ThisiscontentfromElsevier'sDrugInformation
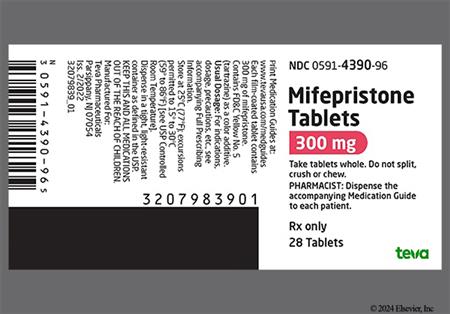
Mifepristone
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
200 mg PO as a single dose, followed by buccal misoprostol 24 to 48 hours later.[28003]
200 mg PO as a single dose, followed by buccal misoprostol 24 to 48 hours later.[28003]
Mifepristone has been designated an orphan drug for this indication by the FDA.
Initially, 300 mg PO once daily with a meal. Increase dose in 300 mg increments, based on clinical response and tolerability. Do not increase more frequently than once every 2 to 4 weeks. Max: 1,200 mg/day and not to exceed 20 mg/kg/day PO. Review drug interactions and product label; specific dosage adjustments and a reduced max dosage are recommended based on the patient's current mifepristone dosage, response, and other treatments. Early symptom improvement, within 6 weeks, may guide dose escalation, later response may guide therapy beyond 2 months. If treatment is interrupted, reinitiate at 300 mg/day. If interruption of treatment is due to an adverse event, titrate to a dose lower than that which resulted in the interruption.[48697] [67118]
600 mg PO given within 72 hours of intercourse was 100% effective in preventing pregnancy and was superior to an estrogen-progestin regimen; adverse effects were less in the mifepristone group[24868]; alternatively, 10 mg PO as a single dose, given within 72 hours of intercourse was found to be as effective as a levonorgestrel regimen (1.5% pregnancy rate in both groups); adverse effects did not differ greatly between the treatment groups.[27310] Mid-level doses of 25 mg, 50 mg, and 100 mg PO of mifepristone have also been successful; pregnancy rates are comparable to the 10 mg dose. Higher doses are associated with a higher incidence in the delay of the start of menses, which may increase patient anxiety.[32604]
2.5 to 10 mg PO once daily.[69364]
200 mg PO as a single dose, followed by intravaginal misoprostol 24 to 36 hours later.[61122] [70356] [70358] [70359] [70360] [70362]
200 mg PO as a single dose, followed by intravaginal misoprostol 24 to 36 hours later.[61122] [70356] [70358] [70359] [70360] [70362]
200 mg PO as a single dose is the FDA-approved maximum dose for termination of pregnancy; 1,200 mg/day PO for Cushing's syndrome and not to exceed 20 mg/kg/day PO; otherwise maximum dose is dependent on the indication for use.
Safety and efficacy have not been established.
200 mg PO as a single dose is the FDA-approved maximum dose for termination of pregnancy; safety and efficacy have not been established for Cushing's syndrome.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Mifeprex (termination of early pregnancy): The effects of hepatic impairment have not been investigated.[28003]
Korlym (Cushing's disease treatment): Do not exceed 600 mg/day PO for mild to moderate hepatic impairment; patients with severe hepatic impairment have not been studied, therefore do not use.[48697]
Mifeprex (termination of early pregnancy): The effects of renal impairment have not been investigated.[28003]
Korlym (Cushing's disease treatment)
CrCl less than 90 mL/min: Do not exceed 600 mg/day PO in patients with renal impairment.[48697]
† Off-label indication
Mifepristone is a synthetic steroid with potent antiprogesterone and antiglucocorticoid activity. It has no estrogenic, antiestrogenic, mineralocorticoid, or antimineralocorticoid activity. It is a derivative of the synthetic progestin norethindrone. Globally, mifepristone is most widely known as a postcoital contraceptive agent and, when used in combination with a prostaglandin, as an abortifacient in early pregnancy. Off-label investigational uses for mifepristone include the treatment of leiomyomata (uterine fibroids), endometriosis, and meningiomas refractory to other therapies. While mifepristone has also been used for cervical priming and for induction of labor at term or in the case of intrauterine fetal death, the data are insufficient to recommend its use over other available drugs. Mifepristone has been studied for the treatment of progesterone receptor positive breast cancer but demonstrated only minimal activity as a single agent.[24818] Mifepristone (e.g., Mifeprex) for the termination of pregnancy (in combination with misoprostol) is available via the Mifepristone REMS program in the United States; more information is available at earlyoptionpill.com.[28003] The FDA approved a separate mifepristone product (Korlym) to control hyperglycemia secondary to hypercortisolism in adults with endogenous Cushing's syndrome who have type 2 diabetes mellitus or glucose intolerance and have failed surgery or are not candidates for surgery.[24819][48697] Mifepristone is a cortisol receptor blocker that improves hyperglycemia and weight gain in these patients; however, use requires expertise in treating Cushing's syndrome and close monitoring for hypokalemia and adrenal insufficiency are needed during chronic therapy. The drug has a long half-life and the potential for many drug-drug interactions.[67118]
