ThisiscontentfromElsevier'sDrugInformation
Trazodone
Learn more about Elsevier’s Drug Information today! Get the reliable drug data and decision support you need to enhance patient safety through timely and accessible information.
150 mg/day PO in divided doses, initially. May increase the dose by 50 mg/day every 3 to 4 days if inadequate response and depending on tolerability. Usual Max: 400 mg/day. Max: 600 mg/day, in divided doses.[43857] [63609] [70469] [71974]
25 mg PO once daily at bedtime, or alternatively 1.5 to 2 mg/kg/day PO in divided doses, initially. May increase the dose every 3 to 4 days if inadequate response and based on tolerability. Max: 100 to 150 mg/day or 6 mg/kg/day in divided doses. Due to limited data, trazodone is not considered a first-line agent in this population.[52618] [57775]
1.5 to 2 mg/kg/day PO in divided doses, initially. May increase the dose every 3 to 4 days if inadequate response and based on tolerability. Max: 6 mg/kg/day in divided doses (not to exceed 150 mg/day). Due to limited data, trazodone is not considered a first-line agent in this population.[52618] [57775]
25 to 50 mg PO once daily at bedtime, initially. Increase the dose as needed and tolerated. Max: 150 mg/day. Guidelines recommend against trazodone for chronic insomnia based on a short-term trial which evaluated trazodone 50 mg/day and found no clinically significant improvement in sleep outcomes and significantly more side effects (e.g., headache, daytime somnolence) vs. placebo; other studies were considered inadequate for assessment. Antidepressants like trazodone may be considered for insomnia when there is a co-existing mood disorder and therapeutic antidepressant doses are used. Findings from one large systematic review suggest a small improvement in sleep quality during short-term use of low-dose trazodone; however, additional studies are needed to determine long-term safety and efficacy.[52062] [58830] [58831] [58836] [60017] [62207] [64074] [64075] [64079]
12.5 to 25 mg PO once daily at bedtime, initially. Increase the dose as needed and tolerated. Max: 150 mg/day. Data to support the use of trazodone in pediatric patients is limited; most studies utilize adult data or include pediatric patients with concomitant neurodevelopmental disorders or depressive symptoms which may contribute to sleep disruptions. As sleep disturbances can be a presenting symptom of underlying physical or psychiatric concerns, treatment should occur after a careful evaluation of the patient.[63272] [70466] [70467]
150 mg/day PO in divided doses, initially. May increase by 50 mg/day every 3 to 4 days as needed/tolerated. In one study, the mean maximum daily effective dose was 255 mg/day. Usual outpatient max: 400 mg/day. Max: 600 mg/day.[52067]
600 mg/day PO for immediate-release dosage forms.
600 mg/day PO for immediate-release dosage forms.
Safety and efficacy have not been established; off-label doses have not exceeded 150 mg/day PO.
6 to 12 years: Safety and efficacy have not been established; off-label max: 6 mg/kg/day PO; off-label doses have not exceeded 150 mg/day PO for those 12 years and older.
1 to 5 years: Safety and efficacy have not been established.
Safety and efficacy have not been established.
Safety and efficacy have not been established.
