ThisiscontentfromElsevier'sDrugInformation
Tofacitinib
Learn more about Elsevier's Drug Information today! Get the drug data and decision support you need, including TRUE Daily Updates™ including every day including weekends and holidays.
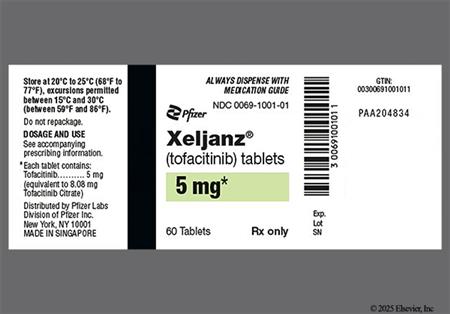
5 mg PO twice daily with or without methotrexate or other non-biologic (conventional) disease-modifying antirheumatic drugs (DMARDs). Higher doses are not recommended. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
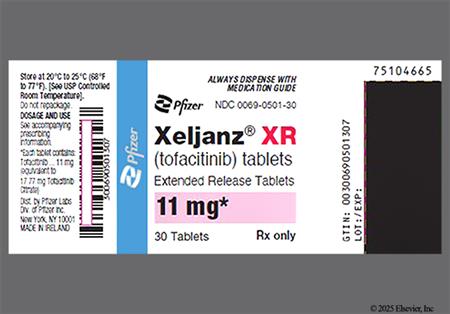
11 mg PO once daily with or without methotrexate or other non-biologic (conventional) disease-modifying antirheumatic drugs (DMARDs). Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
5 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
5 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
4 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
3.2 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
11 mg PO once daily. Persons treated with tofacitinib 5 mg PO twice daily may be switched to the extended-release formulation the day after the last dose of the immediate-release tablets. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
5 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315] [71337] [71338]
11 mg PO once daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315] [71337] [71338]
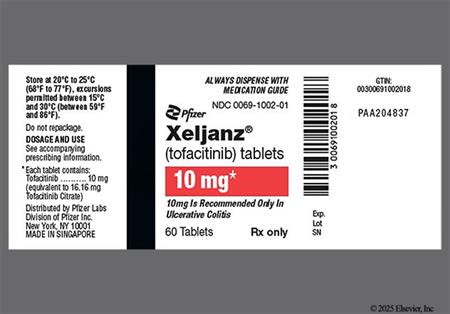
10 mg PO twice daily for at least 8 weeks and up to 16 weeks, then 5 mg PO twice daily. Discontinue 10 mg PO twice daily after 16 weeks if inadequate response. May consider 10 mg PO twice daily for the shortest duration for individuals with loss of response during maintenance treatment. Use the lowest effective dose needed to maintain response. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315] Guidelines strongly recommend tofacitinib for induction of remission in individuals with moderately to severely active ulcerative colitis who have previously failed anti-TNF therapy and for maintenance of remission in individuals who respond to tofacitinib induction.[64393] [65934]
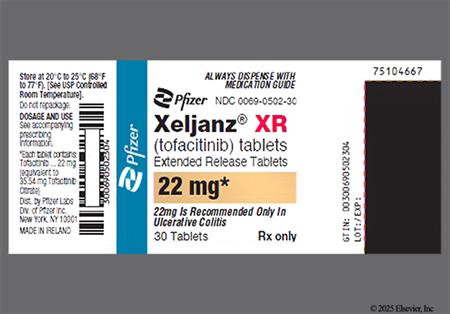
22 mg PO once daily for at least 8 weeks and up to 16 weeks, then 11 mg PO once daily. Discontinue 22 mg PO once daily after 16 weeks if inadequate response. May consider 22 mg PO once daily for the shortest duration for individuals with loss of response during maintenance treatment. Use the lowest effective dose needed to maintain response. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315] Guidelines strongly recommend tofacitinib for induction of remission in individuals with moderately to severely active ulcerative colitis who have previously failed anti-TNF therapy and for maintenance of remission in individuals who respond to tofacitinib induction.[64393] [65934]
NOTE: Although approved for polyarticular course juvenile idiopathic arthritis (pcJIA), tofacitinib is not recommended for the treatment of pediatric patients with systemic juvenile idiopathic arthritis (sJIA) as clinical trials failed to show efficacy.[52315]
5 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
4 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
3.2 mg PO twice daily. Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
10 mg PO twice daily for up to 14 days or until hospital discharge, whichever comes first. The National Institute of Health (NIH) recommends tofacitinib to treat hospitalized adults on supplemental oxygen, IF the individual is exhibiting signs of systemic inflammation and rapidly increasing oxygen needs while on dexamethasone. Further, tofacitinib may be given with dexamethasone to treat people on high-flow oxygen, noninvasive ventilation, mechanical ventilation, or ECMO. Tofacitinib is recommended for use only when other immunomodulators are unavailable or cannot be administered.[65314] Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[52315]
5 to 10 mg PO twice daily. Efficacy is increased at 10 mg PO twice daily; however, the higher dose is associated with an increased risk for adverse effects (e.g., infection, cytopenia). Coadministration of certain drugs may need to be avoided or dosage adjustments may be necessary; review drug interactions.[66610]
Anemia
Monitor hemoglobin at baseline, after 4 to 8 weeks of treatment, and every 3 months thereafter. Do not initiate tofacitinib in patients with anemia defined as a hemoglobin less than 9 grams/dL. If the hemoglobin decreases to less than 8 grams/dL or decreases more than 2 grams/dL from baseline, interrupt dosing until hemoglobin values have normalized.[52315]
Lymphopenia
Monitor lymphocyte counts at baseline and every 3 months thereafter. Do not initiate tofacitinib in patients with an absolute lymphocyte count less than 500 cells/mm3. Discontinue tofacitinib if the lymphocyte count decreases to less than 500 cells/mm3 during therapy, confirmed by repeat testing.[52315]
Neutropenia
Monitor neutrophil counts at baseline, after 4 to 8 weeks of treatment, and every 3 months thereafter. Do not initiate tofacitinib in patients with an absolute neutrophil count (ANC) less than 1,000 cells/mm3. Discontinue tofacitinib if the ANC falls below 500 cells/mm3, regardless of the indication.[52315]
Hyperlipidemia
Assess lipid parameters in all patients approximately 4 to 8 weeks following initiation of tofacitinib therapy. The maximum drug effects on lipid parameters are generally observed within 6 weeks. Manage patients according to clinical guidelines such as those of the National Cholesterol Educational Program (NCEP) for the management of hyperlipidemia.[52315]
20 mg/day PO for immediate-release formulations; 22 mg/day PO for extended-release tablets.