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Termination of early pregnancy (e.g., Mifeprex)
Cushing's syndrome (e.g., Korlym)
Other indications (e.g., Korlym)
The antiprogestational effects of mifepristone will result in the termination of pregnancy (fetal death). Mifepristone promotes unopposed endometrial proliferation that may result in endometrium thickening, cystic dilatation of endometrial glands, and vaginal bleeding. Refer individuals who experience vaginal bleeding during chronic mifepristone treatment to a gynecologist for further evaluation.[48697] The pregnancy termination procedure that uses mifepristone (e.g., Mifeprex) is designed to induce the vaginal bleeding and uterine contractions necessary to produce termination of pregnancy (fetal death). If prolonged heavy bleeding is present following mifepristone administration for termination of pregnancy, the patient should be immediately assessed as this could be a sign of serious complications including, but not limited to, incomplete abortion; prompt medical or surgical intervention may be needed.[28003] According to data from clinical trials, women should expect to experience vaginal bleeding or spotting for an average of 9 to 16 days, while up to 8% may experience some type of bleeding for 30 days or more; bleeding was reported to last for 69 days in one patient in the French trials. In general, the duration of bleeding increase as the duration of the pregnancy to be terminated increases. Of note, 80% to 90% of women report that the bleeding is more heavy than that seen during a normal menstrual period, and uterine hemorrhage occurs in roughly 5% of patients. Excessive uterine bleeding may require treatment by vasoconstrictor drugs, curettage, administration of saline infusions, and/or blood transfusions; decreased hemoglobin concentration, hematocrit, and red blood cell (RBC) count may be seen. In U.S. trials, 4.8% of patients received administration of uterotonic medications, 1% received intravenous fluids, and a blood transfusion was given to 1 of 859 patients. In French trials, vasoconstrictor drugs were used in 4.3%, hemoglobin decreases of more than 2 grams/dL occurred in 5.5%, and blood transfusions were administered in two of 1,800 patients. Heavy bleeding required curettage in 1% of patients. Uterine cramping was common when used for pregnancy termination (83% to 96%). Anemia, leukorrhea, uterine rupture, excessive vaginal bleeding or uterine hemorrhage, ruptured ectopic pregnancy, and hematometra were reported during the postmarketing period when used for pregnancy termination.[28003]
Following pregnancy termination with a mifepristone-containing regimen (e.g., Mifeprex), a high index of suspicion is needed to rule out serious infection or sepsis in any patient presenting with general malaise (including weakness) potential GI infectious symptoms (e.g., emesis, etc.), abdominal discomfort, pelvic pain or tenderness, fever, leukocytosis, sinus tachycardia, or hemoconcentration. Termination of pregnancy poses a risk of serious bacterial infection including fatal septic shock (rare). In the U.S., 0.2% of total women studied (n = 629) experienced sepsis. In the days after a medical abortion, indicators of infection include abdominal or pelvic pain or tenderness, or a sustained fever 100.4 degrees F or greater. Any patient reporting abdominal or pelvic discomfort or general malaise (including weakness), emesis, etc. more than 24 hours after receiving misoprostol, must be carefully evaluated to rule out sepsis (from, for example, Clostridium sordellii). Patients with serious bacterial infections (e.g., Clostridium sordellii) and sepsis can also present without bacteremia, significant findings on pelvic exam, or fever. Deaths have been reported in patients who presented without fever, with or without abdominal/pelvic pain, but with leukocytosis with a marked left shift, sinus tachycardia, hemoconcentration, and general malaise.[28003] As of April 2011, 14 deaths were reported in the U.S. following the use of mifepristone and misoprostol, with 8 of these deaths due to sepsis (7 were Clostridium sordellii positive, 1 was Clostridium perfringens positive) and 1 of the deaths due to a delayed onset of toxic shock-like syndrome (uterine cultures were positive for Peptostreptococcus and fibroid cultures were positive for Prevotella). Of the fatal sepsis cases, 7 reported vaginal misoprostol use and 1 reported buccal misoprostol use. There were also reports of 5 deaths in women from foreign countries with 1 of these deaths being associated with septic shock (Clostridium sordellii was identified in tissue samples). Additionally, during clinical trials with mifepristone for abortion, there were reports of fever and/or chills (48%) and postmarketing reports of post-termination infection including endometritis, endomyometritis, parametritis, pelvic inflammatory disease, salpingitis, and pelvic infection.