Tetralogy of Fallot, Adult
Tetralogy of Fallot is a combination of four heart defects that are present at birth (congenital). This condition develops early in pregnancy, while a baby's heart is developing. When you have tetralogy of Fallot, some blood does not reach the lungs for oxygen, and blood that enters the heart mixes with blood that is leaving the heart. This makes it difficult for the body to get enough oxygen-rich blood.
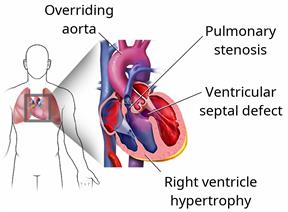
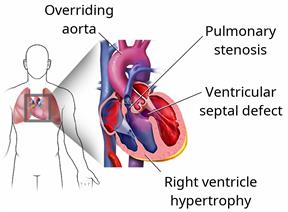
There are four defects that make up this condition:
Ventricular septal defect. This is a hole in the wall between the two lower chambers of the heart (ventricles). The hole allows blood with oxygen to mix with blood without oxygen.
Pulmonary stenosis. This is a condition in which the valve between the right ventricle and the artery that leads to the lungs (pulmonary artery) is too narrow. Pulmonary stenosis results in less blood moving to the lungs than is normal.
Right ventricular hypertrophy. This is an enlargement and thickening of the right ventricle. It occurs because the heart has to work harder than normal to move blood through the pulmonary artery.
Overriding aorta. Normally, the aorta is attached to the left ventricle. In an overriding aorta, it is located between the ventricles and over the ventricular septal defect. An overriding aorta allows the oxygen-poor blood from the right ventricle to travel to the rest of the body.
What are the causes?
The cause of this condition is not known. In some cases, it may be caused by genes that are passed from parent to child (inherited).
What are the signs or symptoms?
In adults, symptoms of this condition may include:
Low energy or tiredness.
Inability to exercise.
Abnormal heart rate. The heart rate may be too fast or too slow.
Abnormal heart rhythm.
A feeling that the heart is fluttering.
Dizziness or fainting.
Shortness of breath or cough.
How is this diagnosed?
This condition may be diagnosed based on:
You may also have other tests, including:
A Holter monitor or event monitor test. You will wear a device that monitors your heart rate as you go about your daily activities.
A pulse oximetry to check the amount of oxygen in your blood.
Cardiac catheterization. A soft tube (catheter) is used to measure pressure inside of the heart.
How is this treated?
You will see a heart specialist (
cardiologist) to manage this condition. Treatment depends on how well your heart is functioning and what changes are likely to develop in the future. Possible treatments include:
- Medicines. Medicines can:
Control your blood pressure and heart rate.
Thin your blood to prevent blood clots in your heart.
Help the body get rid of excess fluids.
- Help prevent infection of the inner layer of the heart or the heart valves. This condition is called endocarditis.
An electrical device that helps to regulate your heart rhythm (pacemaker or cardioverter defibrillator).
Surgery to repair or replace a leaky heart valve.
Surgery to close the hole in the heart.
A heart transplant, if heart failure begins to develop. This is rare.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.