive injection recipients. The following skin disorders have been reported in patients receiving medroxyprogesterone depot contraceptive injections post-marketing: angioedema, dry skin (xerosis), increased body odor and axillary sweating (hyperhidrosis), axillary swelling, melasma, scleroderma, pruritus, rash (unspecified), and urticaria.[42126] [57649] With the use of medroxyprogesterone 400 mg/mL depot injections and medroxyprogesterone tablets as monotherapy (without estrogens), hypersensitivity reactions (anaphylaxis and anaphylactoid reactions, angioedema), urticaria or rash (allergic) with and without pruritus, acne, loss of scalp hair, alopecia, hot flushes, and hirsutism have been reported.[57648] [59800] The following adverse skin reactions have been observed in women receiving combination hormonal therapy (estrogen along with medroxyprogesterone tablets) for hormone replacement therapy (HRT) regimens: chloasma or melasma that may persist when drug is discontinued, erythema multiforme, erythema nodosum, and hemorrhagic eruption, loss of scalp hair, alopecia.[57648] [59800]
Central nervous system (CNS) reactions, including emotional lability, may occur with medroxyprogesterone therapy. Dizziness (less than 5.6%), insomnia (1% to 5%), nervousness (10.8%), depression (1% to 5%), and headache (9% to 16.5%) have been reported in women receiving medroxyprogesterone depot contraceptive injections [42126] [57649]; women receiving medroxyprogesterone monotherapy for other indications have also reported these adverse events, but the incidence is not known.[59800] Changes in headache or migraine pattern during contraceptive or hormonal therapy use may occur; if a headache or migraine has focal features consistent with cerebral ischemia or a potential thrombotic cause, discontinuation of medroxyprogesterone is recommended.[48201] Anxiety and irritability have been reported in 1% to 5% of women receiving medroxyprogesterone depot contraceptive injections.[57649] Drowsiness/somnolence has been reported during postmarketing experience with medroxyprogesterone depot contraceptive injection and with the use of other medroxyprogesterone formulations for various indications.[42126] [57648] [57649] [59800] Other CNS effects reported postmarketing with the contraceptive injections have included facial palsy, fainting, paralysis, and paresthesias.[42126] [57649] Euphoria has been reported in patients receiving medroxyprogesterone depot injection for malignancy.[57648] Patients with a history of seizure disorder should use medroxyprogesterone cautiously since progestins may exacerbate their condition; seizures have been reported in patients receiving medroxyprogesterone for various indications.[42126] [57648] [57649] [59800] Chorea and mood disturbances have been reported in women receiving combined estrogen plus progestin therapy for hormone replacement.[59800]
Gastrointestinal (GI) effects are fairly common with medroxyprogesterone therapy. Abdominal pain/discomfort (11.2%), nausea (3.3%), and bloating (2.3%) are the most common GI effects with medroxyprogesterone IM depot contraceptive injection; abdominal distention, abdominal pain, diarrhea, nausea occurred in approximately 1% to 5% of those receiving depot subcutaneous contraceptive injections in clinical trials. GI side effects reported postmarketing with contraceptive depot injection use include general GI disturbances, jaundice, excessive thirst (polydipsia) and rectal GI bleeding.[42126] [57649] The following adverse reactions have been reported in women taking medroxyprogesterone tablets as monotherapy (without concomitant estrogens): nausea and cholestatic jaundice (jaundice due to cholestasis).[59800] These effects have also been reported in the use of medroxyprogesterone depot injections for other indications; cholestatic jaundice has included neonatal jaundice and hyperbilirubinemia.[57648] Additional adverse events reported in women receiving combined estrogen and progestin treatment include: nausea, vomiting; abdominal pain, cramps, bloating; cholestatic jaundice; increased incidence of gallbladder disease; pancreatitis; and enlargement of hepatic hemangiomas.[59800]
Changes in appetite may occur during medroxyprogesterone treatment. Appetite stimulation may occur. Weight gain iis a common side effects for medroxyprogesterone contraceptive injections in females; increased weight (defined as a more than 10 pound weight gain at 24 months occurs in 37.7% of patients receiving the IM depot contraceptive injection and 6% of those receiving the subcutaneous contraceptive depot injection. Weight gain one of the primary reasons women discontinue the contraceptive (2% or more discontinue due to weight gain).[42126] [57649] A slight amount of weight gain may be due to fluid retention. Edema is reported in 2.2% of contraceptive depot injection recipients.[42126] [57649] Weight gain or weight loss, fluid retention, and/or edema have been reported for medroxyprogesterone tablets for hormone replacement (HRT) in females or in the use of medroxyprogesterone in men or women for palliation of cancer or other indications.[57648] [59800]