20 mg/day PO for immediate-release formulations; 22 mg/day PO for extended-release tablets.
weighing 40 kg or more: 10 mg/day PO immediate-release formulations.
weighing 20 to 39 kg: 8 mg/day PO immediate-release formulations.
2 to 12 years weighing 40 kg or more: 10 mg/day PO immediate-release formulations.
2 to 12 years weighing 20 to 39 kg: 8 mg/day PO immediate-release formulations.
2 to 12 years weighing 10 to 19 kg: 6.4 mg/day PO immediate-release formulations.
1 year: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Adults
Mild impairment (Child-Pugh class A):
Moderate impairment (Child-Pugh class B):
Severe impairment (Child-Pugh class C):
Pediatric Patients
Mild impairment (Child-Pugh class A):
Moderate impairment (Child-Pugh class B):
Severe impairment (Child-Pugh class C):
Adults
Mild impairment (CrCl 51 to 80 mL/minute):
Moderate (CrCL 30 to 50 mL/minute) to severe impairment (CrCL less than 30 mL/minute):
Pediatric Patients
Mild impairment (CrCl 51 to 80 mL/minute):
Moderate (CrCL 30 to 50 mL/minute) to severe impairment (CrCL less than 30 mL/minute):
Dosage Adjustments for COVID-19 per the National Institutes of Health (NIH) treatment guidelines:
eGFR 60 mL/minute/1.73 m2 or more: No dosage adjustment is needed.
eGFR less than 60 mL/minute/1.73 m2: 5 mg PO twice daily immediate-release tablet.
Intermittent hemodialysis
Administer the dose after the dialysis session on dialysis days. Supplemental doses are not recommended after dialysis if the dose was taken before the dialysis procedure.[52315]
† Off-label indication
Tofacitinib is an oral Janus kinase (JAK) inhibitor, and is considered a targeted synthetic disease-modifying antirheumatic drug (tsDMARD). Janus kinases are intracellular enzymes that transmit signals arising from cytokine interactions on the cellular membrane to influence cellular processes of immune cell function. Tofacitinib has been shown to be useful for a variety of inflammatory conditions. It is indicated in individuals who have had an inadequate response or intolerance to 1 or more TNF blockers for the treatment of moderately to severely active rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis, moderate to severe ulcerative colitis, and polyarticular juvenile idiopathic arthritis (pJIA). It has also been studied for the treatment of systemic JIA in pediatric patients; however, clinical trials failed to show efficacy.[52315] In adults with RA or PsA, the drug improves clinical signs and symptoms and improves physical function; in adults with RA, tofacitinib inhibits the radiographic progression of structural joint damage. For individuals with RA, tofacitinib is used as monotherapy or in combination with methotrexate or other nonbiological DMARDs.[52339] Guidelines for PsA state that tofacitinib may be considered in patients with contraindications or adverse effects to TNF inhibitors, with primary TNF-inhibitor failure, or in patients preferring oral medication to injectable biologic agents who do not have severe disease. Tofacitinib is also an option in treatment-naive patients with predominant enthesitis or concurrent active inflammatory bowel disease (IBD).[63834] Guidelines for RA were published before the availability of tofacitinib, but the drug, like other non-TNF targeted treatments, is usually reserved for patients with contraindications, intolerance, or inadequate response to biologic agents such as the TNF inhibitors.[56233] The ideal combination of therapy for individual patients with inflammatory arthritis conditions such as RA and PsA is determined by treat to target strategies and severity of the disease.[56233][62838][63834] Tofacitinib has shown utility in the treatment of inflammatory bowel disease, to induce and maintain remission in UC.[52315] The efficacy of tofacitinib for the treatment of moderately to severely active UC was demonstrated in 3 controlled clinical trials. Two 8-week placebo-controlled trials demonstrated that tofacitinib 10 mg twice daily induces remission in 17% to 18% of patients by week 8. Among patients who achieved a clinical response by week 8, tofacitinib 5 mg or 10 mg given twice daily was effective in inducing remission by week 52 in 34% and 41% of patients, respectively; among patients who achieved remission after 8 weeks of treatment, 35% and 47% achieved sustained corticosteroid-free remission when treated with 5 mg and 10 mg, respectively.[52315] Further research with head-to-head trials between tofacitinib and approved biologic therapies for UC could help determine where the drug or other JAK inhibitors under development fit into treatment algorithms for UC, including treat-to-target strategies; at this time tofacitinib is recommended for patients who have failed anti-TNF treatments.[64393][65934] Tofacitinib was FDA-approved in 2012.[52315]
The use of tofacitinib does present some safety concerns. Serious infections and malignancy may be precipitated by tofacitinib; the drug is not to be used in combination with biologic DMARDs or with potent immunosuppressants such as azathioprine and cyclosporine.[52315] A large, postmarketing, randomized, safety clinical trial showed an increased risk of all-cause mortality (including sudden cardiovascular death), major adverse cardiovascular events (MACE; defined as cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke), thrombosis (including deep venous thrombosis (DVT), pulmonary embolism (PE), and arterial thrombosis), and cancer, excluding non-melanoma skin cancer (NSMC), with the use of tofacitinib 5 mg PO twice daily or tofacitinib 10 mg PO twice daily compared to TNF inhibitors in RA patients aged 50 years or older with one or more CV risk factors. Higher rates of lung cancer and lymphoma were also observed. Current or past tobacco smokers were at increased risk of lung cancer, overall cancers, and major adverse cardiovascular events. Consider the benefits and risks for the individual patient before initiation or continuation of therapy, particularly in those with risk factors such as smoking, cardiovascular risk factors, those who develop malignancy, and those with a known malignancy other than successfully treated non-melanoma skin cancer. Reserve tofacitinib for patients who have an inadequate response or intolerance to one or more TNF inhibitors. Advise patients to seek emergency medical attention if they experience signs and symptoms of a heart attack, stroke, or blood clot[52315][66958]
Updates for coronavirus disease 2019 (COVID-19):
Adult patients
Pediatric patients
For storage information, see the specific product information within the How Supplied section.