[28003] With the use of mifepristone for Cushing's disease (e.g., Korlym), serious infections are not common; during clinical trials, sinusitis (14%) and naso-pharyngitis (12%) were reported. Dyspnea was reported in 16% of patients. Patients with endogenous Cushing's syndrome are at risk for opportunistic infections such as Pneumocystis jiroveci pneumonia during Korlym treatment. Patients may present with respiratory distress or dyspnea shortly after initiation of mifepristone. Appropriate diagnostic tests should be undertaken and treatment for Pneumocystis jiroveci should be considered.[48697]
Gastrointestinal (GI) side effects have been reported with mifepristone use, both for pregnancy termination and for the treatment of Cushing's syndrome. Abdominal pain was reported more frequently when mifepristone was used for pregnancy termination (83% to 96%) than when used for Cushing's disease (5% to 10%). Additionally, GI side effects have included nausea (48% in Cushing's syndrome trials; 51% to 75% for pregnancy termination), vomiting (26% in Cushing's syndrome trials; 37% to 48% for pregnancy termination), and diarrhea (12% in Cushing's syndrome trials; 18% to 43% for pregnancy termination). Gastroesophageal reflux (5 to 10%), xerostomia (18%), polydipsia or thirst (5 to 10%), constipation (10%), anorexia (10%), and decreased appetite (20%) were also reported during use for Cushing's syndrome. Dyspepsia has been reported during the postmarketing period.[28003] [48697]
During clinical trials for Cushing's syndrome, two patients reported a generalized, maculopapular rash (4%) and two others developed pruritus (4%). Rare but significant adverse reactions reported in the literature include 1 case of toxic epidermal necrolysis (TEN) which included stomatitis. Angioedema has also been reported during postmarketing experience with mifepristone use for Cushing's syndrome.[48697] When used for termination of pregnancy, there have been postmarketing reports of allergic reaction including anaphylactoid reactions, angioedema, rash (unspecified), hives (urticaria), and pruritus.[28003]
Female patients may complain of menstrual irregularity when mifepristone is used for chronic endocrine conditions. In clinical trials for the treatment of Cushing's syndrome, endometrial hyperplasia, menstrual irregularity, and unusual vaginal bleeding were reported. Endometrial thickness above the upper limit of normal was reported in 10/26 females who had baseline and end-of-trial transvaginal ultrasound (38%). The endometrial thickness returned to the normal range in 3 out of 10 patients 6 weeks after treatment cessation at the end of the study. Vaginal bleeding occurred in 5 out of 35 females (14%); 2 of the 5 had normal endometrial thickness. Endometrial biopsies were performed in 6 patients; 5 of these patients had endometrial thickening. No endometrial carcinoma was detected in the sampled cases.[48697] When used off-label for endometriosis and uterine leiomyomas, amenorrhea and anovulation occur, and are typically considered desired effects. Hot flashes or emotional lability have been reported. When used for post-coital contraception, a delay in ovulation, with a longer menstrual cycle and later return of menses, occurs in approximately 10% of patients; women who continue to have unprotected intercourse have a 22% higher pregnancy rate compared to women who use a contraceptive based post-coital method (i.e., the Yuzpe method or levonorgestrel regimen).[26313] [32606] [37679] [37680]
Laboratory abnormalities have been reported with mifepristone use for Cushing's syndrome. Hypoglycemia was reported in 5% to 10% of patients receiving the drug during the various clinical trials. Decreased blood potassium concentrations were common and occurred in 34% of patients during clinical trials. In another study of patients with Cushing's syndrome, hypokalemia was observed in 44% of subjects during treatment. In these cases, hypokalemia responded to treatment with potassium supplementation and/or mineralocorticoid antagonist therapy (e.g., spironolactone or eplerenone). Elevations of thyroid-stimulating hormone (TSH) were seen in subjects treated with mifepristone for Cushing's syndrome. Of the 42 subjects with detectable TSH at baseline, eight (19%) had increases in TSH above the normal range, while remaining asymptomatic. The TSH levels returned to normal in most patients without intervention when the drug was discontinued at the end of the study. Increased blood triglyceride concentrations were reported in 5% to 10% of patients during the various clinical trials for Cushing's syndrome. Decreased high density lipoprotein-cholesterol (HDL-C) concentrations were observed during treatment and returned to baseline after drug discontinuation.[48697]
