ThisiscontentfromElsevier'sDrugInformation
Drug Monograph │Oxytocin
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
0.5 to 2 milliunits/minute continuous IV infusion, initially. Titrate by 1 to 2 milliunits/minute every 15 to 60 minutes until the desired contraction pattern is established. Reduce dose similarly once the desired frequency of contractions is obtained and labor has progressed to 5 to 6 cm dilation or if uterine hyperstimulation occurs. Max: 30 milliunits/minute.[27317] [47239] [70457] Low-dose regimens and less frequent increases in dose are associated with decreased uterine hyperstimulation.[27317]
0.5 to 2 milliunits/minute continuous IV infusion, initially. Titrate by 1 to 2 milliunits/minute every 15 to 60 minutes until the desired contraction pattern is established. Reduce dose similarly once the desired frequency of contractions is obtained and labor has progressed to 5 to 6 cm dilation or if uterine hyperstimulation occurs. Max: 30 milliunits/minute.[27317] [47239] [70457] Low-dose regimens and less frequent increases in dose are associated with decreased uterine hyperstimulation.[27317]
6 milliunits/minute continuous IV infusion, initially. Titrate by 3 to 6 milliunits/minute every 15 to 60 minutes until the desired contraction pattern is established. Reduce the incremental increase if uterine hyperstimulation occurs or persistent nonreassuring findings are present on the fetal heart tracing. Max: 40 milliunits/minute.[27317] [65009]
6 milliunits/minute continuous IV infusion, initially. Titrate by 3 to 6 milliunits/minute every 15 to 60 minutes until the desired contraction pattern is established. Reduce the incremental increase if uterine hyperstimulation occurs or persistent nonreassuring findings are present on the fetal heart tracing. Max: 40 milliunits/minute.[27317] [65009]
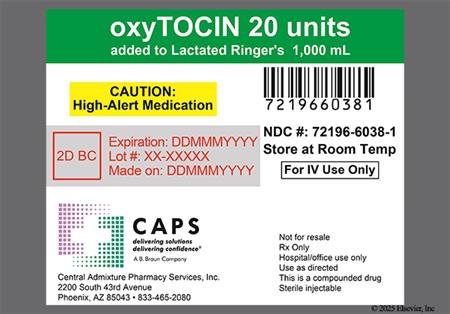
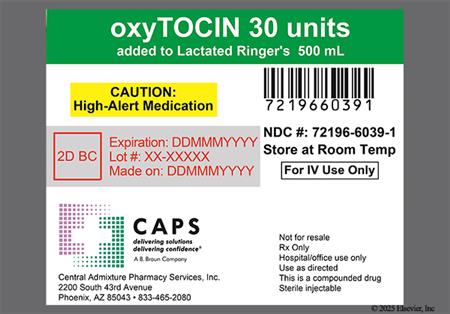
10 to 40 units in 500 to 1,000 mL of dextrose or electrolyte solution continuous IV infusion; adjust infusion rate to sustain uterine contraction and control uterine atony.[27827] [47239]
10 units IM as a single dose after delivery of the placenta.[27827] [47239]
10 to 20 milliunits/minute via continuous IV infusion. Do not exceed 30 units in a 12-hour period. Intravenous oxytocin is usually safe and effective for inducing labor for near term fetal demise, but is less effective remote from term.[27317]
Protocols may vary slightly by institution. Following baseline monitoring for 20 to 30 minutes, initiate at a low dose (e.g., 0.5 to 2.33 milliunits/minute) via continuous IV infusion to the mother. Double the infusion rate every 10 to 30 minutes until the frequency of the contractions are 3 within a 10-minute period (1 contraction every 3 to 4 minutes) and the duration is 40 to 60 seconds. When the desired number of contractions is obtained, record fetal heart rate and contractions until sufficient, then discontinue the infusion. Compare baseline and oxytocin-induced recordings.[62779] [62780]
Specific guidelines for dosage adjustments in hepatic impairment are not available; it appears that no dosage adjustments are needed.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication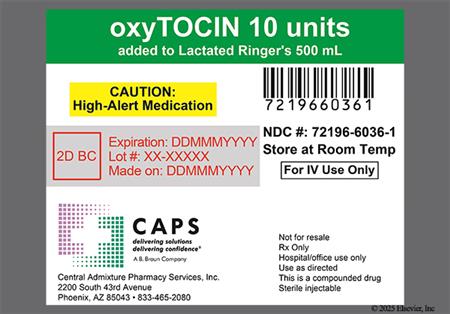



Endogenous oxytocin is a natural human hormone secreted by the supraoptic and paraventricular nuclei of the hypothalamus and stored in the posterior lobe of the pituitary. The pharmacologic and clinical properties of pharmacologic oxytocin, a synthetic agent, are identical to those of naturally occurring oxytocin. Oxytocin injection stimulates contraction of uterine smooth muscle during gestation and causes milk ejection after milk has been produced in the breast. Clinically, oxytocin is primarily used intravenously to induce labor, aid in the delivery of the placenta (third stage of labor), and control postpartum bleeding.[27317] Intranasal preparations of oxytocin, which were previously used to stimulate postpartum milk ejection, are no longer available in the U.S.
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
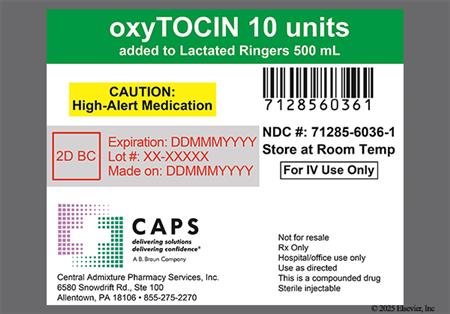
Intravenous infusion:
ISMP Safe Practice Recommendations:
Intramuscular injection:[47239]