During use of medroxyprogesterone, the provider should be alert to possible thrombotic disorders (e.g., cerebrovascular disorder or migraine or headache with focal symptoms that suggest cerebral ischemia, pulmonary embolism or thromboembolism, thromboembolism, heart attack, or unexplained visual disturbance with ocular pain, which might indicate retinal thrombosis). Should any of these occur or be suspected, medroxyprogesterone therapy should be discontinued immediately; with depot-injections, the effects of the hormone may persist for some time after discontinuation.[59800] [57648] [42126] [57649] [48201] HORMONE REPLACEMENT THERAPY: Hormone replacement therapy (HRT) with estrogens and progestins in combination presents a risk for thromboembolism and cardiovascular events in postmenopausal women; these risks are highlighted in the boxed warnings for oral medroxyprogesterone. The Women's Health Initiative (WHI) estrogen plus progestin substudy reported an increased risk of thromboembolism, including deep vein thrombosis (DVT), pulmonary embolism (PE), stroke and myocardial infarction (MI) in postmenopausal women (50 to 79 years of age) during 5.6 years of treatment with daily oral conjugated estrogens [0.625 mg] combined with medroxyprogesterone acetate oral tablets (MPA) [2.5 mg], relative to placebo. In the absence of comparable data, the risk of such events should be assumed to be similar for other doses of conjugated estrogens/medroxyprogesterone or other estrogen/progestin combinations in postmenopausal women. Should any of these cardiovascular or thrombotic events occur or be suspected, estrogen plus progestin HRT should be discontinued immediately.[27272] [59800] PROGESTIN ONLY CONTRACEPTION: Active thrombophlebitis, or current or past history of thromboembolic disorders, or cerebral vascular disease are contraindications to medroxyprogesterone contraceptive injections. Syncope, sinus tachycardia, chest pain (unspecified), thromboembolism, DVT, PE, thrombo-phlebitis, and varicose veins are cardiovascular effects that have been reported in postmarketing reports from the use of medroxyprogesterone depot contraceptive injections. Although MPA has not been causally associated with the induction of thrombotic or thromboembolic disorders, there have been rare reports of serious thrombotic events in women using MPA contraceptive injections. Any patient who develops thrombosis during contraceptive use should discontinue treatment unless she has no other acceptable options for birth control.[42126] [57649] The use of progestin-only contraception may be acceptable in women without a previous or active history of thromboembolic events, but with certain risk factors for thrombosis, when hormonal contraception is desired. Guidances have been published based on expert review of the literature that can help guide contraceptive product selection in patients with risk factors for thrombosis. Progestin-only contraceptives are generally the hormonal contraceptives of choice in patients with a potential risk for thrombosis when reliable contraception must be ensured and the risks of hormonal therapy are acceptable; advantages of these methods usually outweigh proven or theoretical risks; risk versus benefit must be considered individually. For women who are at an increased risk of thromboembolism and have multiple-risk factors for thrombosis (e.g., tobacco smoking woman age 35 and older, diabetes, hypercoagulopathy, etc.), consider an intra-uterine device (IUD) or other estrogen-free contraceptive if appropriate.[48201] OTHER USES: During clinical use of medroxyprogesterone monotherapy for various indications, effects such as pulmonary embolism (PE) and retinal thrombosis have been rarely reported; when combined with estrogens, various types of thromboembolic events have been reported.[57648]
An injection site reaction can occur with both intramuscular and subcutaneous injections of medroxyprogesterone. Adverse local reactions include residual lump, skin discoloration, pain, tenderness, persistent atrophy, indentation, dimpling, lipodystrophy, and sterile abscess.[42126] [57648] [57649] In women receiving medroxyprogesterone depot contraceptive, injection site reaction was reported in 5% of patients, and 1% had persistent skin changes, typically described as small areas of skin induration or skin atrophy.[57649]
The following adverse reactions have been reported in women taking medroxyprogesterone tablets, without concomitant estrogens treatment: neuro-ocular lesions (e.g., retinal thrombosis) and optic neuritis. The following adverse reactions have been reported with estrogen plus progestin therapy: retinal vascular thrombosis and intolerance to contact lenses. Should retinal thrombosis occur or be suspected, estrogen plus progestin therapy should be discontinued immediately.[59800]
MEDROXYPROGESTERONE CONTRACEPTIVE INJECTIONS: Women using medroxyprogesterone contraceptive injections may lose significant bone mineral density. Bone loss (osteopenia) is greater with increasing duration of use and may not be completely reversible. It is unknown if use of these contraceptive injections during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and increase the risk for osteoporotic fracture in later life. There have been postmarketing reports of osteopenia and loss of bone mineral density as well as osteoporosis, including osteoporotic bone fractures, in patients using medroxyprogesterone depot contraceptive injections. Women should not use medroxyprogesterone injections as a long-term birth control method (i.e., longer than 2 years) unless other birth control methods are considered inadequate.