Use with caution since trazodone is extensively metabolized in the liver and has not been studied in people with hepatic impairment.[43857][71974]
Use with caution since trazodone has not been studied in people with renal impairment.[43857][71974]
† Off-label indication










Trazodone is an oral selective serotonin reuptake inhibitor and a serotonin type 2 receptor antagonist. It is approved for the treatment of major depressive disorder in adults. Due to its sedating effects, trazodone is also commonly used off-label at low doses for the treatment of insomnia. Due to a higher side effect burden versus traditional first-line agents such as the selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs), trazodone is typically used as a second-line agent for depression in adults and may be particularly helpful for depressed patients with concomitant insomnia. All product labels for antidepressants contain a boxed warning related to an increased risk of suicidality in children, adolescents, and young adults during the initial stages of therapy when treating depression or other conditions; therefore, the necessity of pharmacologic therapy versus the potential risks should be carefully considered in these populations. Trazodone was initially FDA approved in 1981.[43857][71974][65503][70451][70469]
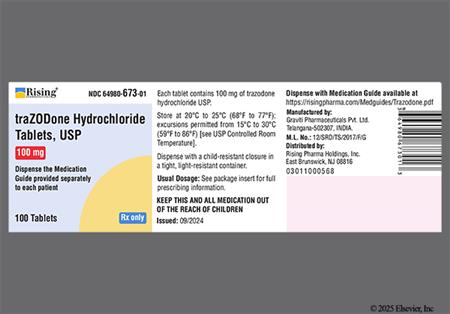
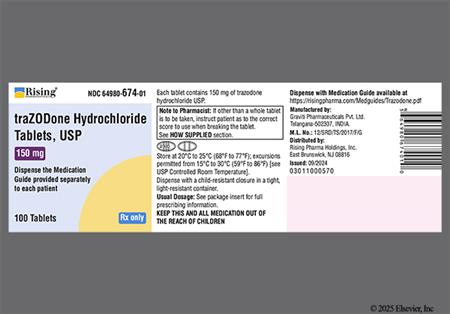
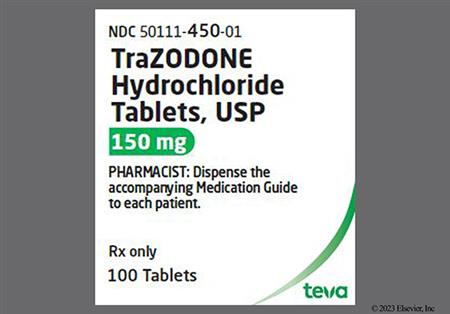
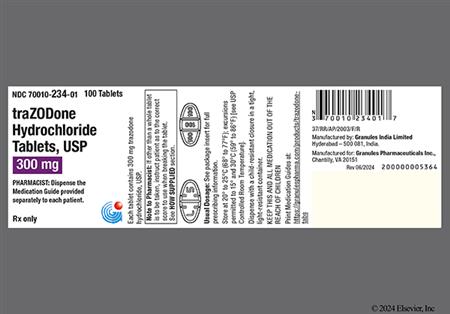
For storage information, see the specific product information within the How Supplied section.
Immediate-release tablets
Oral solution
Drowsiness (24% to 41%) and dizziness (20% to 28%) are the most common central nervous system (CNS) side effects of trazodone. Other CNS effects occurring in 2% or more of trazodone recipients in clinical trials included headache (10% to 20%), nervousness (6% to 15%), fatigue (6% to 11%), confusion (5% to 6%), impaired concentration (1% to 3%), and disorientation (0 to 2%). CNS or psychiatric side effects occurring in less than 2% of treated patients included hallucinations/delusions, hypomania, and memory impairment. Abnormal dreams, agitation, anxiety, hallucinations, insomnia, paranoid reaction (paranoia), psychosis, and stupor have been reported postmarketing.[43857] [71974]
Mania can occur in persons predisposed to bipolar disorder during treatment with an antidepressant. Monitor all antidepressant-recipients for worsening of depression and/or the emergence of suicidal behaviors or suicidal ideation, especially during the initial months of drug therapy and after dosage changes. Caregivers and/or trazodone recipients should immediately notify the care team of changes in behavior or suicidal ideation during trazodone treatment. In a pooled analysis of placebo-controlled trials of antidepressants (n = 4,500 pediatrics and 77,000 adults), there was an increased risk for suicidal thoughts and behaviors in people 24 years of age and younger receiving an antidepressant versus placebo, with considerable variation in the risk of suicidality among drugs. The difference in the absolute risk of suicidal thoughts and behaviors across different indications was highest in those with major depression. No suicides occurred in any of the pediatric trials. These studies did not show an increased risk of suicidal thoughts and behavior with antidepressant use in people over 24 years of age. There was a reduction in risk with antidepressant use in adults 65 years and older.[43857] [71974]
Hypotension (4% to 7%), including orthostatic hypotension, and syncope (3% to 5%), have occurred with trazodone use. Other cardiovascular-related adverse effects associated with trazodone include hypertension (1% to 2%), and shortness of breath (1.3%). Postmarketing reports have also included cases of chest pain (unspecified), cardiospasm, congestive heart failure, cerebrovascular accident (stroke), AV block or other conduction block, myocardial infarction, cardiac arrest.[43857] [71974]
Cardiac arrhythmias (i.e., arrhythmia exacerbation) and palpitations (up to 7% of outpatients in clinical data) have been reported with trazodone at rates lower than what has been documented with tricyclic antidepressants. Isolated premature ventricular contractions (PVCs), ventricular couplets and short episodes (3 to 4 beats) of ventricular tachycardia have also occurred. Bradycardia and atrial fibrillation have been noted in postmarketing reports with trazodone use. Additionally, there have been postmarketing reports of QT prolongation, Torsade de Pointes, and ventricular tachycardia; some events occurred with trazodone at doses of 100 mg per day or less.[43857] [71974]
Various neurologic and musculoskeletal complaints have been reported with trazodone use. Myalgia (more than 1% and up to 6%), tremor (3% to 5%), incoordination or abnormal coordination (2% to 5%) have been reported. Other adverse reactions occurring at an incidence of less than 2% with the use of trazodone in clinical studies included: akathisia, impaired speech (dysarthria), muscle twitches, numbness, and paresthesias. Postmarketing reports have included aphasia, ataxia, extrapyramidal symptoms, grand mal seizures, paresthesias, tardive dyskinesia, and vertigo.[43857] [71974]
