ThisiscontentfromElsevier'sDrugInformation
Sarilumab
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
400 mg IV once. The National Institutes of Health (NIH) COVID-19 treatment guidelines recommend sarilumab in combination with dexamethasone (with or without remdesivir) to treat hospitalized adults requiring supplemental oxygen, IF the individual is exhibiting signs of systemic inflammation and rapidly increasing oxygen needs while on dexamethasone. Further, sarilumab may be given with dexamethasone to treat people on high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO. Sarilumab is to be used as an alternative when other immunomodulators are not available or not feasible to administer.[65314]
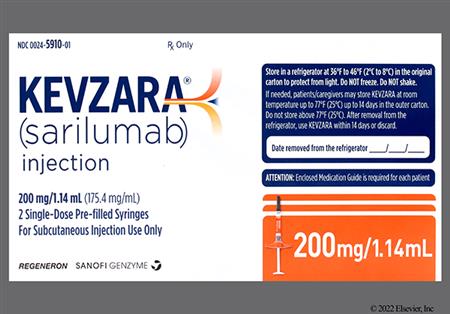
200 mg subcutaneously every 2 weeks as monotherapy or in combination with methotrexate or other conventional DMARDs (cDMARDs). Do not use with other biological DMARDs because of the possibility of increased immunosuppression and increased risk of infection; such combinations have not been studied.[61976]
200 mg subcutaneously every 2 weeks as monotherapy after discontinuation of corticosteroid therapy or in combination with a tapering course of systemic corticosteroids.[61976]
200 mg subcutaneously every 2 weeks as monotherapy or in combination with conventional DMARDs (cDMARDs). Do not use with other biological DMARDs because of the possibility of increased immunosuppression and increased risk of infection; such combinations have not been studied.[61976]
Prior to initiation of treatment
During treatment
Dosage modifications in patients with rheumatoid arthritis (RA) for neutropenia, thrombocytopenia, elevated liver enzymes, or infection
Dosage modifications in patients with polymyalgia rheumatica (PMR) for neutropenia, thrombocytopenia, elevated liver enzymes, or infection
Dosage modifications in patients with polyarticular juvenile idiopathic arthritis (pJIA) for neutropenia, thrombocytopenia, elevated liver enzymes, or infection
200 mg per dose subcutaneously; investigational doses of 400 mg IV have been used for COVID-19.
200 mg per dose subcutaneously; investigational doses of 400 mg IV have been used for COVID-19.
weighing 63 kg or more: 200 mg per dose subcutaneously.
weighing less than 63 kg: Safety and efficacy have not been established.
2 to 12 years weighing 63 kg or more: 200 mg per dose subcutaneously.
2 to 12 years weighing less than 63 kg: Safety and efficacy have not been established.
1 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Prior to treatment initiation: Do not initiate treatment with sarilumab if baseline AST or ALT is more than 1.5-times the upper limit of normal (ULN).
-Hepatic enzyme elevations occurring during treatment for rheumatoid arthritis (RA):
AST or ALT up to 3-times the ULN: Dose modify concomitant DMARDs, if appropriate.
AST or ALT 3- to 5-times the ULN: Interrupt sarilumab dosing until AST/ALT is less than 3 times the ULN. Then, resume sarilumab at 150 mg subcutaneously every 2 weeks, and then increase to 200 mg subcutaneously every 2 weeks as clinically appropriate.
AST or ALT more than 5-times the ULN: Discontinue sarilumab.
-Hepatic enzyme elevations occurring during treatment for polymyalgia rheumatica (PMR):
AST or ALT 3-times ULN or more: Discontinue sarilumab.
-Hepatic enzyme elevations occurring during treatment for polyarticular juvenile idiopathic arthritis (pJIA):
ALT 3- to 5-times the ULN: Hold sarilumab dosing until the clinical condition has been evaluated. The decision to discontinue sarilumab should be based upon a medical assessment of the individual patient. If appropriate, the dose of concurrently administered medications should be modified or discontinued.