[42126] [57329] In a controlled clinical study, adult women using medroxyprogesterone depot-injections for up to 5 years showed a 5% to 6% mean decrease in spine and hip bone mineral density (BMD), compared to no significant change in BMD in the control group. The decline in BMD was more pronounced during the first 2 years of use, with smaller declines reported in subsequent years. Observed mean changes in lumbar spine BMD of -2.86%, -4.11%, -4.89%, -4.93%, and -5.38% after 1, 2, 3, 4, and 5 years, respectively. A partial recovery of BMD toward baseline values during a 2-year post-therapy period was seen following the cessation of medroxyprogesterone depot injections; longer duration of treatment was associated with less complete BMD recovery during this 2-year post-treatment period. An open-label, non-randomized, clinical study was preformed to evaluate the impact of treatment for up to 4.6 years in adolescent females (12 to 18 years). Results showed that medroxyprogesterone depot injections were associated with a significant decline in BMD from baseline. The decline in BMD was greater with longer duration of use, with a mean decreases in BMD at 4.6 years of -6.4% at total hip, -5.4% at femoral neck, and -2.1% at lumbar spine. In addition, the extent of BMD recovery was evaluated during post-treatment follow-up for up to 60 months. Data revealed that adolescents treated for more than 2 years did not recover baseline BMD at femoral neck or total hip, but did recover baseline BMD at lumbar spine after treatment discontinuation. In comparison, adolescents in the untreated group gained BMD throughout the trial period. The evidence suggests that the increase in bone density that is normally seen during the period of growth following menarche may be impaired by medroxyprogesterone depot injection use.[42126] [57329] OTHER USES: It is possible that osteoporosis may occur with medroxyprogesterone depot injections used chronically for other purposes. An evaluation of bone mineral density may be appropriate in some patients who use higher doses of medroxyprogesterone acetate depot injection for long-term treatment of cancer.[57648]
Decreased glucose tolerance has been reported with medroxyprogesterone monotherapy, and may occur in either gender and during use of the hormone for a variety of indications. Hyperglycemia may occur, and patients with diabetes should be carefully monitored for changes in blood glucose control during medroxyprogesterone treatment.[57648] [42126] [57649] [59800]
Hypercalcemia has been reported in patients receiving medroxyprogesterone depot injection for malignancy.[57648] Hypocalcemia has been reported in patients receiving estrogen plus progestin therapy, and is due to estrogen-induced hypocalcemia.[59800]
Musculoskeletal adverse reactions reported in >= 1% and < 5% of patients receiving depot medroxyprogesterone for contraception (intramuscularly or subcutaneously) include leg muscle cramps (approximately 3.7%), arthralgia (1%), back pain and limb pain.[42126] [57649] Backache and arthralgia have been reported in those receiving estrogen-progestin combined hormonal therapy.[57648] [59800]
Asthenia and/or fatigue (4.2%) occur in > 1% and < 5% of patients receiving medroxyprogesterone contraceptive injections. Post marketing, fever, chills, asthenia have been reported.[42126] [57649] General adverse reactions reported with hormonal therapy with medroxyprogesterone for cancer or hormone replacement include edema, pyrexia, fatigue, malaise.[57648] [59800]
Anemia and blood dyscrasia reported during post-marketing experience with medroxyprogesterone contraceptive injections.[42126] [57649] Aggravation of porphyria has been reported in the use of medroxyprogesterone for cancer or hormone replacement therapy.[57648] [59800]
Estrogen/progestin combination hormonal replacement therapy (HRT) does not prevent mild impaired cognition (memory loss) and has been found to increase the risk of dementia in women 65 years and older. The WHIMS study, an ancillary study of the WHI trial to assess the effects of estrogen/progestin therapy on cognitive function in geriatric women (65 years of age or older), reported similar rates of developing mild cognitive impairment in those receiving active treatment vs. placebo. Also, patients receiving estrogen/progestin combination therapy were more likely than patients receiving placebo to be diagnosed with dementia. The applicability of this finding to women who use estrogen alone or to the typical user of HRT (i.e., younger, symptomatic adult women taking hormone replacement therapy to relieve menopausal symptoms) is unclear. Administration of estrogen/progestin combination therapy should be avoided in women 65 years of age and older and estrogen/progestin combination therapy should not be used to prevent or treat dementia or preserve cognition (memory).[27451] [59800]