Various skin, skin structure, hypersenstivitiy, and subcutaneous tissue adverse reactions have been reported with trazodone use. Photosensitivity was reported in less than 1% of patients during clinical trials; the mechanism of this reaction is not known. Night sweats (more than 1%), acne vulgaris (less than 1%), hyperhidrosis (less than 1%), alopecia, flushing or vasodilation, psoriasis, rash, urticaria, pruritus, leukonychia, hirsutism, drug eruption, and sweating/clamminess (up to 1.4%) have also been reported. Hypersensitivity has been reported in less than 1% of patients receiving trazodone.[43857] [71974]
Gastrointestinal (GI) adverse reactions have been reported with trazodone use. Xerostomia (15% to 34%) is a common side effect during therapy with trazodone and is believed to be due to alpha-1 adrenergic blocking effects of the drug. Increased salivation and hypersalivation have also been reported with trazodone use. Other GI-related adverse effects include abdominal pain (more than 1%), constipation (7% to 8%), diarrhea (0% to 9%), dysgeusia (up to 1.4%), flatulence, gastroesophageal reflux (less than 1%), increased amylase, nausea (10% to 21%), and vomiting (up to 12.7%).[43857] [71974]
Hepatic-related adverse events noted in postmarketing reports of trazodone include cholestasis, hyperbilirubinemia, jaundice, and altered hepatic enzymes.[43857] [71974]
Appetite stimulation, weight gain (1% to 5%), and weight loss (up to 6%) have been reported in people receiving trazodone.[43857] [71974]
Blurred vision (6% to 15%) may occur with trazodone therapy. Other ophthalmic effects reported with trazodone use include red, tired, or itchy eyes (0% to 3%). Diplopia has been reported postmarketing. The pupillary dilation that occurs following use of many antidepressant drugs including trazodone may trigger an attack of closed-angle glaucoma in a person with anatomically narrow angles who does not have a patent iridectomy. Trazodone recipients experiencing visual changes, ocular symptoms, or eye pain should have an ophthalmologic examination.[43857] [71974]
Ear and labyrinth disorders reported with trazodone use include hypoacusis/hearing loss (less than 1%) and tinnitus (less than 1.4%).[43857] [71974]
Urinary adverse effects that have been reported with trazodone use include delayed urine flow, increased urinary frequency (less than 2%), urinary incontinence, urinary retention, urinary urgency (greater than 1%), urinary incontinence (less than 1%), bladder discomfort or pain (less than 1%), and hematuria.[43857] [71974]
Cases of priapism (painful erections greater than 6 hours in duration) have been reported in males receiving trazodone. Priapism, if not treated promptly, can result in irreversible damage to the erectile tissue. Males who have an erection lasting more than 4 hours, whether painful or not, should immediately discontinue the drug and seek emergency medical attention. Other reproductive and sexual adverse reactions included clitorism (clitoral priapism in females), impotence (erectile dysfunction) (less than 1%), ejaculation dysfunction (retrograde or no ejaculation) (1.5%), orgasm dysfunction (less than 1%), libido increase (less than 2%), and libido decrease (1.3 to 1.5%).[43857] [71974]
Adverse endocrine effects associated with trazodone use in females include early menses and missed periods (i.e., menstrual irregularity), breast enlargement or engorgement, and breast discharge or lactation.[43857] [71974]
Hematologic lab abnormalities reported in controlled clinical trials include anemia (less than 2%). Postmarketing reports of hemolytic anemia, leukocytosis, and methemoglobinemia have also been associated with the use of trazodone.[43857] [71974]
Hyponatremia may occur as a result of treatment with serotonergic antidepressants, including trazodone. Cases with serum sodium lower than 110 mmol/L have been reported. Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which can lead to falls. Signs and symptoms associated with more severe and/or acute cases have included hallucination, syncope, seizure, coma, respiratory arrest, and death. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Geriatric adults, people taking diuretics, and those who are volume-depleted may be at greater risk of developing hyponatremia. In people with symptomatic hyponatremia, discontinue trazodone and institute appropriate medical intervention.[43857] [71974]
Sinus/nasal congestion (3% to 6%), malaise (0% to 3%), and shortness of breath or dyspnea (less than 2%) were reported as adverse reactions during clinical trials with trazodone. Other general adverse effects reported in postmarketing use have included chills, edema, unexplained death, and weakness. Respiratory disorders reported in postmarketing use include apnea.[43857] [71974]
