ThisiscontentfromElsevier'sDrugInformation
Rucaparib
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
NOTE: Rucaparib is designated by the FDA as an orphan drug for this indication.
600 mg orally twice daily until disease progression or unacceptable toxicity. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. The investigator-assessed median progression-free survival time was significantly improved in patients with BRCA-mutated, platinum-sensitive, recurrent ovarian, primary peritoneal, or fallopian tube carcinoma who received rucaparib compared with placebo (16.6 months vs. 5.4 months; hazard ratio (HR) = 0.23; 95% CI, 0.16 to 0.34) in a subgroup analysis (n = 196) of a randomized (2:1), phase 3 (ARIEL3) trial. At the final overall survival (OS) analysis, the median OS times were 45.9 months and 47.8 months (HR = 0.83; 95% CI: 0.58 to 1.19) in patients with a BRCA-mutation who received rucaparib and placebo, respectively. The median age was 58 (range, 42 to 81) years in patients with a BRCA-mutation who received rucaparib; in these patients, all had received at least 2 (range, 2 to 5) previous platinum-based chemotherapy regimens and 22% of patients had received prior bevacizumab therapy.[61608]
Dosage not available.
600 mg PO twice daily until disease progression or unacceptable toxicity. Patients should concurrently receive treatment with a gonadotropin-releasing hormone (GnRH) analog or have had a bilateral orchiectomy. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions. Treatment with rucaparib resulted in a confirmed objective response rate of 44% in patients with BRCA-mutated metastatic CRPC who had been treated with androgen receptor-directed therapy and taxane-based chemotherapy in an ongoing multicenter, noncomparative trial. The median duration of response was not evaluable.[61608]
Recommended Monitoring
Dosage Adjustments for Treatment-Related Toxicities
Hematologic Toxicity
600 mg PO twice daily.[61608]
600 mg PO twice daily.[61608]
Baseline Hepatic Impairment:
Baseline Renal Impairment:
Rucaparib is an oral poly (ADP-ribose) polymerase (PARP) inhibitor. It is indicated for the maintenance treatment of BRCA-mutated recurrent ovarian cancer after a response to platinum-based chemotherapy and for the treatment of BRCA-mutated metastatic castration-resistant prostate cancer in patients previously treated with androgen receptor-directed therapy and taxane-based chemotherapy. PARP enzymes are involved in normal cellular homeostasis, including DNA transcription, cell cycle regulation, and DNA repair; increased cytotoxicity and anti-tumor activity has been noted in cell lines and mouse tumor models with deficiencies in BRCA. The most common grade 3 or 4 adverse reactions occurring in more than 10% of patients included anemia, asthenia/fatigue, increased ALT, and neutropenia.[61608]
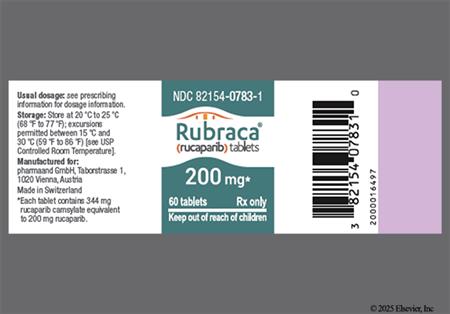
For storage information, see the specific product information within the How Supplied section.