The issue of hormonal influences on the development of cancers (new primary malignancy) has been widely researched for many decades. The risks of various cancers for progestin-only hormonal contraceptive use differ from the risks associated with postmenopausal hormone replacement therapy (HRT) or other hormonal uses. Undiagnosed vaginal bleeding should be evaluated in any patient using medroxyprogesterone as is clinically appropriate, since female genital cancers may be influenced by hormonal therapy. HORMONE REPLACEMENT THERAPY POSTMENOPAUSE: Numerous epidemiologic studies have examined the effects of estrogen and estrogen-progestin hormone replacement therapy (HRT) on the development of new primary malignancy (e.g., breast cancer, endometrial cancer, ovarian cancer) in postmenopausal women. The Women's Health Initiative (WHI) estrogen plus progestin study reported increased risks of invasive breast cancer in patients taking combined estrogen-progestin HRT vs. placebo. The potential risk of breast cancer may increase with longer duration of use. Due to breast cancer and other cancer risks, combined HRT should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.[59800] [27272] [32125] [27273] [50638] There is an association of unopposed estrogen therapy and endometrial cancer in women with an intact uterus. Adding a progestin, such as medroxyprogesterone, to estrogen therapy has been shown to reduce, but not eliminate, the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Clinical surveillance of all women using estrogen-alone or estrogen plus progestin therapy is important. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal vaginal bleeding. The reported endometrial cancer risk among unopposed estrogen users is about 2- to 12-times greater than in non-users, and appears dependent on duration of treatment and on estrogen dose. Most studies show no significant increased risk associated with use of estrogens for less than 1 year. The greatest risk appears associated with prolonged use, with increased risks of 15- to 24-fold for 5 to 10 years or more, and this risk has been shown to persist for at least 8 to 15 years after estrogen therapy is discontinued. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens of equivalent estrogen dose. Among combined estrogen/progestin HRT users, roughly 10% will have some endometrial thickening. Postmarketing reports of endometrial hyperplasia have been reported in women receiving combined estrogen/progestin HRT; however, the incidence of endometrial hyperplasia is estimated to be 1% or less in these patients.[59800] [50638] [23505] [27272] Women who used HRT for menopausal symptoms also had an increased risk for ovarian cancer, but data are still uncertain if risk is associated with a specific duration of use. The contraindications and precautions sections for progesterone HRT product labels more fully discuss the data and what is known about HRT use with respect to risks for various cancers.[59800] [27272] [32125] [27273] [50638] MEDROXYPROGESTERONE CONTRACEPTIVE INJECTIONS: The relative risk of developing breast cancer in patients receiving depot medroxyprogesterone for contraception has been investigated in a number of trials. Among 5 epidemiologic studies assessing the associated risk, 3 of the studies suggested a slightly increased risk of breast cancer in the overall population of users. Data from one study (n = 1,028) of women 20 to 44 years of age, receiving medroxyprogesterone contraceptive injections, showed that recent use (last use within the previous 5 years) for 12 months or longer was associated with a 2.2-fold (95% CI: 1.2 to 4.2) increased risk of invasive breast cancer.[42126] [57649] [58771]
Return to ovulation and fertility is likely to be delayed after stopping these injections. Postmarketing, a delayed return to fertility and prolonged anovulation (temporary infertility) have been reported after discontinuation of medroxyprogesterone injections for contraception/endometriosis. In a large U.S. study of women who discontinued use of intramuscular contraceptive injections to become pregnant, data are available for 61% of them. Of the 188 women who discontinued the study to become pregnant, 114 became pregnant. Based on Life-Table analysis of these data, it is expected that 68% of individuals who do become pregnant may conceive within 12 months, 83% may conceive within 15 months, and 93% may conceive within 18 months from the last injection. The median time to conception for those who do conceive is 10 months following the last injection with a range of 4 to 31 months, and is unrelated to the duration of use. No data are available for 39% of the patients who discontinued the contraceptive injection to become pregnant but were lost to follow-up or changed their mind. Return to ovulation is likely to be delayed after stopping the subcutaneous contraceptive injection, as demonstrated in a study of 15 women who received multiple doses: The median time to ovulation was 10 months after the last injection; the earliest return to ovulation was 6 months after the last injection; and 12 women (80%) ovulated within 1 year of the last injection. However, ovulation has occurred as early as 14 weeks after a single dose of the subcutaneous contraceptive injection. Return to fertility is also likely to be delayed after discontinuing subcutaneous therapy. Among 28 women using subcutaneous contraceptive injection who stopped treatment to become pregnant, 7 women were lost to follow-up. One woman became pregnant within 1 year of her last injection and another woman became pregnant 443 days after her last injection. The remaining 19 women had not become pregnant; it is not known if these 19 women were still attempting to become pregnant or if they had started a new contraceptive method.[42126] [57649]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Medroxyprogesterone is contraindicated in people with undiagnosed abnormal uterine bleeding. Evaluate patients presenting with genital bleeding before prescribing medroxyprogesterone. Nonfunctional causes should be considered and adequate diagnostic measures should be undertaken.[42126][57649][59800]