The use of serotonergic antidepressants, including trazodone, can precipitate serotonin syndrome, a potentially life-threatening condition. The coadministration of trazodone with other serotonergic medications can increase the risk of serotonin syndrome. Symptoms may include nausea, vomiting, sedation, dizziness, diaphoresis (sweating), facial flush, mental status changes, myoclonia, restlessness, shivering, and elevated blood pressure. If serotonin syndrome becomes evident during treatment, trazodone and any other serotonergic agents should be discontinued and appropriate supportive symptomatic medical treatment should be initiated.[43857] [71974]
The coadministration of certain medications may lead to harm and require avoidance or therapy modification; review all drug interactions prior to concomitant use of other medications.
This medication is contraindicated in patients with a history of hypersensitivity to it or any of its components. Trazodone use should also be avoided in people with a hypersensitivity to other phenylpiperazine antidepressants (e.g.,nefazodone).[47267]
Safety and efficacy of trazodone for the treatment of depression have not been established in pediatric patients less than 18 years of age. A boxed warning in the product label describes the risk of suicidality and suicidal ideation in children, adolescents, and young adults receiving antidepressants. Monitor all patients receiving antidepressants closely for clinical worsening, suicidal ideation, and unusual changes in mood or behavior, especially during the first few months of therapy and after any dosage adjustment. Instruct caregivers and patients to immediately notify the prescriber of changes in behavior or suicidal ideation. Consider changing the therapeutic regimen or discontinuing the medication in patients with persistent or worrisome symptoms, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms. In a pooled analysis of placebo-controlled trials of antidepressants (n = 4,500 pediatrics and 77,000 adults), there was an increased risk for suicidal thoughts and behaviors in people 24 years of age and younger receiving an antidepressant versus placebo, with considerable variation in the risk of suicidality among drugs. The difference in absolute risk of suicidal thoughts and behaviors across different indications was highest in those with major depression. The need for an antidepressant in children, adolescents, or young adults for any use must be weighed against the risk of suicidality; it is unknown if this risk extends to long-term use. Monitor for symptom worsening or suicidality, especially at treatment initiation or after dose changes.[63609] [71974]
Activation of mania, hypomania, or a mixed episode may occur with medications used to treat depression, especially in people predisposed to bipolar disorder. A major depressive episode may be the initial presentation of bipolar disorder. Prior to initiating treatment with trazodone, people with depressive symptoms should be screened for risk factors for bipolar disorder, including a detailed personal psychiatric history and family history of bipolar disorder, suicide, and/or depression. If an individual taking trazodone develops symptoms consistent with mania or hypomania, the medication should be discontinued, and appropriate therapy should be initiated.[63609] [71974]
Avoid use of trazodone in people with baseline QT prolongation or who have conditions that may increase the risk of QT prolongation or torsade de pointes, including bradycardia, congenital long QT syndrome, hypocalcemia, hypokalemia, hypomagnesemia, geriatric adults, females, structural abnormalities that interfere with electrical conduction (e.g., cardiomyopathy, coronary artery disease, ischemic heart disease), or in those who have other additional risk factors for QT prolongation or torsade de pointes. The use of other medications that have been associated with QT prolongation or torsade de pointes may further increase risk.[65180] [67452] [72115] [72116] [72117] [72118] [63609] [71974] Trazodone should also be avoided in people with a history of cardiac arrhythmias and is not recommended for use in during the initial recovery phase of myocardial infarction. Clinical studies indicate that trazodone may be arrhythmogenic in people with pre-existing cardiac disease; caution and close monitoring is advised when giving trazodone to people with cardiac disease.[63609] [71974]
Trazodone has the potential to impair judgment, thinking, or motor skills. Patients should use caution when driving or operating machinery or participating in other activities requiring coordination and concentration until they are reasonably certain that trazodone does not affect them adversely. Trazodone may enhance the response to alcohol, barbiturates, and other CNS depressants.[43857] [71974]
