ThisiscontentfromElsevier'sDrugInformation
Ticagrelor
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
General dosing information
Switching from another P2Y12 inhibitor to ticagrelor:
Switching from ticagrelor to another P2Y12 inhibitor:
180 mg PO loading dose, then 90 mg PO twice daily in combination with low-dose aspirin. Reduce dose to 60 mg PO twice daily in combination with low-dose aspirin after 1 year. Initiate ticagrelor with a daily maintenance dose of aspirin 75 mg to 100 mg PO once daily. However, in persons who have undergone a percutaneous coronary intervention, consider single antiplatelet therapy with ticagrelor based on the evolving risk of thrombosis versus bleeding events.[44951]
60 mg PO twice daily in combination with low-dose aspirin.[44951]
180 mg PO loading dose, then 90 mg PO twice daily plus aspirin for up to 30 days.[44951]
180 mg/day PO after an initial 180 mg load for acute coronary syndrome; 120 mg/day PO for coronary artery disease.
180 mg/day PO after an initial 180 mg load for acute coronary syndrome; 120 mg/day PO for coronary artery disease.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Mild hepatic impairment: No dose adjustment needed.
Moderate hepatic impairment: Use with caution; carefully weigh the risks versus the benefits of treatment, considering the probable increase in exposure to ticagrelor.
Severe hepatic impairment: Use is contraindicated.
Specific guidelines for dosage adjustments in renal impairment are not available; it appears that no dosage adjustments are needed.
† Off-label indication




Ticagrelor is an oral platelet P2Y12 adenosine-5'-diphosphate (ADP) receptor antagonist that inhibits platelet aggregation. Ticagrelor is indicated to reduce the rate of thrombotic cardiovascular events in patients with acute coronary syndrome (ACS) (unstable angina, non-ST elevation myocardial infarction, or ST-elevation myocardial infarction); to reduce the risk of first myocardial infarction or stroke in patients with coronary artery disease at high risk for these events, such as patients with type 2 diabetes; and to reduce the risk of stroke in patients with acute ischemic stroke (NIH stroke scale score 5 or less) or high-risk transient ischemic attack (TIA). In the PLATO study, ticagrelor was shown to reduce the rate of a combined endpoint of cardiovascular death, myocardial infarction, or stroke compared to clopidogrel in patients with ACS.[44951] The efficacy and safety of ticagrelor and clopidogrel were found to be similar in a meta-analysis of ACS clinical studies; however, ticagrelor had a higher incidence of dyspnea.[66096] In the THEMIS study that compared the safety and efficacy of ticagrelor plus aspirin versus placebo plus aspirin in patients with stable coronary artery disease and type 2 diabetes mellitus, the incidence of the composite primary efficacy outcome of cardiovascular death, myocardial infarction, or stroke was lower in the ticagrelor plus aspirin group (7%) than in the placebo plus aspirin group (8.5%) (hazard ratio 0.9; 95% CI, 0.81 to 0.99; p = 0.04). The incidence of major bleeding and intracranial bleeding was higher in the ticagrelor group at 2.2% and 0.7%, respectively, compared to 1% and 0.5%, respectively, in the placebo group.[66098] The THALES study enrolled patients with mild to moderate acute noncardioembolic ischemic stroke (NIH stroke scales score 5 or less) or transient ischemic attack to compare the effect of ticagrelor plus aspirin to aspirin on the prevention of stroke or death. Dual therapy with ticagrelor plus aspirin was associated with a reduced risk of the composite end point of stroke and death (5.4%) compared to aspirin (6.5%) (p = 0.02), but there was no difference in the incidence of disability (23.8% versus 24.1%). The incidence of ischemic stroke was also lower with ticagrelor plus aspirin versus aspirin, 5% and 6.2%, respectively (p = 0.004). The incidence of severe bleeding was higher in the ticagrelor plus aspirin group compared to the aspirin group, 0.5% versus 0.1% (p = 0.001).[66099] Ticagrelor has also been found to reduce the risk of stent thrombosis in patients with stents for ACS.[44951] Unlike clopidogrel, ticagrelor does not require hepatic activation to an active form and does not have irreversible effects on platelets.
