ThisiscontentfromElsevier'sDrugInformation
Ondansetron
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
0.15 mg/kg (150 mcg/kg) IV infused over 15 minutes beginning 30 minutes prior to the initiation of emetogenic chemotherapy. No single dose should exceed 16 mg/dose IV. Dosage may be repeated twice, administered 4 and 8 hours after the initial dose. NOTE: Since 2012, a 32 mg IV single-dose regimen is no longer indicated because of the risk of QT prolongation.[31266] [51100] [63197]
0.15 mg/kg IV infused over 15 minutes beginning 30 minutes prior to the initiation of chemotherapy and repeat 4 and 8 hours later (3 doses total). Max: 16 mg/dose.[31266] [52202] The American Society of Clinical Oncology (ASCO) recommends 0.15 mg/kg/dose (Max: 8 mg) twice daily during chemotherapy and for 2 days after completion, or give 1 to 2 hours before each fraction of radiation and for 1 day after completion for highly emetogenic therapy.[63197] Alternatively, ondansetron has been administered every 8 hours and continued for 1 to 5 days after completion of therapy.[49435] [52191] [52192] A single dose of 0.6 mg/kg IV was as effective as standard therapy (0.15 mg/kg/dose up to 8 mg every 4 hours for 4 doses) in a prospective, double-blind study in chemotherapy-naive pediatric oncology patients; however, the maximum dose in the study was 32 mg, which is no longer recommended because of dose-dependent QT prolongation.[52188]
8 mg PO twice daily. Give first dose 30 minutes before the start of emetogenic chemotherapy, with a subsequent dose 8 hours after the initial dose. Further doses may be given every 12 hours for 1 to 2 days after completion of chemotherapy.[49444]
24 mg dose PO once given 30 minutes before administration of single-day highly emetogenic chemotherapy, including cisplatin 50 mg/m2 or more. Multiday, single dose administration of ondansetron 24 mg has not been studied.[49444]
8 mg PO 3 times daily.[49444]
8 mg PO 1 to 2 hours prior to each fraction of radiotherapy each day.[49444]
Initially, 8 mg PO 1 to 2 hours prior to radiotherapy. Then, 8 mg PO every 8 hours after the first dose for 1 to 2 days following completion of radiotherapy.[49444]
8 mg PO twice daily. Give the first dose 30 minutes prior to chemotherapy with a subsequent dose 8 hours after the initial dose. Further doses may be given every 12 hours for 1 to 2 days after completion of therapy.[49444] For radiation, give the first dose 1 to 2 hours prior to therapy. Further doses may be given every 8 to 12 hours for 1 to 5 days after completion of therapy.[63197] [52191] [52192] Alternatively, a single 24 mg PO dose may be given prior to chemotherapy.[52202]
4 mg PO 3 times daily. Give the first dose 30 minutes prior to chemotherapy, with subsequent doses 4 and 8 hours after the initial dose. Further doses may be given every 8 hours for 1 to 2 days after completion of therapy.[49444] For radiation, give the first dose 1 to 2 hours prior to therapy. Further doses may be given every 8 hours for 1 to 5 days after completion of therapy.[52191] [52192] Alternatively, a single 12 mg PO dose may be given prior to chemotherapy.[52202]
4 mg PO 3 times daily.[52194] Give the first dose 30 minutes prior to chemotherapy or 1 to 2 hours prior to radiation.[40241] May be continued for 1 to 5 days after completion of therapy.[40241] [52191]
3 mg PO 3 times daily.[52194] Give the first dose 30 minutes prior to chemotherapy or 1 to 2 hours prior to radiation.[40241] May be continued for 1 to 5 days after completion of therapy.[40241] [52191]
2 mg PO 3 times daily.[52192] [52194] Give the first dose 30 minutes prior to chemotherapy or 1 to 2 hours prior to radiation.[40241] May be continued for 1 to 5 days after completion of therapy.[40241] [52191]
1 mg PO 3 times daily.[52194] Give the first dose 30 minutes prior to chemotherapy or 1 to 2 hours prior to radiation.[40241] May be continued for 1 to 5 days after completion of therapy.[40241] [52191]
4 mg IV once; a 5-HT3 antagonist is recommended if no prophylaxis was given, or for those who received a prophylactic antiemetic from another drug class. Administration of a second IV dose postoperatively in response to inadequate control is generally not effective; consider use of an antiemetic from another pharmacologic class.[57398]
4 mg IV once; a 5-HT3 antagonist is recommended if no prophylaxis was given. Administration of a second IV dose postoperatively in response to inadequate control is generally not effective; consider use of an antiemetic from another pharmacologic class.[31266] [49437]
