ThisiscontentfromElsevier'sDrugInformation
Tocilizumab
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
8 mg/kg/dose (Max: 800 mg) IV once. If clinical signs or symptoms worsen or do not improve after the first dose, 1 additional dose may be administered at least 8 hours after the initial infusion. Administer tocilizumab in combination with a systemic corticosteroid.[38283] The National Institutes of Health (NIH) COVID-19 treatment guidelines recommend tocilizumab in combination with dexamethasone (with or without remdesivir) to treat hospitalized adults requiring supplemental oxygen, IF the individual is exhibiting signs of systemic inflammation and rapidly increasing oxygen needs while on dexamethasone. The NIH also recommends use of tocilizumab plus dexamethasone to treat people on high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO.[65314]
8 mg/kg/dose (Max: 800 mg) IV once. If clinical signs or symptoms worsen or do not improve after the first dose, 1 additional dose may be administered at least 8 hours after the initial infusion.[38283] The NIH COVID-19 treatment guidelines recommend consideration of the addition of tocilizumab for hospitalized individuals requiring high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO who do not have rapid (e.g., within 24 hours) improvement in oxygenation after initiation of dexamethasone. Remdesivir may be added for people requiring high-flow oxygen or noninvasive ventilation.[65314]
12 mg/kg/dose IV once. If clinical signs or symptoms worsen or do not improve after the first dose, 1 additional dose may be administered at least 8 hours after the initial infusion.[38283] The NIH COVID-19 treatment guidelines recommend consideration of the addition of tocilizumab for hospitalized individuals requiring high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO who do not have rapid (e.g., within 24 hours) improvement in oxygenation after initiation of dexamethasone. Remdesivir may be added for people requiring high-flow oxygen or noninvasive ventilation.[65314]
8 mg/kg/dose (Max: 800 mg) IV once. If clinical signs or symptoms worsen or do not improve after the first dose, 1 additional dose may be administered at least 8 hours after the initial infusion. Administer tocilizumab in combination with a systemic corticosteroid.[69541] [70425] [71855] The National Institutes of Health (NIH) COVID-19 treatment guidelines recommend tocilizumab in combination with dexamethasone (with or without remdesivir) to treat hospitalized adults requiring supplemental oxygen, IF the individual is exhibiting signs of systemic inflammation and rapidly increasing oxygen needs while on dexamethasone. The NIH also recommends use of tocilizumab plus dexamethasone to treat people on high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO.[65314]
4 mg/kg/dose IV every 4 weeks. May increase the dose to 8 mg/kg/dose IV every 4 weeks if needed; doses more than 800 mg are not recommended. May use as monotherapy or concomitantly with methotrexate or other non-biologic DMARDs. Avoid concurrent use with biological DMARDs such as tumor necrosis factor (TNF) modifiers, anakinra, rituximab, ofatumumab, and abatacept.[38283] [69541] [70425] [71855]
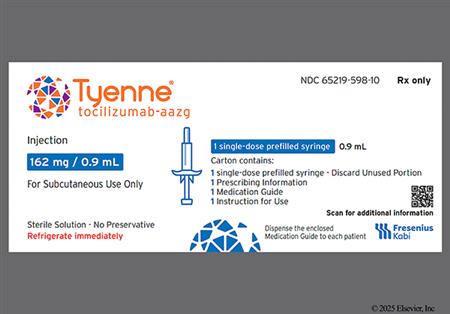
162 mg subcutaneously once weekly as monotherapy or concomitantly with methotrexate or other non-biologic DMARDs. If transitioning from IV tocilizumab, give the first subcutaneous dose instead of the next scheduled IV dose.[38283] [70425] [71855]
162 mg subcutaneously every other week as monotherapy or concomitantly with methotrexate or other non-biologic DMARDs. May increase the dose to 162 mg subcutaneously once weekly based on clinical response. If transitioning from IV tocilizumab, give the first subcutaneous dose instead of the next scheduled IV dose.[38283] [70425] [71855]
NOTE: Tocilizumab has been designated an orphan drug by the FDA for this indication.
8 mg/kg/dose IV every 4 weeks; administer over 1 hour. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [69541] [70425] [71855]
10 mg/kg/dose IV every 4 weeks; administer over 1 hour. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [69541] [70425] [71855]
162 mg/dose subcutaneously every 2 weeks. When transitioning from IV to subcutaneous administration, administer the first subcutaneous dose instead of the next scheduled IV dose. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [70425] [71855]
162 mg/dose subcutaneously every 3 weeks. When transitioning from IV to subcutaneous administration, administer the first subcutaneous dose instead of the next scheduled IV dose. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [70425] [71855]
8 mg/kg/dose IV every 2 weeks; administer over 1 hour. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [69541] [70425] [71855]
12 mg/kg/dose IV every 2 weeks; administer over 1 hour. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [69541] [70425] [71855]
162 mg/dose subcutaneously every week. When transitioning from IV to subcutaneous administration, administer the first subcutaneous dose instead of the next scheduled IV dose. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [70425] [71855]
162 mg/dose subcutaneously every 2 weeks. When transitioning from IV to subcutaneous administration, administer the first subcutaneous dose instead of the next scheduled IV dose. Do not change dose based solely on a single visit body weight measurement, as weight may fluctuate. May use as monotherapy or in combination with methotrexate.[38283] [70425] [71855]
162 mg subcutaneously once weekly. Therapy interruption may be needed for management of dose-related laboratory abnormalities including elevated liver enzymes, neutropenia, and thrombocytopenia.[38283]
6 mg/kg/dose IV every 4 weeks in combination with a tapering course of glucocorticoids. Doses more than 600 mg per infusion are not recommended. Tocilizumab may be used alone after discontinuation of glucocorticoids.[38283] [69541] [70425] [71855]
162 mg subcutaneously once weekly in combination with a tapering course of glucocorticoids. May consider 162 mg subcutaneously every other week based on clinical considerations. Tocilizumab may be used alone after discontinuation of glucocorticoids. If transitioning from IV tocilizumab, give the first subcutaneous dose instead of the next scheduled IV dose.[38283] [70425] [71855]
8 mg/kg IV over 60 minutes for one dose, alone or in combination with corticosteroids. If no clinical improvement in the signs and symptoms of CRS occurs after the first dose, up to 3 additional doses of tocilizumab may be administered at least 8 hours apart; doses exceeding 800 mg are not recommended. Only the intravenous route should be used for the treatment of CRS; subcutaneous administration is not approved for this use. In a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies for hematologic malignancies, 69% of patients with a first episode of CRS who were treated with tocilizumab achieved a response, defined as resolution (lack of fever and off vasopressors for at least 24 hours) within 14 days of the first dose of tocilizumab, less than 2 doses of tocilizumab administered, and no additional treatment beyond tocilizumab and corticosteroids. This was confirmed in a second study using an independent cohort that included 15 patients with CAR T cell-induced CRS.[38283] [70425] [71855]
12 mg/kg IV infusion over 60 minutes for one dose, alone or in combination with corticosteroids. If no clinical improvement in the signs and symptoms of CRS occurs after the first dose, up to 3 additional doses of tocilizumab may be administered at least 8 hours apart; doses exceeding 800 mg are not recommended. Only the IV route should be used for the treatment of CRS; subcutaneous administration is not approved for this use. In a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies for hematologic malignancies, 69% of patients with a first episode of CRS who were treated with tocilizumab achieved a response, defined as resolution (lack of fever and off vasopressors for at least 24 hours) within 14 days of the first dose of tocilizumab, less than 2 doses of tocilizumab administered, and no additional treatment beyond tocilizumab and corticosteroids. This was confirmed in a second study using an independent cohort that included 15 patients with CAR T cell-induced CRS.[38283] [70425] [71855]
8 mg/kg IV over 60 minutes for one dose, alone or in combination with corticosteroids. If no clinical improvement in the signs and symptoms of CRS occurs after the first dose, up to 3 additional doses of tocilizumab may be administered at least 8 hours apart; doses exceeding 800 mg are not recommended. Only the intravenous route should be used for the treatment of CRS; subcutaneous administration is not approved for this use. In a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies for hematologic malignancies, 69% of patients with a first episode of CRS who were treated with tocilizumab achieved a response, defined as resolution (lack of fever and off vasopressors for at least 24 hours) within 14 days of the first dose of tocilizumab, less than 2 doses of tocilizumab administered, and no additional treatment beyond tocilizumab and corticosteroids. This was confirmed in a second study using an independent cohort that included 15 patients with CAR T cell-induced CRS.[38283] [70425] [71855]
12 mg/kg IV infusion over 60 minutes for one dose, alone or in combination with corticosteroids. If no clinical improvement in the signs and symptoms of CRS occurs after the first dose, up to 3 additional doses of tocilizumab may be administered at least 8 hours apart; doses exceeding 800 mg are not recommended. Only the IV route should be used for the treatment of CRS; subcutaneous administration is not approved for this use. In a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies for hematologic malignancies, 69% of patients with a first episode of CRS who were treated with tocilizumab achieved a response, defined as resolution (lack of fever and off vasopressors for at least 24 hours) within 14 days of the first dose of tocilizumab, less than 2 doses of tocilizumab administered, and no additional treatment beyond tocilizumab and corticosteroids. This was confirmed in a second study using an independent cohort that included 15 patients with CAR T cell-induced CRS.[38283] [70425] [71855]
NOTE: Tocilizumab has been designated an orphan drug by the FDA for this indication.