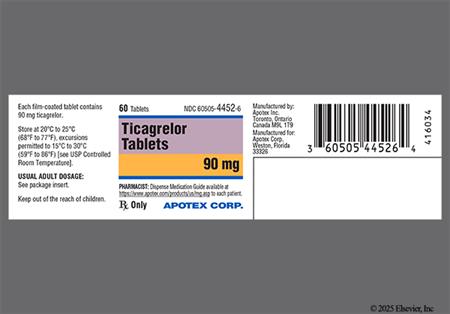
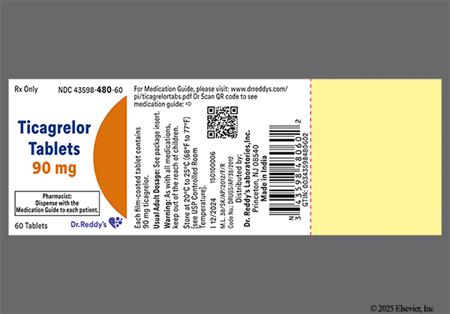
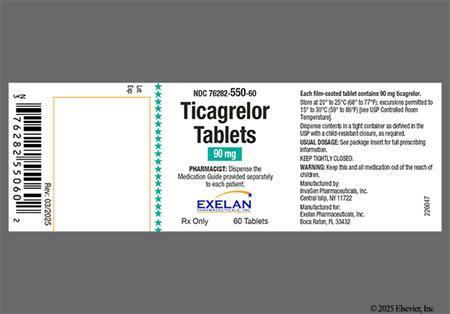
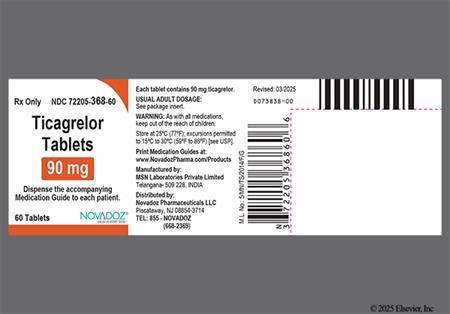
For storage information, see the specific product information within the How Supplied section.
Ticagrelor increases the risk of bleeding and can cause significant, sometimes fatal bleeding. In the PLATO trial, major bleeding events occurred mostly early, at the time of angiography, PCI, CABG, and other procedures, but the risk does persist during later use of antiplatelet therapy. Patients receiving ticagrelor plus aspirin had a greater risk of non-CABG major and minor bleeding compared to patients receiving clopidogrel plus aspirin (7.7% vs. 6.2%, respectively). Additionally, rates of major bleeding were 3.9% for ticagrelor vs. 3.3% for clopidogrel; fatal bleeding occurred in 0.2% of patients in both groups, and intracranial bleeding occurred in 0.3% of patients receiving ticagrelor vs. 0.2% of patients receiving clopidogrel. It should be noted that no baseline demographic factor altered the relative risk of bleeding with ticagrelor compared to clopidogrel. In addition, the rates of total major bleeds in patients who underwent CABG surgery were very high and similar between patients receiving ticagrelor plus aspirin (81.3%) and patients receiving clopidogrel plus aspirin (81.8%). Fatal and life-threatening bleeding rates in patients receiving ticagrelor who underwent CABG surgery were not increased. Bleeding caused permanent discontinuation of study drug in 2.3% of ticagrelor patients and 1% of clopidogrel patients. In the THEMIS study, there were 9 TIMI major bleeding events per 1,000 patient-years with ticagrelor compared to 4 events per 1,000 patient-years in patients receiving placebo. The rate of TIMI major or minor bleeding events, or those requiring medical attention was 46 events per 1,000 patient-years with ticagrelor compared to 18 events per 1,000 patient-years with placebo. In the THALES study, intracranial bleeding occurred in 21 ticagrelor patients and 6 placebo patients. Eleven patients receiving ticagrelor therapy and 2 receiving placebo experienced fatal bleeding events; majority were intracranial bleeding. In order to decrease the risk of bleeding, discontinue ticagrelor 5 days prior to surgery. Bleeding should be suspected in any patient who is hypotensive and has recently undergone coronary angiography, PCI, CABG, or other surgical procedures, even if the patient does not have any signs of bleeding. If possible, manage any bleeding episode without discontinuing ticagrelor as stopping the drug increases the risk of subsequent cardiovascular events. Platelet transfusion did not reverse the antiplatelet effect of ticagrelor in healthy volunteers and is not likely to be of benefit in patients with bleeding.[44951]
Dyspnea has been reported during ticagrelor treatment. If a patient develops worsening, prolonged, or newly reported dyspnea during ticagrelor therapy, exclude underlying diseases that may cause dyspnea and require treatment. There is no treatment for dyspnea caused by ticagrelor. If dyspnea is determined to be caused by ticagrelor, continue treatment without interruption if possible. Discontinuation or interruption of ticagrelor therapy will increase the risk of myocardial infarction, stent thrombosis, and death. If the dyspnea becomes intolerable and ticagrelor discontinuation is needed, consider starting another antiplatelet agent. During the PLATO trial, dyspnea was reported in 13.8% compared to 7.8% of those receiving clopidogrel. The reported dyspnea was usually mild to moderate in intensity and most often resolved with continued ticagrelor treatment. Dyspnea led to study discontinuation in 0.9% of patients receiving ticagrelor compared to 0.1% receiving clopidogrel. Dyspnea was reported in 14.2% and 21% of patients treated with ticagrelor in the PEGASUS and THEMIS trials, respectively, and led to drug discontinuation in 4.3% and 6.9%, respectively, of patients. Further analysis from PLATO indicates there were no adverse effects on pulmonary function (FEV1) after 1 month or at least 6 months of chronic treatment. Central sleep apnea and Cheyne-Stokes respiration have been reported with postmarketing use of ticagrelor. Recurrence or worsening of central sleep apnea or Cheyne-Stokes respiration has also been reported following ticagrelor rechallenge. If central sleep apnea is suspected, consider further clinical challenge.