Emetic Risk
New primary malignancy, including acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS), occurred in 32 of 1,594 patients (2%) with ovarian cancer treated with rucaparib, after a duration of therapy ranging from less than 2 months to about 72 months. These cases were typical of cancer therapy-related MDS/AML; all patients had received prior treatment with platinum-containing chemotherapy and other DNA damaging agents. Fourteen cases (0.9%) occurred during treatment or during the 28-day safety follow-up. MDS/AML was not observed in patients with metastatic castration-resistant prostate cancer (n = 209), regardless of homologous recombination deficiency (HRD) mutation. Monitor complete blood counts (CBC) prior to starting therapy and monthly thereafter. Rucaparib should not be started until any prior hematologic toxicity resolves to grade 1 or lower. If recovery to grade 1 or less has not occurred within 4 weeks, the patient should be referred to a hematologist for further investigations including a bone marrow analysis and cytogenetics. Rucaparib should be discontinued if a diagnosis of MDS or AML is confirmed.[61608]
Neutropenia occurred in 22% of patients who received rucaparib maintenance therapy for platinum-sensitive BRCA-mutated recurrent ovarian cancer compared with 6% of those who received placebo (grade 3 or 4, 8% vs. 0%). A decrease from baseline in leukocytes (leukopenia) (39% to 69%; grade 3 or 4, 3% to 5%), neutrophils (neutropenia) (38% to 62%; grade 3 or 4, 6% to 10%), and lymphocytes (lymphopenia) (33% to 42%; grade 3 or 4, 7% to 17%) were also reported in these patients and in patients with BRCA-mutated metastatic, castration-resistant prostate cancer in a nonrandomized trial.[61608]
Constipation occurred in 27% to 39% (grade 3 or 4, 1% to 4%) and diarrhea in 20% to 34% (grade 3 or 4, 2% or less) of patients treated with rucaparib in clinical trials.[61608]
Fatigue/asthenia occurred in 74% of patients receiving rucaparib maintenance therapy for platinum-sensitive BRCA-mutated recurrent ovarian cancer compared with 52% of those who received placebo (grade 3 or 4, 9% vs. 5%) in a randomized clinical trial and was among the most common adverse reactions leading to dose reductions. Fatigue/asthenia was also reported in 62% (grade 3 or 4, 9%) of patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a noncomparative trial.[61608]
Mild dysgeusia (33% vs. 6%) occurred more often in patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated recurrent ovarian cancer compared with placebo in a randomized, double-blind clinical trial. The incidence of dysgeusia was lower in a noncomparative trial of patients with BRCA-mutated, metastatic castration-resistant prostate cancer (less than 20%).[61608]
Anorexia occurred more often in patients receiving maintenance therapy with rucaparib for BRCA-mutated, recurrent, platinum-sensitive ovarian cancer compared with placebo in a randomized, double-blind clinical trial (23% vs. 14%; grade 3 or 4, 2% vs. 0%). It was also reported in 28% (grade 3 or 4, 2%) of rucaparib-treated patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a nonrandomized trial.[61608]
Dyspnea occurred in 17% of patients receiving rucaparib as maintenance therapy for BRCA-mutated ovarian cancer in a randomized clinical trial; it was also reported in less than 20% of patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a noncomparative trial.[61608]
Rash occurred in 45% of patients receiving rucaparib maintenance therapy for platinum-sensitive BRCA-mutated ovarian cancer compared with 23% of those who received placebo in a randomized, double-blind clinical trial. Rash also occurred in 27% (grade 3 or 4, 2%) of patients with BRCA-mutated, metastatic castration-resistant prostate cancer, including blisters, blood blisters, contact dermatitis, eczema, genital rash, palmar-plantar erythrodysesthesia (hand and foot syndrome), photosensitivity, pruritus, psoriasis, maculopapular rash, exfoliative dermatitis, and urticaria.[61608]
Naso-pharyngitis/upper respiratory tract infection occurred more often in patients receiving maintenance therapy with rucaparib for platinum-sensitive, BRCA-mutated recurrent ovarian cancer compared with placebo in a randomized, double-blind clinical trial (29% vs. 20%; grade 3 or 4, 0% vs. 2%); fever was reported in 15% of patients. Urinary tract infection, pneumonia, and sepsis were each reported in less than 20% of rucaparib-treated patients with BRCA-mutated metastatic castration-resistant prostate cancer in a noncomparative trial. Pneumonia, sepsis, and urinary tract infection were reported in less than 20% of patients.[61608]