ALT more than 5-times the ULN: Discontinue sarilumab.[61976]
CrCl 30 mL/minute or more: No dosage adjustment needed.
CrCl less than 30 mL/minute: Sarilumab has not been studied in patients with severe renal impairment.[61976]
† Off-label indication
Sarilumab is an injectable interleukin-6 (IL-6) receptor antagonist. It is indicated for the treatment of adults with moderate to severe rheumatoid arthritis (RA) who have had an inadequate response or intolerance to 1 or more disease-modifying antirheumatic drugs (DMARDs) and for the treatment of active polyarticular juvenile idiopathic arthritis (pJIA) in pediatric patients 2 years and older weighing at least 63 kg. Sarilumab is also approved to treat adults with polymyalgia rheumatica (PMR) who have had an inadequate response to corticosteroids or who cannot tolerate corticosteroid taper. Prior to initiating treatment, obtain a complete blood count (CBC), liver function test (LFT), and serum lipid profile. Additionally, evaluate the patient for tuberculosis (active and latent infections) and any other active infection. The prescribing label contains a boxed warning regarding an increased risk for developing serious infections with sarilumab therapy. Sarilumab was initially FDA-approved in 2017.[61976]
Updates for coronavirus disease 2019 (COVID-19):
According to the National Institutes of Health (NIH) COVID-19 treatment guidelines, sarilumab may be used as an alternative to other immunomodulators for the treatment of COVID-19 in hospitalized patients:
Sarilumab must be given in combination with dexamethasone (with or without remdesivir), and is only recommended for use when other immunomodulators are unavailable or cannot be administered. For the treatment of COVID-19, sarilumab must be administered as an intravenous infusion; the dose is obtained by diluting the commercially available subcutaneous formulation with 0.9% Sodium Chloride for Injection.[65314]
For storage information, see the specific product information within the How Supplied section.
COVID-19 per the National Institutes of Health (NIH) treatment guidelines:
NOTE: Sarilumab is not approved by the FDA for intravenous administration.
Prefilled Syringe:
Prefilled Pen:
Patients treated with sarilumab are at increased risk of developing a serious infection, including bacterial or viral infections or reactivation of viral infections, that may lead to hospitalization or death. Opportunistic infections have also been reported in patients receiving sarilumab. Most patients who developed an infection were taking concomitant immunosuppressants such as methotrexate or corticosteroids. During and after treatment with sarilumab, closely monitor all patients for the development of signs and symptoms of infection including the possible development of tuberculosis (TB) in patients who tested negative for latent TB infection before sarilumab use. If a serious infection develops, interrupt sarilumab until the infection is controlled. Infections of various types have been reported during clinical trials. During the rheumatoid arthritis placebo-controlled clinical trials of sarilumab plus conventional DMARD, upper respiratory tract infections were reported in 3% and 4% of patients receiving sarilumab 200 mg and 150 mg, respectively (2% placebo). Urinary tract infections were reported in 3% of both sarilumab treatment groups (2% placebo). Naso-pharyngitis was also reported. The rate of serious infections in the 200 mg and 150 mg group was 3.8 to 4.3 and 3 to 4.4 events per 100 patient-years, respectively, compared to 2.5 to 3.1 events per 100 patient-years for placebo. Serious infections reported included pneumonia, cellulitis, and opportunistic infections. Viral reactivation has been reported with the use of immunosuppressive biologic therapies. Herpes zoster was reported in 0.8% and 0.6% of those receiving sarilumab 200 mg and 150 mg, respectively (0.5% placebo). Oral herpes simplex infection occurred in less than 2% of rheumatoid arthritis patients who received sarilumab in clinical trials. In the polymyalgia rheumatica placebo-controlled clinical trial, 3 patients who received sarilumab 200 mg discontinued treatment due to an infection (COVID-19, intervertebral discitis, and pneumonia). However, the overall