8 mg/kg IV once monthly.[62882]
162 mg subcutaneously once weekly.[62883]
Prior to initiation of treatment
Check the patient's absolute neutrophil count (ANC), platelet count, and liver function tests (ALT/AST concentrations) before tocilizumab initiation.
During treatment for adult patients
Dosage modifications for adult patients with rheumatoid arthritis or systemic sclerosis-associated interstitial lung disease
Dosage modifications for adult patients with giant cell arteritis
Pediatric Patients
Rheumatoid arthritis, weighing more than 100 kg: 800 mg per dose IV or 162 mg per dose subcutaneously.
Rheumatoid arthritis, weighing 100 kg or less: 8 mg/kg per dose IV or 162 mg per dose subcutaneously.
Giant cell arteritis, weighing more than 100 kg: 600 mg per dose IV or 162 mg per dose subcutaneously.
Giant cell arteritis, weighing 100 kg or less: 6 mg/kg per dose IV or 162 mg per dose subcutaneously.
Systemic sclerosis-associated interstitial lung disease: 162 mg per dose subcutaneously.
Cytokine Release Syndrome (CRS), weighing 30 kg or more: 800 mg per dose IV.
CRS, weighing less than 30 kg: 12 mg/kg IV.
COVID-19, weighing more than 100 kg: 800 mg per dose IV.
COVID-19, weighing 100 kg or less: 8 mg/kg per dose IV.
Rheumatoid arthritis, weighing more than 100 kg: 800 mg per dose IV or 162 mg per dose subcutaneously.
Rheumatoid arthritis, weighing 100 kg or less: 8 mg/kg per dose IV or 162 mg per dose subcutaneously.
Giant cell arteritis, weighing more than 100 kg: 600 mg per dose IV or 162 mg per dose subcutaneously.
Giant cell arteritis, weighing 100 kg or less: 6 mg/kg per dose IV or 162 mg per dose subcutaneously.
Systemic sclerosis-associated interstitial lung disease: 162 mg per dose subcutaneously.
Cytokine Release Syndrome (CRS), weighing 30 kg or more: 800 mg per dose IV.
CRS, weighing less than 30 kg: 12 mg/kg IV.
COVID-19, weighing more than 100 kg: 800 mg per dose IV.
COVID-19, weighing 100 kg or less: 8 mg/kg per dose IV.
weighing 30 kg or more: 8 mg/kg per dose IV for systemic juvenile idiopathic arthritis (SJIA), polyarticular juvenile idiopathic arthritis (PJIA); 8 mg/kg per dose (Max: 800 mg) IV for cytokine release syndrome (CRS) and COVID-19; 162 mg per dose subcutaneously for PJIA and SJIA.
weighing less than 30 kg: 12 mg/kg per dose IV for systemic juvenile idiopathic arthritis (SJIA), cytokine release syndrome (CRS), and COVID-19; 10 mg/kg per dose IV for polyarticular juvenile idiopathic arthritis (PJIA); 162 mg per dose subcutaneously for SJIA and PJIA.
2 to 12 years weighing 30 kg or more: 8 mg/kg per dose IV for systemic juvenile idiopathic arthritis (SJIA), polyarticular juvenile idiopathic arthritis (PJIA); 8 mg/kg per dose (Max: 800 mg) IV for cytokine release syndrome (CRS) and COVID-19; 162 mg per dose subcutaneously for PJIA and SJIA.
2 to 12 years weighing less than 30 kg: 12 mg/kg per dose IV for systemic juvenile idiopathic arthritis (SJIA), cytokine release syndrome (CRS), and COVID-19; 10 mg/kg per dose IV for polyarticular juvenile idiopathic arthritis (PJIA); 162 mg per dose subcutaneously for SJIA and PJIA.
younger than 2 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Prior to treatment initiation
For COVID-19 patients, it is recommended tocilizumab not be initiated if ALT or AST are greater than 10-times the upper limit of normal (ULN); however, the National Institutes of Health (NIH) COVID-19 guidelines recommend caution in patients with an ALT greater than 5-times the ULN.[65314] For all other patients, do not initiate treatment with tocilizumab if active liver disease or hepatic impairment is present, or if baseline AST or ALT is more than 1.5-times the ULN. Although, patients with severe or life-threatening cytokine release syndrome (CRS) frequently have elevated ALT or AST; the decision to administer tocilizumab should take into account the potential benefit of treating the CRS versus the risks of short-term treatment with tocilizumab.[38283]
Hepatic enzyme elevations that occur during treatment
Adult Patients with rheumatoid arthritis or systemic sclerosis-associated interstitial lung disease with hepatic impairment[38283]
AST and/or ALT of more than 1 times and up to 3 times the ULN:
AST and/or ALT more than 3 times and up to 5 times the ULN:
AST and/or ALT greater than 5 times the ULN: Discontinue tocilizumab.
Adult Patients with giant cell arteritis with hepatic impairment[38283]
AST and/or ALT of more than 1 times and up to 3 times the ULN:
AST and/or ALT more than 3 times and up to 5 times the ULN:
AST and/or ALT greater than 5 times the ULN: Discontinue tocilizumab.
-Pediatric Patients with hepatic impairment[38283]
Tocilizumab dose reduction has not been studied in the systemic juvenile idiopathic arthritis (SJIA) or polyarticular juvenile idiopathic arthritis (PJIA) population. Tocilizumab dose interruptions are recommended for liver enzyme abnormalities in patients with SJIA or PJIA at levels similar to what is outlined for adult patients with rheumatoid arthritis and giant cell arteritis. If appropriate, adjust or stop concomitant DMARDs and hold tocilizumab dosing until the clinical situation has been evaluated. In SJIA and PJIA, base the decision to discontinue tocilizumab upon the medical assessment of the individual patient and the laboratory abnormality involved.
CrCl 30 mL/minute or more: No dosage adjustment is needed.
CrCl less than 30 mL/minute: Tocilizumab has not been studied in patients with severe renal impairment.[38283]
† Off-label indication




Tocilizumab is a humanized interleukin-6 (IL-6) receptor-inhibiting monoclonal antibody produced in mammalian (Chinese hamster ovary) cells. It is used to treat moderate to severe rheumatoid arthritis (RA) in individuals who have had an inadequate response to 1 or more Disease-Modifying Anti-Rheumatic Drug (DMARDs), polyarticular and systemic juvenile idiopathic arthritis (pJIA and sJIA), giant cell arteritis (GCA or temporal arteritis), systemic sclerosis-associated interstitial lung disease (SSc-ILD), cytokine release syndrome (CRS), and coronavirus disease 2019 (COVID-19). Tocilizumab labeling carries a boxed warning regarding the risk for serious infections that may lead to hospitalization or death; live vaccines should not be administered with tocilizumab. Severe hypersensitivity reactions, including anaphylaxis and death, have also been reported with tocilizumab therapy.[38283] In patients with inflammatory diseases such as rheumatoid arthritis, IL-6 concentrations correlate with disease activity and joint or tissue damage. In adults with RA, tocilizumab improves clinical signs and symptoms, inhibits the radiographic progression of structural joint damage, and improves health status. It is often considered as an alternative to TNF-blockers or may be used when TNF-blockers have failed to produce adequate responses. For RA, pJIA, and sJIA, tocilizumab may be used alone or in combination with methotrexate; in treating adult RA, other non-biologic DMARDs may also be used concurrently. The ideal combination of therapy for individual patients with inflammatory arthritis conditions is determined by treat-to-target strategies and severity of disease.[38283][56233][61404] In adults, tocilizumab has proven effective for GCA, where it is used initially with a tapering dose of corticosteroids. It also slows the rate of decline in pulmonary function in adults with SSc-ILD. For COVID-19, tocilizumab is FDA approved for use in hospitalized adult and pediatric patients, who are receiving systemic corticosteroids and require supplemental oxygen, non-invasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation (ECMO). Tocilizumab was FDA-approved in 2010.[38283]
For COVID-19, the National Institutes of Health (NIH) has issued the following recommendations for the use of tocilizumab based on disease severity:[65314]
Adult patients
Pediatric patients
For storage information, see the specific product information within the How Supplied section.
