Thalassemia
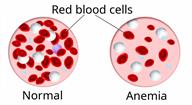
Thalassemia is a blood disorder that causes a low level of red blood cells (anemia). This condition is passed from parent to child (inherited) through gene mutations. These are abnormal changes to genes. The mutations make it hard for a person's body to make the protein in red blood cells (hemoglobin) that carries oxygen from the lungs to the rest of the body. Red blood cells do not live long without hemoglobin. Loss of red blood cells leads to anemia, which is the main symptom of thalassemia.
There are two main types of thalassemia. The type depends on which part of the hemoglobin is affected.
Alpha thalassemia affects the alpha part of the hemoglobin. This is caused by four genes. You could get two from each parent.
Beta thalassemia affects the beta part of the hemoglobin. This is caused by two genes. You could get one from each parent.
Thalassemia is a lifelong condition. There is no cure, but treatment can control symptoms and manage the condition.
What are the causes?
Thalassemia is caused by gene mutations that are passed down through families. This condition ranges from mild to severe. People born with more gene mutations have more severe forms of the condition.
A person who inherits just one gene will be a carrier of the condition (thalassemia trait). A person with thalassemia trait may not have any symptoms or may have only mild anemia.
A person who inherits two or more genes can have thalassemia minor, thalassemia intermedia, or thalassemia major.
What increases the risk?
You are more likely to develop this condition if you have a family history of thalassemia. Also:
You are at higher risk for alpha thalassemia if your ancestors are from Africa, Central America, the Middle East, or the Mediterranean region.
You are at higher risk for beta thalassemia if your ancestors are from Africa, Southeast Asia, India, or the Mediterranean region.
What are the signs or symptoms?
The most common signs and symptoms of thalassemia are the signs and symptoms of anemia. They include:
Weakness or tiredness.
Pounding heartbeat.
Dizziness or headache.
Leg cramps.
Pale skin.
Feeling confused.
Shortness of breath.
Other symptoms may include:
Skin or the white parts of your eyes turn yellow (jaundice), and dark urine. The breakdown of red blood cells can cause a yellowing pigment (bilirubin) to build up in your blood.
Weak bones (osteoporosis) and bone breaks. Bones can weaken from the effort of making more hemoglobin.
An enlarged spleen. This can lead to a swollen belly. Your spleen can become enlarged from filtering dead red blood cells.
Frequent, severe infections. These occur if your spleen and bone marrow become weak. These organs make white blood cells that your body needs to fight infections.
How is this diagnosed?
Your health care provider may suspect thalassemia based on your signs and symptoms, especially if you have a family history of the condition. This condition may be diagnosed:
In childhood, if you have a severe form of thalassemia. With severe forms, symptoms show early in life.
At birth. In the U.S., babies are screened for this condition.
In adulthood, if you have thalassemia trait or thalassemia minor. These may be diagnosed if symptoms of anemia start or if a routine blood test shows unexplained anemia.
Blood tests can confirm a thalassemia diagnosis. Blood tests may show:
You may need to see a health care provider who specializes in blood diseases (hematologist).
How is this treated?
Treatment for this condition depends on the type of thalassemia that you have.
If you have thalassemia trait or thalassemia minor, you may not need treatment. But you may need treatment if you have thalassemia minor and you develop symptoms of it during an infection.
If you have thalassemia intermedia, you will have symptoms that require treatment.
If you have thalassemia major, you will have serious symptoms that require regular treatment.
Thalassemia treatment may include:
Donated blood (transfusions) to replace red blood cells.
Vitamin B (folic acid) supplements to help produce hemoglobin and red blood cells.
Calcium and vitamin D supplements to help prevent osteoporosis.
Medicines or injections to remove iron buildup (chelation). Iron buildup can happen in people who have transfusions often. Iron overload can damage cells of the heart, liver, and brain.
If you have severe thalassemia:
Your spleen may need to be removed if it becomes damaged.
You may need stem cell or bone marrow transplants to transplant cells that can make red blood cells. These may be done if transfusions are not working.
Follow these instructions at home:
Eating and drinking

-
Follow instructions from your health care provider about eating or drinking restrictions. You may need to avoid foods or drinks that are high in iron or that have iron added to them (are fortified).
-
Eat foods that are high in fiber, such as beans, whole grains, and fresh fruits and vegetables. Limit foods that are high in fat and processed sugars, such as fried or sweet foods. Good nutrition can help prevent anemia.
Activity
-
Return to your normal activities as told by your health care provider. Ask your health care provider what activities are safe for you.
-
Exercise is needed for maintaining energy and strong bones. Ask your health care provider what amount and type of exercise is safe for you.
General instructions

-
Take over-the-counter and prescription medicines only as told by your health care provider.
-
Keep all routine vaccinations and flu shots up to date to reduce your risk of infection.
-
Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use hand sanitizer.
-
Try to avoid sick people, and stay out of crowds during cold and flu seasons.
-
Do not use any products that contain nicotine or tobacco. These products include cigarettes, chewing tobacco, and vaping devices, such as e-cigarettes. If you need help quitting, ask your health care provider.
-
Do not drink alcohol.
-
Meet with a genetic counselor if you are or may become pregnant. A genetic counselor can explain the risks of passing thalassemia to a child.
-
Keep all follow-up visits. This is important.
Contact a health care provider if you have:
Summary
-
Thalassemia is a blood disorder that causes anemia.
-
This condition is passed down through families.
-
Thalassemia can range from mild to severe.
-
There is no cure, but treatment can help manage symptoms and prevent anemia.
This information is not intended to replace advice given to you by your health care provider. Make sure you discuss any questions you have with your health care provider.