infection rate was lower in the sarilumab group (37.3%) than in the placebo group (50%), and the rate of serious infections was similar (5.1% vs. 5.2%). Herpes zoster was noted in 2 patients who received sarilumab (3.2%) and 1 patient in the placebo group (1.7%). In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), the rate of infections was 146.6 events per 100 patient-years. The most common infections observed were naso-pharyngitis (36.6%) and upper respiratory tract infections (14%). No cases of hepatitis B reactivation were observed in the trials; however, patients who screened positive for hepatitis were excluded from clinical trials. Among opportunistic infections, TB (pulmonary or extrapulmonary disease), candidiasis, and Pneumocystosis infections were reported with sarilumab. Patients have presented with disseminated rather than localized disease and were often taking concomitant immunosuppressants such as methotrexate or corticosteroids. Carefully consider the risks and benefits of sarilumab in patients with chronic or recurrent infection.[61976]
Gastrointestinal perforation has been reported during sarilumab clinical trials. Reports of GI perforation were primarily noted as complications of diverticulitis including lower GI perforation and abscesses. One patient experienced a GI perforation during sarilumab clinical trials for rheumatoid arthritis (0.11 events per 100 patient-years). In the long-term safety population, the overall rate of GI perforation was consistent with rates of the controlled periods of the studies. Most patients that developed GI perforations were taking concomitant nonsteroidal anti-inflammatory medications (NSAIDs) or corticosteroids. The contribution of these concomitant medications to the development of GI perforations is not known. In the polymyalgia rheumatica clinical trial, 6.8% of drug recipients experienced constipation.[61976]
Sarilumab may cause neutropenia; neutrophil counts should be assessed before and during treatment. During the rheumatoid arthritis placebo-controlled clinical trials of sarilumab plus conventional DMARD, neutropenia was reported in 10% of those who received sarilumab 200 mg and 7% of those who received sarilumab 150 mg. Decreases in absolute neutrophil counts to less than 1,000/mm3 occurred in 6% and 4% of the patients in the sarilumab 200 mg and 150 mg groups, respectively (0% placebo). Severe decreases in neutrophil counts to less than 500/mm3 were reported in 0.7% of both sarilumab treatment groups. Neutropenia was not associated with the occurrence of infections, including serious infections. In the polymyalgia rheumatica clinical trial, 15.3% of adults treated with sarilumab 200 mg developed neutropenia, and 3 patients (5.1%) required permanent treatment discontinuation because of neutropenia. Two patients (3.4%) developed neutrophil counts less than 500/mm3 without any infections. In both cases, the neutrophil counts resolved once sarilumab therapy was stopped. In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), 19.2% of patients weight 30 kg or more and 48.8% of patients weighing between 10 and 29 kg developed absolute neutrophil counts (ANC) less than 1,000/mm3. These decreases in ANC were not associated with the occurrence of infections, including serious infections; however, neutropenia was the most common adverse reaction that resulted in permanent discontinuation of therapy (5.4%). Leukopenia has also been reported. In the rheumatoid arthritis trial, leukopenia was reported in 0.9% of patients receiving sarilumab 150 mg and 2% of patients receiving the 200 mg dose. Leukopenia was also reported in the polymyalgia rheumatica clinical trial, occurring in 6.8% of drug recipients. A decrease in monocyte counts occurred in 4 (4.3%) pJIA patients, which were mild in severity and non-serious.[61976]
Sarilumab may cause thrombocytopenia; platelet counts should be assessed before and during treatment. During the rheumatoid arthritis placebo-controlled clinical trials of sarilumab plus conventional DMARD, decreases in platelet counts to less than 100,000/mm3 occurred in 1% and 0.7% of those receiving sarilumab 200 mg and 150 mg, respectively (0% placebo). In the polymyalgia rheumatica clinical trial, decreases in platelet counts between 75,000 and 100,000/mm3 occurred in 2 patients (3.4%) who received sarilumab 200 mg, compared to no patient in the placebo group. Treatment-related reductions in platelet counts were not associated with bleeding events in clinical trials.[61976]