Infusion Preparation:
Intravenous Infusion Administration:
General information:
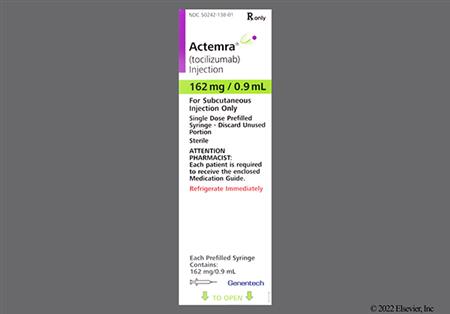
Prefilled Syringe:
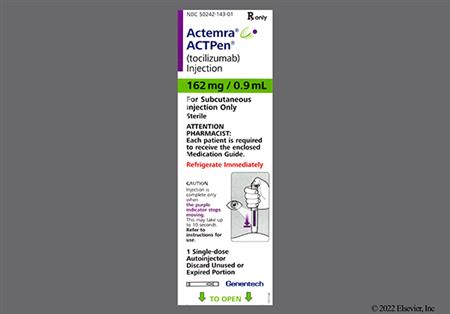
Autoinjector:
Tocilizumab recipients are at increased risk for developing serious infections that may lead to hospitalization or death. Severe and sometimes fatal infections due to bacterial, mycobacterial, invasive fungal, viral, protozoal, or other opportunistic pathogens have been reported in patients receiving immunosuppressive agents including tocilizumab. During and after treatment with tocilizumab, closely monitor all patients for the development of signs and symptoms of infection including the possible development of tuberculosis (TB) in patients who tested negative for latent TB infection before tocilizumab use. If a serious infection develops, interrupt tocilizumab until the infection is controlled. Carefully consider the risks and benefits of continued tocilizumab therapy in patients with chronic or recurrent infection. Infections of various types were reported during clinical trials with tocilizumab. In adults hospitalized with COVID-19, rates of infection and serious infection among those who received 8 mg/kg tocilizumab (n = 974) was 30% and 19%, respectively, as compared to 32% and 23%, respectively, in patients who received placebo (n = 483). Urinary tract infections were reported in 5% of tocilizumab treated patients and 4% of placebo patients. In rheumatoid arthritis patients, upper respiratory tract infection occurred in 7% of patients receiving tocilizumab 8 mg/kg, in 6% of those receiving tocilizumab 4 mg/kg plus DMARDs, and in 8% of patients who received tocilizumab 8 mg/kg plus DMARDs. Naso-pharyngitis was reported in 4% to 7% of patients, and bronchitis was reported in 3% to 4% of patients. The rate of serious infections in the adult tocilizumab 4 mg/kg plus DMARD group was 4.4 events per 100 patient-years, and in the 8 mg/kg plus DMARD group, the rate was 5.3 events per 100 patient-years. Among pediatric patients who received tocilizumab, the rate of serious infections was 11.5 per 100 patient-years for those with systemic juvenile idiopathic arthritis (JIA), 12.2 per 100 patient-years for those with polyarticular JIA and weight less than 30 kg, and 4 per 100 patient-years for those with polyarticular JIA and a weight of 30 kg or more. There is an overall higher incidence of infections in patients with giant cell arteritis (GCA) compared to those with rheumatoid arthritis. The rate of infection or serious infection was 200.2/9.7 events per 100 patient-years in the weekly tocilizumab group and 160.2/4.4 events per 100 patient-years in the tocilizumab every other week group compared to 156/4.2 events per 100 patient-years in the placebo group receiving a 26-week prednisone taper and 210.2/12.5 events per 100 patient-years in the placebo group receiving a 52-week prednisone taper. The rate of serious infections in a cardiovascular outcomes study was 4.5 per 100 patient-years with tocilizumab 8 mg/kg IV, with or without DMARDs, every 4 weeks compared to 3.2 per 100 patient-years with etanercept 50 mg subcutaneously, with or without DMARDs. During clinical trials for any indication, the most common serious infections included pneumonia, urinary tract infection, cellulitis, herpes zoster, gastroenteritis, diverticulitis, sepsis, otitis media, and bacterial arthritis. Among opportunistic infections, tuberculosis (pulmonary or extrapulmonary disease), cryptococcus infection, aspergillosis, candidiasis, and pneumocystosis were reported with tocilizumab. Patients who presented with disseminated rather than localized disease were often taking concomitant immunosuppressants such as methotrexate or corticosteroids. Viral reactivation has been reported with immunosuppressive biologic therapies and cases of herpes zoster exacerbation were observed in tocilizumab clinical studies. No cases of hepatitis B reactivation were observed in the trials; however, patients who screened positive for hepatitis were excluded.[38283] Cases of severe and disseminated strongyloidiasis have been reported following use of tocilizumab in combination with corticosteroids to treat patients with COVID-19. The National Institutes of Health (NIH) COVID-19 treatment guidelines recommend administering ivermectin as prophylactic treatment before giving tocilizumab with a corticosteroid to patients from strongyloidiasis endemic areas.[65314]
Gastrointestinal perforation primarily as a complication of diverticulitis was reported in clinical trials. The overall rate of GI perforation with IV tocilizumab was 0.26 events per 100 patient years. Most patients who developed gastrointestinal perforations were taking concomitant nonsteroidal anti-inflammatory drugs, corticosteroids, or methotrexate. The relative contribution of tocilizumab to the development of gastrointestinal perforations is unknown. Upper abdominal pain occurred in 2% of 288 patients who got tocilizumab 8 mg/kg, in 3% of 774 patients who got tocilizumab 4 mg/kg plus DMARDS, and in 3% of 1582 patients who got tocilizumab 8 mg/kg plus DMARDS. Gastritis occurred in 1% of 288 patients who got tocilizumab 8 mg/kg, in 1% of 774 patients who got tocilizumab 4 mg/kg plus DMARDS, and in 2% of 1582 patients who got tocilizumab 8 mg/kg plus DMARDS. Oral ulceration occurred in 2% of 288 patients who got tocilizumab 8 mg/kg, in 1% of 774 patients who got tocilizumab 4 mg/kg plus DMARDS, and in 2% of 1582 patients who got tocilizumab 8 mg/kg plus DMARDS. Use tocilizumab cautiously in patients who may be at increased risk for gastrointestinal perforation. Promptly evaluate patients presenting with fever, new onset abdominal symptoms, and changes in bowel habits for early identification of gastrointestinal perforation.[38283]
Tocilizumab may cause neutropenia, and patient's neutrophil counts need to be assessed before and during drug receipt. Pooled safety data from adults hospitalized with COVID-19, found 3.4% of patients who received 8 mg/kg tocilizumab (n = 974) had neutrophil counts below 1,000/mm3 as compared to 0.5% of patients who received placebo (n = 483). In the 6-month, controlled clinical studies for rheumatoid arthritis, decreases in neutrophil counts below 1,000/mm3 occurred in 1.8% of patients who received tocilizumab 4 mg/kg/dose and in 3.4% of patients who received tocilizumab 8 mg/kg/dose as compared with 0.1% of patients who received placebo. Decreases in neutrophil counts below 500/mm3 occurred in 0.4% of patients who received tocilizumab 4 mg/kg/dose and in 0.3% of patients who received tocilizumab 8 mg/kg/dose as compared with 0.1% of patients who received placebo. Approximately half of the instances of absolute neutrophil count (ANC) below 1,000/mm3 occurred within 8 weeks of starting tocilizumab. After subcutaneous tocilizumab receipt, 2.9% to 3.7% of tocilizumab recipients had a neutrophil count below 1,000/mm3. Among pediatric patients with polyarticular juvenile idiopathic arthritis (PJIA), 3.7% receiving IV treatment and 15.4% receiving subcutaneous treatment had a neutrophil count below 1,000/mm3 whereas 7% of patients with systemic juvenile idiopathic arthritis (SJIA) did (vs. none in the placebo group). Of note, neutropenia was more frequently observed in patients weighing less than 30 kg (25.9%) than those weighing 30 kg or more (4%) in the subcutaneous administration group. Over an average duration of 73 weeks, a decreased neutrophil count occurred in 17% of tocilizumab recipients. Infections have been uncommonly reported in association with treatment-related neutropenia in long-term extension studies and postmarketing clinical experience, and no clear relationship between decreases in neutrophils below 1,000/mm3 and the occurrence of serious infections was noted. Among healthy patients who received tocilizumab 2 to 28 mg/kg/dose, the ANC nadir occurred 3 to 5 days after tocilizumab receipt. Neutrophils then recovered towards baseline in a dose dependent manner. A similar pattern of ANC after tocilizumab receipt was noted in patients with rheumatoid arthritis.[38283]
Tocilizumab may cause thrombocytopenia, and patient's platelet counts need to be assessed before and during drug receipt. Pooled safety data from adults hospitalized with COVID-19, found 3.2% of patients who received 8 mg/kg tocilizumab (n = 974) had platelet counts below 50,000/mm3 as compared to 1.5% of patients who received placebo (n = 483). In the 6-month, controlled clinical studies for rheumatoid arthritis, decreases in platelet counts below 100,000/mm3 occurred in 1.3% of patients who received tocilizumab 4 mg/kg and in 1.7% of patients who received tocilizumab 8 mg/kg as compared with 0.5% of patients who received placebo. Among patients with polyarticular juvenile idiopathic arthritis (PJIA), 1% had decreases in platelet count of 50,000/mm3 or less. Of patients with systemic juvenile idiopathic arthritis (SJIA), decreases in platelet count of no more than 100,000/mm3 were noted in 1% of tocilizumab recipients and in 3% of placebo recipients at the end of the 12-week control phase. Over an average duration of 73 weeks, 4% of tocilizumab recipients had a decreased platelet count. Treatment-related reduction in platelets was not associated with serious bleeding events in clinical trials.[38283]