Some patients can experience a hypersensitive uterine reaction to the effects of oxytocin. Excessive doses can have the same effect. This can produce increased, hypertonic uterine contractions, possibly prolonged, resulting in a number of adverse reactions such as cervical laceration, postpartum hemorrhage, pelvic hematoma, and uterine rupture. Maternal deaths due to subarachnoid hemorrhage and uterine rupture have been associated with the use of parenteral oxytocic drugs for induction of labor or for augmentation in the first and second stages of labor.[47239]
Cases of fatal afibrinogenemia and intracranial bleeding have been reported in women receiving oxytocin during labor. Maternal deaths due to subarachnoid hemorrhage and uterine rupture have been associated with the use of parenteral oxytocic drugs for induction of labor or for augmentation in the first and second stages of labor.[47239] In one case, subarachnoid hemorrhage mimicked acute water intoxication and delayed the diagnosis of hemorrhage after an oxytocin assisted labor.[27318] Neonatal retinal hemorrhage has also been reported.[47239]
Adverse maternal cardiovascular effects from oxytocin may include arrhythmia exacerbation, premature ventricular contractions (PVCs), and hypertension. In the fetus or neonate, fetal bradycardia, PVCs, and other arrhythmias have been noted. In addition, cases of low Apgar scores at 5 minutes after birth have also been reported. Maternal deaths due to hypertensive episodes and fetal death due to various causes have been reported associated with the use of parenteral oxytocic drugs for induction of labor or for augmentation in the first and second stages of labor.[47239]
Oxytocin has an antidiuretic effect, and severe and fatal water intoxication has been noted and may occur if large doses (40 to 50 milliunits/minute) are infused for long periods. For example, water intoxication with seizures and coma has occurred in association with a slow oxytocin infusion over a 24-hour period. Management of water intoxication includes immediate oxytocin cessation and supportive therapy. In the fetus or neonate, fetal death, permanent CNS or brain damage, and neonatal seizures have been noted with oxytocin. The rare complications of blurred vision, ocular hemorrhage (of the conjunctiva), and pulmonary edema have been associated with oxytocin induced water intoxication.[47239]
Oxytocin administration has been associated with anaphylactoid reactions.[47239]
Oxytocin-induced labor has been implicated in an increased incidence of neonatal hyperbilirubinemia, about 1.6 times more likely than after spontaneous labor. This can lead to neonatal jaundice.[47239]
Nausea and vomiting have been noted with oxytoxin.[47239]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Oxytocin is indicated during pregnancy to induce labor; it precipitates uterine contractions. There are no known indications for use of oxytocin in the first and second trimester of pregnancy other than in relation to spontaneous or induced abortion. Based on the wide experience with this drug and its chemical structure and pharmacological properties, it would not be expected to present a risk of fetal abnormalities when used as indicated.[47239] [27317]
Endogenous oxytocin is involved in the process of lactation and therefore, oxytocin has been used in mothers having difficulty with engorgement and breast-feeding. Because several small studies have failed to show a beneficial effect, oxytocin is not used for this indication. Oxytocin is excreted in the breast-milk, but is not expected to have adverse effects in the infant.[47251]
Use of oxytocin requires an experienced clinician who is trained in the administration and complications of the drug. Oxytocin use also requires a specialized care setting where intensive care and surgical facilities are immediately available. Furthermore, according to the manufacturer, oxytocin should only be used when induction of labor is necessary for medical reasons. It should not be used for elective induction of labor as available data are insufficient to evaluate the risk-benefit ratio in this indication. When oxytocin is used for induction or reinforcement of already existent labor, patients should be carefully selected. Pelvic adequacy must be considered and