Hazardous Drugs Classification
Extended-release tablets
In trials with tofacitinib, lymphopenia, lymphocytosis, neutropenia, anemia, and fatigue were noted. Initially, lymphocytosis was noted at 1 month after tofacitinib initiation. A gradual decrease in mean lymphocyte counts of approximately 10% below the baseline was noted during 12 months of therapy. In clinical trials involving tofacitinib 5 mg and 10 mg twice daily dosing, confirmed decreases in lymphocyte counts less than 500 cells/mm3 occurred in 0.04% of all tofacitinib recipients, and the decreases were associated with an increased incidence of treated and serious infections. During the first 3 months of tofacitinib therapy in clinical trials, confirmed decreases in ANC below 1,000 cells/mm3 occurred in 0.07% of tofacitinib recipients; no confirmed decreases in ANC below 500 cells/mm3 were observed, and no clear relationship between neutropenia and the occurrence of serious infections was apparent. However, tofacitinib receipt was associated with an increased incidence of neutropenia (less than 2,000 cells/mm3) as compared with placebo. During the maintenance trial of tofacitinib in patients with ulcerative colitis, anemia was reported in 2% to 4% of tofacitinib patients compared to 2% of placebo patients. Hemoglobin and neutrophil count should be checked prior to initiation of tofacitinib therapy, after 4 to 8 weeks of treatment, and then every 3 months. Lymphocyte count should be checked prior to initiation of tofacitinib therapy, then every 3 months. Interrupt tofacitinib receipt in patients who develop hemoglobin less than 8 grams/dL or whose hemoglobin concentration drops greater than 2 grams/dL on treatment. In patients who develop a confirmed absolute lymphocyte count less than 500 cells/mm3 or an ANC less than 500 cells/mm3, tofacitinib treatment is not recommended. For patients who develop a persistent ANC of 500 to 1,000 cells/mm3, interrupt tofacitinib receipt until the ANC is greater than 1,000 cells/mm3.[52315]
Hepatitis, steatosis, and elevated hepatic enzymes were noted in the clinical trials of tofacitinib. Most of the enzyme abnormalities occurred in studies with background DMARD (primarily methotrexate) therapy. For example, no differences in the incidence of ALT or AST elevations were observed between the placebo and tofacitinib 5 mg twice daily groups. However, with concurrent DMARDs, ALT elevations greater than 3 times the upper limit of normal (ULN) were observed in 1% of patients receiving placebo, 1.3% of patients receiving tofacitinib 5 mg twice daily, and 1.2% of patients receiving tofacitinib 10 mg twice daily. AST elevations greater than 3 times the ULN were observed in 0.6% of patients receiving placebo, 0.5% of patients receiving tofacitinib 5 mg twice daily, 0.4% of patients receiving tofacitinib 10 mg twice daily. One patient who received tofacitinib 10 mg twice daily for approximately 2.5 months required hospitalization and liver biopsy after developing drug-induced liver injury, symptomatic elevations of greater than 3 times the ULN in AST and ALT and elevations in bilirubin of greater than 2 times the ULN. Monitor liver function tests routinely during tofacitinib therapy and promptly investigate causes of hepatic enzyme elevations to identify potential cases of drug-induced liver injury. If drug-induced hepatotoxicity is suspected, interrupt tofacitinib receipt until drug-induced liver injury has been excluded. In clinical trials, reduction in the dose of concomitant DMARD, interruption of tofacitinib, or reduction in tofacitinib dose resulted in a decrease or the normalization of liver enzymes. Postmarketing cases of hepatitis B reactivation have been reported in patients treated with tofacitinib, and such reactivation may lead to hepatitis B exacerbation. The safety and efficacy of tofacitinib in patients with positive hepatitis B virus or hepatitis C virus serology are not established.[52315]
A serious and sometimes fatal infection due to bacterial, mycobacterial, invasive fungal, viral, or other opportunistic pathogens has been reported in rheumatoid arthritis patients who received tofacitinib. In the 7 controlled trials in patients with rheumatoid arthritis (RA), during the 0 to 3 months exposure, the overall frequency of infections was 20% and 22% in the 5 mg twice daily and 10 mg twice daily groups, respectively, and 18% in the placebo group. The most commonly reported infections were upper respiratory tract infections, naso-pharyngitis, and urinary tract infections (4%, 3%, and 2% of patients, respectively). Among RA patients enrolled in 7 clinical trials (1 to 12 months duration), 34 tofacitinib 5 mg twice daily patients (2.7 events per 100 patient-years) and 33 tofacitinib 10 mg twice daily patients (2.7 events per 100 patient-years) developed serious infections. The most common serious infections included pneumonia, cellulitis, herpes zoster, and urinary tract infection. Opportunistic infections such as cryptococcus, esophageal candidiasis, pneumocystosis, cytomegalovirus, and BK virus were reported in 4 patients who received tofacitinib. The median time of tofacitinib exposure before a diagnosis of an opportunistic infection was 8 months (range, 41 to 698 days). Some patients have presented with disseminated rather than localized disease, and were often taking concomitant immunomodulating agents such as methotrexate or corticosteroids. Six patients (0.5 events per 100 patient-years) who received tofacitinib 10 mg twice daily in RA trials developed tuberculosis compared to zero patients that received tofacitinib 5 mg twice daily. The median time of tofacitinib exposure before a diagnosis of tuberculosis was 10 months (range, 152 to 960 days). In the ulcerative colitis (UC) population, treatment with 10 mg twice daily was associated with a greater risk of serious infections compared to 5 mg twice daily. Additionally, opportunistic herpes zoster infections (including meningoencephalitis, ophthalmologic, and disseminated cutaneous) were seen in patients who were treated with tofacitinib 10 mg twice daily. During the maintenance trial of tofacitinib in patients with UC, naso-pharyngitis was reported in 10% to 14% of patients. Upper respiratory tract infection (6% to 7%), herpes zoster (1% to 5%), and fever (2% or more) were reported in patients receiving tofacitinib for UC. Viral reactivation including cases of herpes virus reactivation (e.g., herpes zoster) were observed; herpes zoster was reported in 1% to 5% of tofacitinib patients. Closely monitor patients for the development of signs and symptoms of infection including tuberculosis during and after treatment with tofacitinib. Monitoring is needed even for patients who tested negative for latent tuberculosis infection before tofacitinib initiation. For any new infection, institute prompt and complete diagnostic testing appropriate for an immunocompromised patient. Also, initiate appropriate antimicrobial therapy and closely monitor the patient. Interrupt tofacitinib if a patient develops a serious or an opportunistic infection until the infection is controlled.[52315]