Adrenocortical insufficiency was reported in two patients (4%) in the controlled clinical trial for Cushing's syndrome. The most typical symptoms were nausea and decreased appetite, and no hypotension or hypoglycemia was reported during the events. Adrenal insufficiency resolved in both cases with mifepristone interruption and/or dexamethasone administration.[48697]
Adverse vascular and cardiovascular related reactions have been reported with mifepristone use. During trials for Cushing's syndrome, hypertension was reported in 24% of mifepristone-treated patients, edema and pitting edema were reported in 5% to 10%, and peripheral edema was reported in 26% of treated patients.[48697] When used for pregnancy termination (e.g., Mifeprex), there have been postmarketing reports of syncope, fainting, loss of consciousness, hypotension (including orthostatic hypotension), lightheadedness, and sinus tachycardia (including racing pulse, heart palpitations, heart pounding).[28003]
Adverse nervous system reactions have been reported with mifepristone use. More common side effects included headache (44% in Cushing's syndrome trials; 2% to 44% when used for termination of pregnancy); dizziness (22% in Cushing's syndrome trials; 9% to 41% for termination of pregnancy); and anxiety (10% in Cushing's syndrome trials; reported postmarketing for termination of pregnancy). Fatigue (48%), pain (unspecified, 14%), somnolence (10%), insomnia (5% to 10%), asthenia (5% to 10%) and malaise (5% to 10%) were reported during trials for Cushing's syndrome.[28003] [48697]
Musculoskeletal system side effects have been reported with mifepristone use. Arthralgia (30%), back pain (16%), myalgia (14%), pain in an extremity (12%), muscular weakness (myasthenia, 5% to 10%), flank pain (5% to 10%), and musculoskeletal pain in the chest (5% to 10%) were reported during trials for Cushing's syndrome.[48697] Back pain and leg pain were reported during postmarketing experience when mifepristone is used for termination of pregnancy.[28003]
Mifepristone has two distinct FDA-approved uses: pregnancy termination and the treatment of Cushing's syndrome. The possibility for teratogenesis may exist, particularly when mifepristone is followed by misoprostol administration, or in the case of inadvertent pregnancy when mifepristone is used for chronic treatment indications.[28003] [48697] The approved labeling for the Korlym product (used in Cushing's syndrome) describes a report of 13 live births following single dose exposure of mifepristone resulting in infants with no abnormalities.[48697] The approved labeling for mifepristone used for pregnancy termination (e.g., Mifeprex) describes only 1 known abnormality detected following administration of mifepristone alone, in a case where mifepristone failed to induce abortion and surgical abortion was then performed. Of 82 cases where mifepristone failed to induce abortion, there were 26 infants born with no detected abnormalities, 9 surgical abortions performed with no detected fetal abnormalities, and 46 cases where the outcome of the infant or fetus is unknown.[28003]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. When used in a medical abortion regimen that requires administration with misoprostol, mifepristone (e.g., Mifeprex) use is also contraindicated in individuals with a history of allergy to misoprostol or other prostaglandins.[28003]
Mifepristone (e.g., Korlym) is for the treatment of hyperglycemia related to Cushing's syndrome. The drug should not be used in the treatment of individuals with type 2 diabetes mellitus unless it is secondary to Cushing's syndrome. In individuals with Cushing's syndrome, changes in glucose control, antidiabetic medication requirements or insulin levels may provide an early assessment of response (within 6 weeks) and may help guide early dose titration.[48697]
The use of mifepristone for medical abortion is assumed to require the same preventive measures as those taken prior to and during surgical abortion to prevent rhesus [Rho] immunization in Rho[D]-negative individuals exposed to Rho[D]-positive fetal blood.[28003]