0.05 to 0.1 mg/kg IV once; a 5-HT3 antagonist is recommended if no prophylaxis was given. Administration of a second IV dose postoperatively in response to inadequate control is generally not effective; consider use of an antiemetic from another pharmacologic class.[31266] [49437] Among children who had at least 2 postoperative episodes of retching or vomiting within 2 hours of surgery and who had not received prophylaxis, 53% had complete control of vomiting (no emesis and no rescue 24 hours after the dose) with a single 0.1 mg/kg (Max: 4 mg) IV ondansetron dose as compared with 17% of placebo recipients.[55979]
4 mg IV as single dose given immediately prior to or following anesthesia induction, or once postoperatively if patient experiences nausea/vomiting shortly after surgery. Administration of a second IV dose postoperatively in response to inadequate control is generally not effective; use of an antiemetic from another pharmacologic class should be considered.[31266] [57398]
0.05 to 0.1 mg/kg IV as single dose given immediately prior to or following anesthesia induction, or once postoperatively if patient experiences nausea/vomiting shortly after surgery. Max: 4 mg/dose. Administration of a second IV dose postoperatively in response to inadequate control is generally not effective; use of an antiemetic from another pharmacologic class should be considered.[31266] [49437] [52205]
4 mg IM as single dose given immediately before anesthesia induction, or once postoperatively if patient experiences nausea/vomiting shortly after surgery. Administration of a second dose postoperatively in response to inadequate control is generally not effective; use of an antiemetic from another pharmacologic class should be considered.[31266]
16 mg PO as single dose given 1 hour before anesthesia induction.[49444] Alteratively, 8 mg ODT PO as a single dose given at the end of surgery is as effective as 4 mg IV according to clinical practice guidelines.[57398]
0.15 mg/kg PO as single dose, immediately prior to or after anesthesia induction, or once postoperatively if patient experiences nausea/vomiting shortly after surgery. Max: 8 mg/dose.[52220] Administration of a second dose postoperatively in response to inadequate control is generally not effective; use of an antiemetic from another pharmacologic class should be considered.[31266] [49437]
4 mg PO every 8 hours as needed.[66066]
8 mg IV every 12 hours as needed.[66066]
0.15 mg/kg/dose (Max: 8 mg/dose) IV as a single dose has been used along with oral or IV rehydration.[27475] [57888] Although routine use of antiemetics is not recommended, some studies have shown that single IV doses of ondansetron are safe and effective for reducing vomiting and increasing patients' ability to tolerate oral rehydration.[27475] [52201] [52241] [57888]
0.2 mg/kg/dose (Max: 8 mg/dose) PO as a single dose along with oral or IV rehydration.[44904] [52245] [70861] [70865] Alternatively, 0.2 mg/kg/dose PO every 8 hours for 3 doses has also been studied.[57896] Studies have shown that single and multiple oral doses of ondansetron are safe and effective for reducing vomiting and increasing individuals' ability to tolerate oral rehydration.[52245] [57896] [61308] [64934] [70861] [70865] [70866] [70867]
0.2 mg/kg/dose (Max: 4 mg/dose) PO as a single dose along with oral or IV rehydration.[44904] [52245] [70861] [70865] Alternatively, 0.2 mg/kg/dose PO every 8 hours for 3 doses has also been studied.[57896] Studies have shown that single and multiple oral doses of ondansetron are safe and effective for reducing vomiting and increasing individuals' ability to tolerate oral rehydration.[52245] [57896] [61308] [64934] [70861] [70865] [70866] [70867]
0.2 mg/kg/dose (Max: 2 mg/dose) PO as a single dose along with oral or IV rehydration.[44904] [52245] [70861] [70865] Alternatively, 0.2 mg/kg/dose PO every 8 hours for 3 doses has also been studied.[57896] Studies have shown that single and multiple oral doses of ondansetron are safe and effective for reducing vomiting and increasing individuals' ability to tolerate oral rehydration.[52245] [57896] [61308] [64934] [70861] [70865] [70866] [70867]
Five patients with severe pruritus secondary to cholestasis were treated with ondansetron. An initial dose of 8 mg IV was administered. Pruritus was relieved completely in 3 patients and partially in 2 with effects lasting 5—16 hours. Three patients were continued on oral therapy of 8 mg PO twice daily, with decreased severity of symptoms.[24001] Dosage should be adjusted in hepatic impairment.