Medroxyprogesterone contraceptive injections do not protect against human immunodeficiency virus (HIV) infection or other sexually transmitted disease. Patients infected with HIV or with known acquired immunodeficiency syndrome (AIDS) should be aware that the use of medroxyprogesterone contraceptive injection will not prevent the transmission of HIV or other sexually transmitted diseases to their partner(s).[42126][57649]
Medroxyprogesterone is contraindicated in patients with pre-existing breast cancer.[42126] [57649] [59800] HORMONE REPLACEMENT THERAPY (HRT): Medroxyprogesterone oral tablets are contraindicated in any other known or suspected estrogen- or progestin-dependent tumor, including cervical cancer, endometrial cancer, uterine cancer, ovarian cancer, or vaginal cancer. There is an increased risk of endometrial cancer in a person with a uterus who uses unopposed estrogens. Adding a progestin to estrogen HRT has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be undertaken to rule out malignancy in postmenopausal women with undiagnosed persistent or recurring abnormal genital bleeding. The use of estrogen-alone or estrogen plus progestin HRT has been reported to result in an increase in abnormal mammograms, requiring further evaluation and observational studies. During the Womens Health Initiative (WHI), estrogen-alone was not associated with an increased risk of invasive breast cancer, but an estrogen plus progestin WHI substudy reported increased risks of invasive breast cancer. Consistent with the WHI clinical trials, observational studies have also reported an increased risk of breast cancer for estrogen plus progestin therapy, and a smaller increased risk for estrogen-alone therapy, after several years of use. All people taking estrogen with or without a progestin as HRT should receive an annual clinical breast examination, perform monthly self-examinations, and have regular mammograms as recommended by their health care professional based on patient age, risk factors, and prior mammogram results.[59800] [71260]
HORMONE REPLACEMENT THERAPY (HRT): Oral medroxyprogesterone is contraindicated in patients with active arterial or venous thromboembolic disease or thromboembolism (e.g., deep venous thrombosis, pulmonary embolism, myocardial infarction (MI), cerebrovascular disease or stroke) or a history of these conditions. Because progesterone and other progestational drugs may cause some degree of fluid retention, conditions which might be influenced by this condition, such as cardiac dysfunction, require careful observation.[59800] Estrogen plus progestin HRT regimens, including the addition of oral medroxyprogesterone to an estrogen HRT regimen, should not be used for the treatment or prevention of cardiovascular disease due to the potential for serious cardiovascular events. The Women's Health Initiative (WHI) estrogen plus progestin HRT substudy reported increased risks of deep vein thrombosis, pulmonary embolism, stroke and myocardial infarction in postmenopausal women (50 to 79 years of age) receiving an estrogen with progestin HRT regimen relative to placebo. Individuals with certain risk factors for arterial vascular disease (e.g., cardiovascular disease, hypertension, diabetes, tobacco smoking, hypercholesterolemia, and morbid obesity) and/or venous thromboembolism (VTE) (e.g., personal history or family history of VTE, obesity, or systemic lupus erythematosus) should be monitored and managed appropriately during oral progesterone use as part of an HRT regimen.[59800] [71260] MEDROXYPROGESTERONE CONTRACEPTIVE INJECTIONS: Medroxyprogesterone contraceptive labels contraindicated use in patients with active thrombophlebitis, or current or history of thromboembolic disorders or thromboembolism, or cerebrovascular disease. Because progesterone and other progestational drugs may cause some degree of fluid retention, conditions which might be influenced by this condition, such as cardiac dysfunction, require careful observation.[42126] [57649] Despite the contraindication against use of medroxyprogesterone contraceptive injection in people with known active or history of thrombotic disease, progestin-only contraceptives are generally the hormonal contraceptives of choice in patients with a potential risk for thrombosis when reliable contraception must be ensured and the risks of hormonal therapy are acceptable; advantages of these methods usually outweigh proven or theoretical risks.[48201] When multiple thrombosis risk factors exist, the risk of thromboembolic disease may increase; determine risk vs. benefit for use of the progestin-only contraceptive. The increase in the risk of thrombosis from newer progestin-only contraceptives (e.g., etonorgestrel implants) is still substantially less than with combined oral contraceptives containing both estrogen and progestin.[48201] For women who are at an increased risk of thromboembolism and have multiple-risk factors for thrombosis, consider an IUD or other estrogen-free contraceptive if appropriate. Use with caution in patients with pre-existing hypertension. A woman who is taking a hormonal contraceptive should have a yearly visit with her care team for a blood pressure check and for other indicated healthcare.[48201]