In rheumatoid arthritis clinical trials, hypertension was reported in 2% of tofacitinib recipients compared to 1% of placebo recipients. Peripheral edema was also noted during clinical trials.[52315]
Of tofacitinib recipients in rheumatoid arthritis clinical trials, 3% to 4% reported headache compared to 2.1% of placebo recipients. Insomnia and paresthesias were also noted in trials. During the maintenance trial of tofacitinib in patients with ulcerative colitis, headache was reported in 3% to 9% of patients compared to 6% of placebo patients.[52315]
Of tofacitinib recipients in rheumatoid arthritis (RA) clinical trials, 3 to 4% had diarrhea as compared with 2% of placebo recipients. Abdominal pain, dyspepsia, vomiting, gastritis, dehydration, diverticulitis, and nausea were also reported during RA trials. During induction trials of tofacitinib in patients with ulcerative colitis (UC), diarrhea was reported in 5% or more of patients. During maintenance UC trials, gastroenteritis (3% to 4%), diarrhea (2% to 5%), and nausea (1% to 4%) were reported with tofacitinib therapy. Serious gastrointestinal (GI) reactions, such as GI perforation, have been noted among tofacitinib recipients, although the role of the drug in these events is unknown. Patients may be at an increased risk of perforation if they have a history of diverticulitis or are taking nonsteroidal antiinflammatory drugs (NSAIDs). In the RA studies, many patients were receiving background therapy with NSAIDs. There was no discernible difference in frequency of GI perforation between the placebo and tofacitinib arms in UC clinical trials and many of the patients were receiving background corticosteroid therapy. Promptly evaluate patients presenting with new-onset abdominal symptoms for early identification of GI perforation. Cautious use of tofacitinib is advised for patients who may be at increased risk for GI perforation, such as those taking NSAID therapy or with a history of diverticulitis. Additionally, the extended-release formulation of tofacitinib (tofacitinib XR) should be used with caution in patients with pre-existing severe GI narrowing (pathologic or iatrogenic). The tofacitinib XR tablets utilize a non-deformable extended-release system. There have been rare reports of symptoms of GI obstruction in patients with known GI stricture following ingestion of other medications utilizing a non-deformable extended-release formulation.[52315]
Tofacitinib receipt may cause dose-dependent increases in lipid parameters including hypercholesterolemia. During the first 12 weeks of rheumatoid arthritis (RA) trials, the mean LDL cholesterol increased by 15% in the 5 mg twice daily arm and by 19% in the 10 mg twice daily arm. The mean HDL cholesterol increased by 10% in the 5 mg twice daily arm and by 12% in the 10 mg twice daily arm. Of note, the mean LDL/HDL ratios were essentially unchanged among tofacitinib recipients. Dose-related elevations in total cholesterol and triglycerides were also noted. Elevations were observed at one month of exposure and remained stable thereafter. Maximum effects were generally observed within 6 weeks. During the maintenance trial of tofacitinib in patients with ulcerative colitis, elevated cholesterol levels (i.e., hypercholesterolemia, hyperlipidemia, dyslipidemia, hypertriglyceridemia, increased LDL cholesterol, or abnormal LDL cholesterol) were reported in 5% to 9% of patients. The effect of lipid parameter elevations on cardiovascular morbidity and mortality has not been determined; manage patients according to clinical guidelines for the management of hyperlipidemia. In a controlled clinical trial involving RA patients, elevations in LDL cholesterol and ApoB decreased to pretreatment concentrations in response to statin therapy. Assess lipid parameters 4 to 8 weeks after initiation of tofacitinib therapy.[52315]
In clinical trials of tofacitinib, cough, nasal congestion, dyspnea, and interstitial lung disease (cases were limited to patients with rheumatoid arthritis and some were fatal) were noted.[52315]
In clinical trials of tofacitinib, musculoskeletal pain, arthralgia, tendinitis, and joint swelling were reported. Increased blood creatine phosphokinase (CPK) was reported in 2% to 7% of patients receiving tofacitinib for ulcerative colitis. In trials with tofacitinib, dose-related elevations in serum creatinine (SCr) were observed. The mean increase in SCr was less than 0.1 mg/dL in the 12-month pooled safety analysis; however, up to 2% of patients discontinued tofacitinib in the long-term extensions because of protocol-specified discontinuation criteria for an increase in SCr by more than 50% of baseline. The clinical significance of the SCr elevations is unknown.[52315]
Hypersensitivity reactions, including urticaria and angioedema, have been reported in patients receiving tofacitinib. In rheumatoid arthritis trials with tofacitinib, dermatologic effects, such as erythema, pruritus, and rash were noted. During trials of tofacitinib in patients with ulcerative colitis, rash and acne vulgaris were reported in 2% or more of patients. Acne vulgaris has also been observed during postmarketing use of the drug for various indications. If a serious hypersensitivity reaction occurs, discontinue treatment and evaluate the potential cause or causes of the reaction.[52315]