Antidepressants, including trazodone, are associated with significant hyponatremia resulting from the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Older adults, people taking diuretics, and those who have hypovolemia appear to be at greatest risk. Hyponatremia during antidepressant use has resulted in serum sodium levels less than 110 mmol/L in some cases. However, the adverse effect appears to be reversible upon discontinuation of the causative medication. Symptomatic hyponatremia may require discontinuation of trazodone, as well as implementation of the appropriate medical interventions.[43857] [71974]
There is limited data examining the use of trazodone during electroconvulsive therapy (ECT). While limited case reports indicate minimal effect on ECT-related seizure duration with trazodone, there have been reports of reduced seizure threshold and increased risk of serotonin syndrome when other serotonergic agents were given concomitantly with ECT.[70461]
Caution is recommended when prescribing trazodone to people with closed-angle glaucoma. The pupillary dilation that can occur with antidepressants may precipitate a closed-angle glaucoma attack in patients with anatomically narrow angles who do not have a patent iridectomy.[43857] [71974]
Use trazodone with caution in people who have conditions that might predispose them to priapism (e.g., sickle cell disease, multiple myeloma, or leukemia), or in people with anatomical deformation of the penis (e.g., penile angulation, cavernosal fibrosis, or Peyronie disease). Rare cases of priapism have been reported with trazodone use.[43857] [71974]
Although available studies cannot definitively establish the absence of risk, published prospective cohort studies, case series, and case reports over several decades with trazodone use during pregnancy have not identified any drug-associated risks of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Hoewver, available studies have methodological limitations, including small sample sizes and inconsistent comparator groups. A prospective, longitudinal study followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants at the beginning of pregnancy. Those who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than those who continued antidepressants. Consider the risk of untreated depression versus the potential for adverse fetal outcomes when discontinuing or changing treatment with trazodone during pregnancy and postpartum. There is a pregnancy exposure registry that monitors outcomes in pregnant patients exposed to trazodone; information about the registry can be obtained at womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants or by calling 1-866-961-2388 or 1-844-405-6185.[43857] [71974]
Data from published literature indicate that trazodone is excreted into breast milk at low levels; however, limited data from postmarketing reports have not identified trazodone-associated adverse effects in the breastfed child. There are no data regarding the effect of trazodone on milk production. Lactating individuals should advise their physician of their intention to breastfeed and alternative therapy may be considered. A pooled analysis found that maternal use of sertraline, nortriptyline, and paroxetine usually produced undetectable or low drug concentrations in infant serum and, therefore, may be the preferred antidepressants for breast-feeding individuals. However, the individual's prior antidepressant trials and the risk of symptom relapse during transition to a new medication may preclude the use of alternatives. The developmental and health benefits of breast-feeding should be considered along with the mother's underlying condition, clinical need for treatment, and the risk of adverse effects in the breastfed infant.[38831] [43857] [45642]
Clinical experience with trazodone has not identified differences in response to the drug in geriatric compared to younger adults, but data are limited. Geriatric adults appear more susceptible than younger adults to trazodone adverse reactions such as sedation, orthostatic hypotension, or hyponatremia due to SIADH.[43857] [71974] The U.S. Omnibus Budget Reconciliation Act (OBRA) regulates antidepressant use in long-term care facilities. When used to manage behavior, stabilize mood, or treat a psychiatric disorder, tapering as outlined in the OBRA guidelines should be attempted unless clinically contraindicated. Dosages and durations of treatment used should align with prescribing labels, published literature recommendations, and expert guidelines.[60742]
Trazodone has a unique mechanism of action via activity at a variety of receptors, making it distinct from other traditional antidepressant medications. At low doses, trazodone has antagonistic effects at alpha-1 adrenergic receptors and histamine H1 receptors, leading to an increased risk for postural hypotension, syncope, and sedation. Unlike other sedating antidepressants, trazodone has minimal effects on REM sleep while improving sleep efficiency and subjective sleep quality. At increased doses, trazodone exerts antidepressant effects by selectively inhibiting reuptake of serotonin (5-HT) while also acting as an antagonist at 5-HT2 receptors. Trazodone is also a partial agonist at 5-HT1A receptors, which may provide mild anxiolytic activity.[43857][58831][71974]