A dosage of 4 mcg/kg PO twice per day, combined with weekly standardized group behavioral therapy, was effective in reducing alcohol consumption. Ondansetron was superior to placebo in increasing percentage of days abstinent and total days abstinent per study week. The results suggest that ondansetron is an effective treatment for patients with early-onset ethanol dependence, presumably by ameliorating an underlying serotonergic abnormality.[26327] NOTE: Pharmacotherapy should be used as a part of a comprehensive management program that includes psychosocial support and treatment.
8 mg IV every 4 to 6 hours as needed.[68523]
0.3 to 0.4 mg/kg/dose (Max: 20 mg/dose) IV every 4 to 6 hours as needed.[31266] [52129] [68524]
8 mg PO every 6 to 8 hours as needed for 24 to 48 hours if intravenous therapy is initially effective.[68523]
4 mg IV or IM as a single dose.[44224] [68519] [68555] [68572] [68573]
4 mg IV or IM as a single dose.[68573]
4 mg PO as a single dose.[68573] [68555]
4 mg PO as a single dose.[68573]
4 mg IV every 6 to 8 hours.[70838]
4 mg IV every 8 hours as needed.[71640] [71641]
0.15 mg/kg/dose (Max: 8 mg/dose) IV every 12 hours as needed.[71641] Alternatively, 4 mg IV as a single dose.[71640]
0.15 mg/kg/dose IV every 12 hours as needed.[71641] Alternatively, 0.1 mg/kg/dose IV as a single dose.[71640]
8 mg PO every 12 hours as needed.[71641]
0.15 mg/kg/dose (Max: 8 mg/dose) PO every 12 hours as needed.[71641]
24 mg/day PO; 0.45 mg/kg/day IV (in 3 divided doses, max single dose = 16 mg IV).
24 mg/day PO; 0.45 mg/kg/day IV (in 3 divided doses, max single dose = 16 mg IV).
0.15 mg/kg/dose IV (Max: 16 mg/dose IV). 16 mg/day PO.
< 4 years: 0.15 mg/kg/dose IV (Max: 16 mg/dose). Safety and efficacy have not been established for PO formulation.
4—11 years: 0.15 mg/kg/dose IV (Max: 16 mg/dose). 12 mg/day PO.
>= 12 years: 0.15 mg/kg/dose IV (Max: 16 mg/dose). 16 mg/day PO.
1—5 months: 0.1 mg/kg IV (single dose). Safety and efficacy have not been established for PO formulation.
>= 6 months: 0.15 mg/kg/dose IV (Max: 16 mg/dose IV). Safety and efficacy have not been established for PO formulation.
Safety and efficacy have not been established.
Per the manufacturer, ondansetron dosage should not exceed 8 mg/day IV or PO in adult patients with severe hepatic impairment (Child-Pugh score >= 10). In such patients, plasma clearance is reduced, resulting in a dramatically prolonged elimination half-life.[31266] No specific pediatric recommendations are available.
No dosage adjustments are recommended. A small percentage (5%) of ondansetron is renally cleared. In patients with severe renal impairment (CrCl < 30 ml/min) the mean plasma clearance is reduced; however, the reduction is not consistent with an increase in half-life.[31266]
† Off-label indication
























Ondansetron is an oral and parenteral serotonin (5-HT3) receptor antagonist. Ondansetron is used as an antiemetic agent for the prevention and treatment of nausea and vomiting during chemotherapy, radiation therapy, and surgery.[31266] Ondansetron has occasionally been utilized for the treatment of hyperemesis gravidarum refractory to other treatments. Novel investigational uses of ondansetron include treatment of gastrointestinal motility disorders and drug dependence (e.g., alcoholism). In the pediatric population, ondansetron is also used off-label for cyclic vomiting syndrome and gastroenteritis-induced vomiting.[52241][52129] Ondansetron is an extremely safe and highly effective antiemetic compared to older, traditional antiemetics (e.g., metoclopramide, droperidol); however, there is a risk of dose-dependent QT-prolongation and torsade de points.[31266][52167] When administered at optimal doses, ondansetron and other 5HT3 receptor antagonists (e.g., granisetron) are equally effective.[52202] The American Society of Clinical Oncology (ASCO) guidelines recommend that adult patients who are treated with moderate to high-emetic-risk chemotherapy agents should be offered a 3-drug combination of a 5-HT3 receptor antagonist, a neurokinin 1 (NK1) receptor antagonist, and dexamethasone; olanzapine is also added to the 3-drug combination during use of high-emetic-risk agents.[63197] Children receiving moderate to high-emetic-risk agents should be offered a 2-drug combination of a 5-HT3 receptor antagonist and dexamethasone; aprepitant is also added to the 2-drug combination during use of high-emetic-risk agents.[63197][49435] The Society for Ambulatory Anesthesia (SAMBA) guidelines recommend the use of a 5-HT3 receptor antagonist as the first choice for prophylaxis of postoperative nausea and vomiting in children.[49437]