Elevated hepatic enzymes have been reported in patients treated with rucaparib in clinical trials. Increased AST/ALT levels were reported in 33% of patients receiving rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated ovarian cancer in a randomized, double-blind clinical trial compared with 3% of those who received placebo (grade 3 or 4, 16% vs. 0%); increased ALT/AST levels were reported in 33% of rucaparib-treated patients with BRCA-mutated metastatic prostate cancer (grade 3 or 4, 5%). Compared to baseline, an increase in AST/ALT levels occurred in 59% to 69% (grade 3 or 4, 1% to 11%) and an increase in alkaline phosphatase level occurred in 39% to 44% (grade 3 or 4, 2% or less) of patients in these trials.[61608]
An increase in cholesterol level (hypercholesterolemia) from baseline occurred in 39% (grade 3 or 4, 3%) of patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated recurrent ovarian cancer in a randomized, double-blind clinical trial compared with 20% of those who received placebo. An increase in triglycerides from baseline (e.g., hypertriglyceridemia) was reported in 42% of rucaparib-treated patients with BRCA-mutated prostate cancer in a noncomparative trial.[61608]
An increase in serum creatinine level from baseline occurred in 96% of patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated recurrent ovarian cancer receiving in a randomized, double-blind clinical trial compared with 89% of those who received placebo; in rare cases, renal failure (unspecified) occurred. Renal failure was reported in less than 20% of rucaparib-treated patients with BRCA-mutated, metastatic prostate cancer, while an increase in creatinine occurred in 43% of these patients (grade 3 or 4, 2%).[61608]
A hypersensitivity reaction including flushing, asthma, chocking sensation, eyelid edema, facial edema, and wheezing, was reported in less than 20% of rucaparib-treated patients with BRCA-mutated, metastatic castration-resistant prostate cancer.[61608]
Headache occurred in 22% and dizziness in 15% of patients receiving rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated ovarian cancer in a randomized, double-blind clinical trial. Dizziness was also reported in less than 20% of patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a separate noncomparative trial.[61608]
Nausea was reported in 79% (grade 3 or 4, 2%) of patients receiving rucaparib as maintenance therapy for BRCA-mutated ovarian cancer in a randomized clinical trial; vomiting occurred in 37% (grade 3 or 4, 4%) of these patients. The incidence of nausea (52%; grade 3 or 4, 3%) and vomiting (22%; grade 3 or 4, 1%) was slightly lower in rucaparib-treated patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a noncomparative trial.[61608]
Abdominal pain/distention was less common in patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated recurrent ovarian cancer compared with placebo in a randomized, double-blind clinical trial (48% vs. 49%; grade 3 or 4, 3% vs. 2%).[61608]
Stomatitis occurred more often in patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated recurrent ovarian cancer compared with placebo in a randomized, double-blind clinical trial (28% vs. 12%; grade 3 or 4, 0.8% vs. 0%). Stomatitis was reported in less than 20% of rucaparib-treated patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a noncomparative trial.[61608]
Dyspepsia was reported in 12% of patients receiving maintenance therapy with rucaparib after a response to platinum-containing chemotherapy for BRCA-mutated, recurrent ovarian cancer in a randomized, double-blind clinical trial. It was also reported in less than 20% of patients with BRCA-mutated, metastatic castration-resistant prostate cancer treated with rucaparib in a noncomparative trial.[61608]
Anemia occurred in 41% of patients who received rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated recurrent ovarian cancer compared with 6% of those who received placebo (grade 3 or 4, 26% vs. 0%); it was also reported in 43% (grade 3 or 4, 25%) of patients with BRCA-mutated metastatic, castration-resistant prostate cancer in a nonrandomized trial. Additionally, a decrease in hemoglobin level from baseline was reported in 59% to 61% (grade 3 or 4, 18% to 25%) of those who received rucaparib.[61608]