Revision Date: 09/24/2025, 01:31:00 AMTrazodone is administered orally. The drug is 89% to 95% protein bound. In vitro studies show that trazodone undergoes metabolism via oxidation to an active metabolite, m-chlorophenylpiperazine (mCPP), by CYP3A4. Other metabolic pathways that may be involved in the metabolism of trazodone have not been well characterized. Less than 1% of an oral dose is excreted unchanged in the urine. Elimination is mainly through the urine, with about 70% to 75% of a dose excreted (mainly as metabolites) within 72 hours. The average terminal elimination half-life of trazodone under fed state is 18 hours.[43857][71974]
Affected cytochrome P450 isoenzymes and drug transporters: CYP3A4
Trazodone is extensively metabolized in the liver, primarily by CYP3A4. The concomitant use of trazodone and strong CYP3A4 inhibitors increased the exposure of trazodone compared to the use of trazodone alone, and a lower dosage of trazodone may be needed.[43857][71974]
Tablets (immediate-release): Trazodone is well absorbed after oral administration, without selective localization in any tissue. Food affects absorption. When taken with or shortly after a meal, there may be an increase in the amount of drug absorbed, a decrease in peak plasma concentrations, and an increase in the time to reach peak concentrations. Peak concentrations are achieved 1 hour after dosing on an empty stomach or 2 hours after dosing when taken with food.[43857]
Oral Solution: No clinically significant difference in pharmacokinetic parameters were observed between the oral solution and the immediate-release trazodone tablet administered under fed conditions. Peak plasma levels occur approximately 1 hour after administration under fed conditions. Ingestion of a high-fat meal with the oral solution lowers the mean Cmax of trazodone by 31% and increases the mean AUC by 8%. Median Tmax was similar between fed and fasted conditions.[71974]
Trazodone has not been studied in people with hepatic impairment but is metabolized extensively in the liver.[43857][71974]
Trazodone has not been studied in people with renal impairment. The primary route of excretion for trazodone metabolites, active and inactive, is via the kidney.[43857][71974]
Although available studies cannot definitively establish the absence of risk, published prospective cohort studies, case series, and case reports over several decades with trazodone use during pregnancy have not identified any drug-associated risks of major birth defects, miscarriage, or adverse maternal or fetal outcomes. Hoewver, available studies have methodological limitations, including small sample sizes and inconsistent comparator groups. A prospective, longitudinal study followed 201 pregnant women with a history of major depressive disorder who were euthymic and taking antidepressants at the beginning of pregnancy. Those who discontinued antidepressants during pregnancy were more likely to experience a relapse of major depression than those who continued antidepressants. Consider the risk of untreated depression versus the potential for adverse fetal outcomes when discontinuing or changing treatment with trazodone during pregnancy and postpartum. There is a pregnancy exposure registry that monitors outcomes in pregnant patients exposed to trazodone; information about the registry can be obtained at womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/antidepressants or by calling 1-866-961-2388 or 1-844-405-6185.[43857] [71974]
Data from published literature indicate that trazodone is excreted into breast milk at low levels; however, limited data from postmarketing reports have not identified trazodone-associated adverse effects in the breastfed child. There are no data regarding the effect of trazodone on milk production. Lactating individuals should advise their physician of their intention to breastfeed and alternative therapy may be considered. A pooled analysis found that maternal use of sertraline, nortriptyline, and paroxetine usually produced undetectable or low drug concentrations in infant serum and, therefore, may be the preferred antidepressants for breast-feeding individuals. However, the individual's prior antidepressant trials and the risk of symptom relapse during transition to a new medication may preclude the use of alternatives. The developmental and health benefits of breast-feeding should be considered along with the mother's underlying condition, clinical need for treatment, and the risk of adverse effects in the breastfed infant.[38831] [43857] [45642]
Cookies are used by this site. To decline or learn more, visit our cookie notice.
Copyright © 2025 Elsevier, its licensors, and contributors. All rights are reserved, including those for text and data mining, AI training, and similar technologies.