Serious cases of hepatotoxicity have been reported with intravenous and subcutaneous tocilizumab therapy; some of these cases resulted in hepatic failure, liver transplant, or death. A majority of the cases presented with elevated hepatic enzymes more than 5-times the upper limit of normal (ULN); however, other cases presented with mild elevations along with signs and symptoms of liver impairment. The time to onset ranged from weeks to years following initiation of tocilizumab therapy, with a median latency of 98 days. Hepatitis, drug-induced liver injury, and jaundice have been reported with postmarketing use of tocilizumab. Patients should have liver function tests (LFTs) monitored during tocilizumab treatment. Check LFTs before tocilizumab receipt, 4 to 8 weeks after the start of therapy for the first 6 months, and then every 3 months thereafter in treated adults. For pediatric patients with either polyarticular or systemic juvenile idiopathic arthritis (PJIA or SJIA), monitor LFTs at the time of the second infusion and then every 4 to 8 weeks for PJIA and every 2 to 4 weeks for SJIA.[38283] [65165] In the 6-month, controlled clinical studies for rheumatoid arthritis, 36% of patients who received tocilizumab 8 mg/kg monotherapy developed an ALT up to 3-times the ULN and 22% experienced AST levels up to 3-times the ULN. Increases in ALT greater than 3- to-5 times ULN occurred in 1%, and increases in ALT of more than 5-times ULN occurred in 0.7%. In a study of 1,538 patients with moderate to severe rheumatoid arthritis, 5.3% and 2.2% of patients developed ALT or AST elevations more than 3-times the ULN, respectively. In addition, one patient developed serious drug-induced hepatitis with hyperbilirubinemia. Increased frequency and magnitude of transaminase elevations were observed when potentially hepatotoxic drugs were used in combination with tocilizumab. For example, among 1,582 patients who received 8 mg/kg tocilizumab plus DMARDs, increases in ALT up to 3-times ULN, greater than 3- to 5-times the ULN, and greater than 5-times the ULN occurred in 48%, 5%, and 1.5% of patients, respectively. Modification of the treatment regimen, such as a reduction in the concomitant DMARD dose, tocilizumab interruption, or tocilizumab dose reduction resulted in a decrease or normalization of liver enzymes. Among pediatric patients with PJIA, 4% had ALT levels 3-times ULN or greater, and less than 1% had AST levels 3-times ULN or greater. Among patients with SJIA, 5% had ALT levels 3-times ULN or greater, and 3% had AST levels greater than 3-times ULN. Over an average duration of 73 weeks in the SJIA extension study, ALT levels 3-times ULN or higher were noted in 13%, and AST levels 3-times ULN or greater were noted in 5%. Among adult patients with rheumatoid arthritis, increases in ALT levels 3-times ULN or greater were noted in 6.5% of weekly subcutaneous tocilizumab recipients and in 3.4% of every other week recipients. In adults hospitalized with COVID-19, 11.7% of patients who received 8 mg/kg of tocilizumab (n = 974) and 9.9% of patients who received placebo (n = 483) had ALT or AST levels at or above 5-times the ULN. Of note, elevated ALT or AST levels may occur in patients hospitalized with COVID-19, and multi-organ failure with involvement of the liver is recognized as a complication of severe COVID-19.[38283]
Tocilizumab may cause hyperlipidemia and hypertriglyceridemia. Assess lipid parameters approximately 4 to 8 weeks after tocilizumab initiation. Subsequently, it is recommended to manage patients according to clinical guidelines [e.g., National Cholesterol Educational Program (NCEP)] for the management of hyperlipidemia. During clinical trials, lipid parameters were first assessed 6 weeks after tocilizumab initiation. Increases in total cholesterol, LDL, HDL, and triglycerides were noted at this time point, but the concentrations remained stable with continued tocilizumab receipt. Triglyceride concentrations greater than 500 mg/dL were rarely observed. In regard to hypercholesterolemia, the mean LDL increase from baseline to week 24 was 25 mg/dL among recipients of tocilizumab 8 mg/kg IV as monotherapy. The mean HDL increase was 4 mg/dL, and the mean LDL/HDL ratio increased by 0.26. ApoB/ApoA1 ratios were essentially unchanged, and elevated lipids responded to lipid-lowering agents. After subcutaneous tocilizumab for rheumatoid arthritis, sustained elevations in total cholesterol more than 240 mg/dL were noted in 19% of the weekly tocilizumab recipients, in 19.6% of the every-other-week tocilizumab recipients, and in 10.2% of the placebo recipients. Among patients with systemic juvenile idiopathic arthritis, 1.5% of tocilizumab recipients had a total cholesterol concentration more than 1.5- to 2-times the upper limit of normal (ULN) as compared with none of the placebo recipients.[38283]
Safety data are available from 974 hospitalized adults who received intravenous tocilizumab doses of 8 mg/kg (maximum dose of 800 mg) to treat COVID-19. Adverse events occurring in at least 3% of drug recipients included anxiety (4%), constipation (9%), diarrhea (4%), hypertension (4%), hypokalemia (4%), insomnia (4%), and nausea (3%).[38283]
Stevens-Johnson syndrome, Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), and hypersensitivity reactions have been reported during postmarketing use of tocilizumab. Postmarketing reports of anaphylaxis, anaphylactic shock, anaphylactoid reactions (such as angioedema), and death have occurred in patients receiving a range of intravenous (IV) tocilizumab doses, with or without concomitant arthritis therapies. These events have occurred in people with and without previous hypersensitivity reactions, in those who received premedication to tocilizumab, and have occurred as early as the first IV infusion. In clinical trials, anaphylaxis or hypersensitivity reactions requiring therapy discontinuation were generally observed during the second to fourth tocilizumab IV infusion , with an incidence of 0.1% to 0.2%. As a comparison, hypersensitivity reactions requiring treatment discontinuation were reported in 0.7% of patients in the subcutaneous tocilizumab clinical trials. For pediatric IV tocilizumab recipients, none of the 188 patients with polyarticular juvenile idiopathic arthritis and 0.9% of 112 patients with systemic juvenile idiopathic arthritis experienced hypersensitivity reactions that required treatment discontinuation. Six of 54 pediatric patients with systemic juvenile idiopathic arthritis (SJIA) developed a hypersensitivity reaction during or within 24 hours of tocilizumab IV; 3 of the reactions were considered serious and required treatment discontinuation. Examples of reactions that required treatment discontinuation include generalized erythema, rash, and urticaria. Infusion-related reactions, defined as events that occurred during or within 24 hours of tocilizumab IV infusion receipt, were noted in 4% to 20.2% of recipients and consisted of hypertension, headache, nausea, hypotension, dizziness, rash, pruritus, urticaria, diarrhea, epigastric discomfort, and arthralgia. In clinical trials of IV tocilizumab for rheumatoid arthritis, rash occurred in 2% to 4% of patients, dyspnea or cough in less than 2%, hypertension in 4% to 6%, headache in 5% to 7%, and dizziness in 2% to 3%. Consider the diagnosis of hypersensitivity or anaphylaxis in any patient who has an IV infusion reaction. Despite prompt medical intervention, one woman died within 24 hours of an anaphylactic event. She experienced lightheadedness and hypotension during her fourth tocilizumab infusion, which was stopped after her symptoms developed. During her fifth infusion 2 weeks later, she experienced dizziness and hypotension moments after the start of the infusion despite premedication with steroids and antihistamines. She became apneic and unresponsive before dying.[38283] [43101] [69541] [70425]
A mild to moderate injection site reaction (7.1% to 10%) including localized erythema, pruritus, pain, and hematoma has been noted with subcutaneous tocilizumab administration in adult patients. As a comparison, 2.4% to 4.1% of subcutaneous placebo recipients had a local reaction. A higher frequency of injection site reaction (28.8% to 41.2%) was observed in pediatric patients receiving subcutaneous tocilizumab. All reactions were mild in severity, but, in the polyarticular arthritis group, occurred more commonly in patients weighing 30 kg or more (44%) compared to those weighing less than 30 kg (14.8%). The majority of injection site reactions resolved without any treatment, and none necessitated drug discontinuation.[38283]