[44951] In addition, cough was reported in 4.9% of patients receiving ticagrelor in the PLATO trial compared to 4.6% of those receiving clopidogrel.[65498]
Cardiovascular adverse events have been reported with ticagrelor therapy. During the PLATO trial, hypertension was reported in 3.8% of patients receiving ticagrelor (vs. 4% clopidogrel) and hypotension was reported in 3.2% of ticagrelor-treated patients (vs. 3.3% clopidogrel). Chest pain (unspecified) was reported in 3.1% of patients taking ticagrelor (vs. 3.5% clopidogrel) and non-cardiac chest pain was reported in 3.7% of patients treated with ticagrelor (vs. 3.3% clopidogrel). Atrial fibrillation occurred more often in patients receiving clopidogrel compared to ticagrelor (4.6% vs. 4.2%). During clinical studies, ticagrelor was associated with an increase in the occurrence of Holter-detected bradyarrhythmias (including ventricular pauses); PLATO excluded patients at risk for bradycardia and associated events (e.g., sick sinus syndrome, second or third degree AV block, bradycardia-related syncope not protected with a pacemaker). During the PLATO trial, syncope, pre-syncope, and loss of consciousness were reported in 1.7% of patients receiving ticagrelor compared to 1.5% in the clopidogrel group. Furthermore, in a substudy of approximately 3,000 patients in PLATO, 6% of patients receiving ticagrelor experienced ventricular pauses compared to 3.5% receiving clopidogrel in the acute phase. After 1 month, ventricular pauses were reported in 2.2% in the ticagrelor group and 1.6% in the clopidogrel group.[44951]
Headache and dizziness have been reported with ticagrelor therapy. During the PLATO trial, headache was reported in 6.5% of patients receiving ticagrelor (vs. 5.8% clopidogrel), and dizziness was reported in 4.5% of those in the ticagrelor group (vs. 3.9% clopidogrel).[44591]
Gastrointestinal effects have been reported with ticagrelor therapy. During the PLATO trial, nausea was reported in 4.3% of patients receiving ticagrelor (vs. 3.8% clopidogrel) and diarrhea was reported in 3.7% of patients in the ticagrelor group (vs. 3.3%).[44951]
During the PLATO trial, fatigue was reported in 3.2% of patients receiving ticagrelor and clopidogrel. Back pain was reported in 3.6% of those receiving ticagrelor compared to 3.3% of those in the clopidogrel group.[44951]
Gynecomastia was reported in 0.23% of men receiving ticagrelor during the PLATO trial compared to 0.05% of men receiving clopidogrel. Other sex-hormonal adverse reactions did not differ between treatment groups.[44951]
Hyperuricemia was reported during the PLATO trial; however, reports of gout did not differ between treatment groups (0.6% for each group). Serum uric acid concentrations increased approximately 0.6 mg/dl above baseline for those receiving ticagrelor and increased 0.2 mg/dl for those receiving clopidogrel. Hyperuricemia normalized within 30 days of discontinuing treatment.[44951]
Hypersensitivity reactions including angioedema and rash (unspecified) have been reported during post-marketing use of ticagrelor.[44951]