Medroxyprogesterone contraceptive injections carry a boxed warning regarding bone mineral density reduction (osteopenia) in pre-menopausal individuals. Do not use medroxyprogesterone injections as a long-term contraceptive method (i.e., longer than 2 years) unless other birth control methods are considered inadequate. Consider alternative methods of contraception in people with increased risk for osteoporosis (e.g., strong family history of osteoporosis, metabolic bone disease, alcohol use disorder, anorexia nervosa, tobacco smoking, or chronic use of drugs that can reduce bone mass, such as anticonvulsants or chronic corticosteroid therapy). People using medroxyprogesterone contraceptive injections may lose significant bone mineral density. Bone loss is greater with increasing duration of use and may not be completely reversible. It is unknown if use of these contraceptive injections during adolescence or early adulthood, a critical period of bone accretion, will reduce peak bone mass and cause increased risk for osteoporosis and osteoporotic fracture in later life.[42126] [57649] [48201]
Medroxyprogesterone contraceptive injections are contraindicated in patients with significant hepatic disease and use of these injections should be discontinued if jaundice or disturbances of liver function occur.[57648] [57649] HORMONE REPLACEMENT THERAPY (HRT): Oral medroxyprogesterone is contraindicated for use in people with known hepatic failure, impairment or disease. Progestins may be poorly metabolized in people with impaired liver function. Use estrogen-progestin HRT with caution if the individual has a history of intrahepatic cholestasis of pregnancy or a history of cholestatic jaundice associated with past estrogen use. In the case of recurrence of cholestatic jaundice or elevated liver function tests (LFTs), the HRT regimen should be discontinued until the health care provider determines the drug was not the cause and the jaundice and/or elevated LFTs have resolved. Estrogen plus progestin HRT may cause an exacerbation of porphyria or hepatic hemangioma (benign liver tumor) and should be used with caution in people with these conditions.[59800]
Individuals with diabetes mellitus may have an increased risk for thromboembolism and should be managed appropriately when hormone replacement therapy (HRT) with estrogen plus medroxyprogesterone is used. Consider whether the benefits of HRT outweigh the risks in people with this condition.[59800] Additionally, a decrease in glucose tolerance has been observed in a small percentage of patients receiving progestins. The mechanism of this decrease is not known. For this reason, people with diabetes should be carefully observed while receiving medroxyprogesterone contraception or HRT.[42126] [57649] [59800]
Medroxyprogesterone contraceptive injections should also be used cautiously in individuals with a history of depression.[42126] [57649]
Estrogen plus progestin hormone replacement therapy (HRT) should be used with caution in people with hypoparathyroidism as estrogen-induced hypocalcemia may occur.[59800]
Progestins may cause exacerbation of asthma and should be used with caution in people with this condition.[42126] [57649] [59800]
Because progestins may cause some degree of fluid retention, conditions which might be influenced by this factor, such as migraine, require careful observation. Discontinue medroxyprogesterone pending examination if there is a migraine with focal neurologic or visual changes.[42126] [57649] [59800]
Because progestogens may cause some degree of fluid retention, conditions which might be influenced by this factor (e.g., epilepsy or seizure disorder) require careful observation during medroxyprogesterone use.[42126] [57649] [59800]
Use caution in people with renal impairment or renal failure since data on the safety and efficacy in these individuals is not available. Progestins may cause fluid retention. Conditions that might be affected by fluid retention, such as renal dysfunction, require careful observation when progestins are prescribed.[42126] [57649] [59800]
Administration of hormone replacement therapy (HRT) for menopause should generally be avoided in geriatric adults 65 years of age and older, and HRT should not be used to prevent or treat dementia or preserve cognition (memory). Estrogen plus progestin combination hormone replacement therapy (HRT) fails to prevent mild cognitive impairment (memory loss) and increases the risk of dementia in females 65 years of age and older.[59800] Overall risk vs. benefit should be considered along with the goals of use of HRT for the individual when considering whether to continue HRT in a geriatric adult woman over 65 years of age.[50638] [27451] [32126] [71260]
Discontinue medroxyprogesterone contraception/endometriosis injections during pregnancy; there is no indication for medroxyprogesterone use during pregnancy. Be alert to the possibility of an ectopic pregnancy among individuals using these medroxyprogesterone injections who become pregnant or complain of severe abdominal pain. Epidemiologic studies and meta-analyses have not found an increased risk of genital or non-genital birth defects (including cardiac anomalies and limb-reduction defects) after inadvertent exposure to progestins before conception or during early pregnancy.[42126] [57649] Oral medroxyprogesterone use for secondary amenorrhea, abnormal uterine bleeding or endometrial hyperplasia prophylaxis is contraindicated during known or suspected pregnancy. There may be an increased risk of minor birth defects, such as hypospadias, clitoral enlargement and labial fusion, when there is exposure to progestins during the first trimester of pregnancy; however, a clear association between these conditions and medroxyprogesterone use has not been established.[59800]