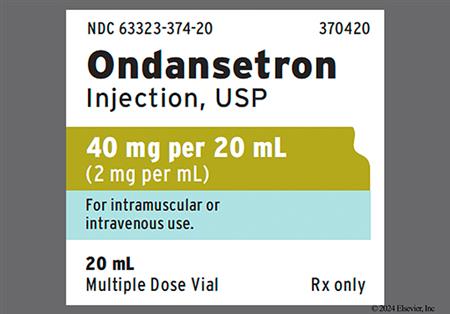
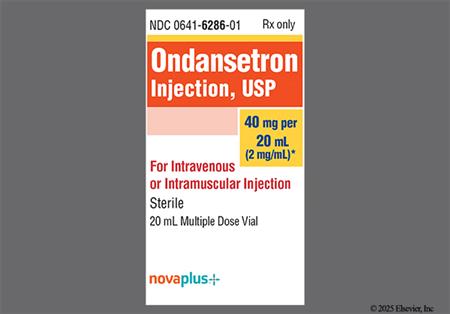
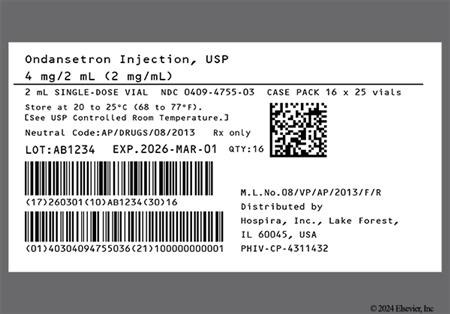
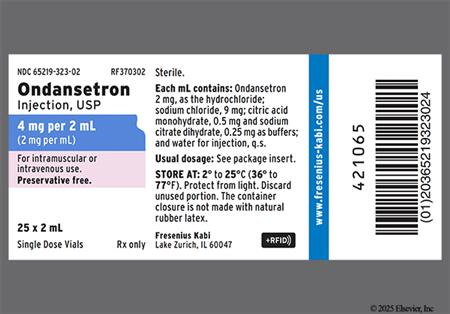
For storage information, see the specific product information within the How Supplied section.
Oral disintegrating tablets (ODT):
Oral soluble film (Zuplenz):
IV Push
Intermittent IV Infusion
Diarrhea (2—16%) and constipation (6—11%) were among the most frequently reported adverse events in patients receiving ondansetron during clinical trials for chemotherapy-induced nausea and vomiting (CINV) with moderate-high emetogenic agents.[31266] [49444] Hiccups have been reported during post-marketing experience with ondansetron.[31266]
Urinary retention (5%) and gynecological disorder (7%) have been reported in patients receiving oral ondansetron for postoperative nausea and vomiting (PONV) during clinical trials.[49444]
Headache (9—27%) was the most frequently reported adverse event during clinical trials of ondansetron and appeared to be more common in patients receiving the drug for chemotherapy-induced nausea and vomiting (CINV). Preliminary observations in a small number of subjects suggest a higher incidence of headache when ondansetron orally disintegrating tablets are taken with water, when compared to without water. Other neurologic side effects reported include drowsiness (8—20%), malaise and fatigue (9—13%), anxiety or agitation (<= 6%), paresthesias (2%), and dizziness (4—7%). Transient dizziness associated with intravenous infusion has been reported post-marketing. Rarely, extrapyramidal reactions, including oculogyric crisis appearing alone or with other types of dystonic reaction, have been reported with ondansetron use.[31266] [49444] In one case, extrapyramidal reactions were confirmed by rechallenge.[31899] In addition, there have been rare reports of grand mal seizures in patients receiving ondansetron, although a casual relationship has not been established.[31266]
Elevated hepatic enzymes were reported in patients receiving either cisplatin- or cyclophosphamide-based chemotherapy during clinical trials. The elevation did not appear to be related to ondansetron dose or duration of therapy. The enzyme levels exceeded twice the upper limit of normal (ULN) in approximately 5% of chemotherapy patients receiving injection dosing, and 1—2% of patients receiving oral therapy, but the increases were transient in nature and did not cause symptomatic hepatic disease. Repeat exposure showed similar elevations in some instances. In addition, hepatic failure and death have been reported in patients with cancer receiving concomitant medications including potentially hepatotoxic cytotoxic chemotherapy and antibiotics; the etiology of the hepatic failure is unclear.[31266] [49444]
Rare cases of hypokalemia have been reported following treatment with ondansetron in oncology patients; the relationship to ondansetron is unclear.[31266] [49444] It may be prudent to monitor serum electrolytes in select patients, as hypokalemia is a risk factor for electrocardiogram (ECG) changes.[31266] [49444]
Ondansetron has been associated with QT prolongation and torsade de pointes. Patients at risk for developing torsade de pointes include those with underlying heart conditions, such as congenital long QT syndrome (avoid use), those who are predisposed to hypokalemia and hypomagnesemia, and those taking other medications that lead to QT prolongation.[45648] Other cardiovascular adverse events reported during clinical trials with ondansetron include angina, chest pain (unspecified), ECG alterations (including second-degree AV block, QT prolongation, and ST-T wave changes), hypotension (5%), and sinus tachycardia. Bradycardia (6% vs. 6% placebo) was reported in patients receiving oral ondansetron for postoperative nausea and vomiting (PONV). Syncope, palpitations, and arrhythmias, including ventricular tachycardia and supraventricular tachycardia (SVT), bradycardia, premature ventricular contractions (PVCs), atrial fibrillation, and acute myocardial ischemia have been reported during postmarketing use of ondansetron. In some cases, predominantly during intravenous administration, the symptoms of myocardial ischemia appeared immediately after administration but resolved with prompt treatment. Coronary vasospasm (coronary artery spasm) appears to be the most common cause of the ischemia. To minimize the risk of these adverse events in patients receiving intravenous treatment, do not exceed the recommended ondansetron infusion rate and monitor patients for signs and symptoms of myocardial ischemia during and after administration. In patients receiving oral therapy, monitor or advise patients of these symptoms.