Thrombotic thrombocytopenic purpura (TTP) has been reported rarely in patients receiving ticagrelor and may occur following a short exposure (less than 2 weeks). A 31-year old man developed TTP following 5 weeks of ticagrelor therapy, ticagrelor was discontinued and he experienced clinical TTP remission following steroid treatment and 5 plasma exchange treatments. An 87-year old man developed TTP following 2 months of ticagrelor therapy. Ticagrelor was temporarily held and intravenous immunoglobulin administered along with plasma exchange and other supportive therapies. Ticagrelor was restarted 6 days later and the patient developed worsening TTP-related symptoms after 3 days of therapy; thus, ticagrelor was again discontinued. The patient subsequently passed away a few days after ticagrelor was stopped the second time. TTP is a serious condition that can be fatal and requires urgent treatment.[44951] [64708] [64709]
Ticagrelor is contraindicated in patients with hypersensitivity (e.g., angioedema) to ticagrelor or any component of the product. Hypersensitivity reactions including angioedema have been reported.[44951]
Ticagrelor is contraindicated in any patient with active pathological bleeding including peptic ulcer (GI bleeding) or intracranial bleeding. Patients with acute ischemic stroke or transient ischemic attacks (TIAs) and an NIH stroke scale score greater than 5, as well as, patients receiving thrombolysis were excluded from the THALES study; thus, ticagrelor is not recommended in these patients. Like other antiplatelet agents, ticagrelor can cause significant, sometimes fatal, bleeding. The risk of bleeding may be increased in older patients, patients with a history of bleeding disorders, performance of percutaneous invasive procedures, and concomitant use of medications that increase the risk of bleeding (e.g., anticoagulant and fibrinolytic therapy, higher doses of aspirin, and chronic nonsteroidal anti-inflammatory drugs [NSAIDS]). In order to decrease the risk of bleeding, discontinue ticagrelor at least 5 days prior to any surgery, particularly in those with a high risk of bleeding, when possible; ticagrelor may be resumed once hemostasis achieved. Do not start ticagrelor in patients planned to undergo urgent coronary artery bypass graft surgery (CABG). Bleeding should be suspected in any patient who is hypotensive and has recently undergone coronary angiography, percutaneous coronary intervention (PCI), CABG, or other surgical procedures in the setting of ticagrelor. Since there is an increased risk of subsequent cardiovascular events associated with discontinuation of ticagrelor, if possible, manage bleeding without stopping ticagrelor. Platelet transfusion did not reverse the antiplatelet effect of ticagrelor in healthy volunteers and is not likely to be of benefit in patients with bleeding.[44951]
Avoid the use of ticagrelor in patients with severe hepatic impairment because it is metabolized by the liver and impaired hepatic function can increase risks for bleeding and other adverse events. In addition, severe hepatic impairment increases the risk of bleeding because of reduced synthesis of coagulation proteins. Ticagrelor has not been studied in patients with moderate or severe hepatic disease or impairment. In patients with moderate hepatic impairment, consider the risks and benefits of treatment, noting the probable increase in exposure to ticagrelor. [44951]
Available data from case-reports of ticagrelor use during pregnancy have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. No adequate or well-controlled studies of ticagrelor in pregnant women exist. In animal reproduction studies, ticagrelor caused structural abnormalities at maternal doses about 5 to 7 times the maximum recommended human dose (MRHD) based on body surface area. Pup death and effects on pup growth were seen when ticagrelor was given at doses 10 times the MRHD to rats during late gestation and lactation. Ticagrelor should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.[44951] Furthermore, ticagrelor should be used with extreme caution near term and during labor and obstetric delivery because of the possibility of maternal postpartum hemorrhage.