Medroxyprogesterone injection may be associated with reproductive risk. When using medroxyprogesterone for endometriosis-associated pain, verify the pregnancy status of people who may become pregnant with pregnancy testing before administering the dose if more than 13 to 14 weeks have passed between injections. Medroxyprogesterone is also indicated for the prevention of pregnancy and would therefore be expected to cause infertility until cessation of treatment.[57649] Individuals may experience a delay in return to ovulation and fertility (conception) after discontinuation of medroxyprogesterone. The median time to conception in fertile individuals is 10 months after the last medroxyprogesterone contraceptive injection (range, 4 to 31 months).[42126] [57649]
Medroxyprogesterone contraception/endometriosis injections may be used during breast-feeding. Although medroxyprogesterone acetate is detectable in human milk following administration of these injections, milk composition, quality, and amount do not appear to be adversely affected during breast-feeding. Effects on milk production and lactation initiation/duration remain unclear when administered before 6 weeks postpartum in those who exclusively breastfeed, and the prescribing labels recommend initiating contraception injections during or after the sixth postpartum week, and this recommendation is consistent with recommendations from the World Health Organization. Neonates and infants exposed to medroxyprogesterone acetate contraceptive/endometriosis injections from breast milk have been studied for developmental and behavioral effects through puberty, and no adverse effects have been noted.[42126] [57649] [48204] The U.S. Medical Eligibility Criteria consider medroxyprogesterone contraception injections compatible with breast-feeding and while caution should be used if the individual is less than 30 days postpartum, the benefits of use likely outweigh any potential risk during that time. Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods) and other progestin-only contraceptives (e.g., norgestrel oral contraceptive, levonorgestrel IUDs).[48201] HORMONE REPLACEMENT: Oral medroxyprogesterone is not recommended for use during breast-feeding due to the fact that detectable amounts of progestin have been identified in the breast milk of individuals receiving progestins, and exposures may be greater than those of the contraceptive injection dosages.[59800]
The primary contraceptive effect of progestins involves the inhibition of gonadotropin secretion (suppression of the midcycle surge of luteinizing hormone, or LH), which prevents follicular maturation and ovulation. The exact mechanism of action, however, is unknown. At the cellular level, progestins diffuse freely into target cells and bind to the progesterone receptor. Target cells include the female reproductive tract, the mammary gland, the hypothalamus, and the pituitary. Once bound to the progesterone receptor, progestins slow the frequency of release of gonadotropin releasing hormone (GnRH) from the hypothalamus and blunt the pre-ovulatory LH surge, thereby preventing follicular maturation and ovulation. Additional mechanisms may be involved. Other contraceptive actions of progestins include alterations in the endometrium that can impair implantation and an increase in cervical mucus viscosity which inhibits sperm migration into the uterus. In five clinical contraception studies, the 12-month failure rate for the group of women treated with medroxyprogesterone-contraceptive depot injection was zero (no pregnancies reported) to 0.7 by Life-Table method.[42126]
Medroxyprogesterone converts a proliferative endometrium into a secretory one in women with adequate endogenous estrogen. Restoring adequate progesterone can help pre-menopausal women with secondary amenorrhea or dysfunctional uterine bleeding to re-establish normal menstrual patterns. The drug reduces endometrial growth in menopausal and postmenopausal women with an intact uterus who are receiving estrogen therapy, thus adding a protective effect against endometrial hyperplasia. Medroxyprogesterone decreases endometriosis related pain by suppressing serum estradiol concentrations and possibly by having a direct action on the lesions of endometriosis. Androgenic and anabolic effects have been noted, but the drug is apparently devoid of significant estrogenic activity. The route and dosage of the drug determine pharmacologic effects. While parenterally administered medroxyprogesterone inhibits gonadotropin production and thus prevents follicular maturation and ovulation, available data indicate that this does not occur when the usually recommended oral dosage is given as single daily doses.[57648][59800]
Progestins are mild, direct stimulants of the respiratory center. During pregnancy and the luteal phase of the menstrual cycle, women can hyperventilate and become hypocapnic due to elevated concentrations of endogenous progestins. Therapeutically, medroxyprogesterone has been used successfully in patients with COPD and hypercapnia, in patients with Pickwickian syndrome, and in patients with sleep apnea.