Thrombosis, including deep venous thrombosis (DVT), pulmonary embolism (PE), and arterial thrombosis, has been reported in patients treated with either tofacitinib or other Janus kinase (JAK) inhibitors; many of these events were serious and some resulted in death. In a randomized, open-label, safety study in rheumatoid arthritis patients 50 years of age and older with one or more cardiovascular risk factors, higher rates of thrombosis (including DVT, PE, and arterial thrombosis), all-cause mortality (including sudden cardiac death), and major adverse cardiovascular (CV) events (MACE; defined as cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke) were observed with tofacitinib 5 mg twice daily or tofacitinib 10 mg twice daily compared to tumor necrosis factor (TNF) inhibitors. The incidence rate of DVT per 100 patient-years was 0.22, 0.28, and 0.16 for tofacitinib 5 mg twice daily, tofacitinib 10 mg twice daily, and TNF inhibitors, respectively. The incidence rates of PE per 100 patient-years were 0.18 for tofacitinib 5 mg twice daily, 0.49 for tofacitinib 10 mg twice daily, and 0.05 for TNF inhibitors. In a long-term extension study of ulcerative colitis patients treated with tofacitinib, there were 5 cases of pulmonary embolism (PE) reported in the group taking 10 mg of the drug twice daily, including one death in a patient with advanced cancer. Tofacitinib 5 mg twice daily, tofacitinib 10 mg twice daily, and TNF inhibitors had incidence rates of all-cause mortality per 100 patient-years of 0.88, 1.23, and 0.69, respectively. The incidence rate of MACE per 100 patient-years was 0.91 for tofacitinib 5 mg twice daily, 1.11 for tofacitinib 10 mg twice daily, and 0.79 for TNF inhibitors. In addition, the incidence rates of fatal or non-fatal myocardial infarction per 100 patient-years was 0.36 for tofacitinib 5 mg twice daily, 0.39 for tofacitinib 10 mg twice daily, and 0.2 for TNF inhibitors. Patients who are current or past tobacco smokers are at an additional risk of adverse events. The tofacitinib 10 mg twice daily dosage is not recommended for the treatment of rheumatoid arthritis, psoriatic arthritis or ankylosing spondylitis. Avoid tofacitinib therapy in patients at risk of thrombosis. Use the lowest effective dose of tofacitinib for the shortest duration necessary to achieve and maintain therapeutic response. Health care providers should consider the risks and benefits of tofacitinib when deciding to initiate or continue therapy, especially in patients with one or more CV risk factors and patients who are current or past smokers. Advise patients on the potential risks of tofacitinib therapy and to seek immediate medical attention if signs and symptoms of thromboembolism or thrombosis, myocardial infarction, or stroke develop. Discontinue tofacitinib therapy in any patient who develops a thrombosis, thromboembolism, myocardial infarction, or stroke.[52315] [63972]
Tofacitinib may cause a new primary malignancy, including lymphoma, solid cancers, or non-melanoma skin cancer (NMSC), and may be associated with an increased risk of Epstein Barr virus-associated post-transplant lymphoproliferative disorder (PTLD). In a randomized, open-label, safety study in rheumatoid arthritis patients 50 years of age and older with one or more cardiovascular risk factors, a higher rate of malignancies (excluding NMSC) was observed in patients treated with tofacitinib 5 mg twice daily (1.13 events per 100 patient-years) or tofacitinib 10 mg twice daily (1.13 events per 100 patient-years) compared to patients treated with tumor necrosis factor (TNF) inhibitors (0.77 events per 100 patient-years). Patients with a current or past tobacco smoking had an additional increased risk of malignancy, including lung cancer. A higher rate of lymphomas and lung cancers, subsets of all malignancies, were also observed in patients treated with both tofacitinib doses compared to TNF inhibitors. The incidence rates for lymphomas per 100 patient-years were 0.07, 0.11, and 0.02 for tofacitinib 5 mg twice daily, tofacitinib 10 mg twice daily, and TNF inhibitors, respectively. Among smokers, the incidence rates of lung cancer per 100 patient-years were 0.48 for tofacitinib 5 mg twice daily, 0.59 for tofacitinib 10 mg twice daily, and 0.27 for TNF inhibitors. The tofacitinib 10 mg twice daily dosage is not recommended for the treatment of rheumatoid arthritis, psoriatic arthritis, or ankylosing spondylitis. Among rheumatoid arthritis patients who were enrolled in 7 clinical trials, malignancies occurred in 5 patients receiving tofacitinib 5 mg twice daily (0.4 events per 100 patient-years) and 7 patients receiving tofacitinib 10 mg twice daily (0.6 events per 100 patient-years) within the first 12 months of treatment; tofacitinib was given with or without disease-modifying antirheumatic drugs (DMARDs). No malignancies were reported with placebo. One of the malignancies reported with tofacitinib 10 mg twice daily was lymphoma. The most common types of malignancy, including malignancies observed during the long-term extension, were lung and breast cancer, followed by gastric, colorectal, renal cell, prostate cancer, lymphoma, and malignant melanoma. During the psoriatic arthritis clinical trials, 3 malignancies were reported in adult patients receiving tofacitinib plus a non-biologic DMARD (n = 474) compared to no malignancies reported in the placebo plus non-biologic DMARD group (n = 106). No lymphomas were reported. Malignancies also have been reported in the long-term extension psoriatic arthritis trial. During the ulcerative colitis controlled clinical studies, which included 1,220 patients, there were no cases of solid cancer or lymphoma in patients treated with tofacitinib. In the long-term extension study, malignancies (including solid cancers and lymphomas) were observed more often in patients treated with 10 mg twice daily. In a tofacitinib dose-ranging study involving de novo renal transplant patients who received induction therapy with basiliximab, high-dose corticosteroids, and mycophenolic acid agents, Epstein Barr virus-associated PTLD occurred in 5 tofacitinib patients (2.3%) compared to zero cyclosporine patients. Lung cancer, breast cancer, melanoma, prostate cancer, and pancreatic cancer have been reported with postmarketing use of tofacitinib. NMSCs have been reported with tofacitinib therapy and, among ulcerative colitis patients, the 10 mg twice daily dose was associated with a greater risk of NMSCs. Consider periodic skin examinations for all patients at increased risk for skin cancer. Consider the risks and benefits of tofacitinib prior to initiating or continuing therapy in patients with a known malignancy (excluding NMSC), patients who develop a malignancy while receiving tofacitinib, and patients who are current or past smokers.[52315]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components.