Mifepristone use for Cushing's disease (e.g., Korlym) is contraindicated for use in individuals with a history of abnormal uterine bleeding, endometrial cancer, or atypical endometrial hyperplasia, due to the potential for mifepristone-induced hormonal and endometrial changes. Mifepristone promotes unopposed endometrial proliferation that may result in endometrium thickening, cystic dilatation of endometrial glands, and vaginal bleeding.[48697]
Serious and sometimes fatal infections and bleeding occur very rarely following spontaneous, surgical, and medical abortions, including following use of mifepristone (e.g., Mifeprex) for medical abortion. These infections may have an atypical presentation. Patients with serious bacterial infections and sepsis can present without fever, bacteremia or significant findings on pelvic examination. A high index of suspicion is needed to rule out serious infection and sepsis. Prolonged heavy bleeding after mifepristone use for medical aborption may be a sign of incomplete abortion or other complications and prompt medical or surgical intervention may be needed.[28003]
When used for pregnancy termination, mifepristone is contraindicated in individuals with an intrauterine device (IUD) in place. Mifepristone can be used if the IUD is removed.[28003]
Mifepristone (e.g., Mifeprex) is contraindicated for pregnancy termination in individuals receiving anticoagulant therapy and individuals with a bleeding disorder, due to the risk for heavy bleeding. Use with caution in individuals with pre-existing severe anemia.[28003] Mifepristone for treatment of Cushing's syndrome (e.g., Korlym) should be used with caution in females who have a bleeding disorder or are receiving concurrent anticoagulant therapy. Being an antagonist of the progesterone receptor, mifepristone promotes unopposed endometrial proliferation that may result in endometrium thickening, cystic dilatation of endometrial glands, and vaginal bleeding during chronic use. Individuals who experience unexplained vaginal bleeding during treatment should be referred to a gynecologist for further evaluation.[48697]
Mifepristone (e.g., Mifeprex) is contraindicated for pregnancy termination in people with chronic adrenal insufficiency or failure due to a risk of acute adrenal insufficiency.[28003] During chronic use of mifepristone for Cushing's syndrome (e.g., Korlym), monitor closely for signs and symptoms of adrenal insufficiency, including weakness, nausea, increased fatigue, hypotension, and hypoglycemia with chronic use. Discontinue mifepristone if adrenal insufficiency is suspected and administer glucocorticoids immediately; high doses and prolonged treatment may be necessary, taking into account the long half-life of mifepristone (85 hours). After symptom resolution, re-instate mifepristone therapy at a lower dose with close monitoring.[48697]
Mifepristone (e.g., Mifeprex) for pregnancy termination is contraindicated in people with inherited porphyria due to the risk of worsening or precipitating attacks.[28003]
Avoid the use of mifepristone for treatment of Cushing's syndrome (e.g., Korlym) in people with baseline QT prolongation or who have conditions that may increase the risk of QT prolongation or torsade de pointes, including bradycardia, congenital long QT syndrome, hypocalcemia, hypokalemia, hypomagnesemia, geriatric adults, females, structural abnormalities that interfere with electrical conduction (e.g., cardiomyopathy, coronary artery disease, ischemic heart disease), or in those who have other additional risk factors for QT prolongation or torsade de pointes. The use of other medications that have been associated with QT prolongation or torsade de pointes may further increase risk.[48697] [65180] [67452] [72115] [72116] [72117] [72118] No research has been conducted to determine the effect of high dose exposure, concomitant dosing with other QT-prolonging drugs, or potassium channel variants resulting in a long QT interval. Therefore, administer mifepristone at the lowest effective dose and monitor for adverse cardiac events.[48697] Hypokalemia should be corrected before mifepristone treatment for Cushing's syndrome (e.g., Korlym) begins. During clinical trials for Cushing's syndrome, hypokalemia was observed during mifepristone (e.g., Korlym) therapy and can occur at any time during treatment. Monitor serum potassium 1 to 2 weeks following dose initiation or increase and periodically thereafter. Correct mifepristone-induced hypokalemia with intravenous or oral potassium supplementation based on clinical need. If hypokalemia persists in spite of potassium supplementation, consider adding mineralocorticoid antagonists.[48697]
Mifepristone (e.g., Korlym), when used in the treatment of Cushing's syndrome, should not be used in people with severe hepatic impairment (Child-Pugh class C) or hepatic failure. Use caution when using mifepristone (e.g., Korlym) in the treatment of Cushing's syndrome in people with mild hepatic impairment (Child-Pugh class A) or moderate hepatic impairment (Child-Pugh class B); maximum dosage adjustments are recommended.[48697]