Sarilumab is associated with elevated hepatic enzymes. Liver function tests should be assessed before and during sarilumab treatment. In those experiencing elevated liver enzymes, modification of the treatment regimen (i.e., dose reduction or interruption) usually results in a decrease or normalization of the liver enzyme. During the rheumatoid arthritis placebo-controlled clinical trials of sarilumab plus conventional DMARD, an AST greater than the upper limit of normal (ULN) to 3-times ULN or less were reported in 30% of patients receiving sarilumab 200 mg and 27% of those receiving 150 mg compared to 15% of those receiving placebo. AST elevations of more than 3-times the ULN to 5-times the ULN were reported in 1% (0% for placebo), and AST more than 5-times ULN were reported in 0.2% to 0.7% (0% for placebo) of those receiving any dose of sarilumab. Similarly, ALT more than the ULN up to 3-times ULN were reported in 43% of patients receiving sarilumab 200 mg and 38% of those receiving 150 mg vs. 25% of those receiving placebo. ALT elevations of more than 3-times the ULN to 5-times the ULN were reported in 3% to 4% of those receiving any dose of sarilumab (1% for placebo), and ALT greater than 5-times ULN were reported in 0.7% to 1% of those receiving sarilumab (0% for placebo). These increases in liver enzymes were not associated with clinically relevant increases in direct bilirubin or evidence of hepatitis or hepatic impairment. In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), 9 (9.7%) patients had increases in ALT. These included 1 (1.1%) patient with an ALT more than 3-times the ULN to 5-times the ULN, and 2 (2.2%) patients with ALT more than 5-times the ULN to 10-times the ULN which resulted in permanent treatment discontinuation; all patients recovered. In the polymyalgia rheumatica clinical trial, no patient receiving sarilumab 200 mg per dose experienced an ALT or AST greater than 3-times the ULN.[61976]
An injection site reaction may occur with the use of sarilumab. In the rheumatoid arthritis clinical trials, injection site reactions were reported in 7% and 6% of those who received sarilumab 200 mg and sarilumab 150 mg, respectively. Injection site reactions included pruritus (2%) and erythema (4% to 5%). Mild injection site pruritis was also noted in 3 patients (5.1%) who received sarilumab 200 mg during the polymyalgia rheumatica clinical trial. In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), injection site reactions occurred in 13 (14%) patients and the most commonly reported reaction was injection site erythema (9.7%). Most of these events were mild in severity and none of the injection site reactions required treatment withdrawal or dose interruption.[61976]
Hypersensitivity reactions have been reported with the administration of sarilumab. In the rheumatoid arthritis clinical trials, reactions that required treatment discontinuation were reported in 0.2 to 0.3% of patients. Injection site rash, rash (unspecified), and urticaria were reported most frequently. In the polymyalgia rheumatica clinical trial, pruritic rash (5.1%) was among the most common adverse reactions. Advise patients to seek medical attention if they experience any symptoms of a hypersensitivity reaction. If anaphylactoid reactions or other hypersensitivity reaction occurs, immediately stop the administration of sarilumab.[61976]
Sarilumab may cause hyperlipidemia, including hypercholesterolemia and hypertriglyceridemia. Assess lipid parameters during sarilumab treatment and manage patients according to clinical guidelines [e.g., National Cholesterol Educational Program (NCEP)] for the management of hyperlipidemia. During the rheumatoid arthritis placebo-controlled trials of sarilumab plus conventional DMARD, lipid parameters were measured 4 weeks following sarilumab initiation. Among those receiving sarilumab 150 mg, the mean LDL cholesterol increased by 12 mg/dL, mean triglycerides increased by 20 mg/dL, and mean HDL increased by 3 mg/dL. Among those receiving