Antibody formation against tocilizumab occurred in 46 of 2,876 adult patients with rheumatoid arthritis (1.6%) who received IV tocilizumab; 5 of the 46 had an associated, medically significant hypersensitivity reaction that led to tocilizumab withdrawal. Thirty adult patients developed neutralizing antibodies to tocilizumab. In polyarticular juvenile idiopathic arthritis trials, 1 patient receiving IV tocilizumab and 3 patients receiving subcutaneous tocilizumab developed positive antibodies without developing a clinically significant hypersensitivity reaction. Of the 2 patients in the systemic juvenile idiopathic arthritis (SJIA) trials that developed positive antibodies, one patient experienced symptoms associated with an anaphylactic reaction (urticaria and angioedema) and the other developed macrophage activation syndrome; both patients discontinued therapy. After subcutaneous drug receipt, 0.9% of 1,454 adult patients with rheumatoid arthritis developed anti-tocilizumab antibodies, and all but 1 patient also developed neutralizing antibodies. The rate is consistent with previous IV experience, and no correlation of antibody development to adverse events or loss of clinical response was observed. In the systemic sclerosis-associated interstitial lung disease studies, 3 of the 169 patients (1.8%) developed antibodies of neutralizing potential; none of the patients experienced hypersensitivity reactions.[38283]
Pancreatitis has been reported with the postmarketing use of tocilizumab.[38283]
Multiple sclerosis and chronic inflammatory demyelinating polyneuropathy were reported rarely in clinical studies of tocilizumab. Closely monitor patients for signs and symptoms potentially indicative of demyelinating disorders, such as optic neuritis or other visual impairment, peripheral neuropathy (numbness or tingling), or unusual fatigue or weakness.[38283]
Tocilizumab may increase the risk of macrophage activation syndrome (hemophagocytic lymphohistiocytosis or MAS), which is a life-threatening disorder that may develop in patients with rheumatic conditions, especially systemic juvenile idiopathic arthritis (SJIA). Limited data from clinical development experience do not suggest that tocilizumab increases the incidence of MAS; during clinical trials for SJIA, 3 cases were observed in 112 patients who received tocilizumab. Two patients had tocilizumab receipt interrupted, and one patient had tocilizumab discontinued for MAS. All three received treatment, and the MAS resolved without sequelae. Of note, infection is a trigger for MAS, and tocilizumab is associated with an increased risk of serious infections. Be attentive to symptoms of infection or worsening arthritis symptoms; SJIA worsening is also a trigger for macrophage activation syndrome.[38283] [54707]
Tocilizumab may increase the risk of a new primary malignancy. Tocilizumab is an immunosuppressant, and treatment with immunosuppressants may result in an increased risk of cancer. Malignancies were observed in clinical studies for rheumatoid arthritis, but the impact of tocilizumab receipt on the development of malignancies is not known. Over 6 months, 15 malignancies were diagnosed in tocilizumab IV recipients as compared with 8 malignancies in patients in the control groups. Exposure-adjusted incidence was similar in the tocilizumab groups (1.32 events per 100 patient-years) and in the placebo plus DMARD group (1.37 events per 100 patient-years). In the all-exposure population, the rate of malignancies remained consistent with the rate observed in the 24-week, controlled period.[38283]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Update immunizations in agreement with current immunization guidelines prior to initiating tocilizumab therapy whenever possible. Avoid concurrent use of live vaccines and tocilizumab. The interval between live vaccinations and initiation of tocilizumab should be in accordance with current vaccination guidelines. No data are available on the secondary transmission of infection from persons receiving live vaccines to patients receiving tocilizumab.[38283]
Treatment with tocilizumab increases the risk of a serious infection that may lead to hospitalization or death. Avoid use in people with an active infection (other than COVID-19), including localized infections. For patients with COVID-19 and other concurrent infections, consider the risks and benefits of treatment with tocilizumab as data are limited in these patients. The risks and benefits of treatment should also be considered prior to administering tocilizumab to geriatric adults (65 years and older) or patients with chronic or recurrent infections, history of serious or opportunistic infections, underlying conditions that may predispose to infection, or those receiving concomitant immunosuppressants (e.g., corticosteroids, methotrexate). Patients residing in or with travel history to regions where mycoses are endemic (e.g., Ohio and Mississippi River valleys, Southwest) are at increased risk for invasive fungal infections. Viral reactivation (herpes zoster) has occurred with tocilizumab treatment; however, it is unknown if tocilizumab increases the risk of hepatitis B reactivation. Tocilizumab also increases the risk of tuberculosis (TB) infection. For patients with COVID-19, baseline testing for latent infection is not necessary; however, for all other patients, evaluate for TB risk factors and test for latent infection prior to starting tocilizumab. If the test is positive for latent TB, treat with standard antimycobacterial therapy before starting tocilizumab. Consider anti-tuberculosis therapy in patients with a history of latent or active TB in whom an adequate course of treatment cannot be confirmed, and in those with risk factors for TB infection. Consult a physician with expertise in treating TB about whether starting anti-tuberculosis therapy is appropriate for the individual patient. Monitor for signs and symptoms of TB and other infections during and after therapy, even in patients who tested negative for latent TB prior to initiation. For patients who develop an infection during treatment with tocilizumab, perform a prompt and complete diagnostic workup appropriate for immunocompromised patients and initiate appropriate antimicrobial therapy. If a patient develops a serious infection, opportunistic infection, or sepsis, interrupt treatment with tocilizumab until the infection is controlled.[38283]
For most indications, initiation of tocilizumab is not recommended for thrombocytopenia defined as a platelet count below 100,000 cells/mm3 or for neutropenia defined as an absolute neutrophil count (ANC) below 2,000 cells/mm3. For the treatment of COVID-19, it is recommended tocilizumab not be used in patients with an ANC less than 1,000 cells/mm3 or platelet count less than 50,000 cells/mm3; however, the National Institutes of Health (NIH) COVID-19 guidelines recommend caution in patients with an ANC less than 500 cells/mm3 or platelet count less than 50,000 cells/mm3.[65314] Thrombocytopenia and neutropenia have been noted with tocilizumab, and drug interruption or discontinuation may be needed. Monitor platelet count and ANC before tocilizumab receipt, 4 to 8 weeks after tocilizumab initiation, and every 3 months thereafter for treated adults. For pediatric patients with either polyarticular or systemic juvenile idiopathic arthritis (JIA), monitor neutrophils and platelets at the time of the second infusion and then every 4 to 8 weeks for PJIA and every 2 to 4 weeks for SJIA. In patients with severe or life-threatening cytokine release syndrome (CRS) who also have cytopenias due to lymphodepleting chemotherapy or the CRS, consider the potential benefit of treating the CRS versus the risks of short-term treatment with tocilizumab.[38283]
Use tocilizumab with caution in patients with a preexisting or recent onset demyelinating disorder, as rare cases of multiple sclerosis and chronic inflammatory demyelinating polyneuropathy have been reported. Monitor for signs and symptoms potentially indicative of demyelinating disorders.[38283]
Gastrointestinal perforations have been reported in patients receiving tocilizumab, primarily as complications of diverticulitis. Use tocilizumab with caution in patients who may be at increased risk for gastrointestinal perforation, including patients with a history of diverticulitis or those receiving concomitant nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or methotrexate. Promptly evaluate patients presenting with fever, new onset abdominal symptoms, and changes in bowel habits.[38283]