maternal and fetal conditions evaluated prior to initiation. The use of oxytocin is contraindicated in the following circumstances: where there is significant cephalopelvic disproportion, in unfavorable fetal positions or presentations which are undeliverable without conversion prior to delivery (i.e., transverse lies), in obstetrical emergencies where the benefit-to-risk ratio for either the fetus or the mother favors surgical intervention, in fetal distress where delivery is not imminent, where adequate uterine activity fails to achieve satisfactory progress, where the uterus is already hyperactive or hypertonic, and in cases where vaginal delivery is contraindicated (i.e., invasive cervical cancer, active herpes infection, total placenta previa, vasa previa, and cord presentation or prolapse of the cord). Except in unusual circumstances, oxytocin should be avoided when the following conditions or situations are present: evidence of fetal distress, hydramnios, fetal prematurity, abnormal fetal position (including unengaged head), partial placenta previa, borderline cephalopelvic disproportion, overdistention of the uterus, grand multiparity, any condition in which there is a predisposition for uterine rupture, such as a previous major surgery of the uterus or cervix (including cesarean section), overdistension of the uterus, past history of uterine sepsis or of traumatic delivery, or in any condition presenting as an obstetric emergency requiring surgical intervention. Due to the variability of the combinations of factors which may exist in these conditions, the definition of unusual circumstance must be left to the judgement of the physician. The decision can only be made by carefully weighing the potential benefits which oxytocin can provide in a given case against rare but definite potential for the drug to produce hypertonicity or tetanic spasm. During oxytocin administration, uterine contractions, fetal and maternal heart rate, maternal blood pressure, and, if possible, intrauterine pressure should be continuously monitored to avoid complications. Only intrauterine pressure recording can accurately measure the intrauterine pressure during contractions. A fetal scalp electrode provides a more dependable recording of the fetal heart rate than any external monitoring system. If uterine hyperactivity occurs, oxytocin administration should be immediately discontinued; oxytocin-induced stimulation of the uterine contractions usually decreases soon after discontinuance of the drug.[47239]
Oxytocin may possess antidiuretic effects, and prolonged use can increase the possibility of an antidiuretic effect. Prolonged use of oxytocin and administration in large volumes of low-sodium infusion fluids are not recommended, particularly in patients with eclampsia or who have unresponsive uterine atony. In addition, consideration should be given to the possibility of water intoxication if the patient is receiving fluids by mouth. Antidiuretic effects have the potential to lead to water intoxication and convulsive episodes due to hypertension.[47239]
Synthetic oxytocin elicits the same pharmacological response produced by endogenous oxytocin, with cervical dilation, parity, and gestational age as predictors of the dose response to oxytocin administration for labor stimulation.[27317] Oxytocin increases the sodium permeability of uterine myofibrils, indirectly stimulating contraction of the uterine smooth muscle. The uterus responds to oxytocin more readily in the presence of high estrogen concentrations and with the increased duration of pregnancy. There is a gradual increase in uterine response to oxytocin for 20 to 30 weeks gestation, followed by a plateau from 34 weeks of gestation until term, when sensitivity increases.[27317] Women who are in labor have a greater response to oxytocin compared to women who are not in labor; only very large doses will elicit contractions in early pregnancy. In the term uterus, contractions produced by exogenous oxytocin are similar to those that would occur during spontaneous labor. Oxytocin increases the amplitude and frequency of uterine contractions, which transiently impede uterine blood flow and decrease cervical activity, causing dilation and effacement of the cervix.