sarilumab 200 mg, the mean LDL increased by 16 mg/dL, mean triglycerides increased by 27 mg/dL, and mean HDL increased by 3 mg/dL. In the long-term safety population, the observations in lipid parameters were consistent with what was observed in the rheumatoid arthritis trials. In the polymyalgia rheumatica clinical trial, cholesterol levels of 299.27 mg/dL or greater were observed in 8 patients (13.8%) who received 200 mg sarilumab compared to 4 patients (6.9%) in the placebo group. Triglyceride levels of at least 407.4 mg/dL were observed in 3 sarilumab patients (5.2%) and 1 placebo patient (1.7%). At treatment Week 52, mean increases from baseline for LDL and triglycerides were observed in the sarilumab group, though both remained within the normal range. There was no difference in mean HDL levels between sarilumab and placebo. In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), triglyceride levels of at least 150 mg/dL (1-time ULN) were observed in 1 (1.1%) patient. Three (3.2%) patients overall had mildly elevated triglyceride levels that were non-serious. No significant changes in mean LDL, HDL, or total cholesterol were observed during the entire 156-week treatment period.[61976]
In the polymyalgia rheumatica clinical trial, myalgia (6.8%) and fatigue (5.1%) were among the most common adverse reactions in PMR patients who received treatment with sarilumab 200 mg.[61976]
In rheumatoid arthritis patients treated with sarilumab monotherapy, 9.2% of patients exhibited an anti-drug antibody (ADA) response with 6.9% of patients also exhibiting neutralizing antibodies (NAbs). Prior to the administration of sarilumab, 2.3% of patients exhibited an ADA response. In the pre-rescue population, 4% of patients treated with sarilumab 200 mg plus DMARD and 5.7% of patients treated with sarilumab 150 mg plus DMARD exhibited an ADA response, compared with 1.9% of patients receiving placebo plus DMARD. Neutralizing antibodies were detected in 1% of patients on sarilumab 200 mg plus DMARD and 1.6% of patients on sarilumab 150 mg plus DMARD (versus 0.2% of patients on placebo plus DMARD). No correlation was observed between antibody formation and adverse events or loss of efficacy. In the polymyalgia rheumatica population, 1 patient (1.8%) who received sarilumab 200 mg plus 14-week corticosteroid taper exhibited an ADA response, compared with no patient in the placebo plus 52-week corticosteroid taper group. Neutralizing antibodies were detected in the sarilumab recipient, and that patient did not demonstrate a clinical response. In pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis (pJIA), 3 (4.3%) patients who received sarilumab 200 mg per dose exhibited an ADA response. Neutralizing antibodies were detected in 1 of the 3 patients with an ADA response. Due to the low occurrence of ADA in polymyalgia rheumatica and pJIA patients, the effect of these antibodies on safety and effectiveness of sarilumab in these populations is unknown.[61976]
Sarilumab may increase the risk for a new primary malignancy. In the 52-week placebo-controlled trial, 9 malignancies (exposure-adjusted event rate of 1 event per 100 patient-years) were reported in patients receiving sarilumab and a DMARD compared to 4 malignancies (exposure-adjusted event rate of 1 event per 100 patient-years) in the control group. In the long-term safety population, the rate of malignancies was consistent with the rate observed in the placebo-controlled period.[61976]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Update immunizations in agreement with current immunization guidelines prior to initiating sarilumab therapy. Avoid concurrent use of live vaccines and sarilumab due to the potential for increased risk of infection. The interval between live vaccinations and initiation of sarilumab should be in accordance with current vaccination guidelines. No data are available on the secondary transmission of infection from persons receiving live vaccines to patients receiving sarilumab.[61976]