Use caution when using mifepristone (e.g., Korlym) in the treatment of Cushing's syndrome in people with renal impairment or renal failure, as no initial dosage adjustment is required, but the maximum dose should be adjusted.[48697]
Mifepristone (e.g., Mifeprex) is contraindicated for use if ectopic pregnancy is present. Do not use the mifepristone-misoprostol combination regimen in patients with confirmed or suspected ectopic pregnancy or an undiagnosed adnexal mass; the drug treatment procedure will not be effective to terminate an ectopic pregnancy. Any abdominal pain should be evaluated prior to use and throughout the treatment period, as this may indicate ectopic pregnancy or may indicate an infectious process, which may be serious. An undetected ectopic pregnancy may then rupture and cause serious morbidity. Because ectopic pregnancy may be present despite efforts to rule it out prior to use of the drug, the practitioner should consider the possibility of ectopic pregnancy throughout the treatment period and have a plan for its management.[28003]
Mifepristone has potent antiprogestational effects that will result in the termination of pregnancy. Mifepristone for treatment of Cushing's syndrome (e.g., Korlym) is contraindicated in pregnancy. Should an individual become pregnant while taking mifepristone chronically, the individual should be apprised of the potential fetal risk. There are no data that assess the risk of birth defects in women exposed to mifepristone during pregnancy. Available data limited to exposure following a single dose of mifepristone during pregnancy showed a higher rate of major birth defects compared to the general population comparator. Animal studies also indicate a potential for fetal harm.[48697] Medical abortion with mifepristone (e.g., Mifeprex) is indicated when the objective is termination of the pregnancy at 70 days gestation or less, but should not be used for termination of later pregnancy. Mifepristone disrupts pregnancy, leading to the expulsion of the products of conception; mifepristone also has the pharmacologic effect of inducing uterine contractions and labor. Should the medication regimen fail to terminate a pregnancy as intended, the individual should be apprised of the potential fetal risks. The risk of adverse developmental outcomes with a continued pregnancy after a failed pregnancy termination with mifepristone in a regimen with misoprostol is unknown; however, the process of a failed pregnancy termination could disrupt normal embryo-fetal development and result in adverse developmental effects. Cases of failed terminations and continued pregnancy should be reported to the manufacturer at 1-877-432-7596 or visit www.earlyoptionpill.com. Conception can occur following termination and before resumption of normal menses, so appropriate contraception can be initiated as soon as the pregnancy termination has been confirmed, or before the individual resumes sexual intercourse.[28003]
Counsel people who will receive mifepristone treatment for Cushing's syndrome (e.g., Korlym) about the reproductive risk associated with mifepristone in people who may become pregnant. The antiprogestational effects of mifepristone will result in the termination of pregnancy. Exclude pregnancy before the initiation of treatment. Pregnancy testing should occur before starting the chronic use of mifepristone and if the drug is discontinued for more than 14 days. People who may become pregnant should use non-hormonal contraceptives during treatment and for 1 month after stopping treatment, unless the individual has had a surgical sterilization, in which case no additional contraception is needed. Should a treated individual become pregnant, the individual should be apprised of the potential fetal risk.[48697]
Single-dose regimens of mifepristone may be used with caution during breast-feeding. Limited data show undetectable to negligible levels in human milk after single doses with a relative infant dose range of 0.04% to 0.5%.[70364] [70365] The effects in a nursing infant or on milk production are unknown.[28003] [48697] To minimize exposure to a breastfed infant, individuals who discontinue or interrupt chronic mifepristone treatment may consider pumping and discarding breast milk during treatment and for 18 to 21 days (5 to 6 half-lives) after the last dose, before breast-feeding.[48697]
Mifepristone is a potent antagonist of glucocorticoid and progesterone receptors. Mifepristone is a competitive antagonist with progesterone at the progesterone receptor. The drug has varied actions that contribute to its efficacy for selected indications.