According to the manufacturer, it is unknown if ticagrelor or its metabolites are excreted into human breast milk. Since many drugs are excreted into human milk and due to the potentially serious adverse effects to the infant, the manufacturer states that breastfeeding is not recommended during ticagrelor therapy; thus, either ticagrelor therapy or breast-feeding should be discontinued.[44951] Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition.
Avoid interruption or the abrupt discontinuation of ticagrelor therapy in patients being treated for coronary artery disease (CAD). Discontinuation of ticagrelor increases the risk of myocardial infarction, stent thrombosis, and death. If it is absolutely necessary to temporarily discontinue treatment (e.g., to treat bleeding or for elective surgery), restart therapy as soon as possible.[44951]
Use ticagrelor with caution in patients with a history of sick sinus syndrome, second or third degree AV block, or syncope related to bradycardia and not protected by a pacemaker. Ticagrelor can cause ventricular pauses. Bradyarrhythmias, including AV block, have been reported with the postmarketing use of ticagrelor. Patients with sick sinus syndrome, AV block, or bradycardia-related syncope were excluded from ticagrelor clinical trials and may be at increased risk of developing bradyarrhythmias with ticagrelor.[44951]
Ticagrelor is indicated for use with aspirin at doses of 75 to 100 mg per day. Avoid higher aspirin maintenance doses, as ticagrelor efficacy is decreased when aspirin coadministration exceeds 100 mg per day.[44951]
No difference in safety or efficacy is seen between geriatric and younger patients. Approximately half of the patients in the PLATO, PEGASUS, THEMIS, and THALES trials were 65 years of age and older and at least 15% were 75 years of age and older. The relative risk of bleeding was similar in both age and treatment groups. Although no differences were seen in clinical trials, some older patients may be more sensitive to the effects of ticagrelor.[44951]
Ticagrelor has been reported to cause false negative results in platelet function tests, including the heparin-induced platelet aggregation (HIPA) assay, in patients with heparin-induced thrombocytopenia (HIT). Platelet function test interference is related to P2Y12-receptor inhibition on healthy donor platelets by ticagrelor in the affected patient. Ticagrelor is not expected to have an impact on PF4 antibody testing for HIT. Knowledge of current treatment with ticagrelor is needed with interpretation of HIT functional tests.[44951]
Central sleep apnea, including Cheyne-Stokes respiration, has been reported with postmarketing use of ticagrelor. Patients with central sleep apnea may experience a worsening of their symptoms with ticagrelor therapy. Recurrence or worsening of central sleep apnea or Cheyne-Stokes respiration has been reported in patients following ticagrelor rechallenge. If central sleep apnea is suspected, consider further clinical assessment.[44951]
Ticagrelor and its major metabolite reversibly bind to the platelet P2Y12 ADP receptor thereby antagonizing ADP and preventing platelet activation. The maximum inhibition of platelet aggregation (IPA) effect of ticagrelor is reached in approximately 2 hours and maintained for at least 8 hours.[44951]
Revision Date: 10/08/2025, 01:31:00 AMTicagrelor is administered orally. Extensive plasma protein binding (more than 99%) occurs with ticagrelor and the active metabolite. The volume of distribution at steady state is 88 L. Systemic exposure of the active metabolite is approximately 30 to 40% of ticagrelor. The main hepatic isoenzyme responsible for the metabolism of ticagrelor is CYP3A4. Ticagrelor is metabolized to an active metabolite and the primary routes of elimination for ticagrelor and its metabolite are hepatic and biliary, respectively. After oral administration of radiolabeled ticagrelor, approximately 84% recovery of radioactivity was seen (58% in the feces, 26% in the urine). Recovery of ticagrelor and the active metabolite in the urine were less than 1%. The mean half-life is approximately 7 hours for ticagrelor and 9 hours for the active metabolite.[44951]