[31266] [49444] Intravenous (IV) ondansetron given as a single 32 mg dose causes QT prolongation in a dose-dependent manner; therefore, single IV doses should not exceed 16 mg/dose IV; the 32 mg IV single-dose regimen is no longer indicated for chemotherapy-induced nausea and vomiting (CINV). Oral dosing recommendations have not changed.[51100] ECG monitoring is recommended in patients with electrolyte imbalance (e.g., hypokalemia or hypomagnesemia), congestive heart failure, significant bradycardia, or in patients taking other medications that can lead to QT prolongation.[31266] [49444] [45648]
Several reports of anaphylactoid reactions have been associated with serotonin (5-HT3) receptor antagonists, such as ondansetron.[23534] [52212] Manifestations of anaphylactoid reactions have included angioedema, bronchospasm, dyspnea, hypotension, laryngeal edema, stridor, and/or urticaria. Laryngospasm, shock, cardiac arrest, and respiratory arrest have been reported during allergic reactions in patients receiving injectable ondansetron. Rash (unspecified) (1%), pruritus (2—5%), and flushing have been reported in clinical trials with both oral and injectable formulations.[31266] [49444] Stevens-Johnson syndrome and toxic epidermal necrolysis (TENS) have been reported with post-marketing use of ondansetron.[31266] [49444]
An injection site reaction (4%) was reported in patients receiving ondansetron injection intravenously over 2 to 5 minutes during clinical trials for post-operative nausea/vomiting (PONV); symptoms included pain, erythema, and burning at the site.[31266]
Visual impairment has occurred with ondansetron use. Cases of transient blindness, predominantly during intravenous (IV) administration, have been reported; resolution occurred within minutes up to 48 hours. Sudden blindness (amaurosis) of 2—3 minute duration occurred in one patient who was administered ondansetron 72 mg IV as a single dose.[49444] [31266] In another case, transient blindness was reported in a patient who received ondansetron 4mg as a post-operative rapid IV bolus dose.[31837] The mechanism by which ondansetron may cause visual impairment is not well understood. Clinicians in the latter case suggest that it may be related to the rate of administration. Transient blurred vision, in some cases associated with accommodation disorder, has also been reported during post-marketing experience.[31266]
Fever (2—8%) and shivers or chills (2—5%) were reported in patients receiving ondansetron during clinical trials. Wound problems (28% vs. 31% placebo) were reported in patients receiving oral ondansetron for postoperative nausea and vomiting (PONV).[31266] [49444]
Serotonin syndrome has been reported with 5-HT3 receptor antagonists, such as ondansetron, during concurrent use of other medications known to increase CNS or peripheral serotonin levels or during overdose. Some of the reported cases were fatal; most occurred in a post-anesthesia care unit or infusion center. If serotonin syndrome becomes evident during treatment, discontinue ondansetron and any other serotonergic agents and initiate appropriate medical treatment. Serotonin syndrome is a range of signs and symptoms that can include mental status changes (e.g., agitation, hallucinations, delirium, coma), gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), and/or seizures. Cases consistent with serotonin syndrome have been reported in pediatric patients after inadvertent overdose of oral ondansetron (estimated ingestion > 5 mg/kg). Symptoms reported in these cases included somnolence, agitation, tachycardia, tachypnea, hypertension, flushing, mydriasis, diaphoresis, myoclonic movements, horizontal nystagmus, hyperreflexia, and seizures. Patients required supportive care, including intubation in some cases, with complete recovery in 1—2 days.[31266] [49444]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Use with caution in individuals with known granisetron hypersensitivity, palonosetron hypersensitivity, dolasetron hypersensitivity, or sensitivity to related drugs.[31266] Cross-sensitivity is possible between these agents; there have been several reports of anaphylactic/anaphylactoid reactions associated with the use of drugs in this class.[23534][52212] Antagonism at serotonin (5-HT) receptors, and the subsequent increased concentrations of serotonin, may increase the risk of developing bronchospasm and/or vasoconstriction.[52208][52210][52211]