Tocilizumab is not recommended for use in people with active hepatic disease or hepatic impairment. For patients with COVID-19, the manufacturer recommends avoiding treatment initiation if ALT or AST are greater than 10-times the upper limit of normal (ULN); however, the National Institutes of Health (NIH) COVID-19 guidelines recommend caution in patients with an ALT greater than 5-times the ULN.[65314] For all other indications, avoid starting tocilizumab if ALT or AST are greater than 1.5-times the ULN. Monitor liver function tests before and during therapy. Dose modifications or treatment interruptions may be required for patients who experience elevated hepatic enzymes during treatment with tocilizumab.[38283]
Available data from a pregnancy exposure registry, retrospective cohort study, pharmacovigilance, and published literature are not sufficient to determine whether the use of tocilizumab during human pregnancy is associated with a risk for major birth defects, miscarriages, or other adverse maternal or fetal outcomes. However, animal reproduction studies indicate there may be a potential fetal risk. Intravenous administration of tocilizumab to Cynomolgus monkeys during organogenesis resulted in abortion/embryo-fetal death at doses 1.25-times or more of the maximum recommended human dose (MRHD). Health care providers are advised to consider that for people with rheumatoid arthritis, published data suggest the risk of adverse pregnancy outcomes [e.g., preterm delivery (before 37 weeks gestation), low birth weight (less than 2,500 grams), small for gestational age at birth] is associated with increased disease activity. Consider the risks and benefits before administering live or live-attenuated vaccines to neonates or infants exposed to tocilizumab in utero, as monoclonal antibodies are increasingly transported across the placenta as pregnancy progresses, with the largest amount transferred during the third trimester. This may affect the immune response in the in utero exposed infant.[38283] [69541] Due to limited data during pregnancy, guidelines state that tocilizumab should be replaced before conception by another medication, if possible. Tocilizumab should be used during pregnancy only when no other pregnancy-compatible drug can effectively control the maternal disease.[62180] For COVID-19, the National Institutes of Health (NIH) states that the decision to administer tocilizumab to a pregnant patient must be shared between the patient and their care team, and that potential maternal benefit and fetal risks must be considered.[65314] Tocilizumab may affect labor and obstetric delivery. Inhibition of IL-6 signaling may interfere with cervical ripening and dilatation and myometrial contractile activity, leading to potential delays in parturition.[38283]
The lack of clinical data during lactation precludes clear determination of the risk of tocilizumab to the breast-feeding infant; therefore the developmental and health benefits of breast-feeding should be considered along with the mother's clinical need for tocilizumab and the potential adverse effects on the breastfed child from exposure to the drug or the underlying maternal condition. There is no information available on the presence of tocilizumab in human milk or its effects on the breast-fed infant or milk production. Maternal immunoglobulin G (IgG) is present in human milk. If tocilizumab is transferred into human milk, the effects of local exposure in the gastrointestinal (GI) tract and potential limited systemic exposure in the infant to tocilizumab are unknown.[38283] Until more data are available, guidelines state that tocilizumab should generally be avoided during breast-feeding if another therapy is available to control the maternal disease. The drug has a large molecular weight, and experts suggest the oral bioavailability of any drug exposure to the infant through the GI tract is likely low. Breast-feeding should not be discouraged, however, when using the drug if no other options are available.[62180] For COVID-19, the National Institutes of Health (NIH) states that tocilizumab should be offered to lactating patients who qualify for therapy, and that breast-feeding can continue without interruption.[65314]
Patients who undergo surgery while taking biologic therapy, such as tocilizumab, may be at greater risk for postoperative infections. For a planned procedure, balance the risk of postoperative infection against the risk of developing a severe or unstable disease by stopping the biologic therapy. The American College of Rheumatology recommends holding tocilizumab for one full dosing interval before undergoing total knee or total hip arthroplasties.[71153]
Tocilizumab inhibits IL-6-mediated signaling by competitively binding to both soluble and membrane-bound IL-6 receptors. IL-6 is a proinflammatory cytokine that is involved in diverse physiological processes such as T-cell activation, immunoglobulin secretion induction, hepatic acute-phase protein synthesis initiation, and hematopoietic precursor cell proliferation and differentiation stimulation. IL-6 is produced by various cell types, including T- and B-cells, lymphocytes, monocytes, and fibroblasts. IL-6 is also produced by synovial and endothelial cells leading to local production of IL-6 in joints affected by inflammatory processes such as rheumatoid arthritis.[38283]
Revision Date: 08/14/2025, 03:01:26 PMTocilizumab is administered subcutaneously or intravenously as an infusion. The pharmacokinetics of tocilizumab are characterized by nonlinear elimination, which is a combination of linear clearance and Michaelis-Menten elimination. The nonlinear part of tocilizumab elimination leads to an increase in exposure that is more than dose-proportional. The pharmacokinetic parameters of tocilizumab do not change with time. Due to the dependence of total clearance on tocilizumab serum concentrations, the half-life of tocilizumab is also concentration-dependent and varies depending on the serum concentration level. At higher concentrations, clearance is mainly determined by the linear clearance, which was estimated to be 12.5 mL/hour. Linear clearance increases with body size. The concentration-dependent nonlinear clearance plays a major role at low concentrations. The half-life of tocilizumab is dependent on the concentration.[38283]
The pharmacokinetics of tocilizumab in adults with COVID-19 was estimated by a population pharmacokinetic analysis of 380 patients treated with intravenous doses of 8 mg/kg. The volume of distribution (Vd) was 8.75 L (4.52 central Vd and 4.23 peripheral Vd). The average linear clearance in the population pharmacokinetic analysis was estimated to be 17.6 mL/hour in patients with baseline ordinal scale (OS) category 3 (i.e., patients requiring supplemental oxygen), 22.5 mL/hour in patients with baseline OS category 4 (i.e., patients requiring high-flow oxygen or noninvasive ventilation), 29 mL/hour in patients with baseline OS category 5 (i.e., patients requiring mechanical ventilation), and 35.4 mL/hour in patients with baseline OS category 6 (i.e., patients requiring ECMO or mechanical ventilation plus additional organ support). Following a single 8 mg/kg infusion, the serum concentrations were below the limit of quantification after 35 days on average.[38283]
A population pharmacokinetic model, based on data in rheumatoid arthritis patients who received either intravenous or subcutaneous tocilizumab, found a terminal half-life of approximately 21.5 days at high serum concentrations and linear clearance of tocilizumab. Among adult patients with rheumatoid arthritis (RA), the tocilizumab Vd at steady-state was 6.4 L: the central Vd was 3.5 L, and the peripheral Vd was 2.9 L. For patients with rheumatoid arthritis, the concentration-dependent apparent half-life at steady-state is up to 11 days for 4 mg/kg/dose IV, up to 13 days for 8 mg/kg/dose IV every 4 weeks, up to 13 days for 162 mg subcutaneously every week, and 5 days for 162 mg subcutaneously every other week. For adults with giant cell arteritis (GCA) at steady-state, the effective half-life for 162 mg subcutaneously every week and every other week was 18.3 to 18.9 days and 4.2 to 7.9 days, respectively. Following 6 mg/kg IV every 4 weeks to GCA patients, the concentration-dependent apparent half-life was 13.2 days. In GCA patients, the Vd at steady-state was 7.46 L: central Vd was 4.09 L and peripheral Vd was 3.37 L. For adults with systemic sclerosis-associated interstitial lung disease (SSc-ILD) at steady-state, the effective half-life for 162 mg subcutaneously every week was between 12.1 to 13 days. In SSc-ILD patients, the Vd at steady-state was 6.74 L: central Vd was 4.16 L and peripheral Vd was 2.58L.[38283]