The maximum inhibition of platelet aggregation (IPA) effect of ticagrelor is reached in approximately 2 hours and maintained for at least 8 hours.[44951]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4, CYP3A5, P-gp, BCRP
Both ticagrelor and its active metabolite are weak inhibitors of CYP3A4, potential activators of CYP3A5, and inhibitors of the P-glycoprotein (P-gp) transporter. Ticagrelor and its active metabolite are P-gp substrates. Based on in vitro studies, ticagrelor is also BCRP inhibitor. Ticagrelor and its metabolite were shown to have no inhibitory effect on CYP1A2, CYP2C19, and CYP2E1.[44951]
The mean absolute bioavailability of ticagrelor is 36% (range 30% to 42%). The maximum concentrations for ticagrelor are seen within 1.5 hours (range 1 to 4 hours) and 2.5 hours (range 1.5 to 5 hours) for the active metabolite. When administered as crushed tablets mixed in water either orally or via nasogastric tube, the mixture is bioequivalent to whole tablets with a median Tmax of 1 hour for ticagrelor and 2 hours for the active metabolite. Ingestion of a high-fat meal has no effect on ticagrelor Cmax but does increase AUC by 21%. In contrast, a high-fat meal results in a decrease in the active metabolite Cmax by 22% with no change in AUC. The drug may be taken with or without food.[44951]
There are no studies of ticagrelor in individuals with severe hepatic impairment and only limited experience with ticagrelor in individuals with moderate hepatic impairment. Although the AUC and Cmax of ticagrelor and the active metabolite are somewhat increased in individuals with mild hepatic impairment compared to those with normal hepatic function, no adjustment in the ticagrelor dose is required for patients with mild hepatic impairment.[44951]
Although the AUC and Cmax of ticagrelor and the active metabolite are somewhat decreased in individuals with severe renal impairment compared to those with normal renal function, no adjustment in the ticagrelor dose is required. Individuals with end-stage renal disease on hemodialysis were found to have an increase of 38% and 51% in AUC and Cmax, respectively, when ticagrelor 90 mg was administered on a non-dialysis day. The AUC and Cmax of ticagrelor were similarly elevated when administered immediately prior to hemodialysis, indicating that ticagrelor is not dialyzable. Ticagrelor's inhibition of platelet aggregation in hemodialysis patients with end-stage renal disease was similar to healthy adults with normal renal function.[44951]
Although the AUC and Cmax of ticagrelor and the active metabolite are somewhat increased in geriatric individuals compared to younger individuals, no adjustment in the ticagrelor dose is required.[44951]
Although the AUC and Cmax of ticagrelor and the active metabolite are somewhat increased in females compared to males, no adjustment in the ticagrelor dose is required.[44951]
Although the exposure and Cmax of ticagrelor and the active metabolite are somewhat increased in Japanese individuals compared to White individuals, no adjustment in the ticagrelor dose is required.[44951]
Available data from case-reports of ticagrelor use during pregnancy have not identified a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. No adequate or well-controlled studies of ticagrelor in pregnant women exist. In animal reproduction studies, ticagrelor caused structural abnormalities at maternal doses about 5 to 7 times the maximum recommended human dose (MRHD) based on body surface area. Pup death and effects on pup growth were seen when ticagrelor was given at doses 10 times the MRHD to rats during late gestation and lactation. Ticagrelor should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.[44951] Furthermore, ticagrelor should be used with extreme caution near term and during labor and obstetric delivery because of the possibility of maternal postpartum hemorrhage.
According to the manufacturer, it is unknown if ticagrelor or its metabolites are excreted into human breast milk. Since many drugs are excreted into human milk and due to the potentially serious adverse effects to the infant, the manufacturer states that breastfeeding is not recommended during ticagrelor therapy; thus, either ticagrelor therapy or breast-feeding should be discontinued.[44951] Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition.
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.