The use of ondansetron may mask the symptoms of adynamic ileus, GI obstruction, or gastric distention after abdominal surgery or during use to prevent chemotherapy-induced nausea and vomiting. Ondansetron is not a drug that stimulates gastric or intestinal peristalsis; it should not be used instead of nasogastric suction.[31266]
Ondansetron is extensively metabolized in the liver and should be used with caution in individuals with hepatic failure or elevated hepatic enzymes because of possible increased plasma levels, reduced clearance, and subsequent toxicity. A dosage adjustment is required for individuals with severe hepatic impairment (Child-Pugh class C).[31266] [49444]
Individuals with phenylketonuria should be informed that ondansetron orally disintegrating tablets (ODT) contain phenylalanine (a component of aspartame). Each 4 mg and 8 mg ODT contains less than 0.03 mg phenylalanine.[49444]
Avoid use of ondansetron in people with baseline QT prolongation or who have conditions that may increase the risk of QT prolongation or torsade de pointes, including bradycardia, congenital long QT syndrome, hypocalcemia, hypokalemia, hypomagnesemia, geriatric adults, females, structural abnormalities that interfere with electrical conduction (e.g., cardiomyopathy, coronary artery disease, ischemic heart disease), or in those who have other additional risk factors for QT prolongation or torsade de pointes. The use of other medications that have been associated with QT prolongation or torsade de pointes may further increase risk. Electrocardiogram (ECG) monitoring and cautious use is recommended in individuals with hypokalemia, hypomagnesemia, heart failure, significant bradycardia, or in individuals receiving other medications known to prolong the QT interval.[31266] [49444] [65180] [67452] [72115] [72116] [72117] [72118]
Data on the use of ondansetron during pregnancy from published clinical and epidemiological studies are inconsistent and have important methodological limitations, including the uncertainty of whether people who filled a prescription actually took the medicine, the concomitant use of other medications or treatments, recall bias, and other un-adjusted confounders, that do not reliably inform a drug associated risk of adverse fetal outcomes. In aggregate analysis, ondansetron exposure in utero has not been associated with major congenital malformations. Some studies have not shown a statistically significant increase in the risk of birth defects with the use of ondansetron; however, others have shown a possible increased risk of cleft palate and cardiovascular malformations.[31266] [46607] [49444] [59645] [59647] [59650] [59651] Ondansetron has been shown to cross the placenta in early pregnancy with a median fetal to maternal ratio of 0.41.[46606] Evidence is limited on the safety or efficacy of the serotonin 5HT-3 inhibitors for nausea and vomiting of pregnancy. There are more data for ondansetron use during pregnancy than with other 5HT-3 antagonists. The American College of Obstetricians and Gynecologists (ACOG) includes oral ondansetron as a third-line pharmacologic treatment option for nausea and vomiting of pregnancy in patients who are not dehydrated and have failed other therapies and IV ondansetron for patients who are dehydrated, require IV fluid replacement, and have failed other therapies. Although some studies have shown an increased risk of birth defects with early ondansetron use, other studies have not and the absolute risk to any fetus is considered, per ACOG, to be low. Some studies have suffered from small sample sizes and potential methodological bias. However, women should be counseled regarding the available data, and the use of ondansetron before 10 weeks of gestation should be individualized weighing the risks and benefits.[66066] [59650] [59651] [59647]