Decreases in C-reactive protein to within normal ranges were seen as early as week 2 after tocilizumab 4 mg/kg/dose or 8 mg/kg/dose initiation in adults with RA. Decreases in rheumatoid factor, erythrocyte sedimentation rate, serum amyloid A, fibrinogen, and increases in hemoglobin were noted with both tocilizumab doses, but the greatest improvements were noted with the 8 mg/kg dose. Population pharmacokinetic analyses in any patient population tested so far indicate no relationship between apparent clearance and the presence of anti-drug antibodies.[38283]
Affected cytochrome P450 (CYP450) isoenzymes and drug transporters: Unknown, possibly influences CYP enzyme activity
In vitro data suggest that IL-6 reduces mRNA expression for several CYP450 isoenzymes including CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6 and CYP3A4, and this reduced expression was reversed by coincubation with tocilizumab at clinically relevant concentrations. Accordingly, inhibition of IL-6 signaling in patients treated with tocilizumab may restore CYP450 activities to higher levels than those in the absence of the drug, leading to increased metabolism of drugs that are CYP450 substrates. The drug's effect on CYP2C8 or drug transporters (e.g., P-glycoprotein) is unknown.[38283]
The restoration of CYP450 enzyme activities may be clinically relevant for CYP450 substrate drugs with a narrow therapeutic index (NTI), where the dose is individually adjusted. Upon initiation of tocilizumab, therapeutic monitoring of the effect or drug concentration of the NTI drug should be performed; adjust the dose of the NTI drug as needed. Caution should be exercised when tocilizumab is coadministered with drugs where a decrease in effectiveness is undesirable (e.g., oral contraceptives, which are CYP3A4 substrates). The effect of tocilizumab on CYP450 enzyme activity may persist for several weeks after stopping tocilizumab.[38283]
The pharmacokinetics of tocilizumab in adults with COVID-19 was estimated by a population pharmacokinetic analysis of 380 patients treated with intravenous doses of 8 mg/kg. The estimated median maximum plasma concentration (Cmax) and the concentration on Day 28 (Cday28) were 151 mcg/mL (range: 77.5 to 319 mcg/mL) and 0.229 mcg/mL (range: 0.00119 to 19.4 mcg/mL), respectively, after a single dose. After 2 doses, separated by 8 hours, the estimated median Cmax was 290 mcg/mL (range: 152 to 604 mcg/mL) and the Cday28 was 7.04 mcg/mL (0.00474 to 54.8 mcg/mL).[38283]
After receipt of either 4 mg/kg/dose IV or 8 mg/kg/dose IV every 4 weeks, a more than dose-proportional increase in systemic exposure and in the trough concentration was noted in rheumatoid arthritis (RA) patients. At steady-state, the mean concentration with 8 mg/kg dosing was 3-fold higher than the systemic exposure after 4 mg/kg dosing. The trough concentration at steady-state with 8 mg/kg dosing was 134-fold higher than the trough concentration after 4 mg/kg dosing. In contrast, the maximum tocilizumab concentration (Cmax) increased dose-proportionally. After 4 mg/kg/dose IV every 4 weeks, the estimated median (range) Cmean at steady-state was 18 mcg/mL (8.9 to 50.7 mcg/mL), the median (range) steady-state Cmin was 0.1 mcg/mL (0.0 to 14.6 mcg/mL), and the median (range) steady-state Cmax was 86.1 mcg/mL (44.8 to 202 mcg/mL). Ninety percent of steady-state was reached after the first dose for Cmax and AUC and after the fourth dose for Cmin. After 8 mg/kg/dose IV every 4 weeks, the median (range) Cmean at steady-state was 54 mcg/mL (17 to 260 mcg/mL), the median (range) Cmin at steady-state 13.4 mcg/mL (0.1 to 154 mcg/mL), and median (range) Cmax at steady-state was 176 mcg/mL (75.4 to 557 mcg/mL). Approximately 90% of steady-state was reached after the first dose for Cmax, after the third dose for AUC, and after the fourth dose for Cmin. In a non-compartmental pharmacokinetic analysis of 22 giant cell arteritis (GCA) patients treated with 6 mg/kg IV every 4 weeks, the median (range) Cmax, Ctrough, and Cmean at steady-state were 178 mcg/mL (115 to 320 mcg/mL), 22.7 mcg/mL (3.38 to 54.5 mcg/mL), and 57.5 mcg/mL (32.9 to 110 mcg/mL), respectively. Steady-state trough concentrations with IV tocilizumab were within range of those seen in GCA patients treated with 162 mg subcutaneously every week or every other week. Based on pharmacokinetic exposure and extrapolation between RA and GCA patients, when tocilizumab is given on a mg/kg basis, doses greater than 600 mg per infusion are not recommended in GCA patients.[38283]
After weekly or every other week of 162 mg subcutaneous tocilizumab receipt to patients with rheumatoid arthritis (RA), steady-state was achieved after 10 weeks and 12 weeks, respectively. At steady state, the estimated median (range) Cmean was 47.3 mcg/mL (2.4 to 147 mcg/mL), Cmin was 42.9 mcg/mL (1.3 to 144 mcg/mL), and Cmax was 49.8 mcg/mL (3 to 150 mcg/mL) with once-weekly subcutaneous dosing. After every other week subcutaneous dosing, the estimated median (range) Cmean was 9.2 mcg/mL (0.2 to 43.6 mcg/mL), Cmin was 4.1 mcg/mL (0.0 to 34.2 mcg/mL), and Cmax was 12.1 mcg/mL (0.4 to 49.3 mcg/mL) at steady-state. Systemic exposures with once-weekly dosing were 5.1-fold higher for Cmean and 10.5-fold higher for Cmin compared to every other week dosing. Accumulation for Cmin was greater following subcutaneous, both once weekly and every other week regimens, compared to intravenous administration and is expected based on the non-linear clearance at lower concentrations. Greater than 90% of the steady-state value for Cmax was achieved after the fifth dose with the once-weekly regimen and 12th dose with every other week regimen. Ninety percent of the steady-state values for the Cmean and Cmin were achieved after the 6th and 12th injections, for the every other week and once-weekly regimens, respectively.[38283]
In patients, at steady-state, with giant cell arteritis (GCA) who received 162 mg tocilizumab subcutaneously every week, the estimated median (range) Cmax was 72.1 mcg/mL (12.2 to 151 mcg/mL), Cmin was 67.2 mcg/mL (10.7 to 145 mcg/mL), and Cmean was 70.6 mcg/mL (11.7 to 149 mcg/mL). For patients at steady-state who received 162 mg every other week, the estimated median (range) Cmax, Cmin, and Cmean were 17.2 mcg/mL (1.1 to 56.2 mcg/mL), 7.7 mcg/mL (0.1 to 37.3 mcg/mL), and 13.7 mcg/mL (0.5 to 49 mcg/mL), respectively. Steady-state was reached at 17 weeks and 14 weeks following once weekly and every other week dosing regimens, respectively.[38283]
Following administration of 162 mg tocilizumab subcutaneously every week for systemic sclerosis-associated interstitial lung disease, the estimated median (range) Cmax was 52.5 mcg/mL (14.8 to 121 mcg/mL), Cmin was 47.2 mcg/mL (10.8 to 114 mcg/mL), and Cmean was 50.4 mcg/mL (13.4 to 119 mcg/mL) at steady-state. Steady-state was reached after 13 weeks of therapy. The accumulation ratios for Cmean, Cmin, and Cmax were 7.11, 6.56, and 5.89, respectively.[38283]
No formal study of the effect of hepatic impairment on the pharmacokinetics of tocilizumab was conducted; treatment with tocilizumab is not recommended in patients with active hepatic disease or hepatic impairment.[38283]
Mild to moderate renal impairment defined as a CrCl 30 to 79 mL/minute did not impact the pharmacokinetic parameters of tocilizumab during clinical trials for various indications; no dosage adjustments are needed for patients with mild to moderate renal impairment.[38283]
Children and Adolescents 2 to 17 years
Polyarticular juvenile idiopathic arthritis (PJIA)
In pediatric patients with PJIA, the central volume of distribution (Vd) of tocilizumab is 1.98 L, and the peripheral Vd is 2.1 L, resulting in a steady-state Vd of 4.08 L. Linear clearance is 5.8 mL/hour. Half-life is up to 17 days for IV administration or 10 days for subcutaneous administration.[38283]
Average and trough concentrations of tocilizumab at steady-state in pediatric patients (dose = 8 mg/kg/dose or 10 mg/kg/dose IV every 4 weeks) are comparable to those observed in adult rheumatoid arthritis (RA) patients receiving 4 mg/kg/dose or 8 mg/kg/dose IV every 4 weeks and peak concentration similar to adult dose of 8 mg/kg/dose IV every 4 weeks in adult RA patients. The average concentration (Cmean) of tocilizumab in PJIA patients is slightly lower compared than that observed in adult RA patients. For doses of 8 mg/kg/dose IV every 4 weeks (patients weighing 30 kg or more), estimated median Cmax, Cmin, and Cmean were 181 mcg/mL, 3.28 mcg/mL, and 38.6 mcg/mL, respectively, during pharmacokinetic trials. For doses of 10 mg/kg/dose IV every 4 weeks (patients weighing less than 30 kg), estimated median Cmax, Cmin, and Cmean were 167 mcg/mL, 0.35 mcg/mL, and 30.8 mcg/mL, respectively.[38283]