Mifepristone is administered orally. Protein binding is approximately 98%, mostly to alpha-1-acid glycoprotein and to albumin. Mifepristone and its metabolites are distributed to other tissues, including the central nervous system (CNS). It readily crosses the placenta with a maternal:fetal ratio in plasma of 9.1 for mifepristone and 17.1 for the monodemethylated metabolite. Following a distribution phase, elimination is slow at first (50% of a single-dose eliminated in 12 to 17 hours) and then becomes more rapid. Mifepristone is metabolized to demethylated and hydroxylated active metabolites, primarily via hepatic microsomal isoenzyme CYP3A4. The 3 major metabolites are RU-42-433 (a N-monodemethylated metabolite most widely found in the plasma); RU-42-848 (demethylated metabolite); and RU-42-698 (hydroxylated metabolite). Excretion is primarily (approximately 90%) via the fecal route. The half-life after a single 200 mg dose is approximately 18 hours; serum concentrations are undetectable 11 days after administration is discontinued.[28003] Time to steady state is within 2 weeks following chronic dosing, and the mean (SD) half-life of the parent mifepristone was 85 (61) hours following multiple doses of 600 mg/day. [48697]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: CYP3A4, CYP2C8/2C9, and CYP2B6
Because mifepristone is an inhibitor of CYP3A, concurrent use of mifepristone with a drug whose metabolism is largely or solely mediated by CYP3A is likely to result in increased plasma concentrations of that drug, especially with drugs that also have high first-pass effect. Discontinuation or dose reduction of such medications may be necessary with mifepristone use. In addition, Medications that inhibit CYP3A could increase plasma mifepristone concentrations and dose reduction of mifepristone may be required; when used with strong CYP3A inhibitors, the maximum dose of mifepristone must be limited. Mifepristone also inhibits CYP2C8, 2C9 and 2B6, and therefore may increase the concentrations of drugs largely dependent on these CYP enzymes for drug metabolism.[48697] Based on the long terminal half-life of mifepristone after reaching steady state when used in chronic dosing regimens, at least 2 weeks should elapse after cessation of mifepristone before initiating or increasing the dose of any interacting concomitant medication.[48697]
In vitro studies also indicate an interaction potential for drugs metabolized by CYP2A6, 2C19, 1A2, 2D6 and 2E1, by mifepristone and/or its metabolites. However, clinical in vivo drug-drug interaction studies have not been performed. Additionally, mifepristone binds P-glycoprotein (P-gp), inhibiting P-gp activity and breast cancer resistance protein (BCRP).[34716]
The absolute bioavailability of mifepristone after a 20 mg dose is 69%. Following oral administration, time to peak plasma concentrations (Tmax) of mifepristone occurred between 1 and 2 hours following a single dose, and between 1 and 4 hours following multiple doses of 600 mg of mifepristone in healthy volunteers. After ingestion of a single 200 mg dose, mean Cmax of 1.77 +/- 0.7 mg/L occurs; mean AUC was 25.8 +/- 6.2 mg x hour/L.[28003] After ingestion of a single 600 mg dose, a Cmax of 1.98 +/- 1 mg/L was attained. Mean plasma concentrations of the 3 active metabolites of mifepristone peak between 2 and 8 hours after multiple doses of 600 mg/day, and the combined concentrations of the metabolites exceed that of the parent mifepristone. Exposure to mifepristone is substantially less than dose proportional.[48697]