Treatment with sarilumab increases the risk of a serious infection that may lead to hospitalization or death. Avoid use in people with an active infection, including localized infections. Use sarilumab with caution in patients at increased risk for infections, including geriatric adults (65 years and older) and those with chronic or recurrent infections, a history of serious or opportunistic infections, underlying conditions that may predispose to infection, and those receiving concomitant immunosuppressants (e.g., corticosteroids, methotrexate). Patients residing in or with travel history to regions where mycoses are endemic (e.g., Ohio and Mississippi River valleys, Southwest) are at increased risk for invasive fungal infections. Viral reactivation (herpes zoster) has occurred with sarilumab treatment; however, it is unknown if sarilumab increases the risk of hepatitis B reactivation. Sarilumab also increases the risk of tuberculosis (TB) infection. Screen all patients for active and latent TB infection prior to starting sarilumab. If positive for active TB, do not give sarilumab. If positive for latent TB, treat with standard antimycobacterial therapy before starting sarilumab. Consider anti-tuberculosis therapy in patients with a history of latent or active TB in whom an adequate course of treatment cannot be confirmed, and in those with risk factors for TB infection. Consult a physician with expertise in treating TB about whether starting anti-tuberculosis therapy is appropriate for the individual patient. Monitor for signs and symptoms of TB and other infections during therapy, even in patients who tested negative for latent TB prior to initiation. For patients who develop an infection during treatment with sarilumab, perform a prompt and complete diagnostic workup appropriate for immunocompromised patients and initiate appropriate antimicrobial therapy. If a patient develops a serious or opportunistic infection, interrupt treatment with sarilumab until the infection is controlled.[61976]
Initiation of sarilumab therapy is not recommended in people with thrombocytopenia defined as a platelet count less than 150,000/mm3 or with neutropenia defined as an absolute neutrophil count (ANC) below 2,000/mm3. Thrombocytopenia and neutropenia have occurred with sarilumab, and drug interruption, dose reduction, or discontinuation may be needed, depending on the platelet counts or ANC. Assess platelet count and ANC in all treated patients at 4 to 8 weeks after sarilumab initiation and every 3 months thereafter.[61976]
Use sarilumab with caution in people with a history of diverticulitis. Gastrointestinal perforations have been reported in patients receiving sarilumab, primarily as complications of diverticulitis. The risk for GI perforation may be increased in patients with concurrent diverticulitis or those receiving concomitant nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids. Promptly evaluate treated patients presenting with new onset abdominal symptoms.[61976]
Sarilumab is not recommended in people with active hepatic disease or hepatic impairment, as treatment with sarilumab has been associated with transaminase elevations. Assess liver function tests (LFTs) before and during treatment with sarilumab. Avoid starting sarilumab in patients who have ALT or AST more than 1.5-times the upper limit of normal (ULN).[61976]
Available data on the use of sarilumab during pregnancy are insufficient to evaluate a drug-associated risk of major birth defects, miscarriage, or other adverse outcomes. Monoclonal antibodies, like sarilumab, are increasingly transported across the placenta as pregnancy progresses, with the largest amount transferred during the third trimester. In an animal reproduction study, consisting of a combined embryo-fetal and pre- and postnatal development study with monkeys that received intravenous sarilumab, there was no evidence of embryotoxicity or fetal malformations with exposures up to approximately 84 times the maximum recommended human dose (MRHD). Animal data suggest sarilumab may affect labor and obstetric delivery. Inhibition of IL-6 signaling may interfere with cervical ripening and dilatation and myometrial contractile activity, leading to potential delays in parturition. For mice deficient in IL-6, parturition was delayed compared to wild-type mice without IL-6 deficiency. Administration of recombinant IL-6 to the deficient mice restored the normal timing of delivery.[61976]