Bioavailability for subcutaneous tocilizumab in PJIA patients is 96%, and the absorption half-life is around 2 days. Average trough concentrations in pediatric patients after subcutaneous dosing are within the range of those achieved in adult patients with RA. Patients treated with subcutaneous tocilizumab have a steady-state Cmin at or higher than that achieved with IV administration. In general, steady-state Cmin is comparable in patients in both body weight groups (less than 30 kg and 30 kg or more), while steady-state Cmax and Cmean are higher for patients in the lower weight group. For doses of 162 mg subcutaneous every 2 weeks (patients weighing 30 kg or more), estimated median Cmax, Cmin, and Cmean were 29.7 mcg/mL, 12.7 mcg/mL, and 23 mcg/mL, respectively, during pharmacokinetic trials. For doses of 162 mg subcutaneous every 3 weeks (patients weighing less than 30 kg), estimated median Cmax, Cmin, and Cmean were 62.4 mcg/mL, 13.4 mcg/mL, and 35.7 mcg/mL, respectively.[38283]
Systemic juvenile idiopathic arthritis (SJIA)
In pediatric patients with SJIA, the central Vd of tocilizumab is 1.87 L, and the peripheral Vd is 2.14 L, resulting in a steady-state Vd of 4.01 L. Linear clearance is 5.7 mL/hour. Half-life is up to 16 days for IV administration or 14 days for subcutaneous administration.[38283]
For doses of 8 mg/kg/dose IV every 2 weeks (patients weighing 30 kg or more), estimated median Cmax, Cmin, and Cmean were 253 mcg/mL, 70.7 mcg/mL, and 117 mcg/mL, respectively, during pharmacokinetic trials. For doses of 12 mg/kg/dose IV every 2 weeks (patients weighing less than 30 kg), estimated median Cmax, Cmin, and Cmean were 274 mcg/mL, 65.9 mcg/mL, and 124 mcg/mL, respectively. Steady-state was reached by 8 weeks for both groups. Mean estimated tocilizumab exposure parameters were similar between the 2 dose groups defined by body weight.[38283]
Bioavailability for subcutaneous tocilizumab in SJIA patients is 95%, and absorption half-life is around 2 days. Patients treated with subcutaneous tocilizumab have a steady-state Cmax lower than that achieved with IV administration. Steady-state Cmin and Cmean are comparable in patients after subcutaneous or IV dosing across body weights. For doses of 162 mg subcutaneous every week (patients weighing 30 kg or more), estimated median Cmax, Cmin, and Cmean were 89.8 mcg/mL, 72.4 mcg/mL, and 82.4 mcg/mL, respectively, during pharmacokinetic trials. For doses of 162 mg subcutaneous every 2 weeks (patients weighing less than 30 kg), estimated median Cmax, Cmin, and Cmean were 127 mcg/mL, 64.2 mcg/mL, and 92.7 mcg/mL, respectively. Steady-state was reached by 12 weeks for both groups.[38283]
COVID-19
Based on PK modeling and simulation, the recommended dosing is expected to achieve plasma exposure of tocilizumab in pediatric patients 2 years and older with COVID-19 that is comparable to the exposure observed in adults with COVID-19.[38283]
Age was not shown to have an effect on the pharmacokinetics of tocilizumab.[38283]
Gender was not shown to have an effect on the pharmacokinetics of tocilizumab.[38283]
Race was not shown to have an effect on the pharmacokinetics of tocilizumab.[38283]
Population analysis identified body weight as a significant covariate impacting the pharmacokinetics of tocilizumab. When given IV on a mg/kg basis, individuals weighing 100 kg or more are predicted to have mean steady-state exposures higher than mean values for the patient population. In RA patients, the body weight-based dose (8 mg per kg) resulted in approximately 86% higher exposure in patients weighing more than 100 kg in comparison to patients who weigh less than 60 kg. Therefore, tocilizumab doses exceeding 800 mg per IV infusion are not recommended in patients with RA. There was an inverse relationship between tocilizumab exposure and body weight for flat dose subcutaneous regimens. Due to the flat dosing employed for subcutaneous administration of tocilizumab, no modifications are necessary by this dosing route.[38283]
In GCA patients treated with subcutaneous tocilizumab, higher exposure was observed in patients with lower body weight. For the 162 mg every week subcutaneous dosing regimen, the steady-state Cmean was 51% higher in patients with body weight less than 60 kg compared to patients weighing between 60 and 100 kg. For the 162 mg every other week subcutaneous regimen, the steady-state Cmean was 129% higher in patients weighing less than 60 kg compared to patients weighing between 60 and 100 kg. There is limited data for patients above 100 kg (n=7). Due to the flat dosing employed for subcutaneous administration of tocilizumab, no modifications are necessary by this dosing route.[38283]
In adults with COVID-19, exposure to tocilizumab following weight-based dosing (i.e., 8 mg/kg IV, with a maximum dose of 800 mg) was dependent on body weight and disease severity. Within a specific ordinal scale (OS) category, tocilizumab exposure was 20% lower in patients weighing less than 60 kg, as compared to patients with a mean body weight of 80 kg. Exposure in patients weighing more than 100 kg was in the same range as those with a mean body weight of 80 kg. For an 80 kg patient, exposure decreased as disease severity increased; for each category increase on the OS, exposure decreased consistently by 13%.[38283]
Available data from a pregnancy exposure registry, retrospective cohort study, pharmacovigilance, and published literature are not sufficient to determine whether the use of tocilizumab during human pregnancy is associated with a risk for major birth defects, miscarriages, or other adverse maternal or fetal outcomes. However, animal reproduction studies indicate there may be a potential fetal risk. Intravenous administration of tocilizumab to Cynomolgus monkeys during organogenesis resulted in abortion/embryo-fetal death at doses 1.25-times or more of the maximum recommended human dose (MRHD). Health care providers are advised to consider that for people with rheumatoid arthritis, published data suggest the risk of adverse pregnancy outcomes [e.g., preterm delivery (before 37 weeks gestation), low birth weight (less than 2,500 grams), small for gestational age at birth] is associated with increased disease activity. Consider the risks and benefits before administering live or live-attenuated vaccines to neonates or infants exposed to tocilizumab in utero, as monoclonal antibodies are increasingly transported across the placenta as pregnancy progresses, with the largest amount transferred during the third trimester. This may affect the immune response in the in utero exposed infant.[38283] [69541] Due to limited data during pregnancy, guidelines state that tocilizumab should be replaced before conception by another medication, if possible. Tocilizumab should be used during pregnancy only when no other pregnancy-compatible drug can effectively control the maternal disease.[62180] For COVID-19, the National Institutes of Health (NIH) states that the decision to administer tocilizumab to a pregnant patient must be shared between the patient and their care team, and that potential maternal benefit and fetal risks must be considered.[65314] Tocilizumab may affect labor and obstetric delivery. Inhibition of IL-6 signaling may interfere with cervical ripening and dilatation and myometrial contractile activity, leading to potential delays in parturition.[38283]
The lack of clinical data during lactation precludes clear determination of the risk of tocilizumab to the breast-feeding infant; therefore the developmental and health benefits of breast-feeding should be considered along with the mother's clinical need for tocilizumab and the potential adverse effects on the breastfed child from exposure to the drug or the underlying maternal condition. There is no information available on the presence of tocilizumab in human milk or its effects on the breast-fed infant or milk production. Maternal immunoglobulin G (IgG) is present in human milk. If tocilizumab is transferred into human milk, the effects of local exposure in the gastrointestinal (GI) tract and potential limited systemic exposure in the infant to tocilizumab are unknown.[38283] Until more data are available, guidelines state that tocilizumab should generally be avoided during breast-feeding if another therapy is available to control the maternal disease. The drug has a large molecular weight, and experts suggest the oral bioavailability of any drug exposure to the infant through the GI tract is likely low. Breast-feeding should not be discouraged, however, when using the drug if no other options are available.[62180] For COVID-19, the National Institutes of Health (NIH) states that tocilizumab should be offered to lactating patients who qualify for therapy, and that breast-feeding can continue without interruption.[65314]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.