Oxytocin causes contraction of the myoepithelial cells surrounding the alveolar ducts of the of the breast. This forces milk from the alveolar channels into the larger sinuses, and thus facilitates milk ejection. While oxytocin possesses no galactopoietic properties, if it is absent the milk-ejection reflex in the breast fails.
Oxytocin causes dilation of vascular smooth muscle, thus increasing renal, coronary, and cerebral blood flow. Blood pressure usually remains unaffected, but with the administration of very large doses or high concentration solutions blood pressure may decrease transiently. This transient decrease in blood pressure leads to reflex tachycardia and an increase in cardiac output; any fall in blood pressure is usually followed by a small, but sustained, increase in blood pressure.
Oxytocin does possess antidiuretic effects, but they are minimal. If oxytocin is administered with an excessive volume of electrolyte-free IV solution and/or at too rapid a rate, the antidiuretic effects are more apparent and water intoxication can result.
Oxytocin appears to have important roles in sexual function and bonding responses in both males and females.[27315]
Revision Date: 09/03/2025, 05:02:23 PMOxytocin administered effectively by parenteral injection. Steady-state is usually achieved in plasma by 40 minutes after parenteral administration.[27317] Oxytocin's plasma half-life is between 1 and 6 minutes. The drug distributes throughout the extracellular fluid, with minimal amounts reaching the fetus. Oxytocinase, a glycoprotein aminopeptidase that is capable of degrading oxytocin, is produced during pregnancy and is present in the plasma. Enzyme activity increases gradually until term approaches when there is a sharp rise in plasma levels and activity is high in the plasma, placenta, and uterus. After obstetric delivery, the enzyme activity declines. Oxytocinase most likely originates from the placenta and regulates the amount of oxytocin in the uterus; there is little or no degradation of oxytocin in men, nonpregnant women, or cord blood. Oxytocin is rapidly removed from the plasma by the liver and the kidneys, with only small amounts being excreted unchanged in the urine. Oxytocin is metabolized in the lactating mammary gland and is distributed into breast-milk.
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: None
Chymotrypsin, present in the GI tract, destroys oxytocin, rendering oral administration ineffective.
When administered by IV infusion, the uterus responds almost immediately to oxytocin, with response subsiding in about an hour.
When oxytocin is administered by IM injection, the uterus responds within 3 to 5 minutes, with response subsiding in approximately 2 to 3 hours.
Oxytocin is indicated during pregnancy to induce labor; it precipitates uterine contractions. There are no known indications for use of oxytocin in the first and second trimester of pregnancy other than in relation to spontaneous or induced abortion. Based on the wide experience with this drug and its chemical structure and pharmacological properties, it would not be expected to present a risk of fetal abnormalities when used as indicated.[47239] [27317]
Endogenous oxytocin is involved in the process of lactation and therefore, oxytocin has been used in mothers having difficulty with engorgement and breast-feeding. Because several small studies have failed to show a beneficial effect, oxytocin is not used for this indication. Oxytocin is excreted in the breast-milk, but is not expected to have adverse effects in the infant.[47251]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.