Prior to initiating tofacitinib consider performing an active and latent tuberculosis (TB) infection evaluation, viral hepatitis screening in accordance with clinical guidelines, a complete blood count, and baseline hepatic function evaluation. Update immunizations in agreement with current immunization guidelines prior to initiating tofacitinib therapy. Avoid the use of live vaccines concurrently with tofacitinib. The interval between live vaccinations and the initiation of tofacitinib should be in accordance with current vaccination guidelines regarding immunosuppressive agents.[52315]
Treatment with tofacitinib increases the risk of serious infections that may lead to hospitalization or death. Avoid use in people with an active, serious infection, including localized infections. Use tofacitinib with caution in patients at increased risk for serious infections, including geriatric patients (65 years and older), those with chronic or recurrent infections, a history of serious or opportunistic infections, underlying conditions that may predispose to infection [diabetes mellitus, chronic lung disease, interstitial lung disease, lymphopenia (avoid use if absolute lymphocyte count less than 500 cells/mm3)], and those receiving concomitant immunosuppressants (e.g., corticosteroids, methotrexate). Patients residing in or with travel history to regions where mycoses are endemic (e.g., Ohio and Mississippi River valleys, Southwest) are at increased risk for invasive fungal infections. Viral reactivation (herpes zoster, hepatitis B) has occurred with tofacitinib treatment, with the risk of herpes zoster being higher in certain geographic regions (e.g., Japan, Korea). Perform screening for viral hepatitis in accordance with clinical guidelines before starting tofacitinib. Tofacitinib also increases the risk of tuberculosis (TB) infection. Screen all patients for active or latent TB infection prior to initiating therapy and periodically during treatment. Initiate treatment for latent TB prior to starting tofacitinib. Consider anti-tuberculosis therapy in patients with a history of latent or active TB in whom an adequate course of treatment cannot be confirmed, and in those with risk factors for TB infection. Consult a physician with expertise in treating TB about whether starting anti-tuberculosis therapy is appropriate for the individual patient. Monitor for signs and symptoms of TB and other infections during and after therapy, even in patients who tested negative for latent TB prior to initiation. For patients who develop an infection during treatment with tofacitinib, perform a prompt and complete diagnostic workup appropriate for immunocompromised patients and initiate appropriate antimicrobial therapy. Discontinue tofacitinib if a patient develops a serious infection, opportunistic infection, or sepsis.[52315]
Due to the risk for serious cardiovascular events, reserve tofacitinib for patients who have had an inadequate response or intolerance to one or more TNF inhibitors. Avoid the use of tofacitinib in people at increased risk of thrombosis and thromboembolism. Tobacco smoking (current or history of past use) adds to the increased risk of these events. Consider the benefits and risks for the individual patient before starting or continuing tofacitinib therapy, particularly in those with thrombophilia, risk factors for cardiovascular disease, or who are current or past smokers. Serious cardiovascular events have been reported with the Janus kinase (JAK) inhibitors class of medications. A higher rate of all-cause mortality (including sudden cardiovascular death), major adverse cardiovascular events (MACE; defined as cardiovascular death, non-fatal myocardial infarction (MI), and non-fatal stroke), and thrombosis [including deep venous thrombosis (DVT), pulmonary embolism (PE)] were observed in rheumatoid arthritis patients taking tofacitinib compared to patients taking tumor necrosis factor (TNF) inhibitors. Thrombosis, including DVT, PE, and arterial thrombosis, have been observed at an increased incidence in tofacitinib recipients; many events were serious and some resulted in death.[52315] [66958]
Tofacitinib may increase the risk of malignancy; reserve tofacitinib for patients who have an inadequate response or intolerance to 1 or more tumor necrosis factor (TNF) inhibitors. In a large, postmarketing, randomized safety clinical trial in rheumatoid arthritis patients, higher rates of lymphoma and malignancy [excluding non-melanoma skin cancer (NMSC)] were observed with the use of tofacitinib compared to TNF inhibitors. A higher rate of lung cancer was also observed in current or past tobacco smokers treated with tofacitinib compared to those treated with TNF inhibitors. Malignancies observed in clinical studies and in the postmarketing setting include lung cancer, breast cancer, melanoma, prostate cancer, and pancreatic cancer. Consider the benefits and risks for the individual patient before starting or continuing tofacitinib therapy, particularly in those with risk factors such as smoking, those who develop malignancy, and those with a known malignancy other than successfully treated NMCS. NMSCs have been reported in patients treated with tofacitinib; thus, periodic skin examinations are recommended for patients who are at increased risk for skin cancer.[52315] [66958]
Use tofacitinib with caution in patients who may be at increased risk for gastrointestinal (GI) perforation, such as those with a history of diverticulitis or those taking nonsteroidal anti-inflammatory drugs (NSAIDs). Promptly evaluate patients presenting with new onset abdominal symptoms for early identification of GI perforation. In people with a history of GI obstruction or severe GI narrowing (pathologic or iatrogenic), the extended-release formulation of tofacitinib (tofacitinib XR) should be used with caution. Tofacitinib XR utilizes a non-deformable material which may cause obstructive symptoms in patients with known GI strictures.[52315]
Routine monitoring of liver function tests (LFT) is recommended during treatment with tofacitinib. Use of tofacitinib is not recommended in people with severe hepatic impairment (Child-Pugh class C) or hepatic failure. Dosage adjustments are required in patients with moderate hepatic impairment (Child-Pugh class B).[52315]
Avoid starting tofacitinib in patients with neutropenia, defined as an absolute neutrophil count (ANC) less than 1,000 cells/mm3. Monitor neutrophil counts at baseline and during treatment. If the ANC decreases to 500 to 1,000 cells/mm3, interrupt therapy until the ANC is above 1,000 cells/mm3. For patients with ulcerative colitis taking the higher dose, dose reductions are recommended for this ANC, with resumption of the previous dosing when the ANC is greater than 1,000 cells/mm3, based on clinical response. Discontinue tofacitinib if the ANC falls below 500 cells/mm3, regardless of the indication.[52315]
Avoid starting tofacitinib in patients with anemia, defined as a hemoglobin less than 9 g/dL. Monitor hemoglobin concentrations at baseline and during treatment. If the hemoglobin decreases to less than 8 g/dL or decreases by more than 2 g/dL from baseline, interrupt dosing until hemoglobin values have normalized.[52315]
Patients with moderate or severe renal impairment have increased tofacitinib exposure. Dosage adjustments are recommended in these patients, including those with renal failure undergoing hemodialysis. No dosage adjustment is required in mild renal impairment.[52315]