Consider the risks and benefits prior to administering live or live-attenuated vaccines to neonates and infants exposed to this medication in utero. Sarilumab is an immunomodulatory agent. Monoclonal antibodies, like sarilumab, are increasingly transported across the placenta as pregnancy progresses, with the largest amount transferred during the third trimester. Based on its mechanism of action and animal data, concentrations of immunoglobulin G (IgG), in response to antigen challenge, may be reduced in neonates and infants exposed to sarilumab in utero.[61976]
Use sarilumab with caution during breast-feeding. There is no information available on the presence of sarilumab in human milk, its effects on the breastfed child, or its effect on milk production. Maternal immunoglobulin G (IgG) is present in human milk. The effects of local sarilumab exposure on the gastrointestinal tract or from limited systemic exposure to the breast-fed child are unknown. Consider the benefits of breast-feeding, the patient's clinical need for treatment, and any potential adverse effects on the breast-fed child from the medication or from the patient's underlying medical condition.[61976]
Sarilumab binds to both soluble and membrane-bound interleukin-6 (IL-6) receptors (sIL-6R and mIL-6R), and has been shown to inhibit IL-6-mediated signaling through these receptors. IL-6 is a pleiotropic pro-inflammatory cytokine produced by a variety of cell types including T-cells and B-cells, lymphocytes, monocytes, and fibroblasts. IL-6 has been shown to be involved in diverse physiological processes such as T-cell activation, induction of immunoglobulin secretion, initiation of hepatic acute phase protein synthesis, and stimulation of hematopoietic precursor cell proliferation and differentiation. IL-6 is also produced by synovial and endothelial cells leading to local production of IL-6 in joints affected by inflammatory processes such as rheumatoid arthritis.[61976]
Revision Date: 07/28/2025, 10:24:58 AMSarilumab is administered subcutaneously. The volume of distribution at steady state is 7.3 L. Sarilumab is eliminated by parallel linear and non-linear pathways. At higher concentrations, the elimination is predominately through the linear, non-saturable proteolytic pathway. At lower concentrations, non-linear saturable target-mediated elimination predominates. The half-life is concentration-dependent. At steady-state following administration of 150 mg or 200 mg subcutaneously every 2 weeks, the half-life is up to 8 or 10 days, respectively. After the last steady-state dose of 150 mg and 200 mg, the median times to non-detectable concentration are 28 and 43 days, respectively. Sarilumab is expected to be degraded into small peptides and amino acids via catabolic pathways, similar to endogenous IgG. Monoclonal antibodies are not eliminated via renal or hepatic pathways.[61976]
Decreases in C-reactive protein to within normal ranges were seen as early as week 2 after single-dose administration of sarilumab 150 mg or 200 mg during trials in adult patients with rheumatoid arthritis. Treatment with sarilumab resulted in decreases in serum amyloid A and fibrinogen and increases in hemoglobin and serum albumin. Decreases in C-reactive protein and erythrocyte sedimentation rate (ESR) were also observed in pediatric patients with polyarticular juvenile idiopathic arthritis after sarilumab administration.[61976]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: various CYP450 isoenzymes
The formation of CYP450 enzymes may be suppressed by increased concentrations of cytokines, such as IL-6, during chronic inflammation. Thus, it is expected that the formation of CYP450 enzymes could be normalized during sarilumab receipt leading to increased metabolism of drugs that are CYP450 substrates. Exercise caution when coadministering sarilumab with CYP3A4 substrate drugs where a decrease in effectiveness is undesirable. The effect of sarilumab on CYP450 enzyme activity may persist for several weeks after stopping the medication.[61976]