The pharmacokinetics of mifepristone in subjects with moderate hepatic impairment was similar to those with normal hepatic function; however, due to lack of discrete safety data, maximum doses in these patients are recommended to be reduced. Mifepristone has not been studied in patients with severe hepatic impairment (Child-Pugh Class C). The pharmacokinetics of mifepristone in patients with moderate hepatic impairment (Child-Pugh Class B) were evaluated in a single- and multiple-dose study (600mg for 7 days). Pharmacokinetic parameters were similar compared to patients with normal hepatic function. There was a large variability in the exposure of mifepristone and its metabolites in patients with hepatic impairment compared to those with normal function for AUC of mifepristone (1.02 [CI 0.59 to 1.76]), metabolite 1 (0.95 [CI 0.52 to 1.71]), metabolite 2 (1.37 [CI 0.71 to 2.62]), and metabolite 3 (0.62 [CI 0.33 to 1.16]).[48697] When used for termination of early pregnancy, mifepristone pharmacokinetic parameters have not been evaluated in patients with hepatic impairment.[28003]
No change in the initial dose of mifepristone is needed for renal impairment, but the maximum dose allowed is reduced. The pharmacokinetics of mifepristone 1,200 mg/day for 7 days were evaluated in patients with severe renal impairment (CrCl less than 30 mL/minute, but not on dialysis). Compared to patients with normal renal function, mean exposure increased 31%, with similar or smaller increases in metabolite exposure. There was large variability in the exposure of mifepristone and its metabolites in patients with severe renal impairment compared to those with normal renal function for AUC of mifepristone, and its 3 active metabolites.[48697] When used for termination of early pregnancy, mifepristone pharmacokinetic parameters not been evaluated in patients with renal impairment.[28003]
Mifepristone has potent antiprogestational effects that will result in the termination of pregnancy. Mifepristone for treatment of Cushing's syndrome (e.g., Korlym) is contraindicated in pregnancy. Should an individual become pregnant while taking mifepristone chronically, the individual should be apprised of the potential fetal risk. There are no data that assess the risk of birth defects in women exposed to mifepristone during pregnancy. Available data limited to exposure following a single dose of mifepristone during pregnancy showed a higher rate of major birth defects compared to the general population comparator. Animal studies also indicate a potential for fetal harm.[48697] Medical abortion with mifepristone (e.g., Mifeprex) is indicated when the objective is termination of the pregnancy at 70 days gestation or less, but should not be used for termination of later pregnancy. Mifepristone disrupts pregnancy, leading to the expulsion of the products of conception; mifepristone also has the pharmacologic effect of inducing uterine contractions and labor. Should the medication regimen fail to terminate a pregnancy as intended, the individual should be apprised of the potential fetal risks. The risk of adverse developmental outcomes with a continued pregnancy after a failed pregnancy termination with mifepristone in a regimen with misoprostol is unknown; however, the process of a failed pregnancy termination could disrupt normal embryo-fetal development and result in adverse developmental effects. Cases of failed terminations and continued pregnancy should be reported to the manufacturer at 1-877-432-7596 or visit www.earlyoptionpill.com. Conception can occur following termination and before resumption of normal menses, so appropriate contraception can be initiated as soon as the pregnancy termination has been confirmed, or before the individual resumes sexual intercourse.[28003]
Single-dose regimens of mifepristone may be used with caution during breast-feeding. Limited data show undetectable to negligible levels in human milk after single doses with a relative infant dose range of 0.04% to 0.5%.[70364] [70365] The effects in a nursing infant or on milk production are unknown.[28003] [48697] To minimize exposure to a breastfed infant, individuals who discontinue or interrupt chronic mifepristone treatment may consider pumping and discarding breast milk during treatment and for 18 to 21 days (5 to 6 half-lives) after the last dose, before breast-feeding.[48697]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.