Avoid the use of tofacitinib during pregnancy. Available data from the tofacitinib pregnancy registry (n = 11), pharmacovigilance, and published literature are insufficient to determine the drug-associated risk of major birth defects, miscarriages, or other adverse maternal or fetal outcomes.[52315] [61808] [62180] In the tofacitinib clinical development program in rheumatoid arthritis and other registry monitoring data, birth defects (e.g., pulmonary valve stenosis), and miscarriages were reported.[62380] Based on animal studies, tofacitinib may cause fetal harm. Fetocidal and teratogenic effects were noted when pregnant rats and rabbits received tofacitinib during the period of organogenesis at exposures of 73-times and 6.3-times the human dose of 10 mg twice daily, respectively. Teratogenic effects observed include external and soft tissue malformations of anasarca and membranous ventricular septal defects, respectively; cranial and skeletal malformations or variations; thoracogastroschisis, omphalocele, and membranous ventricular septal defects. In addition, reductions in live litter size, postnatal survival, and pup body weights occurred with exposure levels approximately 36-times the MRHD of 10 mg twice daily. No developmental toxicity was observed in rabbits at exposure levels approximately 1.5-times the MRHD of 10 mg twice daily.[52315]
Inform tofacitinib recipients of the potential reproductive risk if they are of childbearing reproductive potential; consider pregnancy planning and prevention for these individuals. Fetocidal and teratogenic effects were noted when animals were given tofacitinib during the period of organogenesis, and there is potential for fetal harm. While specific contraception requirements have not been advised in the label, consider the use of adequate contraception in those of childbearing reproductive potential. Advise these patients to contact their health care provider immediately if they become pregnant or if pregnancy is suspected. The administration of tofacitinib may result in reduced fertility (infertility) in females of reproductive potential based on animal data. It is not known if this effect is reversible. Reduced fertility due to an increased post-implantation loss was observed in animals exposed to tofacitinib levels approximately 8.3-times the maximum recommended human dose (MRHD) of 10 mg twice daily. There was no impairment of female animal fertility at exposure levels of tofacitinib of 0.5-times the MRHD. No effect was seen on male fertility, sperm motility, or sperm concentration.[52315] [62380]
Advise tofacitinib recipients not to breastfeed. Instruct patients to avoid breast-feeding during treatment and for at least 18 hours after the last dose of the immediate-release tablets or 36 hours after the last dose of extended-release tablets (approximately 6 elimination half-lives). Based on published data, tofacitinib is present in human milk. Data on the effects of the drug on the breastfed infant is limited to a few cases with no reported adverse effects. Additionally, there are no data on the effects of tofacitinib on milk production.[52315] [62180] Assess indication and patient-specific factors before considering an alternative agent.[61808] [62180]
Patients who undergo surgery while taking biologic therapy, such as tofacitinib, may be at greater risk for postoperative infections. For a planned procedure, balance the risk of postoperative infection against the risk of developing a severe or unstable disease by stopping the biologic therapy. The American College of Rheumatology recommends holding tofacitinib for 3 days before undergoing total knee or total hip arthroplasties.[71153]
Tofacitinib is an oral Janus kinase (JAK) inhibitor. Janus kinases are intracellular enzymes that transmit signals arising from cytokine or growth factor receptor interactions such as interferons, interleukins, and erythropoietin on the cellular membrane to influence cellular processes of immune cell function and hematopoiesis. JAK-mediated signaling is pivotal in immune activation, as cytokine receptors are expressed on most immune cells. Upon ligand and receptor interaction, JAKs are activated and, thus, phosphorylate their receptors and activate the signal transducers and activators of transcription proteins, which modulate intracellular activity including gene expression. Tofacitinib affects the signaling pathway at the point of JAKs. Cytokine signaling is transmitted through the pairing of JAKs such as JAK1/JAK3, JAK1/JAK2, JAK/TyK2, and JAK2/JAK2. Tofacitinib primarily inhibits JAK1 and JAK3 and, to a lesser extent, JAK2. For example, tofacitinib inhibited the in vitro activities of JAK1/JAK2, JAK1/JAK3, and JAK2/JAK2 combinations with IC50 of 406, 56, and 1,377 nM, respectively. The primary inhibition of JAK1 and JAK3 by tofacitinib is thought to be advantageous in terms of potential hematologic toxicity because hematopoietic cytokine receptors, such as the erythropoietin receptor, associate with JAK2 homodimers. However, the relevance of specific JAK combinations to therapeutic effectiveness is not known.[52315]
Revision Date: 10/21/2025, 03:56:12 PMTofacitinib is administered orally. Protein binding is approximately 40%, and it binds predominantly to albumin; it does not appear to bind to alpha1-acid glycoprotein. Tofacitinib distributes equally between red blood cells and plasma. A volume of distribution (Vd) of 87 L was found after intravenous administration. Metabolism of tofacitinib is primarily mediated by CYP3A4 with a minor contribution from CYP2C19. Approximately 70% is cleared by hepatic metabolism, and 30% is cleared by renal excretion of the parent drug. After oral administration of the immediate-release and extended-release tablets, the elimination half-life is around 3 hours and 6 to 8 hours, respectively. In a human radiolabeled study, more than 65% of the total circulating radioactivity was accounted for by unchanged tofacitinib, with the remaining 35% attributed to 8 inactive metabolites, each accounting for less than 8% of total radioactivity. Tofacitinib pharmacokinetics were similar between rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and ulcerative colitis patients.[52315]
Rapid decreases in serum C-reactive protein (CRP) were observed and maintained throughout the treatment period among patients with rheumatoid arthritis. The observed changes in CRP do not reverse fully within 2 weeks after discontinuation of tofacitinib. The results indicate a longer duration of activity as compared with the pharmacokinetic half-life.[52315]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4 and CYP2C19
Tofacitinib is a substrate of primarily CYP3A4 with minor contributions from CYP2C19. Patients receiving potent CYP3A4 inhibitors or receiving 1 or more concomitant medications that result in both moderate inhibition of CYP3A4 and potent inhibition of CYP2C19 require tofacitinib dose reductions.[52315] The potential for tofacitinib to inhibit transporters such as P-glycoprotein (P-gp) and organic anionic or cationic transporters at therapeutic concentrations is low. In vitro data showed that it does not significantly inhibit or induce the activity of the major human drug-metabolizing CYPs (CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A4) at concentrations corresponding to the steady-state Cmax of a 10 mg twice daily dose. In vivo, no changes in the pharmacokinetic parameters of the CYP3A4 substrate midazolam were noted when coadministered. In patients with rheumatoid arthritis, the oral clearance does not vary with time and indicates that tofacitinib does not normalize CYP enzyme activity. Thus, tofacitinib is not expected to cause clinically relevant increases in the metabolism of CYP substrates.[52315]
The absolute oral bioavailability of tofacitinib is 74%.