Thrombocytopenia occurred in 35% of patients who received rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated recurrent ovarian cancer compared with 3% of those who received placebo (grade 3 or 4, 6% vs. 0%); it was also reported in 25% (grade 3 or 4, 10%) of patients with BRCA-mutated metastatic, castration-resistant prostate cancer in a nonrandomized trial. Additionally, a decrease in platelets from baseline was reported in 40% to 47% (grade 3 or 4, 2% to 10%) of those who received rucaparib.[61608]
Bleeding was reported in less than 20% of rucaparib-treated patients with BRCA-mutated, metastatic castration-resistant prostate cancer in a noncomparative trial.[61608]
A decrease in serum phosphate levels from baseline (hypophosphatemia) occurred in 68% of rucaparib-treated patients with BRCA-mutated metastatic prostate cancer in a nonrandomized trial (grade 3 or 4, 15%); a decrease in sodium from baseline (hyponatremia) was reported in 38% of these patients (grade 3 or 4, 3%).[61608]
Venous thromboembolism and ischemic cardiovascular events were each reported in less than 20% of patients with BRCA-mutated, metastatic castration-resistant prostate cancer treated with rucaparib in a nonrandomized trial.[61608]
Insomnia (19%) and depression (11%) were reported in patients who received rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated recurrent ovarian cancer in a randomized clinical trial.[61608]
Peripheral edema was reported in 12% of patients who received rucaparib maintenance therapy for platinum-sensitive, BRCA-mutated recurrent ovarian cancer in a randomized clinical trial.[61608]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Do not start therapy with rucaparib until patients have recovered from any bone marrow suppression caused by previous chemotherapy (to grade 1 or less). Monitor complete blood counts at baseline and monthly thereafter. An interruption of therapy and/or dose reduction or discontinuation of therapy may be necessary if hematologic toxicity occurs. If therapy is interrupted and hematologic toxicities do not recover to grade 1 or less within 4 weeks, discontinue rucaparib treatment and refer the patient to a hematologist for further evaluation, including bone marrow analysis and blood sample for cytogenetics.[61608]
Rucaparib can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. There are no available data of rucaparib use during human pregnancy to inform a drug-associated risk. Administration of rucaparib to pregnant rats during organogenesis resulted in embryo-fetal death in all animals at exposures equal to 0.04 times the AUC expected at recommended human doses.[61608]
Counsel people who may become pregnant and people who can cause pregnancy in others about the reproductive risk associated with rucaparib. Rucaparib may cause fetal harm. Verify pregnancy status prior to treatment initiation. Advise people who may become pregnant to use effective contraception while taking rucaparib and for 6 months after the last dose. Rucaparib can cause male-mediated teratogenicity. For those that can cause pregnancy in others, contraception should be used during rucaparib treatment and for 3 months after the last dose. Counsel patients to abstain from sperm donation during rucaparib therapy and for 3 months after the last dose.[61608]
Advise patients to avoid breast-feeding while taking rucaparib and for 2 weeks after the last dose. There are no data on the presence of rucaparib in human milk, its effects on the breast-fed child, or its effects on milk production.[61608]
Rucaparib inhibits poly (ADP-ribose) polymerase (PARP) enzymes, including PARP1, PARP2, and PARP3. PARP enzymes are involved in normal cellular homeostasis, such as DNA transcription, cell cycle regulation, and DNA repair. In vitro, inhibition of PARP enzyme activity by rucaparib results in increased PARP-DNA complexes, causing DNA damage, apoptosis, and cell death. Increased cytotoxicity has been observed with rucaparib exposure in tumor cell lines with deficiencies in BRCA 1/2 and other DNA repair genes. In mouse xenograft models of human cancer with or without BRCA deficiencies, rucaparib has been shown to decrease tumor growth.[61608]