Revision Date: 10/15/2025, 01:33:00 AMMedroxyprogesterone is administered orally or injected intramuscularly or subcutaneously as a depot injection. Greater than 90% of the absorbed drug is protein bound. Medroxyprogesterone acetate is extensively metabolized in the liver via hydroxylation, with subsequent conjugation and elimination in the urine. Most metabolites are excreted in the urine as glucuronide conjugates with only minor amounts excreted as sulfates.[59800]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: CYP3A4
CYP3A4 is the principal enzyme responsible for the overall metabolism of medroxyprogesterone.[61948]
Peak serum concentrations after oral administration of medroxyprogesterone occur within 2 to 4 hours. The half-life following oral administration of 10 mg for 7 days is variable, but is approximately 16.6 hours to 30 hours. Administration with food increases bioavailability. A 10 mg dose, taken immediately before or after a meal, increased maximum concentration (50 to 70%) and AUC (18 to 33%). The half-life of medroxyprogesterone acetate was not changed with food.[59800]
Peak serum concentrations of medroxyprogesterone occur within 3 weeks after a single IM depot suspension dose. Once peak concentrations are achieved with the IM injection, serum concentrations then begin to decrease exponentially to undetectable levels at 120 to 200 days following the injection. The half-life is roughly 50 days following IM depot administration.[42126][57648]
Peak serum concentrations of medroxyprogesterone are reached within approximately 1 week after a single subcutaneous depot dose. Following subcutaneous administration, serum concentrations at 12 to 14 weeks are generally below 0.5 ng/mL. The half-life is roughly 40 days following subcutaneous depot administration.[57649]
Discontinue medroxyprogesterone contraception/endometriosis injections during pregnancy; there is no indication for medroxyprogesterone use during pregnancy. Be alert to the possibility of an ectopic pregnancy among individuals using these medroxyprogesterone injections who become pregnant or complain of severe abdominal pain. Epidemiologic studies and meta-analyses have not found an increased risk of genital or non-genital birth defects (including cardiac anomalies and limb-reduction defects) after inadvertent exposure to progestins before conception or during early pregnancy.[42126] [57649] Oral medroxyprogesterone use for secondary amenorrhea, abnormal uterine bleeding or endometrial hyperplasia prophylaxis is contraindicated during known or suspected pregnancy. There may be an increased risk of minor birth defects, such as hypospadias, clitoral enlargement and labial fusion, when there is exposure to progestins during the first trimester of pregnancy; however, a clear association between these conditions and medroxyprogesterone use has not been established.[59800]
Medroxyprogesterone contraception/endometriosis injections may be used during breast-feeding. Although medroxyprogesterone acetate is detectable in human milk following administration of these injections, milk composition, quality, and amount do not appear to be adversely affected during breast-feeding. Effects on milk production and lactation initiation/duration remain unclear when administered before 6 weeks postpartum in those who exclusively breastfeed, and the prescribing labels recommend initiating contraception injections during or after the sixth postpartum week, and this recommendation is consistent with recommendations from the World Health Organization. Neonates and infants exposed to medroxyprogesterone acetate contraceptive/endometriosis injections from breast milk have been studied for developmental and behavioral effects through puberty, and no adverse effects have been noted.[42126] [57649] [48204] The U.S. Medical Eligibility Criteria consider medroxyprogesterone contraception injections compatible with breast-feeding and while caution should be used if the individual is less than 30 days postpartum, the benefits of use likely outweigh any potential risk during that time. Alternate contraceptive agents to consider for the breast-feeding individual include non-hormonal contraceptive methods (e.g., copper IUD, barrier methods) and other progestin-only contraceptives (e.g., norgestrel oral contraceptive, levonorgestrel IUDs).[48201] HORMONE REPLACEMENT: Oral medroxyprogesterone is not recommended for use during breast-feeding due to the fact that detectable amounts of progestin have been identified in the breast milk of individuals receiving progestins, and exposures may be greater than those of the contraceptive injection dosages.[59800]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.