Ondansetron is considered compatible with breast-feeding. Small amounts are present in human milk with a relative infant dose of 1.6% to 3.7% and an estimated daily infant dose of 0.002 mg/kg/day. Ondansetron is labeled for use in infants as young as 1 month of age; infant exposure from human milk is significantly below doses for therapeutic use. No infant adverse effects have been reported with postpartum use. There is no data on the effects of ondansetron on milk production.[31266] [70364] [70365]
Ondansetron is a 5-HT3 receptor antagonist. Although other neurotransmitters are involved, serotonin plays an important role in the emetogenic pathways associated with chemotherapy- and radiation-induced nausea and vomiting. During the early or acute phase, the primary site of emetogenesis in chemotherapy-induced nausea and vomiting (CINV) is thought to be the gut wall. Chemotherapy is cytotoxic to enterochromaffin cells in the small intestine. Enterochromaffin cell death leads to serotonin release and therefore increased serotonin binding on nerve endings, leading to sensory input that contributes to emesis.[52167][52168] Peripherally, ondansetron preferentially blocks the serotonin 5-hydroxytryptamine, type 3 (5-HT3) receptors at the peripheral vagal nerve terminals in the intestines, blocking the signal transmission to the central nervous system and antagonizing the effects of serotonin. Ondansetron is also a weak antagonist of the 5-HT1B, 5-HT1C, alpha-adrenergic, and opioid mu receptors; the clinical implications of these actions is uncertain. It has no activity at dopamine receptors.[31266][52167]
Much like chemotherapy-induced nausea and vomiting (CINV), postoperative nausea and vomiting (PONV) is not controlled by a single neurotransmitter, but serotonin is believed to play a major role. The process of postoperative nausea and vomiting is coordinated by the vomiting center in the central nervous system. Stimulation can be initiated centrally in areas such as the cerebral cortex and otic or vestibular nerves, or peripherally in areas such as the oropharynx, mediastinum, gastrointestinal track, renal pelvis, peritoneum, or genitalia. Stretching and inflammation that occur during or after surgery may trigger chemical stimulation that lead to nausea and vomiting. Centrally, ondansetron blocks the 5-HT3 receptor site at the chemoreceptor trigger zone, stopping the vomiting reflex produced by the vomiting center. Because of multiple neurochemical receptor sites involved during surgery, combination antiemetic therapy with drugs of different mechanisms is often necessary.[31266][52169]
Revision Date: 09/24/2025, 01:31:00 AMOndansetron is administered orally and parenterally. It is approximately 70—76% bound to plasma protein; circulating drug also distributes into erythrocytes (approximately 36%). Animal data indicate it distributes into breast milk. Systemic exposure does not increase proportionately to the dose. Less than 5% of a dose is excreted in the urine unchanged. The mean elimination half-life in adults ranges 3.1 to 5.8 hours.[31266][49444]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4, CYP1A2, CYP2D6, CYP2C9, P-gp
Ondansetron undergoes extensive metabolism, mainly by hydroxylation, followed by glucuronide or sulfate conjugation. In vitro studies indicate that ondansetron is metabolized by hepatic cytochrome P450 (CYP450) drug-metabolizing enzymes, including CYP1A2, CYP2D6, and CYP3A4; with CYP3A4 playing the largest role. Because multiple enzymes are involved in the metabolism of ondansetron, inhibition or loss of any one enzyme may not affect the overall rate of metabolism. Additionally, it is likely that inhibition or loss of one enzyme (e.g., CYP2D6 genetic deficiency) will be compensated by others and may result in little change in overall rates of ondansetron elimination.[31266] Interactions with inhibitors or inducers of these enzymes have not been reported clinically; however, the potential exists for these interactions to change the clearance and, hence, the half-life of ondansetron. On the basis of limited available data, no dosage adjustment is recommended for patients receiving CYP-interacting drugs. Ondansetron is also a substrate of P-glycoprotein.[31266][34653] The inactive metabolites are eliminated in the urine.