When administered subcutaneously to rheumatoid arthritis patients, the time to maximum concentration (Tmax) was 2 to 4 days. At steady state, the exposure (AUC) increased 2-fold with an increase in dose from 150 mg to 200 mg every 2 weeks. Steady-state was reached in 14 to 16 weeks with a 2- to 3-fold accumulation compared to single-dose exposure. For the 150 mg every 2 week regimen, the estimated mean (+/- SD) steady-state AUC was 202 +/- 120 mg x day/L, the minimum concentration (Cmin) was 6.35 +/- 7.54 mg/L, and the maximal concentration (Cmax) was 20 +/- 9.2 mg/L. For the 200 mg every 2 week regimen, the estimated mean (+/- SD) steady-state AUC, Cmin, and Cmax were 395 +/- 207 mg x day/L, 16.5 +/- 14.1 mg/L, and 35.6 +/- 15.2 mg/L, respectively. Data from a population pharmacokinetic analysis of 58 patients found sarilumab exposures were generally higher in those with polymyalgia rheumatica as compared to those with rheumatoid arthritis. For the dosing regimen of 200 mg every 2 weeks, the estimated mean (+/- SD) steady-state AUC, Cmin, and Cmax in polymyalgia rheumatica patients were 551 +/- 321 mg x day/L, 27 +/-21.5 mg/L, and 46.5 +/- 23 mg/L, respectively. Accumulation was observed, with an accumulation ratio of approximately 6-fold based on the mean trough concentrations.[61976]
Mild (CrCl 60 to 90 mL/minute) and moderate (CrCl 30 to 60 mL/minute) renal impairment does affect the exposure of sarilumab; however, the effect is not sufficient enough to warrant dose adjustment. Patients with severe renal impairment have not been studied.[61976]
The pharmacokinetics of sarilumab were evaluated in 101 pediatric patients (2 to 17 years) with polyarticular juvenile idiopathic arthritis. In patients weighing 30 kg or more who received doses of 3 mg/kg every 2 weeks, the estimated mean steady-state AUC, Cmin, and Cmax of sarilumab were 276 +/- 121 mg x day/L, 9.57 +/- 5.84 mg/L, and 27.1 +/- 11.6 mg/L, respectively. In patients weighing 10 to 29 kg who received 4 mg/kg every 2 weeks, the estimated mean steady-state AUC, Cmin, and Cmax of sarilumab were 395 +/- 101 mg x day/L, 14.4 +/- 9.81 mg/L, and 40.4 +/- 7.77 mg/L, respectively. Steady-state was achieved in 12 to 28 weeks with a 2 to 4-fold accumulation as compared to single dose exposures for 3 and 4 mg/kg every 2 weeks. Steady-state concentrations were within the range of exposures in adult rheumatoid arthritis (RA) patients who received 150 to 200 mg every 2 weeks.[61976]
Age does not affect the pharmacokinetic profile of sarilumab.[61976]
Gender does not affect the pharmacokinetic profile of sarilumab.[61976]
Race does not affect the pharmacokinetic profile of sarilumab.[61976]
Although body weight influenced the pharmacokinetics of sarilumab, no dose adjustments are recommended.[61976]
Available data on the use of sarilumab during pregnancy are insufficient to evaluate a drug-associated risk of major birth defects, miscarriage, or other adverse outcomes. Monoclonal antibodies, like sarilumab, are increasingly transported across the placenta as pregnancy progresses, with the largest amount transferred during the third trimester. In an animal reproduction study, consisting of a combined embryo-fetal and pre- and postnatal development study with monkeys that received intravenous sarilumab, there was no evidence of embryotoxicity or fetal malformations with exposures up to approximately 84 times the maximum recommended human dose (MRHD). Animal data suggest sarilumab may affect labor and obstetric delivery. Inhibition of IL-6 signaling may interfere with cervical ripening and dilatation and myometrial contractile activity, leading to potential delays in parturition. For mice deficient in IL-6, parturition was delayed compared to wild-type mice without IL-6 deficiency. Administration of recombinant IL-6 to the deficient mice restored the normal timing of delivery.[61976]
Use sarilumab with caution during breast-feeding. There is no information available on the presence of sarilumab in human milk, its effects on the breastfed child, or its effect on milk production. Maternal immunoglobulin G (IgG) is present in human milk. The effects of local sarilumab exposure on the gastrointestinal tract or from limited systemic exposure to the breast-fed child are unknown. Consider the benefits of breast-feeding, the patient's clinical need for treatment, and any potential adverse effects on the breast-fed child from the medication or from the patient's underlying medical condition.[61976]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.