Immediate-release formulations
After oral administration, peak plasma concentration (Cmax) occurs within 0.5 to 1 hour, and a dose-proportional increase in systemic exposure is observed in the therapeutic dose range. After twice-daily administration, steady-state concentrations are achieved in 24 to 48 hours with negligible accumulation. Patient population pharmacokinetic analyses indicated that pharmacokinetic characteristics were similar between patients with rheumatoid arthritis, psoriatic arthritis, and ulcerative colitis. The coefficient of variation (%) in AUC of tofacitinib was generally similar across patients with different disease states, ranging from 22% to 34%. In clinical trials, tofacitinib was administered without regard to meals. Coadministration of tofacitinib with a high-fat meal resulted in no changes in systemic exposure, although the Cmax was reduced by 32%.[52315]
Extended-release formulations
After oral administration, peak plasma concentration (Cmax) occurs at approximately 4 hours. After coadministration of tofacitinib 11 mg and 22 mg extended-release tablets with a high-fat meal, the peak plasma concentrations (Cmax) were increased by 27% and 19%, respectively, and the time to maximum concentration (Tmax) was extended by 1 hour; there was no change in tofacitinib exposure (AUC). After once-daily administration, steady-state concentrations are achieved within 48 hours with negligible accumulation.[52315]
Patients with moderate hepatic impairment have increased blood concentrations of tofacitinib compared to those with normal hepatic function. Higher blood concentration may increase the incidence of adverse effects of tofacitinib therapy. Dosage adjustments are recommended in patients with moderate hepatic impairment. Tofacitinib is not recommended for patients with severe hepatic impairment, as it has not been studied in this patient population.[52315]
Increased systemic exposure of tofacitinib occurs with moderate or severe renal impairment, and dosage adjustments are needed. The mean tofacitinib AUC was increased by about 40% in patients with end-stage renal disease (ESRD) maintained on hemodialysis compared to healthy patients; this is consistent with the approximate 30% contribution of renal clearance to the total tofacitinib clearance. Tofacitinib dosage adjustments are also recommended in patients with ESRD maintained on hemodialysis.[52315]
Bodyweight significantly impacts tofacitinib exposure, which supports weight-based dosing in the pediatric population.[52315]
Population pharmacokinetic analysis in patients with rheumatoid arthritis indicated no clinically relevant change in tofacitinib exposure after accounting for differences in creatinine clearance between patients based on age. Of the 1,156 tofacitinib-treated patients in the UC program, a total of 77 patients (7%) were 65 years of age or older. The number of patients aged 65 years and older was not sufficient to determine whether they responded differently from younger patients.[52315]
Population pharmacokinetic analysis in patients with rheumatoid arthritis indicated no clinically relevant change in tofacitinib exposure after accounting for differences in creatinine clearance between patients based on gender.[52315]
Population pharmacokinetic analysis in patients with rheumatoid arthritis indicated no clinically relevant change in tofacitinib exposure after accounting for differences in creatinine clearance between patients based on race.[52315]
Population PK analysis in rheumatoid arthritis patients indicated no clinically relevant change in tofacitinib exposure, after accounting for differences in creatinine clearance between patients based on weight. An approximately linear relationship between body weight and volume of distribution was observed, resulting in higher peak (Cmax) and lower trough (Cmin) tofacitinib concentrations in lighter patients. However, this difference is not considered to be clinically relevant.[52315]
Avoid the use of tofacitinib during pregnancy. Available data from the tofacitinib pregnancy registry (n = 11), pharmacovigilance, and published literature are insufficient to determine the drug-associated risk of major birth defects, miscarriages, or other adverse maternal or fetal outcomes.[52315] [61808] [62180] In the tofacitinib clinical development program in rheumatoid arthritis and other registry monitoring data, birth defects (e.g., pulmonary valve stenosis), and miscarriages were reported.[62380] Based on animal studies, tofacitinib may cause fetal harm. Fetocidal and teratogenic effects were noted when pregnant rats and rabbits received tofacitinib during the period of organogenesis at exposures of 73-times and 6.3-times the human dose of 10 mg twice daily, respectively. Teratogenic effects observed include external and soft tissue malformations of anasarca and membranous ventricular septal defects, respectively; cranial and skeletal malformations or variations; thoracogastroschisis, omphalocele, and membranous ventricular septal defects. In addition, reductions in live litter size, postnatal survival, and pup body weights occurred with exposure levels approximately 36-times the MRHD of 10 mg twice daily. No developmental toxicity was observed in rabbits at exposure levels approximately 1.5-times the MRHD of 10 mg twice daily.[52315]
Advise tofacitinib recipients not to breastfeed. Instruct patients to avoid breast-feeding during treatment and for at least 18 hours after the last dose of the immediate-release tablets or 36 hours after the last dose of extended-release tablets (approximately 6 elimination half-lives). Based on published data, tofacitinib is present in human milk. Data on the effects of the drug on the breastfed infant is limited to a few cases with no reported adverse effects. Additionally, there are no data on the effects of tofacitinib on milk production.[52315] [62180] Assess indication and patient-specific factors before considering an alternative agent.[61808] [62180]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.