Following oral administration, ondansetron is well absorbed from the gastrointestinal tract and undergoes first-pass metabolism. After a dose of a single 8-mg tablet, mean oral bioavailability in healthy adult subjects is 56%. The AUC from a 16 mg-tablet is 24% greater than predicted from an 8-mg tablet dose, indicating reduced first-pass metabolism at higher oral doses. Food slightly enhances tablet bioavailability, but antacids have no effect. Of note, 4- and 8-mg oral ondansetron tablets, orally disintegrating tablets (ODT), and oral solution are bioequivalent.[49444] After a single 8-mg dose of ondansetron oral soluble film in adult patients, peak plasma concentrations are achieved in 1.3 hours, and mean Cmax is 37.28 ng/mL and the mean AUC 225 n x h/mL. The Cmax and AUC of the oral soluble film is comparable to that of the same dose of ondansetron ODT. Water does not affect the exposure of ondansetron oral soluble film administration. Administration of the oral soluble film with a high-fat meal delays the Tmax by approximately 1 hour, but the AUC is unaffected.[41272]
In adults, a single 4-mg dose administered as a 5-minute intravenous (IV) infusion demonstrated a mean AUC of 156 ng x h/ml. Mean peak plasma concentrations were 42.9 ng/ml at 10 minutes after IV infusion.[31266]
In adult patients with mild to moderate hepatic impairment, ondansetron clearance is reduced two-fold and mean half-life is increased to 11.6 hours, compared to 3—5.7 hours in patients without hepatic impairment. In adult patients with severe hepatic impairment, clearance is reduced two-fold to three-fold and volume of distribution is increased, resulting in an increase in elimination half-life to 20 hours.[31266]
A small percentage (5%) of ondansetron is renally cleared. In patients with severe renal impairment (creatinine clearance < 30 ml/min) the mean plasma clearance is reduced by approximately 40%; however, the reduction is variable and is not consistent with an increase in half-life.[31266] A dose reduction is not necessary in this population.
In general, pediatric patients have a higher ondansetron clearance compared to adult patients, resulting in a shorter half-life; mean half-life is approximately 2.8 hours in pediatric cancer patients 4—15 years of age; patients older than 15 years exhibit pharmacokinetic parameters similar to adults. A pharmacokinetic study of postoperative children 3—12 years of age given a single dose of 2 or 4 mg IV demonstrated an elimination half-life of 2.5—3.5 hours. Another surgical study in infants and children 5—24 months receiving 0.1—0.2 mg/kg IV ondansetron as a single dose demonstrated an elimination half-life of 2.9 hours. Notably, during the same study, infants 1—4 months of age had a higher Vd (3.5 L/kg), longer half-life (6.7 hours), and slower clearance (0.401 L/kg/h) relative to older children.[31266] During a pharmacokinetic study in infants and children age 1—48 months, simulations showed that an intravenous dose of ondansetron 0.1 mg/kg in infants < 6 months produced exposure similar to a 0.15 mg/kg dose in older infants and young children.[52159]
Patients over 75 years also have a reduced clearance of ondansetron and an increased elimination half-life, however, no dosage adjustments are recommended.[31266]
Gender differences exist in the disposition of single-dose ondansetron. The extent and rate of ondansetron absorption is greater in women than men. Slower clearance in women, a smaller apparent volume of distribution (adjusted for weight), and higher absolute bioavailability resulted in higher plasma concentrations, which may in part be due to differences in body weight between men and women. It is not known if these gender-related differences are clinically important.[31266]
Data on the use of ondansetron during pregnancy from published clinical and epidemiological studies are inconsistent and have important methodological limitations, including the uncertainty of whether people who filled a prescription actually took the medicine, the concomitant use of other medications or treatments, recall bias, and other un-adjusted confounders, that do not reliably inform a drug associated risk of adverse fetal outcomes. In aggregate analysis, ondansetron exposure in utero has not been associated with major congenital malformations. Some studies have not shown a statistically significant increase in the risk of birth defects with the use of ondansetron; however, others have shown a possible increased risk of cleft palate and cardiovascular malformations.[31266] [46607] [49444] [59645] [59647] [59650] [59651] Ondansetron has been shown to cross the placenta in early pregnancy with a median fetal to maternal ratio of 0.41.[46606] Evidence is limited on the safety or efficacy of the serotonin 5HT-3 inhibitors for nausea and vomiting of pregnancy. There are more data for ondansetron use during pregnancy than with other 5HT-3 antagonists. The American College of Obstetricians and Gynecologists (ACOG) includes oral ondansetron as a third-line pharmacologic treatment option for nausea and vomiting of pregnancy in patients who are not dehydrated and have failed other therapies and IV ondansetron for patients who are dehydrated, require IV fluid replacement, and have failed other therapies. Although some studies have shown an increased risk of birth defects with early ondansetron use, other studies have not and the absolute risk to any fetus is considered, per ACOG, to be low. Some studies have suffered from small sample sizes and potential methodological bias. However, women should be counseled regarding the available data, and the use of ondansetron before 10 weeks of gestation should be individualized weighing the risks and benefits.[66066] [59650] [59651] [59647]
Ondansetron is considered compatible with breast-feeding. Small amounts are present in human milk with a relative infant dose of 1.6% to 3.7% and an estimated daily infant dose of 0.002 mg/kg/day. Ondansetron is labeled for use in infants as young as 1 month of age; infant exposure from human milk is significantly below doses for therapeutic use. No infant adverse effects have been reported with postpartum use. There is no data on the effects of ondansetron on milk production.[31266] [70364] [70365]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.