Revision Date: 09/16/2025, 01:32:00 AMRucaparib is administered orally. In vitro, rucaparib is 70% protein bound in human plasma. It is preferentially distributed to red blood cells with a blood-to-plasma concentration ratio of 1.8. The mean apparent volume of distribution is 2,300 liters (CV, 21%). The mean terminal half-life of rucaparib is 26 hours (CV, 39%). The mean apparent clearance at steady-state is 44.2 L/hour (CV, 45%). After administration of a single radiolabeled dose, unchanged rucaparib accounted for 64% of the radioactivity in plasma. Rucaparib accounted for 45% of radioactivity in the urine and 95% of radioactivity in the feces.[61608]
Affected cytochrome P450 isoenzymes (CYP450) or drug transporters: CYP1A2, CYP2C9, CYP2C19, CYP3A4
In vitro, rucaparib is primarily metabolized by CYP2D6 and to a lesser extent by CYP1A2 and CYP3A4. Additionally, N-demethylation, N-methylation, and glucuronidation are involved in rucaparib metabolism. In vitro, rucaparib is a substrate of P-glycoprotein (P-gp) and BCRP. In clinical studies, rucaparib is a moderate CYP1A2 inhibitor as well as a weak inhibitor of CYP2C9, CYP2C19, CYP3A4, and P-gp. In vitro, rucaparib inhibited CYP2C8, CYP2D6, UGT1A1, OATP1B1, OATP1B3, OAT1, OAT3, MATE1, MATE2K, OCT1, OCT2, and MRP4; it induced CYP1A2.[61608]
The exposure-response relationship and time course of pharmacodynamic response for the safety and effectiveness of rucaparib has not been fully characterized. The mean steady-state Cmax of rucaparib at the approved recommended dosing was 1,940 ng/mL (CV, 54%), reached at a Tmax of 1.9 hours (range, 0 to 5.98 hours). The AUC was 16,900 ng x hour/mL (CV, 54%), and the mean AUC accumulation ratio was 3.5-fold to 6.2-fold. Mean absolute bioavailability is 36% (range, 30% to 45%). The pharmacokinetics (AUC and Cmax) of rucaparib were linear from a dose of 240 mg to 840 mg twice daily.[61608]
A high-fat meal (approximately 800 to 1,000 calories; 250 calories from carbohydrates, 500 to 600 calories from fat, and 150 calories from protein) increased the Cmax by 20% and the AUC by 38%, while the Tmax was delayed by 2.5 hours as compared to fasting conditions.[61608]
Mild hepatic impairment (total bilirubin less than the upper limit of normal [ULN] and AST greater than ULN; or total bilirubin 1.1 to 1.5 times ULN and any AST) did not have a clinically meaningful effect on the pharmacokinetics of rucaparib. Moderate hepatic impairment (total bilirubin 1.6 to 3 times ULN and any AST) increased the AUC of rucaparib by 45% but had no effect on Cmax compared to patients with normal hepatic function. The effect of severe hepatic impairment (total bilirubin greater than 3 times ULN and any AST) has not been studied.[61608]
Mild to moderate renal impairment (CrCl 30 mL/min or higher) did not have a clinically meaningful effect on the pharmacokinetics of rucaparib. The effect of severe renal impairment (CrCl 15 to 29 mL/min) or end-stage renal disease (CrCl less than 15 mL/min) has not been studied.[61608]
The safety and efficacy of rucaparib has not been established in pediatric patients.[61608]
Age (20 to 86 years) does not have a clinically meaningful effect on the pharmacokinetics of rucaparib.[61608]
Sex does not have a clinically meaningful effect on the pharmacokinetics of rucaparib.[61608]
Race (White, Black, and Asian) does not have a clinically meaningful effect on the pharmacokinetics of rucaparib.[61608]
Body weight (41 to 171 kg) does not have a clinically meaningful effect on the pharmacokinetics of rucaparib.[61608]
Pharmacogenomics
CYP2D6 or CYP1A2 genotype polymorphisms did not have a clinically meaningful effect on the pharmacokinetics of rucaparib.[61608]
Rucaparib can cause fetal harm or death when administered during pregnancy based on its mechanism of action and animal studies. There are no available data of rucaparib use during human pregnancy to inform a drug-associated risk. Administration of rucaparib to pregnant rats during organogenesis resulted in embryo-fetal death in all animals at exposures equal to 0.04 times the AUC expected at recommended human doses.[61608]
Advise patients to avoid breast-feeding while taking rucaparib and for 2 weeks after the last dose. There are no data on the presence of rucaparib in human milk, its effects on the breast-fed child, or its effects on milk production.[61608]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.